Twenty-Three-Year Mortality in Parkinson’s Disease: A Population-Based Prospective Study (NEDICES)
Abstract
1. Introduction
2. Methods
2.1. Study Areas
2.2. Study Design
2.3. Statistical Analyses
3. Results
3.1. Study Population
3.2. Baseline Characteristics
3.3. Follow-Up and Mortality Outcomes
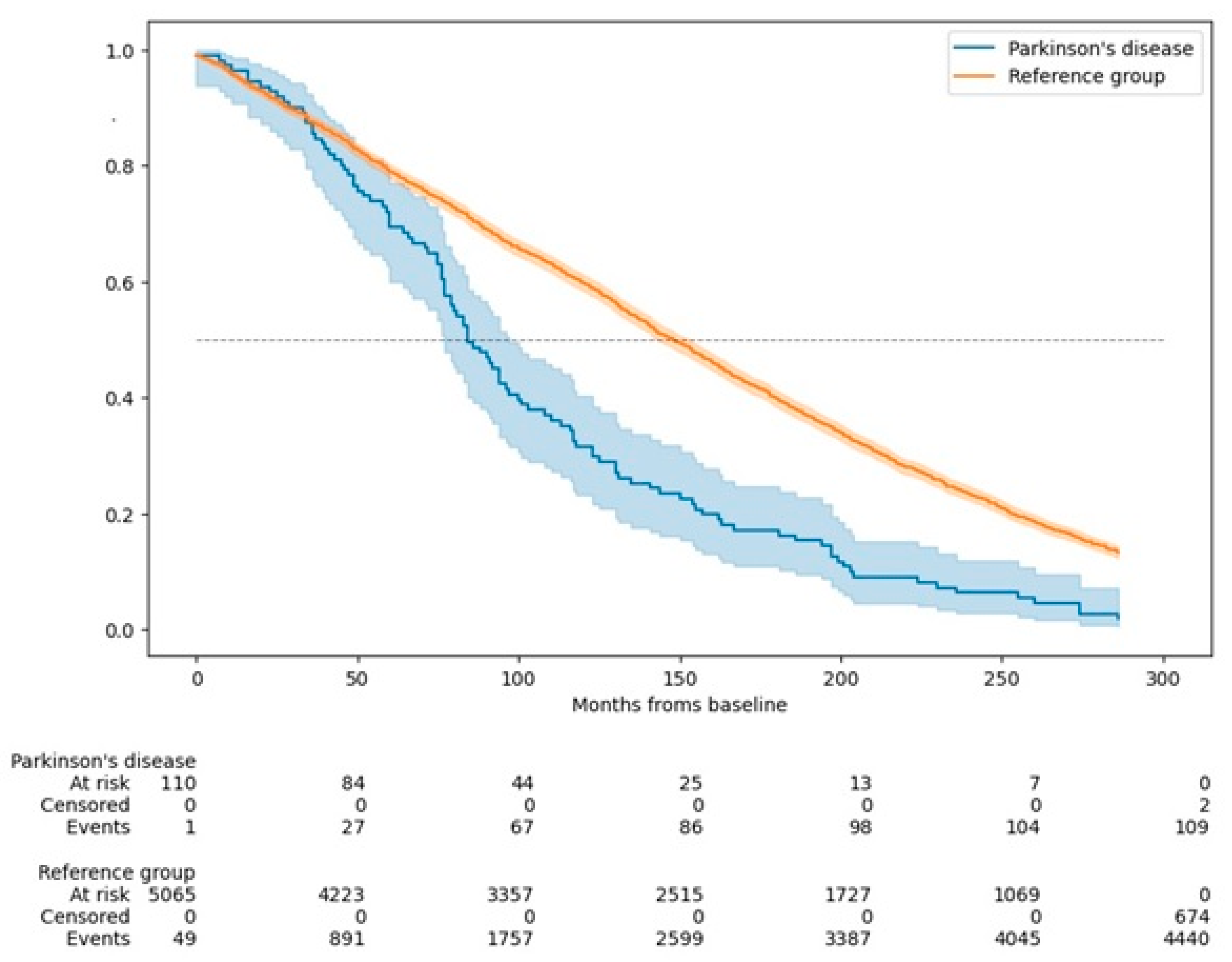
3.4. Survival Curves
3.5. Causes of Death
4. Discussion
4.1. Key Findings
4.2. Impact of Dementia
4.3. Age of Onset and Mortality
4.4. Underlying Causes of Mortality
4.5. Strengths and Limitations
4.6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
References
- Reeve, A.; Simcox, E.; Turnbull, D. Ageing and Parkinson’s disease: Why is advancing age the biggest risk factor? Ageing Res. Rev. 2014, 14, 19–30. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Gong, D.D.; Man, C.F.; Fan, Y. Parkinson’s disease and risk of mortality: Meta-analysis and systematic review. Acta Neurol. Scand. 2014, 129, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Alster, P.; Madetko-Alster, N. Significance of dysautonomia in Parkinson’s Disease and atypical parkinsonisms. Neurol. Neurochir. Pol. 2024, 58, 147–149. [Google Scholar] [CrossRef] [PubMed]
- De Pablo-Fernández, E.; Lees, A.J.; Holton, J.L.; Warner, T.T. Prognosis and Neuropathologic Correlation of Clinical Subtypes of Parkinson Disease. JAMA Neurol. 2019, 76, 470–479. [Google Scholar] [CrossRef] [PubMed]
- Postuma, R.B.; Berg, D.; Stern, M.; Poewe, W.; Olanow, C.W.; Oertel, W.; Obeso, J.; Marek, K.; Litvan, I.; Lang, A.E.; et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov. Disord. 2015, 30, 1591–1601. [Google Scholar] [CrossRef]
- Dommershuijsen, L.J.; Darweesh, S.K.L.; Ben-Shlomo, Y.; Kluger, B.M.; Bloem, B.R. The elephant in the room: Critical reflections on mortality rates among individuals with Parkinson’s disease. npj Park. Dis. 2023, 9, 145. [Google Scholar] [CrossRef] [PubMed]
- Posada, I.J.; Benito-León, J.; Louis, E.D.; Trincado, R.; Villarejo, A.; Medrano, M.J.; Bermejo-Pareja, F. Mortality from Parkinson’s disease: A population-based prospective study (NEDICES). Mov. Disord. 2011, 26, 2522–2529. [Google Scholar] [CrossRef]
- Benito-León, J.; Porta-Etessam, J.; Bermejo, F. Epidemiology of Parkinson disease. Neurologia 1998, 13 (Suppl. S1), 2–9. [Google Scholar] [PubMed]
- Benito-Leon, J. Epidemiology of Parkinson’s disease in Spain and its contextualisation in the world. Rev. Neurol. 2018, 66, 125–134. [Google Scholar]
- Ebmeier, K.P.; Calder, S.A.; Crawford, J.R.; Stewart, L.; Besson, J.A.; Mutch, W.J. Parkinson’s disease in Aberdeen: Survival after 3.5 years. Acta Neurol. Scand. 1990, 81, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Ben-Shlomo, Y.; Marmot, M.G. Survival and cause of death in a cohort of patients with parkinsonism: Possible clues to aetiology? J. Neurol. Neurosurg. Psychiatry 1995, 58, 293–299. [Google Scholar] [CrossRef]
- Morens, D.M.; Davis, J.W.; Grandinetti, A.; Ross, G.W.; Popper, J.S.; White, L.R. Epidemiologic observations on Parkinson’s disease: Incidence and mortality in a prospective study of middle-aged men. Neurology 1996, 46, 1044–1050. [Google Scholar] [CrossRef]
