Is It Feasible to Apply a Virtual Box and Block Test in Children with Unilateral Cerebral Palsy?: A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Materials
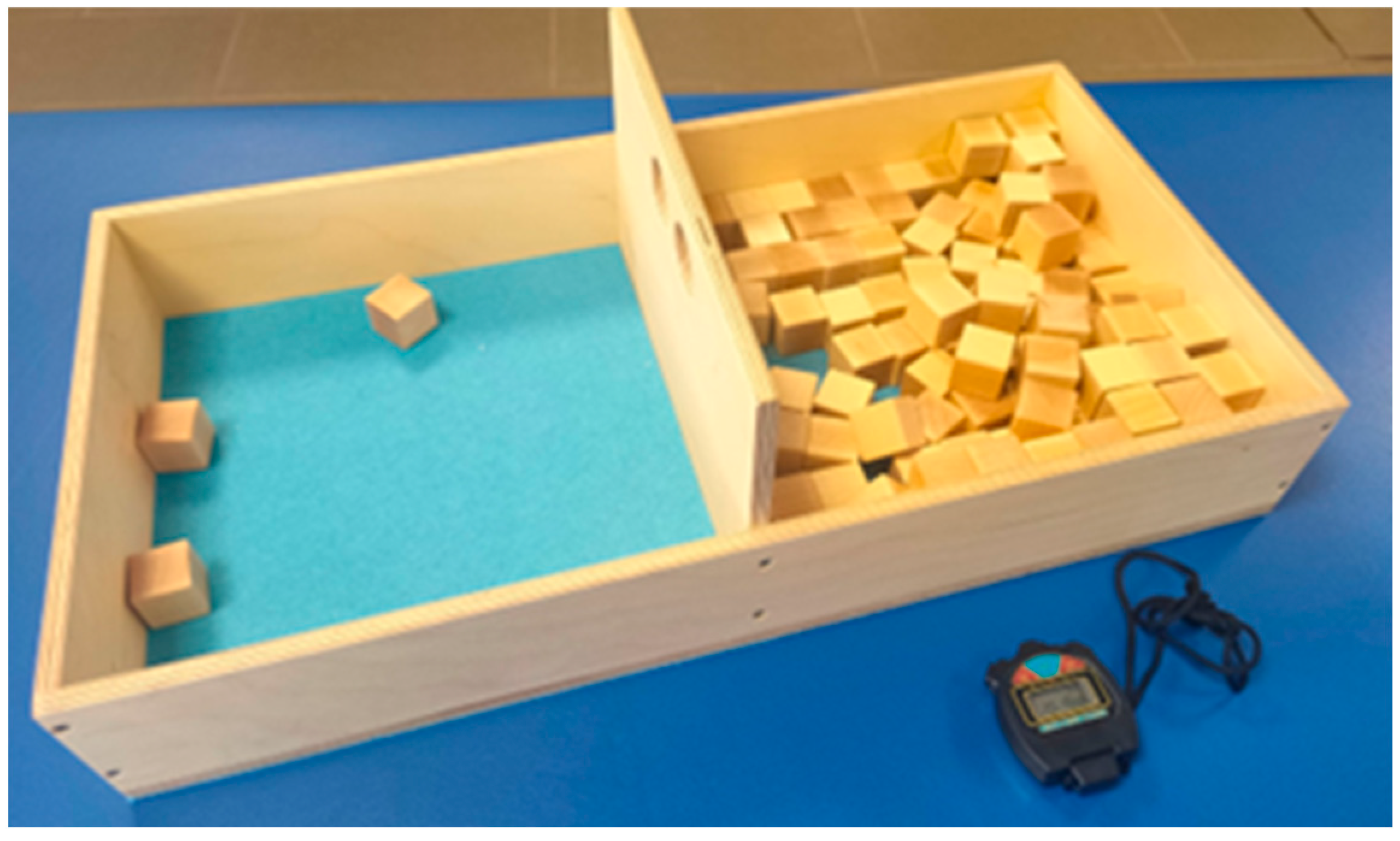
2.2.1. Box and Block Test
2.2.2. Virtual Box and Block Test Based on Leap Motion Controller
- SceneElements: this includes the scene’s main camera, lights and particle systems.
