Systemic Administration of Tranexamic Acid Improves Postoperative Outcome in Abdominoplasty
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics
2.2. Study Design
2.3. Surgical and Perioperative Procedures
2.4. Statistical Analysis
3. Results
3.1. Demographic Data
3.2. Surgery-Specific Data
3.3. Postoperative Outcome and Drainage Pattern
3.4. Complications
3.5. Laboratory Parameters
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| TXA | Tranexamic Acid |
| Hb | hemoglobin |
| Hct | hematocrit |
| BMI | Body Mass Index |
| PTS | Progressive tension sutures |
References
- Almutairi, K.; Gusenoff, J.A.; Rubin, J.P. Body contouring. Plast. Reconstr. Surg. 2016, 137, 586e–602e. [Google Scholar] [CrossRef]
- Global Survey 2024. Available online: https://www.isaps.org/discover/about-isaps/global-statistics/global-survey-2024-full-report-and-press-releases/ (accessed on 10 September 2025).
- Stewart, K.; Stewart, D.; Coghlan, B.; Harrison, D.; Jones, B.; Waterhouse, N. Complications of 278 consecutive abdominoplasties. J. Plast. Reconstr. Aesthetic Surg. 2006, 59, 1152–1155. [Google Scholar] [CrossRef] [PubMed]
- Neaman, K.C.; Armstrong, S.D.; Baca, M.E.; Albert, M.; Vander Woude, D.L.; Renucci, J.D. Outcomes of traditional cosmetic abdominoplasty in a community setting: A retrospective analysis of 1008 patients. Plast. Reconstr. Surg. 2013, 131, 403e–410e. [Google Scholar] [CrossRef]
- Shander, A. Financial and clinical outcomes associated with surgical bleeding complications. Surgery 2007, 142, S20–S25. [Google Scholar] [CrossRef] [PubMed]
- Chauncey, J.M.; Wieters, J.S. Tranexamic Acid; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Shakur, H.; Roberts, I. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant hemorrhage (CRASH-2): A randomized, placebo-controlled trial. In 50 Landmark Papers Every Trauma Surgeon Should Know; CRC Press: Boca Raton, FL, USA, 2019; pp. 31–34. [Google Scholar]
- Shakur, H.; Roberts, I.; Fawole, B.; Chaudhri, R.; El-Sheikh, M.; Akintan, A.; Qureshi, Z.; Kidanto, H.; Vwalika, B.; Abdulkadir, A. Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with post-partum haemorrhage (WOMAN): An international, randomised, double-blind, placebo-controlled trial. Lancet 2017, 389, 2105–2116. [Google Scholar] [CrossRef]