- Louis, E.D.; Marder, K.; Cote, L.; Tang, M.; Mayeux, R. Mortality from Parkinson Disease. Arch. Neurol. 1997, 54, 260–264. [Google Scholar] [CrossRef]
- Berger, K.; Breteler, M.M.; Helmer, C.; Inzitari, D.; Fratiglioni, L.; Trenkwalder, C.; Hofman, A.; Launer, L.J. Prognosis with Parkinson’s disease in europe: A collaborative study of population-based cohorts. Neurologic Diseases in the Elderly Research Group. Neurology 2000, 54 (Suppl. S5), S24–S27. [Google Scholar] [PubMed]
- Donnan, P.T.; Steinke, D.T.; Stubbings, C.; Davey, P.G.; MacDonald, T.M. Selegiline and mortality in subjects with Parkinson’s disease: A longitudinal community study. Neurology 2000, 55, 1785–1789. [Google Scholar] [CrossRef] [PubMed]
- Morgante, L.; Salemi, G.; Meneghini, F.; Di Rosa, A.E.; Epifanio, A.; Grigoletto, F.; Ragonese, P.; Patti, F.; Reggio, A.; Di Perri, R.; et al. Parkinson disease survival: A population-based study. Arch. Neurol. 2000, 57, 507–512. [Google Scholar] [CrossRef] [PubMed]
- Fall, P.-A.; Saleh, A.; Fredrickson, M.; Olsson, J.-E.; Granérus, A.-K. Survival time, mortality, and cause of death in elderly patients with Parkinson’s disease: A 9-year follow-up. Mov. Disord. 2003, 18, 1312–1316. [Google Scholar] [CrossRef]
- De Lau, L.M.L.; Schipper, C.M.A.; Hofman, A.; Koudstaal, P.J.; Breteler, M.M.B. Prognosis of Parkinson Disease: Risk of Dementia and Mortality: The Rotterdam Study. Arch. Neurol. 2005, 62, 1265. [Google Scholar] [CrossRef] [PubMed]
- Forsaa, E.B.; Larsen, J.P.; Wentzel-Larsen, T.; Alves, G. What predicts mortality in Parkinson disease?: A prospective population-based long-term study. Neurology 2010, 75, 1270–1276. [Google Scholar] [CrossRef] [PubMed]
- Savica, R.; Grossardt, B.R.; Bower, J.H.; Ahlskog, J.E.; Boeve, B.F.; Graff-Radford, J.; Rocca, W.A.; Mielke, M.M. Survival and Causes of Death Among People with Clinically Diagnosed Synucleinopathies with Parkinsonism: A Population-Based Study. JAMA Neurol. 2017, 74, 839–846. [Google Scholar] [CrossRef]
- Hobson, P.; Meara, J. Mortality and quality of death certification in a cohort of patients with Parkinson’s disease and matched controls in North Wales, UK at 18 years: A community-based cohort study. BMJ Open 2018, 8, e018969. [Google Scholar] [CrossRef] [PubMed]
- Keener, A.M.; Paul, K.C.; Folle, A.; Bronstein, J.M.; Ritz, B. Cognitive Impairment and Mortality in a Population-Based Parkinson’s Disease Cohort. J. Park. Dis. 2018, 8, 353–362. [Google Scholar] [CrossRef] [PubMed]
- Hoogland, J.; Post, B.; De Bie, R.M.A. Overall and Disease Related Mortality in Parkinson’s Disease—A Longitudinal Cohort Study. JPD 2019, 9, 767–774. [Google Scholar] [CrossRef]
- Morales, J.M.; Bermejo, F.P.; Benito-León, J.; Rivera-Navarro, J.; Trincado, R.; Gabriel, S.R.; Vega, S.; NEDICES Study Group. Methods and demographic findings of the baseline survey of the NEDICES cohort: A door-to-door survey of neurological disorders in three communities from Central Spain. Public Health 2004, 118, 426–433. [Google Scholar] [CrossRef] [PubMed]
