Short-Term Cardiovascular Compensatory Responses to Varying Levels of Orthostatic Stress During Active Standing in Older Adults
Abstract
1. Introduction
2. Materials and Methods
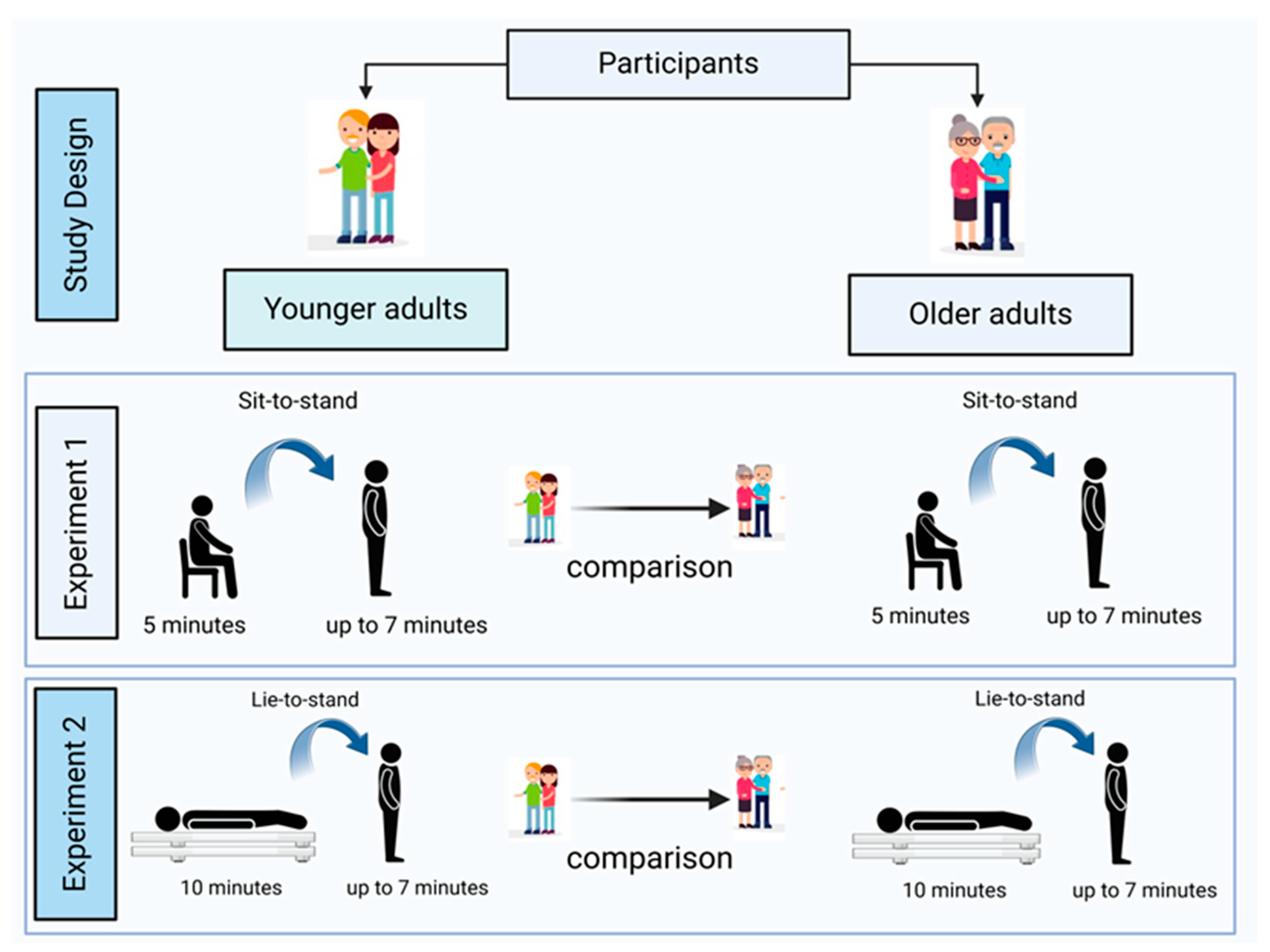
2.1. Study Design
2.2. Settings
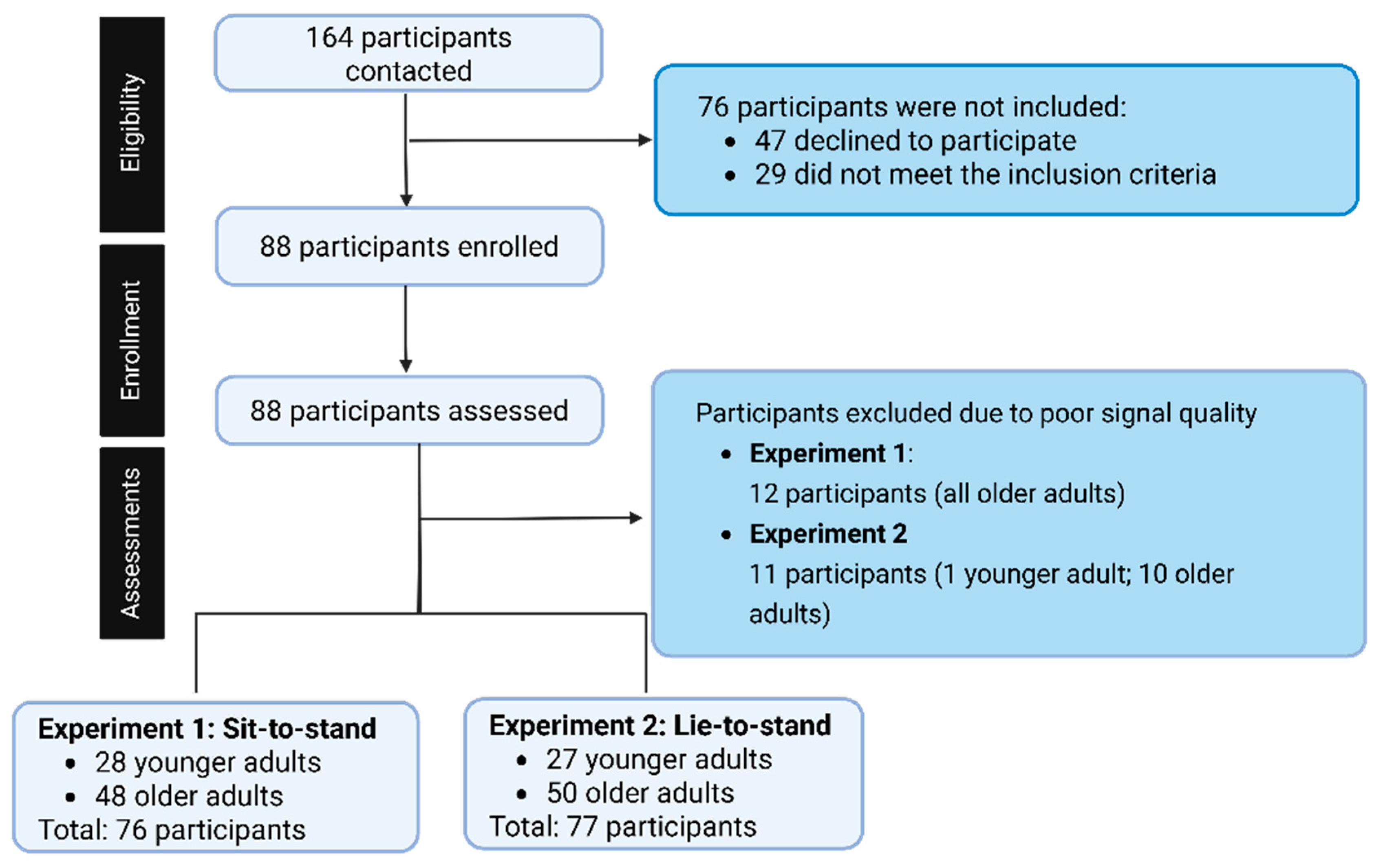
2.3. Participants
2.4. Data Collection
2.5. Demographic and Anthropometric Measurements
2.6. Assessment of Cardiovascular Responses
2.7. Sample Size
2.8. Data Analysis
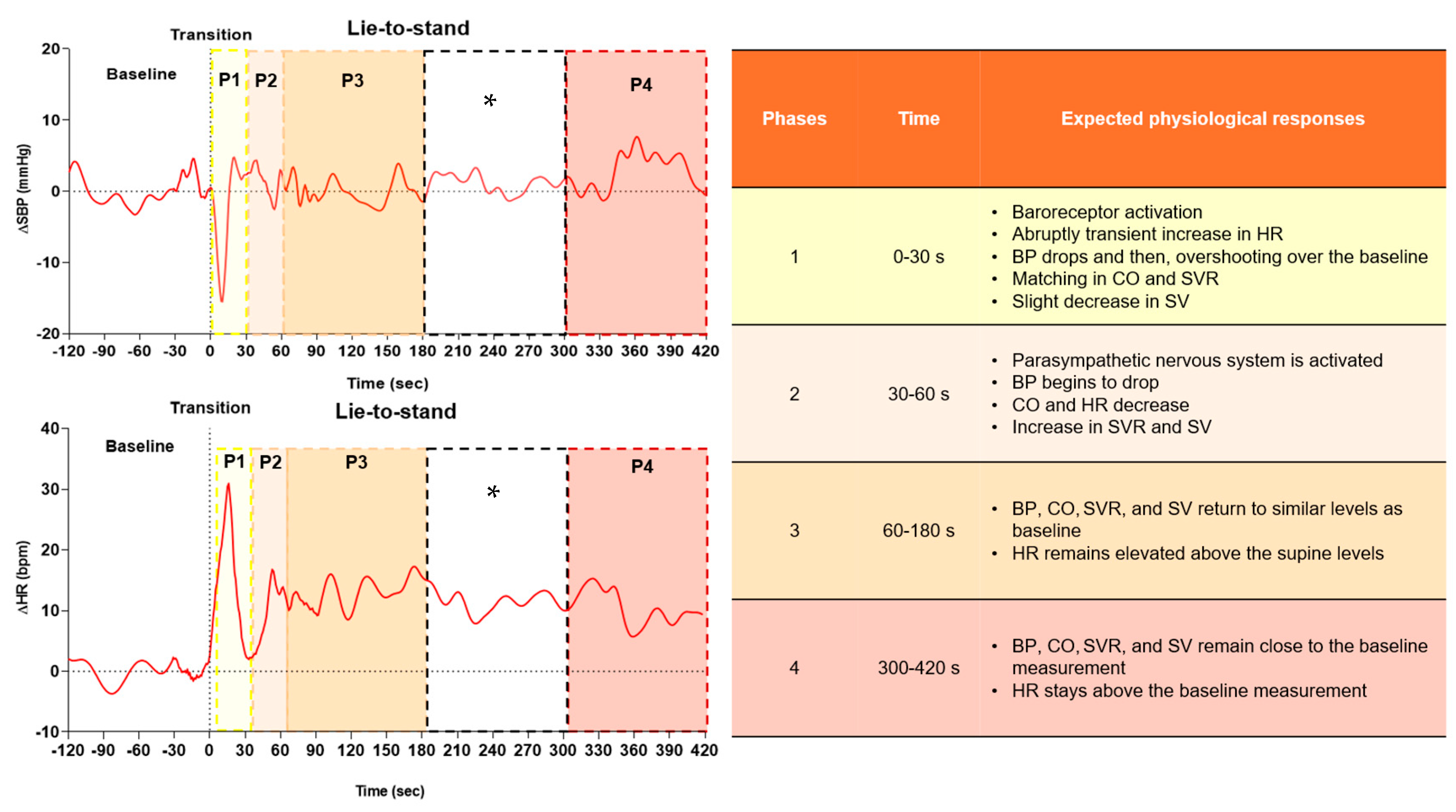
2.9. Variables Extracted and Analyzed During Active Standing
2.10. Statistical Analysis
3. Results
3.1. Sit to Stand Responses
3.2. Lie to Stand Responses
4. Discussion
4.1. Immediate Cardiovascular Responses to Active Standing
4.2. Short-Term Cardiovascular Compensatory Responses Across Phases During Active Standing Orthostatic Stress
4.3. Cardiac Output and Systemic Vascular Resistance Matching Responses During Active Standing Orthostatic Stress
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ACE | Angiotensin-Converting Enzyme |
| ARB | Angiotensin Receptor Blocker |
| BMI | Body Mass Index |
| BP | Blood Pressure |
| CI | Confidence Interval |
| CO | Cardiac Output |
| CO-SVR | Cardiac Output–Systemic Vascular Resistance Matching |
| CSEP | Canadian Society for Exercise Physiology |
| DBP | Diastolic Blood Pressure |
| ECG | Electrocardiogram |
| FDR | False Discovery Rate |
| HR | Heart Rate |
| IQR | Interquartile Range |
| MAP | Mean Arterial Pressure |
| OA | Older Adults |
| OH | Orthostatic Hypotension |
| OI | Orthostatic Intolerance |
| SBP | Systolic Blood Pressure |
| SD | Standard Deviation |
| STROBE | Strengthening the Reporting of Observational Studies in Epidemiology |
| SV | Stroke Volume |
| SVR | Systemic Vascular Resistance |
| YA | Younger Adults |
References
- de Matos, D.G.; de Santana, J.L.; Aidar, F.J.; Cornish, S.M.; Giesbrecht, G.G.; Mendelson, A.A.; Duhamel, T.A.; Villar, R. Cardiovascular Regulation during Active Standing Orthostatic Stress in Older Adults Living with Frailty: A Systematic Review. Arch. Gerontol. Geriatr. 2025, 136, 105894. [Google Scholar] [CrossRef]
- de Matos, D.G.; de Santana, J.L.; Mendelson, A.A.; Duhamel, T.A.; Villar, R. Integrated Dynamic Autonomic and Cardiovascular Regulation during Postural Transitions in Older Adults Living with Frailty: A Systematic Review Protocol. Int. J. Environ. Res. Public Health 2023, 20, 566. [Google Scholar] [CrossRef]
- van Wijnen, V.K.; Ten Hove, D.; Finucane, C.; Wieling, W.; van Roon, A.M.; Ter Maaten, J.C.; Harms, M.P.M. Hemodynamic Mechanisms Underlying Initial Orthostatic Hypotension, Delayed Recovery and Orthostatic Hypotension. J. Am. Med. Dir. Assoc. 2018, 19, 786–792. [Google Scholar] [CrossRef]