- Álvarez, J.C.; Santiveri, F.X.; Ramos, I.; Vela, E.; Puig, L.; Escolano, F. Tranexamic acid reduces blood transfusion in total knee arthroplasty even when a blood conservation program is applied. Transfusion 2008, 48, 519–525. [Google Scholar] [CrossRef]
- Colomina, M.J.; Contreras, L.; Guilabert, P.; Koo, M.; Sabate, A. Clinical use of tranexamic acid: Evidences and controversies. Braz. J. Anesthesiol. 2022, 72, 795–812. [Google Scholar] [CrossRef]
- Zucal, I.; De Pellegrin, L.; Pagnamenta, A.; Schmauss, D.; Brucato, D.; De Monti, M.; Schweizer, R.; Harder, Y.; Parodi, C. Topical Application of Tranexamic Acid in Abdominoplasties Leads to Lower Drainage Volume and Earlier Drain Removal. Plast. Reconstr. Surg.–Glob. Open 2025, 13, e6799. [Google Scholar] [CrossRef] [PubMed]
- Zaussinger, M.; Kerschbaumer, C.; Schwartz, B.; Bachleitner, K.; Ehebruster, G.; Schmidt, M. Influence of tranexamic acid in body contouring surgery: Significant changes on complication rates after abdominoplasty. Aesthetic Plast. Surg. 2024, 48, 2872–2878. [Google Scholar] [CrossRef]
- Guggenheim, L.; Magni, S.; Catic, A.; Pagnamenta, A.; Harder, Y.; Schmauss, D. The Effects of Systemic Tranexamic Acid Administration on Drainage Volume, Duration of Drain Placement, and Length of Hospital Stay in Skin-and Nipple-Sparing Mastectomies with Immediate Expander-Based Breast Reconstruction. J. Clin. Med. 2024, 13, 6507. [Google Scholar] [CrossRef]
- Wachtel, C.; Rothenberger, J.; Ederer, I.A.; Souquet, J.; Rieger, U. Systemic tranexamic acid for reduced postoperative blood loss and less bleeding complications in fleur-de-lis abdominoplasty and apronectomy. Aesthetic Plast. Surg. 2024, 48, 2465–2474. [Google Scholar] [CrossRef]
- Magni, S.; Guggenheim, L.; Fournier, G.; Parodi, C.; Pagnamenta, A.; Schmauss, D.; Harder, Y. The Effects of Systemic Tranexamic Acid Administration on Drainage Volume, Length of Hospital Stay, and Postoperative Complications in Reduction Mammaplasty. J. Clin. Med. 2024, 14, 151. [Google Scholar] [CrossRef]