- Vega, S.; Benito-León, J.; Bermejo-Pareja, F.; Medrano, M.J.; Vega-Valderrama, L.M.; Rodríguez, C.; Louis, E.D. Several factors influenced attrition in a population-based elderly cohort: Neurological disorders in Central Spain Study. J. Clin. Epidemiol. 2010, 63, 215–222. [Google Scholar] [CrossRef]
- Bermejo-Pareja, F.; Benito-León, J.; Vega, S.; Olazarán, J.; de Toledo, M.; Díaz-Guzmán, J.; Sánchez-Sánchez, F.; Morales-González, J.M.; Trincado, R.; Portera-Sánchez, A.; et al. Consistency of clinical diagnosis of dementia in NEDICES: A population-based longitudinal study in Spain. J. Geriatr. Psychiatry Neurol. 2009, 22, 246–255. [Google Scholar] [CrossRef]
- Benito-León, J.; Bermejo-Pareja, F.; Morales, J.; Vega, S.; Molina, J. Prevalence of essential tremor in three elderly populations of central Spain. Mov. Disord. 2003, 18, 389–394. [Google Scholar] [CrossRef]
- Benito-León, J.; Bermejo-Pareja, F.; Rodríguez, J.; Molina, J.-A.; Gabriel, R.; Morales, J.-M.; Neurological Disorders in Central Spain (NEDICES) Study Group. Prevalence of PD and other types of parkinsonism in three elderly populations of central Spain. Mov. Disord. 2003, 18, 267–274. [Google Scholar] [CrossRef]
- Díaz-Guzmán, J.; Bermejo-Pareja, F.; Benito-León, J.; Vega, S.; Gabriel, R.; Medrano, M.J. Prevalence of Stroke and Transient Ischemic Attack in Three Elderly Populations of Central Spain. Neuroepidemiology 2008, 30, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Benito-León, J.; Bermejo-Pareja, F.; Morales-González, J.M.; Porta-Etessam, J.; Trincado, R.; Vega, S.; Louis, E.D.; Neurological Disorders in Central Spain (NEDICES) Study Group. Incidence of Parkinson disease and parkinsonism in three elderly populations of central Spain. Neurology 2004, 62, 734–741. [Google Scholar] [CrossRef]
- The ILSA Group; Maggi, S.; Zucchetto, M.; Candelise, L.; Scarpini, E.; Scarlato, G.; Amaducci, L. The Italian Longitudinal Study on Aging (ILSA): Design and methods. Aging Clin. Exp. Res. 1994, 6, 464–473. [Google Scholar] [CrossRef]
- Bermejo, F.; Gabriel, R.; Vega, S.; Morales, J.M.; Rocca, W.A.; Anderson, D.W. Problems and Issues with Door-To-Door, Two-Phase Surveys: An Illustration from Central Spain. Neuroepidemiology 2001, 20, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Fahn, S.; Elton, R.; Members of the UPDRS Development Committee. The Unified Parkinson’s Disease Rating Scale. In Recent Developments in Parkinson’s Disease; Fahn, S., Marsden, C.D., Calne, D.B., Goldstein, M., Eds.; McMellam Health Care Information: Florham Park, NJ, USA, 1987; Volume 2, pp. 153–163. [Google Scholar]
- American Psychiatric Association. AP Association Task Force on DSM-IV. In Diagnostic and Statistical Manual of Mental Disorders: DSM-IV; American Psychiatric Association: Washington, DC, USA, 1994. [Google Scholar]
- Hoehn, M.M.; Yahr, M.D. Parkinsonism: Onset, progression, and mortality. 1967. Neurology 2001, 57 (Suppl. S3), S11–S26. [Google Scholar] [PubMed]
- Carey, I.M.; Shah, S.M.; Harris, T.; DeWilde, S.; Cook, D.G. A new simple primary care morbidity score predicted mortality and better explains between practice variations than the Charlson index. J. Clin. Epidemiol. 2013, 66, 436–444. [Google Scholar] [CrossRef]