- LeapElements: elements that allow the capture of hand movements by the Leap Motion sensor.
- Graphical User Interface (GUI).
- WoodBox: formed by the box where the cubes and triggers used in the virtual application will be placed.
- Instructions panel, with the explanatory videos that are played before the game.
- Elements that compose the countdown of the start of the game (text and progress bar).
- Button and panel for selecting the hand to be used.
- Participant feedback elements: progress bar within the VR as well as the countdown clock.
- Score indicator (number of cubes).
- Summary panel after finishing a level, showing information about the level.
- Save game panel.
2.3. Experimental Setup
2.4. Data Analysis
3. Results
3.1. Correlation Analysis Between the Real and Virtual BBTs
Clinical Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rosenbaum, P.; Paneth, N.; Leviton, A.; Goldstein, M.; Bax, M. A report: The definition and classification of cerebral palsy April 2006. Dev. Med. Child Neurol. Suppl. 2007, 109, 8–14. [Google Scholar] [PubMed]
- Bax, M.; Goldstein, M.; Rosenbaun, P.; Leviton, A.; Paneth, N.; Dan, B.; Jacobsson, B.; Damiano, D. Proposed definition and classification of cerebral palsy, April 2005. Dev. Med. Child Neurol. 2005, 47, 571–576. [Google Scholar] [CrossRef] [PubMed]
- McIntyre, S.; Goldsmith, S.; Webb, A.; Ehlinger, V.; Hollung, S.J.; McConnell, K.; Arnaud, C.; Smithers-Sheedy, H.; Oskoui, M.; Khandaker, G.; et al. Global prevalence of cerebral palsy: A systematic analysis. Dev. Med. Child. Neurol. 2022, 64, 1494–1506. [Google Scholar] [CrossRef]
- Galea, C.; Mcintyre, S.; Smithers-Sheedy, H.; Reid, S.M.; Gibson, C.; Delacy, M.; Watson, L.; Goldsmith, S.; Badawi, N.; Blair, E. Cerebral palsy trends in Australia (1995–2009): A population-based observational study. Dev. Med. Child. Neurol. 2019, 61, 186–193. [Google Scholar] [CrossRef]
- Choi, J.Y.; Yi, S.H.; Shim, D.; Yoo, B.; Park, E.S.; Rha, D.W. Home-based virtual reality-enhanced upper limb training system in children with brain injury: A randomized controlled trial. Front. Pediatr. 2023, 11, 1131573. [Google Scholar] [CrossRef] [PubMed]
- Sakzewski, L.; Ziviani, J.; Boyd, R.N. Efficacy of upper limb therapies for unilateral cerebral palsy: A meta-analysis. Pediatrics 2014, 133, e175–e204. [Google Scholar] [CrossRef] [PubMed]
- Hoare, B.; Wallen, M.A.; Thorley, M.N.; Jackman, M.L.; Carey, L.M.; Imms, C. Constraint-induced movement therapy in children with unilateral cerebral palsy. Cochrane Database Syst. Rev. 2019, 4, CD004149. [Google Scholar] [CrossRef] [PubMed]
- Sakzewski, L.; Boyd, R.; Ziviani, J. Clinimetric properties of participation measures for 5-to 13-year-old children with cerebral palsy: A systematic review. Dev. Med. Child. Neurol. 2007, 49, 232–240. [Google Scholar] [CrossRef] [PubMed]
- Liang, K.J.; Chen, H.L.; Shieh, J.Y.; Wang, T.N. Measurement properties of the box and block test in children with unilateral cerebral palsy. Sci. Rep. 2021, 11, 20955. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.J.; Ku, K.H.; Park, Y.S.; Park, J.G.; Cho, E.S.; Seo, J.S.; Kim, C.W.; Hwi, O.S. Effects of Virtual Reality-Based Rehabilitation on Upper Extremity Function among Children with Cerebral Palsy. Healthcare 2020, 8, 391. [Google Scholar] [CrossRef]