- Clavien, P.A.; Barkun, J.; De Oliveira, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; De Santibañes, E.; Pekolj, J.; Slankamenac, K.; Bassi, C. The Clavien-Dindo classification of surgical complications: Five-year experience. Ann. Surg. 2009, 250, 187–196. [Google Scholar] [CrossRef]
- Dindo, D. The Clavien–Dindo classification of surgical complications. In Treatment of Postoperative Complications After Digestive Surgery; Springer: Berlin/Heidelberg, Germany, 2013; pp. 13–17. [Google Scholar]
- Patel, P.A.; Wyrobek, J.A.; Butwick, A.J.; Pivalizza, E.G.; Hare, G.M.; Mazer, C.D.; Goobie, S.M. Update on applications and limitations of perioperative tranexamic acid. Anesth. Analg. 2022, 135, 460–473. [Google Scholar] [CrossRef]
- Brown, S.; Brown, T.; Rohrich, R.J. Clinical applications of tranexamic acid in plastic and reconstructive surgery. Plast. Reconstr. Surg. 2024, 154, 1253e–1263e. [Google Scholar] [CrossRef]
- Fillingham, Y.A.; Ramkumar, D.B.; Jevsevar, D.S.; Yates, A.J.; Bini, S.A.; Clarke, H.D.; Schemitsch, E.; Johnson, R.L.; Memtsoudis, S.G.; Sayeed, S.A. Tranexamic acid use in total joint arthroplasty: The clinical practice guidelines endorsed by the American association of hip and knee surgeons, American society of regional anesthesia and pain medicine, American academy of orthopaedic surgeons, hip society, and knee society. J. Arthroplast. 2018, 33, 3065–3069. [Google Scholar] [CrossRef]
- Tibi, P.; McClure, R.S.; Huang, J.; Baker, R.A.; Fitzgerald, D.; Mazer, C.D.; Stone, M.; Chu, D.; Stammers, A.H.; Dickinson, T. STS/SCA/AmSECT/SABM update to the clinical practice guidelines on patient blood management. J. Extracorpor. Technol. 2021, 53, 97–124. [Google Scholar] [CrossRef]
- Scarafoni, E.E. A systematic review of tranexamic acid in plastic surgery: What’s new? Plast. Reconstr. Surg. Glob. Open 2021, 9, e3172. [Google Scholar] [CrossRef] [PubMed]
- Yao, A.; Wang, F.; Benacquista, T.; Draper, L.B.; Garfein, E.S.; Monaco, C.; Tepper, O.M.; Weichman, K.E.; Ricci, J.A. Topical tranexamic acid does not reduce hematoma in reduction mammaplasty: A double-blind randomized controlled trial. Plast. Reconstr. Surg. 2024, 154, 30–37. [Google Scholar] [CrossRef]
- Alves, M.; Mendes, M.; Valença-Filipe, R.; Rebelo, M.; Peres, H.; Costa-Ferreira, A. Long drainers after abdominoplasty: A risk analysis. Aesthetic Plast. Surg. 2025, 49, 2525–2533. [Google Scholar] [CrossRef] [PubMed]