- Fereshtehnejad, S.-M.; Yao, C.; Pelletier, A.; Montplaisir, J.Y.; Gagnon, J.-F.; Postuma, R.B. Evolution of prodromal Parkinson’s disease and dementia with Lewy bodies: A prospective study. Brain 2019, 142, 2051–2067. [Google Scholar] [CrossRef]
- Diederich, N.J.; Sauvageot, N.; Pieri, V.; Hipp, G.; Vaillant, M. The Clinical Non-Motor Connectome in Early Parkinson’s Disease. J. Park. Dis. 2020, 10, 1797–1806. [Google Scholar] [CrossRef] [PubMed]
- Siderowf, A.; Stern, M.B. Premotor Parkinson’s disease: Clinical features, detection, and prospects for treatment. Ann. Neurol. 2008, 64 (Suppl. S2), S139–S147. [Google Scholar] [CrossRef]
- Siderowf, A.; Lang, A.E. Premotor Parkinson’s disease: Concepts and definitions. Mov. Disord. 2012, 27, 608–616. [Google Scholar] [CrossRef]
- Fezeu, F.; Jbara, O.F.; Jbarah, A.; Choucha, A.; De Maria, L.; Ciaglia, E.; De Simone, M.; Samnick, S. PET imaging for a very early detection of rapid eye movement sleep behaviour disorder and Parkinson’s disease—A model-based cost-effectiveness analysis. Clin. Neurol. Neurosurg. 2024, 243, 108404. [Google Scholar] [CrossRef] [PubMed]
- Levy, G.; Tang, M.-X.; Louis, E.D.; Alfaro, B.; Mejia, H.; Stern, Y.; Marder, K. The association of incident dementia with mortality in PD. Neurology 2002, 59, 1708–1713. [Google Scholar] [CrossRef] [PubMed]
- Fasano, A.; Canning, C.G.; Hausdorff, J.M.; Lord, S.; Rochester, L. Falls in Parkinson’s disease: A complex and evolving picture. Mov. Disord. 2017, 32, 1524–1536. [Google Scholar] [CrossRef] [PubMed]
- Daley, D.J.; Myint, P.K.; Gray, R.J.; Deane, K.H.O. Systematic review on factors associated with medication non-adherence in Parkinson’s disease. Park. Relat. Disord. 2012, 18, 1053–1061. [Google Scholar] [CrossRef]
- Cereda, E.; Cilia, R.; Klersy, C.; Siri, C.; Pozzi, B.; Reali, E.; Colombo, A.; Zecchinelli, A.L.; Mariani, C.B.; Tesei, S.; et al. Dementia in Parkinson’s disease: Is male gender a risk factor? Park. Relat. Disord. 2016, 26, 67–72. [Google Scholar] [CrossRef]
- Hoogland, J.; Boel, J.A.; De Bie, R.M.A.; Schmand, B.A.; Geskus, R.B.; Dalrymple-Alford, J.C.; Marras, C.; Adler, C.H.; Weintraub, D.; Junque, C.; et al. Risk of Parkinson’s disease dementia related to level I MDS PD-MCI. Mov. Disord. 2019, 34, 430–435. [Google Scholar] [CrossRef] [PubMed]
- Wickremaratchi, M.M.; Ben-Shlomo, Y.; Morris, H.R. The effect of onset age on the clinical features of Parkinson’s disease. Eur. J. Neurol. 2009, 16, 450–456. [Google Scholar] [CrossRef]
- Pagano, G.; Ferrara, N.; Brooks, D.J.; Pavese, N. Age at onset and Parkinson disease phenotype. Neurology 2016, 86, 1400–1407. [Google Scholar] [CrossRef] [PubMed]
- Pinter, B.; Diem-Zangerl, A.; Wenning, G.K.; Scherfler, C.; Oberaigner, W.; Seppi, K.; Poewe, W. Mortality in Parkinson’s disease: A 38-year follow-up study. Mov. Disord. 2015, 30, 266–269. [Google Scholar] [CrossRef]
- Benito-León, J.; Louis, E.D.; Villarejo-Galende, A.; Romero, J.P.; Bermejo-Pareja, F. Under-reporting of Parkinson’s disease on death certificates: A population-based study (NEDICES). J. Neurol. Sci. 2014, 347, 188–192. [Google Scholar] [CrossRef]