- Meriggi, P.; Mandalà, M.; Randazzo, M.; Brazzoli, E.; Castagna, A.; Di Giusto, V.; Cavallini, A.; Marzegan, A.; Lencioni, T.; Olivieri, I. Non-immersive virtual reality based treatment for children with unilateral cerebral palsy: Preliminary results. J. Pediatr. Rehabil. Med. 2024, 17, 107–123. [Google Scholar] [CrossRef] [PubMed]
- Cruz, J.; Garcia, M.; Garza, C.; DeLucia, P.R.; Yang, J. Object shape affects hand grip function for heavy objects in younger and older adults. Ergonomics 2021, 64, 722–732. [Google Scholar] [CrossRef] [PubMed]
- Seo, N.J.; Enders, L.R. Hand grip function assessed by the box and block test is affected by object surfaces. J. Hand Ther. 2012, 25, 397–405. [Google Scholar] [CrossRef] [PubMed]
- Poitras, I.; Martinie, O.; Robert, M.T.; Campeau-Lecours, A.; Mercier, C. Impact of Sensory Deficits on Upper Limb Motor Performance in Individuals with Cerebral Palsy: A Systematic Review. Brain Sci. 2021, 11, 744. [Google Scholar] [CrossRef]
- Oña, E.D.; Jardón, A.; Cuesta-Gómez, A.; Sánchez-Herrera-Baeza, P.; Cano-de-la-Cuerda, R.; Balaguer, C. Validity of a Fully-Immersive VR-Based Version of the Box and Blocks Test for Upper Limb Function Assessment in Parkinson’s Disease. Sensors 2020, 20, 2773. [Google Scholar] [CrossRef] [PubMed]
- Harris, K.; Reid, D. The influence of virtual reality play on children’s motivation. Can. J. Occup. Ther. 2005, 72, 21–29. [Google Scholar] [CrossRef]
- Parker, S.M.; Ricks, B.; Zuniga, J.; Knarr, B.A. Comparison of virtual reality to physical box and blocks on cortical an neuromuscualar activations in young adults. Sci. Rep. 2023, 13, 16567. [Google Scholar] [CrossRef] [PubMed]
- Maggio, M.G.; Valeri, M.C.; De Luca, R.; Di Iulio, F.; Ciancarelli, I.; De Francesco, M.; Calabrò, R.S.; Morone, G. The Role of Immersive Virtual Reality Interventions in Pediatric Cerebral Palsy: A Systematic Review across Motor and Cognitive Domains. Brain Sci. 2024, 14, 490. [Google Scholar] [CrossRef] [PubMed]
- Bryanton, C.; Bossé, J.; Brien, M.; McLean, J.; McCormick, A.; Sveistrup, H. Feasibility, motivation, and selective motor control: Virtual reality compared to conventional home exercise in children with cerebral palsy. Cyberpsychol. Behav. 2006, 9, 123–128. [Google Scholar] [CrossRef]
- Prochaska, E.; Ammenwerth, E. A Digital Box and Block Test for Hand Dexterity Measurement: Instrument Validation Study. JMIR Rehabil. Assist. Technol. 2023, 10, e50474. [Google Scholar] [CrossRef] [PubMed]
- Everard, G.; Otmane-Tolba, Y.; Rosselli, Z.; Pellissier, T.; Ajana, K.; Dehem, S.; Auvinet, E.; Edwards, M.G.; Lebleu, J.; Lejeune, T. Concurrent validity of an immersive virtual reality version of the Box and Block Test to assess manual dexterity among patients with stroke. J. Neuroeng. Rehabil. 2022, 19, 7. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Rodríguez, M.; López-Dolado, E.; Salas-Monedero, M.; Lozano-Berrio, V.; Ceruelo-Abajo, S.; Gil-Agudo, A.; de los Reyes-Guzmán, A. Concurrent Validity of a Virtual Version of Box and Block Test for Patients with Neurological Disorders. World J. Neurosci. 2020, 10, 79–89. [Google Scholar] [CrossRef]