- Dani, M.; Dirksen, A.; Taraborrelli, P.; Panagopolous, D.; Torocastro, M.; Sutton, R.; Lim, P.B. Orthostatic Hypotension in Older People: Considerations, Diagnosis and Management. Clin. Med. J. R. Coll. Physicians Lond. 2021, 21, E275–E282. [Google Scholar] [CrossRef] [PubMed]
- van Twist, D.J.L.; Mostard, G.J.M.; Sipers, W.M.W.H. Delayed Recovery from Initial Orthostatic Hypotension: An Expression of Frailty in the Elderly. Clin. Auton. Res. 2020, 30, 105–106. [Google Scholar] [CrossRef] [PubMed]
- Christopoulos, E.M.; Tran, J.; Hillebrand, S.L.; Lange, P.W.; Iseli, R.K.; Meskers, C.G.M.M.; Maier, A.B. Initial Orthostatic Hypotension and Orthostatic Intolerance Symptom Prevalence in Older Adults: A Systematic Review. Int. J. Cardiol. Hypertens. 2021, 8, 100071. [Google Scholar] [CrossRef] [PubMed]
- Wehrwein, E.A.; Joyner, M.J. Regulation of Blood Pressure by the Arterial Baroreflex and Autonomic Nervous System. Handb. Clin. Neurol. 2013, 117, 89–102. [Google Scholar] [CrossRef]
- Ricci, F.; De Caterina, R.; Fedorowski, A. Orthostatic Hypotension: Epidemiology, Prognosis, and Treatment. J. Am. Coll. Cardiol. 2015, 66, 848–860. [Google Scholar] [CrossRef]
- Fedorowski, A.; Ricci, F.; Hamrefors, V.; Sandau, K.E.; Hwan Chung, T.; Muldowney, J.A.S.; Gopinathannair, R.; Olshansky, B. Orthostatic Hypotension: Management of a Complex, But Common, Medical Problem. Circ. Arrhythmia Electrophysiol. 2022, 15, E010573. [Google Scholar] [CrossRef]
- Finucane, C.; O’Connell, M.D.L.; Fan, C.W.; Savva, G.M.; Soraghan, C.J.; Nolan, H.; Cronin, H.; Kenny, R.A. Age-Related Normative Changes in Phasic Orthostatic Blood Pressure in a Large Population Study: Findings from the Irish Longitudinal Study on Ageing (TILDA). Circulation 2014, 130, 1780–1789. [Google Scholar] [CrossRef]
- Vargas, E. Physiological Responses To Postural Change Young And Old Healthy Individuals In The Sydrome of Postural Hypotension Increases in Incidence with Increasing Age so That up to 20070 of Old People Suffer from the Syndrome. Exp. Gerontol. 1983, 17, 445–451. [Google Scholar] [CrossRef]
- Wieling, W.; Veerman, D.P.; Dambrink, J.H.A.; Imholz, B.P.M. Disparities in Circulatory Adjustment to Standing between Young and Elderly Subjects Explained by Pulse Contour Analysis. Clin. Sci. 1992, 83, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Kawaguchi, T.; Uyama, O.; Konishi, M.; Nishiyama, T.; Iida, T. Orthostatic Hypotension in Elderly Persons during Passive Standing: A Comparison with Young Persons. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.J.; Hughes, C.V.; Ptacin, M.J.; Barney, J.A.; Tristani, F.E.; Ebert, T.J. The Effect of Age on Hemodynamic Response to Graded Postural Stress in Normal Men. J. Gerontol. 1987, 42, 406–411. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.A.; Fasler, J.J. Age-Related Changes in Autonomic Function: Relationship with Postural Hypotension. Age Ageing 1983, 12, 206–210. [Google Scholar] [CrossRef]