- Coomber, R.; Alshameeri, Z.; Masia, A.F.; Mela, F.; Parker, M.J. Hip fractures and Parkinson’s disease: A case series. Injury 2017, 48, 2730–2735. [Google Scholar] [CrossRef]
- Burchill, E.; Watson, C.J.; Fanshawe, J.B.; Badenoch, J.B.; Rengasamy, E.; Ghanem, D.A.; Holle, C.; Conti, I.; Sadeq, M.A.; Saini, A.; et al. The impact of psychiatric comorbidity on Parkinson’s disease outcomes: A systematic review and meta-analysis. Lancet Reg. Health Eur. 2024, 39, 100870. [Google Scholar] [CrossRef]
- Hong, C.T.; Hu, H.H.; Chan, L.; Bai, C.-H. Prevalent cerebrovascular and cardiovascular disease in people with Parkinson’s disease: A meta-analysis. Clin. Epidemiol. 2018, 10, 1147–1154. [Google Scholar] [CrossRef]
- Williams, D.R.; de Silva, R.; Paviour, D.C.; Pittman, A.; Watt, H.C.; Kilford, L.; Holton, J.L.; Revesz, T.; Lees, A.J. Characteristics of two distinct clinical phenotypes in pathologically proven progressive supranuclear palsy: Richardson’s syndrome and PSP-parkinsonism. Brain 2005, 128 Pt 6, 1247–1258. [Google Scholar] [CrossRef]
- Caspell-Garcia, C.; Simuni, T.; Tosun-Turgut, D.; Wu, I.-W.; Zhang, Y.; Nalls, M.; Singleton, A.; Shaw, L.A.; Kang, J.-H.; Trojanowski, J.Q.; et al. Multiple modality biomarker prediction of cognitive impairment in prospectively followed de novo Parkinson disease. PLoS ONE 2017, 12, e0175674. [Google Scholar] [CrossRef]
- Fereshtehnejad, S.-M.; Zeighami, Y.; Dagher, A.; Postuma, R.B. Clinical criteria for subtyping Parkinson’s disease: Biomarkers and longitudinal progression. Brain 2017, 140, 1959–1976. [Google Scholar] [CrossRef] [PubMed]
- Espay, A.J.; Kalia, L.V.; Gan-Or, Z.; Williams-Gray, C.H.; Bedard, P.L.; Rowe, S.M.; Morgante, F.; Fasano, A.; Stecher, B.; Kauffman, M.A.; et al. Disease modification and biomarker development in Parkinson disease: Revision or reconstruction? Neurology 2020, 94, 481–494. [Google Scholar] [CrossRef]


| Year | Study | Cohort Characteristics | Key Findings |
|---|---|---|---|
| 1990 | Ebmeier et al. [10] | 267 patients and 233 matched controls in Scotland were followed for 3.5 years | The relative mortality rate was 2.35. Factors predicting death included cognitive impairment, older age, late disease onset, long-term smoking, low blood pressure, and Parkinson’s-related mobility issues |
| 1995 | Ben-Shlomo and Marmot [11] | 220 parkinsonian patients and 421 matched controls in the UK were followed for 20 years | The all-cause hazard ratio for patients compared with controls was 2.6. Both ischemic heart disease (2.3) and cerebrovascular disease (3.6) showed significantly increased hazard ratios |
| 1996 | Morens et al. [12] | 8006 middle-aged men from the Honolulu Heart Study were followed for 29 years | Between the ages of 70 and 89, Parkinson’s disease patients had a two- to three-fold increase in the mortality risk (mortality ratio = 2.5); survival was reduced by 8 years compared to controls |