- Eliasson, A.C.; Krumlinde-Sundholm, L.; Rösblad, B.; Beckung, E.; Arner, M.; Öhrvall, A.M.; Rosenbaum, P. The Manual Ability Classification System (MACS) for children with cerebral palsy: Scale development and evidence of validity and reliability. Dev. Med. Child. Neurol. 2006, 48, 549–554. [Google Scholar] [CrossRef]
- Palisano, R.; Rosenbaum, P.; Walter, S.; Russell, D.; Wood, E.; Galuppi, B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev. Med. Child. Neurol. 1997, 39, 214–223. [Google Scholar] [CrossRef]
- Mathiowetz, V.; Federman, S.; Wiemer, D. Box and block test of manual dexterity: Norms for 6–19 year olds. Can. J. Occup. Ther. 1985, 52, 241–245. [Google Scholar] [CrossRef]
- McGraw, K.O.; Wong, S.P. Forming inferences about some intraclass correlation coefficients. Psychol. Methods. 1996, 96, 30–46. [Google Scholar] [CrossRef]
- Shrout, P.E.; Fleiss, J.L. Intraclass correlations: Uses in assessing rater reliability. Psychol. Bull. 1979, 86, 420–428. [Google Scholar] [CrossRef]
- Everard, G.; Burton, Q.; Van de Sype, V.; Bibentyo, T.N.; Auvinet, E.; Edwards, M.G.; Batcho, C.S.; Lejeune, T. Extended reality to assess post-stroke manual dexterity: Contrasts between the classic box and block test, immersive virtual reality with controllers, with hand-tracking, and mixed-reality tests. J. Neuroeng. Rehabil. 2024, 21, 36. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Liu, X.; Tang, M.; Huo, H.; Chen, D.; Wu, Z.; An, R.; Fan, Y. A haptic-feedback virtual reality system to improve the box and block test (BBT) for upper extremity motor function assessment. Virtual Real. 2023, 27, 1199–1219. [Google Scholar] [CrossRef]
- Cho, S.; Kim, W.S.; Paik, N.J.; Bang, H. Upper-limb function assessment using VBBTs for stroke patients. IEEE Comput. Graph. Appl. 2016, 36, 70–78. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, J.M.; Fernandes, R.C.; Pinto, C.S.; Pinheiro, P.R.; Ribeiro, S.; de Albuquerque, V.H. Novel Virtual Environment for Alternative Treatment of Children with Cerebral Palsy. Comput. Intell. Neurosci. 2016, 2016, 8984379. [Google Scholar] [CrossRef] [PubMed]
- Jongbloed-Pereboom, M.; Nijhuis-van der Sanden, M.W.G.; Steenbergen, B. Norm scores of the box and block test for children ages 3-10 years. Am. J. Occup. Ther. 2013, 67, 312–318. [Google Scholar] [CrossRef]
- Figueiredo, P.R.P.; Mancini, M.C.; Feitosa, A.M.; Teixeira, C.M.M.F.; Guerzoni, V.P.D.; Elvrum, A.G.; Ferre, C.L.; Gordon, A.M.; BrandÃo, M.B. Hand-arm bimanual intensive therapy and daily functioning of children with bilateral cerebral palsy: A randomized controlled trial. Dev. Med. Child. Neurol. 2020, 62, 1274–1282. [Google Scholar] [CrossRef]
- Erkek, S.; Çekmece, Ç. Investigation of the Relationship between Sensory-Processing Skills and Motor Functions in Children with Cerebral Palsy. Children 2023, 10, 1723. [Google Scholar] [CrossRef] [PubMed]
- Crotti, M.; Ortibus, E.; Itzhak, N.B.; Kleeren, L.; Decraene, L.; Leenaerts, N.; Feys, H.; Mailleux, L. The relation between visual functions, functional vision, and bimanual function in children with unilateral cerebral palsy. Res. Dev. Disabil. 2024, 152, 104792. [Google Scholar] [CrossRef]