- Wieling, W.; van Twist, D.J.L.; van Wijnen, V.K.; Harms, M.P.M. Spectrum of Hemodynamic Responses in the First 60 Seconds after Active Standing Up: Importance of Time Course of Blood Pressure Changes and Definitions. J. Am. Med. Dir. Assoc. 2021, 22, 2401–2403. [Google Scholar] [CrossRef]
- Finucane, C.; O’Connell, M.D.L.; Donoghue, O.; Richardson, K.; Savva, G.M.; Kenny, R.A. Impaired Orthostatic Blood Pressure Recovery Is Associated with Unexplained and Injurious Falls. J. Am. Geriatr. Soc. 2017, 65, 474–482. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef]
- Canadian Society for Exercise Physiology. Canadian Physical Activity Guidelines for Older Adults 65 Years and Older; CSEP, Ed.; Canadian Society for Exercise Physiology: Ottawa, ON, Canada, 2011. [Google Scholar]
- Guelen, I.; Westerhof, B.E.; Van Der Sar, G.L.; Van Montfrans, G.A.; Kiemeneij, F.; Wesseling, K.H.; Bos, W.J.W. Finometer, Finger Pressure Measurements with the Possibility to Reconstruct Brachial Pressure. Blood Press. Monit. 2003, 8, 27–30. [Google Scholar] [CrossRef]
- Finapres Medical Systems. FinometerTM User’s Guide; Finapres Medical System BV: Amsterdam, The Netherlands, 2005. [Google Scholar]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A Flexible Statistical Power Analysis Program for the Social, Behavioral, and Biomedical Sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Van Der Velde, N.; Van Den Meiracker, A.H.; Stricker, B.H.C.; Van Der Cammen, T.J.M. Measuring Orthostatic Hypotension with the Finometer Device: Is a Blood Pressure Drop of One Heartbeat Clinically Relevant? Blood Press. Monit. 2007, 12, 167–171. [Google Scholar] [CrossRef] [PubMed]
- Mol, A.; Slangen, L.R.N.; Trappenburg, M.C.; Reijnierse, E.M.; van Wezel, R.J.A.; Meskers, C.G.M.; Maier, A.B. Blood Pressure Drop Rate after Standing up Is Associated with Frailty and Number of Falls in Geriatric Outpatients. J. Am. Heart Assoc. 2020, 9, 7. [Google Scholar] [CrossRef] [PubMed]
- Romero-Ortuno, R.; Cogan, L.; Fan, C.W.; Kenny, R.A. Intolerance to Initial Orthostasis Relates to Systolic BP Changes in Elders. Clin. Auton. Res. 2010, 20, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Gibbons, C.H.; Freeman, R. Delayed Orthostatic Hypotension: A Frequent Cause of Orthostatic Intolerance. Neurology 2006, 67, 28–32. [Google Scholar] [CrossRef]