| 1997 | Louis et al. [13] | 288 Parkinson’s disease patients, Manhattan, USA | The mortality risk, when compared with nondemented elderly subjects, was highest among those with both Parkinsón’s disease and dementia (rate ratio = 4.9). Dementia in the absence of Parkinson’s disease also was associated with an increased mortality risk (rate ratio = 1.6). A high baseline total extrapyramidal signs score was associated with significantly earlier mortality |
| 2000 | Berger et al. [14] | Pooled analysis of five European population-based cohorts (16,143 participants, including 252 with Parkinson’s disease) | The relative risk of death in Parkinson’s disease = 2.3. The risk for death in men with Parkinson’s disease (relative risk = 3.1) was higher than in women (relative risk = 1.8) |
| 2000 | Donnan et al. [15] | 97 Parkinson’s disease patients in Scotland | Parkinson’s disease patients, in relation to comparators, had higher mortality with a rate ratio of 1.76 in the 7-year cohort. There was significantly greater mortality in PD patients who received levodopa monotherapy (rate ratio = 2.45) |
| 2000 | Morgante et al. [16] | 59 patients and 118 matched controls in Sicily, Italy, were followed for 8 years. | Parkinson’s disease mortality was significantly higher, with a relative risk of 2.3; pneumonia was the most common cause of death |
| 2003 | Fall et al. [17] | 170 Parkinson’s disease patients and 510 matched controls in Sweden were followed for 9.4 years | The mortality rate ratio was 1.6 when comparing Parkinson’s disease patients with controls, and the all-cause hazard ratio was 2.4. PD patients also experienced a significantly higher proportion of deaths due to pneumonia |
| 2005 | de Lau et al. [18] (Rotterdam Study) | 6969 participants, including 99 prevalent and 67 incident Parkinson’s disease patients | Increased mortality risk (hazard ratio = 1.83). Within PD patients, mortality risk was influenced by disease duration and by the occurrence of dementia |
| 2010 | Forsaa et al. [19] | 230 Parkinson’s disease patients, followed from 1993 to 2009, Norway | Median survival was 15.8 years; mortality predictors included higher age at onset, older age, male sex, more severe motor impairment, psychotic symptoms, and dementia |
| 2011 | Posada et al. [7] (NEDICES Study) | 5262 participants, including 81 Parkinson’s disease patients, followed over 13 years in Spain | Parkinson’s disease mortality was higher (adjusted hazard ratio = 1.75); dementia further increased the risk (adjusted hazard ratio = 2.60) |
| 2017 | Savica et al. [20] | 461 patients with synucleinopathies, Minnesota, USA | Parkinson’s disease with dementia had a hazard ratio for death of 3.86. Parkinson’s disease alone had a hazard ratio of 1.75, while multiple system atrophy with parkinsonism exhibited the highest mortality, with a hazard ratio of 10.51 |
| 2018 | Hobson and Meara [21] | 166 Parkinson’s disease patients and 102 controls, followed for 18 years in Wales | Compared with the general UK population, Parkinson’s disease patients had a higher mortality risk, with a standardized mortality ratio of 1.82. The most common causes of death were pneumonia and cardiac-related conditions |