- Shermak, M.A.; Rotellini-Coltvet, L.A.; Chang, D. Seroma development following body contouring surgery for massive weight loss: Patient risk factors and treatment strategies. Plast. Reconstr. Surg. 2008, 122, 280–288. [Google Scholar] [CrossRef] [PubMed]
- D’Ettorre, M.; Gniuli, D.; Bracaglia, R.; Tambasco, D.; Mingrone, G.; Gentileschi, S.; Massi, G. Micro-and macroscopic structural modification of subcutaneous adipose tissue after bariatric surgery. Aesthetic Plast. Surg. 2012, 36, 213–214. [Google Scholar] [CrossRef] [PubMed]
- De Paep, K.; Van Campenhout, I.; Van Cauwenberge, S.; Dillemans, B. Post-bariatric abdominoplasty: Identification of risk factors for complications. Obes. Surg. 2021, 31, 3203–3209. [Google Scholar] [CrossRef] [PubMed]
- Fijany, A.J.; Holan, C.A.; Troia, T.; Montorfano, L.; Mubang, R.N.; Givechian, K.B.; Karagoz, H.; Martinez-Jorge, J.; Perdikis, G.; Connor, L.M. Tranexamic Acid in Body Contouring Surgery: A Systematic Review and Meta-Analysis. Aesthetic Surg. J. 2025, 45, 1026–1034. [Google Scholar] [CrossRef]
- Ker, K.; Edwards, P.; Perel, P.; Shakur, H.; Roberts, I. Effect of tranexamic acid on surgical bleeding: Systematic review and cumulative meta-analysis. BMJ 2012, 344, e3054. [Google Scholar] [CrossRef]
- Swedenhammar, E.; Stark, B.; Hållstrand, A.H.; Ehrström, M.; Gahm, J. Surgical training and standardised management guidelines improved the 30-day complication rate after abdominoplasty for massive weight loss. World J. Surg. 2018, 42, 1647–1654. [Google Scholar] [CrossRef]
- Di Martino, M.; Nahas, F.X.; Kimura, A.K.; Sallum, N.; Ferreira, L.M. Natural evolution of seroma in abdominoplasty. Plast. Reconstr. Surg. 2015, 135, 691e–698e. [Google Scholar] [CrossRef]
- Rao, G.; Daneshi, K.; Ceccaroni, A.; Gentile, A.; El-Shazali, H.; Owens, N.; Vyas, K.; Khajuria, A. A Systematic Review and Meta-Analysis Evaluating the Surgical Outcomes of Progressive Tension Suturing Compared to Drains in Abdominoplasty Surgery. Aesthetic Surg. J. 2025, 45, 71–83. [Google Scholar] [CrossRef]

| Total | TXA | Non-TXA | p-Value | |
|---|---|---|---|---|
| Number of patients | 58 | 24 | 34 | - |