- Byun, J.I.; Moon, J.; Kim, D.Y.; Shin, H.; Sunwoo, J.S.; Lim, J.A.; Kim, T.J.; Lee, W.J.; Lee, H.S.; Jun, J.S.; et al. Delayed Orthostatic Hypotension: Severity of Clinical Symptoms and Response to Medical Treatment. Auton. Neurosci. Basic. Clin. 2018, 213, 81–85. [Google Scholar] [CrossRef]
- Yoav Benjamini and Yosef Hochberg. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J. R. Stat. Soc. Ser. B (Methodol.) 1995, 57, 289–300. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis. Curr. Dir. Psychol. Sci. 1992, 1, 98–101. [Google Scholar] [CrossRef]
- Kerby, D.S. The Simple Difference Formula: An Approach to Teaching Nonparametric Correlation. Compr. Psychol. 2014, 3, 11.IT.3.1. [Google Scholar] [CrossRef]
- Kim, Y.S.; Bogert, L.W.J.; Immink, R.V.; Harms, M.P.M.; Colier, W.N.J.M.; Van Lieshout, J.J. Effects of Aging on the Cerebrovascular Orthostatic Response. Neurobiol. Aging 2011, 32, 344–353. [Google Scholar] [CrossRef]
- Mohrman, D.L.H. Cardiovascular Physiology, 8th ed.; McGraw-Hill Education: New York, NY, USA, 2013; ISBN 0071793119. [Google Scholar]
- Ten Harkel, A.D.; Van Lieshout, J.J.; Van Lieshout, E.J.; Wieling, W. Assessment of Cardiovascular Reflexes: Influence of Posture and Period Preceding Rest. Eurorehab 1990, 68, 147–153. [Google Scholar] [CrossRef]
- Saeidifard, F.; Medina-Inojosa, J.R.; Supervia, M.; Olson, T.P.; Somers, V.K.; Prokop, L.J.; Stokin, G.B.; Lopez-Jimenez, F. The Effect of Replacing Sitting With Standing on Cardiovascular Risk Factors: A Systematic Review and Meta-Analysis. Mayo Clin. Proc. Innov. Qual. Outcomes 2020, 4, 611–626. [Google Scholar] [CrossRef]
- De Bruïne, E.S.; Reijnierse, E.M.; Trappenburg, M.C.; Pasma, J.H.; De Vries, O.J.; Meskers, C.G.M.; Maier, A.B. Standing Up Slowly Antagonises Initial Blood Pressure Decrease in Older Adults with Orthostatic Hypotension. Gerontology 2017, 63, 137–143. [Google Scholar] [CrossRef]
- O’Connor, J.D.; O’Connell, M.D.L.; Nolan, H.; Newman, L.; Knight, S.P.; Kenny, R.A. Impact of Standing Speed on the Peripheral and Central Hemodynamic Response to Orthostasis: Evidence from the Irish Longitudinal Study on Ageing. Hypertension 2020, 75, 524–531. [Google Scholar] [CrossRef]
- Wieling, W.; Karemaker, J.M. Measurement of Heart Rate and Blood Pressure to Evaluate Disturbances in Neurocardiovascular Control. Auton. Fail. 2013, 290–306. [Google Scholar] [CrossRef]
- Freeman, R.; Abuzinadah, A.R.; Gibbons, C.; Jones, P.; Miglis, M.G.; Sinn, D.I. Orthostatic Hypotension: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2018, 72, 1294–1309. [Google Scholar] [CrossRef] [PubMed]