| 2018 | Keener et al. [22] | 360 Parkinson’s disease patients in California with a mean follow-up period of 5.8 years | Lower baseline Mini-mental State scores, reported longer average sleep duration, greater motor symptom severity, and motor subtype (postural instability gait difficulty) were significant predictors of mortality |
| 2019 | Hoogland et al. [23] | 133 newly diagnosed Parkinson’s disease patients in the Netherlands followed for at least 13 years | Increased mortality was associated with mild cognitive impairment, higher levodopa dose, and earlier onset |
| Parkinson’s Disease (N = 111) | Without Parkinson’s (N = 5114) | p Value | |
|---|---|---|---|
| Age in years | 76.5 ± 5.7 (76.0) | 74.3 ± 7.0 (73.0) | <0.001 |
| Sex (female) | 49 (44.1%) | 2949 (57.7%) | 0.004 |
| Study area | 0.359 | ||
| - Arévalo | 47 (42.3%) | 1874 (36.6%) | |
| - Las Margaritas | 31 (27.9%) | 1725 (33.7%) | |
| - Lista | 33 (29.6%) | 1515 (29.6%) | |
| Education in years of study completed * | 5.7 ± 7.1 (6.0) | 6.0 ± 5.3 (6.0) | 0.270 |
| Smoking habit * | 0.118 | ||
| - Smoker | 5 (5.4%) | 489 (12.2%) | |
| - Ex-smoker | 29 (31.5%) | 1068 (26.7%) | |
| - Never smoked | 58 (63.0%) | 2436 (61.0%) | |
| Alcohol consumption * | 0.233 | ||
| - Regular drinker | 23 (25.0%) | 1334 (33.4%) | |
| - Ex-drinker | 21 (22.8%) | 830 (20.8%) | |
| - Never drank | 48 (52.2%) | 1825 (45.8%) | |
| Arterial hypertension * | 62 (56.4%) | 2483 (51.0%) | 0.267 |
| Comorbidity index | 1.6 ± 1.8 (1.0) | 1.1 ± 1.5 (0.0) | 0.005 |
| Alive (N = 676) | Deceased (N = 4549) | p Value | |
|---|---|---|---|
| Age in years | 68.9 ± 3.9 (68.0) | 75.1 ± 7.0 (74.0) | <0.001 |
| Sex (female) | 460 (68.0%) | 2538 (55.8%) | <0.001 |
| Study area | 0.006 | ||
| - Arévalo | 211 (31.2%) | 1710 (37.6%) | |
| - Las Margaritas | 249 (36.8%) | 1507 (33.1%) | |
| - Lista | 216 (32.0%) | 1332 (29.3%) | |
| Education in years of study completed * | 6.8 ± 5.7 (7.0) | 5.9 ± 5.3 (6.0) | <0.001 |
| Smoking habit * | 0.002 | ||
| - Smoker | 62 (10.8%) | 432 (12.3%) | |
| - Ex-smoker | 125 (21.7%) | 972 (27.7%) | |
| - Never smoked | 388 (67.5%) | 2106 (60.0%) | |
| Alcohol consumption * | 0.050 | ||
| - Regular drinker | 208 (36.3%) | 1149 (32.8%) | |
| - Ex-drinker | 99 (17.3%) | 752 (21.4%) | |
| - Never drank | 266 (46.4%) | 1607 (45.8%) | |
| Arterial hypertension * | 254 (38.4%) | 2291 (53.1%) | <0.001 |
| Comorbidity index | 0.6 ± 1.0 (0.0) | 1.2 ± 1.6 (1.0) | <0.001 |
| A.Mortality Hazard Ratios in Parkinson’s Disease Patients Versus Those Without Parkinson’s Disease | ||||||||||||
| Unadjusted | Model 1 | Model 2 | Model 3 | |||||||||
| Hazard ratio | 95% CI | p Value | Hazard ratio | 95% CI | p Value | Hazard ratio | 95% CI | p Value | Hazard ratio | 95% CI | p Value | |
| Parkinson’s disease patients (N = 111) | 1.91 | 1.58–2.32 | <0.001 | 1.56 | 1.29–1.89 | <0.001 | 1.64 | 1.33–2.04 | <0.001 | 1.62 | 1.31–2.01 | <0.001 |
| Participants without Parkinson’s disease (N = 5114) (reference group) | 1.0 | _ | 1.0 | 1.0 | _ | 1.0 | 1.0 | _ | 1.0 | 1.0 | _ | 1.0 |
| B.Mortality hazard ratios in Parkinson’s disease patients, stratified by the presence or absence of dementia | ||||||||||||