| Age at the time of surgery (in years) | 46.66 (±11.82) [27|77] | 44.96 (±10.58) [32|70] | 47.85 (±12.64) [27|77] | 0.363 |
| Body mass index (kg/m2) | 27.43 (±4.63) | 26.37 (±4.32) | 28.18 (±4.75) | 0.145 |
| [17.1|35.2] | [19.7|35] | [17.1|35.2] | ||
Gender
| 0.726 | |||
| 10 (17.2%) | 5 (20.8%) | 5 (14.7%) | ||
| 48 (82.8%) | 19 (79.2%) | 29 (85.3%) | ||
| Diabetes | 10 (17.2%) | 3 (12.5%) | 7 (20.6%) | 0.499 |
| Number of smokers | 11 (19.0%) | 4 (16.7%) | 7 (20.6%) | 1.000 |
| Anticoagulation | 4 (6.9%) | 0 | 4 (11.8%) | 0.134 |
| History of thromboembolism | 3 (5.2%) | 0 | 3 (8.8%) | 0.260 |
| Total | TXA | No-TXA | p-Value | |
|---|---|---|---|---|
| Number of patients | 58 | 24 | 34 | - |
Indication
| 0.041 | |||
| 40 (69.0%) | 13 (54.2%) | 27 (79.4%) | ||
| 18 (31.0%) | 11 (45.8%) | 7 (20.6%) | ||
Technique
| 0.984 | |||
| 41 (70.7%) | 17 (70.8%) | 24 (70.6%) | ||
| 17 (29.3%) | 7 (29.2%) | 10 (29.4%) | ||
| Additional liposuction in the abdominal region | 17 (29.3%) | 5 (20.8%) | 12 (35.3%) | 0.260 |
| Combined procedures | 12 (20.7%) | 6 (25.0%) | 6 (17.6%) | 0.496 |
| Rectus diastasis repair | 24 (41.4%) | 15 (62.5%) | 9 (26.5%) | 0.006 |
| Weight of resection (grams) | 2123 (±1676) | 1713 (±1846) | 2438 (±1676) | 0.024 |
| Time of incision to suture abdominoplasty only (hh:mm) | (n = 46) | (n = 18) | (n = 28) | 0.338 |
| 3:19 (±0:42) | 3:11 (±0:40) | 3:24 (±0:43) | ||
| [2:01|4:43] | [2:23|4:24] | [2:01|4:43} | ||
| Time of incision to suture combined procedures (hh:mm) | (n = 12) 5:42 (±1:20) [3:46|8:40] | (n = 6) 5:55 (±0:55) [4:44|7:30] | (n = 6) 5:30 (±1:43) [3:46|7:30] | 0.512 |
| Total | TXA | No-TXA | p-Value | |
|---|---|---|---|---|
| Number of patients | 58 | 24 | 34 | - |
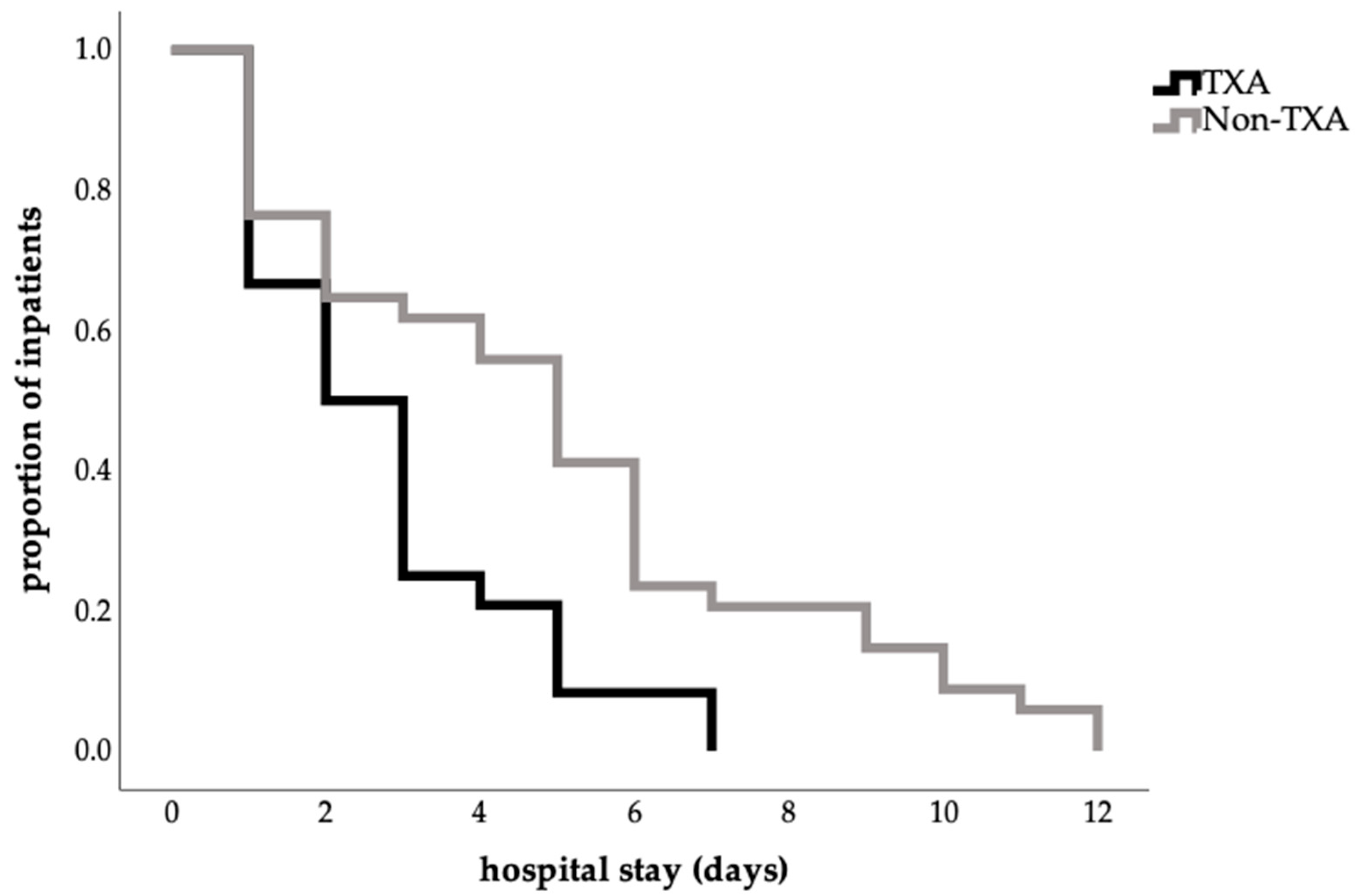
| Length of hospital stay (days) | 4.1 (±3.01) | 2.79 (±1.86) | 4.94 (±3.08) | 0.008 |
| [1|12] | [1|7] | [1|12] | ||
| Time to first drain removal (days) | (n = 53) | (n = 21) | (n = 32) | 0.729 |
| 2.17 (±1.28) | 2.00 (±0.95) | 2.17 (±1.28) | ||
| [1|7] | [1|5] | [1|7] | ||
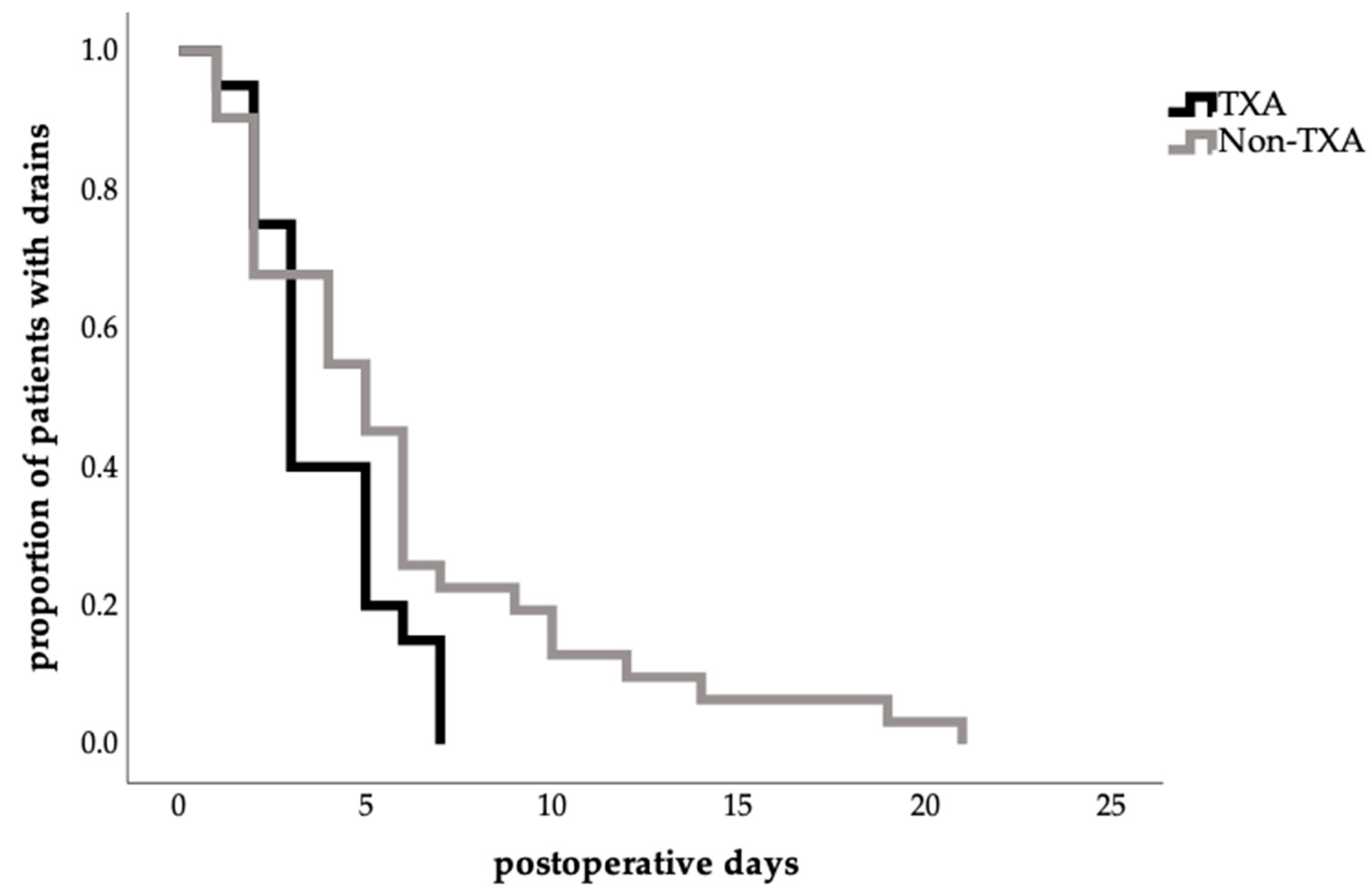
| Time to total drain removal (days) | (n = 51) | (n = 20) | (n = 31) | 0.243 |
| 5.16 (±4.16) | 3.85 (±1.87) | 6.00 (±4.97) | ||
| [1|21] | [1|7] | [1|21] | ||