- Stice, J.P.; Lee, J.S.; Pechenino, A.S.; Knowlton, A.A. Estrogen, Aging and the Cardiovascular System. Future Cardiol. 2009, 5, 93–103. [Google Scholar] [CrossRef] [PubMed]
- Fu, Q.; Vangundy, T.B.; Shibata, S.; Auchus, R.J.; Williams, G.H.; Levine, B.D. Menstrual Cycle Affects Renal-Adrenal and Hemodynamic Responses during Prolonged Standing in the Postural Orthostatic Tachycardia Syndrome. Hypertension 2010, 56, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Shankhwar, V.; Urvec, J.; Steuber, B.; Schmid Zalaudek, K.; Salon, A.; Hawliczek, A.; Bergauer, A.; Aljasmi, K.; Abdi, A.; Naser, A.; et al. Effects of Menstrual Cycle on Hemodynamic and Autonomic Responses to Central Hypovolemia. Front. Cardiovasc. Med. 2024, 11, 1–9. [Google Scholar] [CrossRef]
- Fu, Q.; Okazaki, K.; Shibata, S.; Shook, R.P.; Vangunday, T.B.; Galbreath, M.M.; Reelick, M.F.; Levine, B.D. Menstrual Cycle Effects on Sympathetic Neural Responses to Upright Tilt. J. Physiol. 2009, 587, 2019–2031. [Google Scholar] [CrossRef]
- Claydon, V.E.; Younis, N.R.; Hainsworth, R. Phase of the Menstrual Cycle Does Not Affect Orthostatic Tolerance in Healthy Women. Clin. Auton. Res. 2006, 16, 98–104. [Google Scholar] [CrossRef]
- Sachse, C.; Trozic, I.; Brix, B.; Roessler, A.; Goswami, N. Sex Differences in Cardiovascular Responses to Orthostatic Challenge in Healthy Older Persons: A Pilot Study. Physiol. Int. 2019, 106, 236–249. [Google Scholar] [CrossRef]


| Anthropometry | |||||||
|---|---|---|---|---|---|---|---|
| Younger Adults | Older Adults | ||||||
| Variable | Mean ± SD | CI 95% | Min; Max | Mean ± SD | CI 95% | Min; Max | p-Value |
| Age (years) | 21.0 ± 2.3 | 20.8; 22.6 | 18.0; 28.0 | 70.5 ± 3.9 ↑ | 69.3; 71.5 | 63.0; 78.0 | <0.001 * |
| Height (m) | 1.73 ± 0.07 | 1.69; 1.76 | 1.56; 1.86 | 1.64 ± 0.08 ↓ | 1.62; 1.66 | 1.46; 1.84 | <0.001 * |
| Body mass | 67.6 ± 11.9 | 62.9–72.2 | 42.6; 90.5 | 73.7 ± 15.4 | 69.4; 78.0 | 42.5; 110.0 | 0.07 |
| BMI (kg/m2) | 22.6 ± 3.38 | 21.3–23.9 | 16.5; 30.4 | 27.3 ± 5.6 ↑ | 25.8; 28.9 | 17.1; 48.4 | <0.001 * |
| Younger Adults | Older Adults | p-Value | |||||
| Hypertension | n | % | ---- | n | % | ---- | ---- |
| 0 | 0 | 20 | 40 | <0.001 * | |||
| Diabetes | n | % | ---- | n | % | ---- | |
| 0 | 0 | 2 | 4 | 0.53 | |||
| Medications | n | % | ---- | n | % | ---- | |
| Cardiovascular | 0 | 0 | ---- | 20 | 40 | ---- | <0.001 * |
| Psychotropic | 2 | 7 | --- | 7 | 14 | ---- | 0.47 |
| Variable | Group | Baseline | Amplitude | Phase 1 | Phase 2 | Phase 3 | Phase 4 |
|---|---|---|---|---|---|---|---|
| SBP (mmHg) | Younger adults | 111.6 ± 9.1 (108; 115) | −8.4|6.4 (2.6; 43.8) | 4.8|4.0 (−5.1; 22.0) | 2.6 ± 4.6 (0.8; 4.4) | 1.8|3.3 (−3.3; 20.0) | −1.0 ± 3.6 (−2.4; 0.4) |