| Unadjusted | Model 1 | Model 2 | Model 3 | |||||||||
| Hazard ratio | 95% CI | p value | Hazard ratio | 95% CI | p value | Hazard ratio | 95% CI | p value | Hazard ratio | 95% CI | p value | |
| Parkinson’s disease patients with dementia (N = 14) | 4.27 | 2.52–7.23 | <0.001 | 2.13 | 1.26–3.62 | 0.005 | 2.19 | 1.24–3.88 | 0.007 | 2.19 | 1.24–3.89 | 0.007 |
| Parkinson’s disease patients without dementia (N = 97) | 1.77 | 1.44–2.17 | <0.001 | 1.50 | 1.23–1.84 | <0.001 | 1.58 | 1.26–1.99 | <0.001 | 1.56 | 1.24–1.96 | <0.001 |
| Participants without either condition (N = 5114) (reference group) | 1.0 | _ | 1.0 | 1.0 | _ | 1.0 | 1.0 | _ | 1.0 | 1.0 | _ | 1.0 |
| C.Mortality hazard ratios in Parkinson’s disease patients, stratified by disease onset | ||||||||||||
| Unadjusted | Model 1 | Model 2 | Model 3 | |||||||||
| Hazard ratio | 95% CI | p value | Hazard ratio | 95% CI | p value | Hazard ratio | 95% CI | p value | Hazard ratio | 95% CI | p value | |
| Parkinson’s disease onset at age 65 or later (N = 92) | 1.87 | 1.52–2.30 | <0.001 | 1.46 | 1.19–1.80 | <0.001 | 1.58 | 1.25–1.99 | <0.001 | 1.56 | 1.24–1.97 | <0.001 |
| Parkinson’s disease onset before age 65 (N = 19) | 2.16 | 1.38–3.40 | <0.001 | 2.32 | 1.48–3.66 | <0.001 | 2.15 | 1.25–3.71 | 0.006 | 2.11 | 1.22–3.64 | 0.007 |
| Participants without Parkinson’s disease (N = 5114) (reference group) | 1.0 | _ | 1.0 | 1.0 | _ | 1.0 | 1.0 | _ | 1.0 | 1.0 | _ | 1.0 |
| Main Cause of Death | Parkinson’s Disease | Without Parkinson’s Disease | p Value ** |
|---|---|---|---|
| Dementia | 316 (7.2%) | 7 (6.4%) | 0.760 |
| Cardiovascular and cerebrovascular diseases | 1576 (35.8%) | 30 (27.5%) | 0.073 |
| Parkinson’s disease | 17 (0.4%) | 16 (14.7%) | <0.001 |
| Cancer | 950 (21.6%) | 17 (15.6%) | 0.131 |
| Respiratory diseases | 660 (15.0%) | 15 (13.8%) | 0.719 |
| Dementia | 316 (7.2%) | 7 (6.4%) | 0.760 |
| Other causes | 879 (20.0%) | 24 (22.0%) | 0.601 |
| Total | 4398 (100%) | 109 (100%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benito-Rodríguez, C.M.; Bermejo-Pareja, F.; Berbel, Á.; Lapeña-Motilva, J.; Benito-León, J. Twenty-Three-Year Mortality in Parkinson’s Disease: A Population-Based Prospective Study (NEDICES). J. Clin. Med. 2025, 14, 498. https://doi.org/10.3390/jcm14020498
Benito-Rodríguez CM, Bermejo-Pareja F, Berbel Á, Lapeña-Motilva J, Benito-León J. Twenty-Three-Year Mortality in Parkinson’s Disease: A Population-Based Prospective Study (NEDICES). Journal of Clinical Medicine. 2025; 14(2):498. https://doi.org/10.3390/jcm14020498
Chicago/Turabian StyleBenito-Rodríguez, Carla María, Félix Bermejo-Pareja, Ángel Berbel, José Lapeña-Motilva, and Julián Benito-León. 2025. "Twenty-Three-Year Mortality in Parkinson’s Disease: A Population-Based Prospective Study (NEDICES)" Journal of Clinical Medicine 14, no. 2: 498. https://doi.org/10.3390/jcm14020498
APA StyleBenito-Rodríguez, C. M., Bermejo-Pareja, F., Berbel, Á., Lapeña-Motilva, J., & Benito-León, J. (2025). Twenty-Three-Year Mortality in Parkinson’s Disease: A Population-Based Prospective Study (NEDICES). Journal of Clinical Medicine, 14(2), 498. https://doi.org/10.3390/jcm14020498