| Drainage volume in total (mL) | (n = 47) | (n = 17) | (n = 30) | 0.352 |
| 497 (±606) | 292 (±255) | 614 (±712) | ||
| [20|2510] | [40|1060] | [20|2510] |
| Total | TXA | No-TXA | p-Value | |
|---|---|---|---|---|
| Number of patients | 58 | 24 | 34 | - |
| With | ||||
| 24 (41.4%) | 6 (25.0%) | 18 (52.9%) | 0.033 |
| 14 (24.1%) | 4 (16.7%) | 10 (29.4%) | 0.356 |
| 10 (17.2%) | 2 (8.3%) | 8 (23.5%) | 0.171 |
| Seroma formation | 14 (24.1%) | 4 (17.4%) | 10 (29.4%) | 0.361 |
| Wound healing disorder | 13 (22.4%) | 3 (12.5%) | 10 (29.4%) | 0.202 |
| Transfusion of packed red blood cells | 3 (5%) | 1 (4%) | 2 (6%) | 1.000 |
| Total | TXA | No-TXA | p-Value | |
|---|---|---|---|---|
| Number of patients | 54 | 21 | 33 | - |
| Decrease in hematocrit (hct) | 8.20% (±3.39) | 7.66% (±3.20) | 8.55% (±3.52) | 0.353 |
| [2.4|18.1] | [2.4|13.2] | [2.7|18.1] | ||
| Decrease in hemoglobin (hb) | 2.69% (±1.09) | 2.47% (±1.08) | 2.82% (±1.09) | 0.255 |
| [0.6|6.1] | [0.6|4.5] | [1.1|6.6} |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sahinovic, L.; Kohne, M.L.; Jiang, J.; Machens, H.-G.; Kükrek, H.; Dornseifer, U.; Schmauss, D.; Moog, P. Systemic Administration of Tranexamic Acid Improves Postoperative Outcome in Abdominoplasty. J. Clin. Med. 2025, 14, 7556. https://doi.org/10.3390/jcm14217556
Sahinovic L, Kohne ML, Jiang J, Machens H-G, Kükrek H, Dornseifer U, Schmauss D, Moog P. Systemic Administration of Tranexamic Acid Improves Postoperative Outcome in Abdominoplasty. Journal of Clinical Medicine. 2025; 14(21):7556. https://doi.org/10.3390/jcm14217556
Chicago/Turabian StyleSahinovic, Leila, Marie Louise Kohne, Jun Jiang, Hans-Guenther Machens, Haydar Kükrek, Ulf Dornseifer, Daniel Schmauss, and Philipp Moog. 2025. "Systemic Administration of Tranexamic Acid Improves Postoperative Outcome in Abdominoplasty" Journal of Clinical Medicine 14, no. 21: 7556. https://doi.org/10.3390/jcm14217556
APA StyleSahinovic, L., Kohne, M. L., Jiang, J., Machens, H.-G., Kükrek, H., Dornseifer, U., Schmauss, D., & Moog, P. (2025). Systemic Administration of Tranexamic Acid Improves Postoperative Outcome in Abdominoplasty. Journal of Clinical Medicine, 14(21), 7556. https://doi.org/10.3390/jcm14217556