| Older adults | 129.5 ± 12.9 ↑ (126; 133) | −20.4|11.0 ↑ (5.4; 41.0) | 2.7|9.7 (−15.7; 21.9) | 3.3 ± 1.1 (5.5; 7.6) | 2.1|7.8 ↑ (−15.0; 22.4) | 3.4 ± 2.2 ↑ (1.5; 5.3) | |
| Adj p | 0.003 * | 0.003 * | 0.23 | 0.6 | 0.003 * | 0.003 * | |
| ES | 1.5 | 1.1 | −0.3 | 0.1 | 0.76 | 0.8 | |
| DBP (mmHg) | Younger adults | 76|6 (54; 82) | −7.8|4.4 (3.4; 28.3) | 2.8|3.0 (−9.7; 8.2) | 1.5|2.7 (−8.5; 6.7) | 2.3|2.7 (−8.9; 11.4) | 1.1|2.2 (−12.0; 6.2) |
| Older adults | 80|10 ↑ (56; 92) | −13.0|6.7 ↑ (5.5; 27.7) | 0.6|3.8 (−11.8; 7.6) | 1.2|3.0 (−9.9; 10.9) | 3.3|37 (−9.3; 13.6) | 2.0|4.1 (−11.6; 11.3) | |
| Adj p | 0.029 * | 0.035 * | 0.23 | 0.30 | 0.11 | 0.2 | |
| ES | 0.3 | 0.5 | 0.3 | 0.1 | 0.11 | 0.2 | |
| MAP (mmHg) | Younger adults | 87 ± 5.05 (85.1; 89) | −7.7|4.4 (3.4; 28.3) | 2.1|3.6 (−6.3; 10.4) | 2.8|3.0 (−9.7; 8.2) | 2.4|2.7 (−8.2; 11.7) | −0.1|4.3 (−13.7; 3.9) |
| Older adults | 95.5 ± 8.52 ↑ (93.2; 97.9) | −13.3|6.7 ↑ (5.5; 27.7) | 1.3|4.3 (−12.0; 9.1) | 0.6|3.8 (−11.8; 7.8) | 3.3|3.7 ↑ (−9.3; 13.6) | 1.9|4.3 ↑ (−12.6; 10.6) | |
| Adj p | 0.002 * | 0.023 * | 0.11 | 0.9 | 0.012 * | 0.008 * | |
| ES | 1.1 | 0.7 | 0.2 | 0.01 | 0.36 | 0.4 | |
| SVR (mmHg·min−1·L−1) | Younger adults | 20.6|6.5 (13.8; 31.1) | −7.0|2.7 (2.7; 11.6) | 0.7 ± 1.8 ↑ (−0.0; 1.4) | 1.6 ± 1.7 (0.9; 2.3) | 1.7|2.1 (−1.8; 6.9) | 0.2|1.7 (−1.9; 3.3) |
| Older adults | 25.8|8.4 ↑ (18.2; 49.8) | −11.3|6.6 ↑ (5.3; 21.5) | −2.0 ± 3.3 (−2.9; −1.0) | −1.3 ± −2.1 ↓ (−0.5; 2.7) | 0.5|5.7 (−6.1; 11.4) | −0.4|5.4 (−7.9; 9.3) | |
| Adj p | 0.0017 * | 0.0017 * | 0.0017 * | 0.0017 * | 0.23 | 0.4 | |
| ES | 0.6 | 0.7 | −0.9 | −1.2 | 0.1 | 0.1 | |
| HR (bpm) | Younger adults | 71.9 ± 10.2 (68.0; 75.9) | 29.2 ± 5.3 (27.1; 31.3) | 29.2 ± 5.3 (27.1; 31.3) | 11.7 ± 8.3 (8.5; 15.0) | 18.0 ± 7.8 (15.0; 21.1) | 14.1 ± 5.5 (11.9; 16.3) |
| Older adults | 64.5 ± 61.8 ↓ (67.1; 9.0) | 12.3 ± 4.4 ↓ (11.0; 13.6) | 12.3 ± 4.4 ↓ (11.0; 13.6) | 7.0 ± 5.9 ↓ (8.1; 3.8) | 9.3 ± 3.9 ↓ (8.1; 10.5) | 7.5 ± 4.2 ↓ (6.2; 8.7) | |
| Adj p | 0.001 * | 0.001 * | 0.001 * | 0.001 * | 0.001 * | 0.001 * | |
| ES | −0.8 | −3.5 | −3.5 | −0.8 | −1.5 | −1.4 | |
| CO (L·min−1) | Younger adults | 5.4 ± 1.2 (5.0; 6.0) | 2.0|1.3 (0.7; 4.5) | 2.0|1.3 (0.7; 4.5) | 0.3 ± 0.4 (0.1; 0.6) | 0.4 ± 0.5 (0.2; 0.7) | −0.1 ± 0.4 (−0.2; 0.1) |
| Older adults | 3.5 ± 0.8 ↓ (3.3; 3.8) | 1.6|0.8 ↓ (0.5; 4.7) | 1.6|0.8 ↓ (0.5; 4.7) | 2.2 ± 0.9 (1.9; 2.6) | 0.5 ± 0.4 (0.4; 0.7) | 0.1 ± 0.4 ↑ (0.0; 0.3) | |
| Adj p | 0.035 * | 0.005 * | 0.005 * | 0.11 | 0.4 | 0.028 * | |
| ES | −1.9 | 0.4 | 0.4 | 0.4 | 0.2 | 0.5 | |
| SV (mL) | Younger adults | 77.3 ± 18.3 (70.2; 84.4) | 9.1 ± 7.8 (6.0; 12.2) | −3.7|9.2 (−30.8; 14.0) | −8.1 ± 7.1 (−10.9; −5.3) | −10.0|1.1 (8.6; −28.7) | −22.3|11.5 (−46.9; −7.5) |
| Older adults | 55.9 ± 14.4 ↓ (51.7; 60.1) | 13.6 ± 8.1 ↑ (11.2; 16.0) | 3.8|9.5 ↑ (−7.2; 53.1) | 0.1 ± 8.1 ↑ (−2.2; 2.5) | −3.9|7.4 ↑ (−25.8; 28.3) | −15.0|12.2 ↑ (−42.6; 30.0) | |
| Adj p | 0.0014 * | 0.02 * | 0.0014 * | 0.0014 * | 0.0014 * | 0.011 * | |
| ES | −1.3 | 0.6 | 0.5 | 1.0 | 0.6 | 0.35 |
| Variable | Group | Baseline | Amplitude | Phase 1 | Phase 2 | Phase 3 | Phase 4 |
|---|---|---|---|---|---|---|---|
| SBP (mmHg) | Younger adults | 111.6 ± 9.1 (108; 115) | −15.1 ± 6.6 (12.4; 17.7) | 5.9 ± 4.9 (4.0; 7.9) | 3.2|6.0 (−6.4; 9.7) | 2.5|4.1 (−2.2; 8.3) | −0.9|3.5 (−4.1; 4.2) |
| Older adults | 129.5 ± 12.9 ↑ (126; 133) | −31.7 ± 12.4 ↑ (28.1; 35.3) | −2.5 ± 10.7 ↓ (−15.7; 21.9) | −1.2|9.0 ↓ (−29.1; 21.4) | 2.6|8.0 (−23.2; 27.1) | −1.2|11.9 (−32.8; 19.9) | |
| Adj p | 0.003 * | 0.0035 * | 0.035 * | 0.007 * | 0.5 | 0.23 | |
| ES | 1.5 | 1.5 | −0.9 | 0.4 | 0.1 | 0.2 | |
| DBP (mmHg) | Younger adults | 76|6 (54; 82) | −11.2|4.0 (2.5; 17.9) | 4.0|3.8 (−2.6; 14.0) | 3.0|3.1 (−2.4; 10.6) | 4.3|2.8 (0.6; 14.0) | 2.4|2.0 (−0.3; 10.3) |
| Older adults | 80|10 ↑ (56; 92) | −19.5|5.9 ↑ (0.0; 34.6) | 0.1|7.0 ↓ (−9.8; 21.7) | 1.2|5.8 ↓ (−10.0; 27.1) | 2.5|6.6 (−7.6; 32.5) | 2.8|6.0 (−8.2; 28.3) | |
| Adj p | 0.029 * | 0.0017 * | 0.0017 * | 0.004 * | 0.46 | 0.9 | |
| ES | 0.3 | 0.8 | 0.6 | 0.4 | 0.1 | 0.01 | |
| MAP (mmHg) | Younger adults | 87 ± 5.05 (85.1; 89) | −10.7 ± 5.5 (9.2; 12.1) | 4.2 ± 3.2 (3.0; 5.5) | 3.0|3.1 (−2.4; 10.6) | 4.4|2.8 (0.6; 4.0) | 1.7|8.6 (−14.5; 21.9) |
| Older adults | 95.5 ± 8.52 ↑ (93.2; 97.9) | −19.8 ± 6.9 ↑ (17.8; 21.8) | 0.5 ± 3.9 ↓ (−0.6; 1.6) | −1.6|7.3 ↓ (−16.8; 20.9) | 2.6|6.6 (−7.6; 32.5) | 2.2|8.6 (−14.5; 21.9) | |
| Adj p | 0.002 * | 0.0014 * | 0.0014 * | 0.0014 * | 0.58 | 0.90 | |
| ES | 1.1 | 1.8 | −1.1 | 0.5 | 0.1 | 0.01 | |
| SVR (mmHg·min−1·L−1) | Younger adults | 19.4 ± 3.6 (18.0; 20.9) | −6.4|3.2 (3.1; 2.3) | 2.4|4.9 (−2.7; 11.0) | 3.6|4.8 (−2.0; 10.0) | 4.4|3.9 (−2.3; 10.0) | 1.7|3.7 (−4.3; 7.2) |
| Older adults | 27.8 ± 7.0 ↑ (25.8; 29.8) | −12.5|5.2 ↑ (4.9; 25.3) | −1.7|4.1 ↓ (−13.1; 19.5) | −0.8|4.1 ↓ (−11.9; 24.9) | 2.7|6.4 (−11.1; 40.8) | 0.2|6.8 (−13.3; 40.5) | |
| Adj p | 0.0017 * | 0.0017 * | 0.0017 * | 0.0017 * | 0.14 | 0.7 | |
| ES | 1.4 | 0.9 | 0.6 | 0.5 | 0.2 | 0.03 | |
| HR (bpm) | Younger adults | 66.4 ± 9.8 (62.5; 70.2) | 35.4|8.1 ↑ (25.8; 53.7) | 35.4|8.1 (25.8; 53.7) | 16.7|12.5 (−1.9; 47.8) | 21.7|12.0 (11.5; 44.7) | 18.8|9.0 (3.8; 35.5) |
| Older adults | 62.6 ± 8.8 (60.0; 65.1) | 16.2|5.8 (5.6; 40.4) | 16.2|5.8 ↓ (5.6; 40.4) | 10.9|6.8 ↓ (0.4; 41.3) | 13.5|8.2 ↓ (4.5; 42.8) | 9.1|7.1 ↓ (1.8; 32.1) | |
| Adj p | 0.08 | 0.0014 * | 0.0014 * | 0.0081 * | 0.0014 * | 0.0014 * | |
| ES | −0.4 | 0.9 | 0.9 | 0.4 | 0.7 | 0.7 | |
| CO (L·min−1) | Younger adults | 5.5|1.3 ↑ (3.9; 9.0) | 1.7|1.0 (0.7; 5.4) | 1.7|1.0 (0.7; 5.3) | 0.1 ± 0.8 (−0.2; 0.4) | 0.1 ± 0.6 (−0.0; 0.4) | −0.2|0.8 (−1.5; 1.3) |
| Older adults | 3.4|1.0 (2.2; 5.6) | 1.7|1.5 (0.3; 6.0) | 1.7|1.5 (0.3; 6.0) | 0.4 ± 0.6 (0.2; 0.6) | 0.5 ± 0.5 (0.4; 0.7) | −0.0|0.7 (−2.7; 1.0) | |
| Adj p | 0.035 * | 0.4 | 0.4 | 0.17 | 0.17 | 0.28 | |
| ES | 0.8 | 0.1 | 0.1 | 0.4 | 0.3 | 0.1 | |
| SV (mL) | Younger adults | 85.3|22.9 ↑ (61.8; 122.2) | −0.1|16.7 (−27.7; 21.6) | −16.8|11.2 (−37.9; 3.1) | −19.6 ± 8.5 (−23.0; −16.3) | −23.1 ± 8.5 (−26.5; −19.7) | −19.4|16.4 (−42.6; −0.3) |
| Older adults | 55.7|14.9 (35.4; 93.1) | 10.5|10.7 ↑ (−5.4; 49.7) | 3.9|11.0 ↑ (−18.0; 33.8) | −5.5 ± 7.9 ↑ (−7.8; −3.2) | −8.4 ± 7.1 ↑ (−10.8; −6.0) | −17.5|24.4 (−55.7; 3.7) | |
| Adj p | 0.0011 * | 0.0011 * | 0.0011 * | 0.0011 * | 0.0011 * | 0.8 | |
| ES | 0.8 | 0.5 | 0.85 | 1.7 | 1.7 | 0.03 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Matos, D.G.; de Santana, J.L.; Aidar, F.J.; Cornish, S.M.; Giesbrecht, G.G.; Nunes-Silva, A.; Raj, S.R.; Romero-Ortuno, R.; Duhamel, T.A.; Villar, R. Short-Term Cardiovascular Compensatory Responses to Varying Levels of Orthostatic Stress During Active Standing in Older Adults. J. Clin. Med. 2025, 14, 7202. https://doi.org/10.3390/jcm14207202
de Matos DG, de Santana JL, Aidar FJ, Cornish SM, Giesbrecht GG, Nunes-Silva A, Raj SR, Romero-Ortuno R, Duhamel TA, Villar R. Short-Term Cardiovascular Compensatory Responses to Varying Levels of Orthostatic Stress During Active Standing in Older Adults. Journal of Clinical Medicine. 2025; 14(20):7202. https://doi.org/10.3390/jcm14207202
Chicago/Turabian Stylede Matos, Dihogo Gama, Jefferson Lima de Santana, Felipe J. Aidar, Stephen M. Cornish, Gordon G. Giesbrecht, Albená Nunes-Silva, Satish R. Raj, Roman Romero-Ortuno, Todd A. Duhamel, and Rodrigo Villar. 2025. "Short-Term Cardiovascular Compensatory Responses to Varying Levels of Orthostatic Stress During Active Standing in Older Adults" Journal of Clinical Medicine 14, no. 20: 7202. https://doi.org/10.3390/jcm14207202
APA Stylede Matos, D. G., de Santana, J. L., Aidar, F. J., Cornish, S. M., Giesbrecht, G. G., Nunes-Silva, A., Raj, S. R., Romero-Ortuno, R., Duhamel, T. A., & Villar, R. (2025). Short-Term Cardiovascular Compensatory Responses to Varying Levels of Orthostatic Stress During Active Standing in Older Adults. Journal of Clinical Medicine, 14(20), 7202. https://doi.org/10.3390/jcm14207202