- James, S.; Ziviani, J.; Ware, R.S.; Boyd, R.N. Relationships between activities of daily living, upper limb function, and visual perception in children and adolescents with unilateral cerebral palsy. Dev. Med. Child. Neurol. 2015, 57, 852–857. [Google Scholar] [CrossRef] [PubMed]
- Vaz, D.V.; Mancini, M.C.; Fonseca, S.T.; Vieira, D.S.R.; de Melo Pertenece, A.E. Muscle stiffness and strength and their relation to hand function in children with hemiplegic cerebral palsy. Dev. Med. Child. Neurol. 2006, 48, 728–733. [Google Scholar] [CrossRef] [PubMed]
- Russo, R.N.; Skuza, P.P.; Sandelance, M.; Flett, P. Upper limb impairments, process skills, and outcome in children with unilateral cerebral palsy. Dev. Med. Child. Neurol. 2019, 61, 1080–1086. [Google Scholar] [CrossRef]
- Şahin, S.; Köse, B.; Aran, O.T.; Ağce, Z.; Kayıhan, H. The Effects of Virtual Reality on Motor Functions and Daily Life Activities in Unilateral Spastic Cerebral Palsy: A Single-Blind Randomized Controlled Trial. Games Health J. 2020, 9, 45–52. [Google Scholar] [CrossRef]


| Participant | Age (Years) | Sex (M/F) | Diagnosis CP | Affectionate Side (R/L) | GMFCS Level | MACS Level |
|---|---|---|---|---|---|---|
| 1 | 8 | M | UCP Spastic | L | II | III |
| 2 | 6 | M | UCP Spastic | R | I | II |
| 3 | 4 | M | UCP Spastic | R | I | II |
| 4 | 4 | M | UCP Spastic | R | I | II |
| 5 | 4 | M | UCP Spastic | R | I | II |
| 6 | 4 | M | UCP Spastic | R | I | II |
| 7 | 6 | M | UCP Spastic | R | I | III |
| (m ± SD) | 5.1 ± 1.6 | - | - | - | - | - |
| Box and Block Test (Number of Cubes) Real Test | Box and Block Test (Number of Cubes) Virtual Test | |||||
|---|---|---|---|---|---|---|
| T1 | T2 | T3 | T1 | T2 | T3 | |
| Dominant (less affected side) | 26.43 ± 7.26 | 23.57 ± 8.00 | 28.17 ± 6.31 | 5.33 ± 5.39 | 8.20 ± 4.60 | 9.00 ± 5.90 |
| Mean ± SD | 25.95 ± 7.14 | 7.47 ± 5.29 | ||||
| Non-Dominant (more affected side) | 4.14 ± 3.98 | 5.71 ± 5.23 | 10.17 ± 8.38 | 2.33 ± 3.51 | 3.60 ± 3.98 | 3.67 ± 3.67 |
| Mean ± SD | 6.50 ± 6.21 | 3.18 ± 3.52 | ||||
| BBT Real–BBT Virtual | |||
|---|---|---|---|
| T1 | T2 | T3 | |
| Dominant (less affected side) | 0.647 | 0.918 * | 0.708 |
| Non-Dominant (more affected side) | 0.638 | 0.894 * | 0.530 |
| Non-Dominant (More Affected Side) | |||
|---|---|---|---|
| Strength Measure | T1 | T2 | T3 |
| Elbow flexors | 4 (4–4) | 4 (4–4.75) | 4 (4–4) |
| Elbow extensors | 3 (3–4) | 3.5 (3–4) | 3 (3–3.75) |
| Wrist flexors | 0 (0–2) | 1.5 (0.25–2.75) | 1.5 (1–2.75) |
| Wrist extensors | 1 (0–1) | 1 (0.25–1) | 1 (0.25–3.25) |
| Finger flexors | 1 (1–3) | 2 (1.25–3.5) | 3 (2.25–3.75) |
| Finger abductors | 1 (0–2) | 1 (1–2.5) | 2 (0.25–3) |
| Hypertonia | |||
| Elbow pronators | 1 (0–1) | 0 (0–0.75) | 1 (0.25–1.75) |
| Wrist flexors | 1 (0–1) | 0.5 (0–1) | 0 (0–1.5) |
| Finger flexors | 0 (0–0) | 0 (0–0) | 0 (0–0) |
| Non-Dominant (More Affected Side) | Box and Block Real Test | Box and Block Virtual Test | ||
|---|---|---|---|---|
| Strength Measure | r | p-Value | r | p-Value |
| Wrist Flexors | 0.522 | 0.022 | 0.758 | <0.001 |
| Wrist Extensors | 0.465 | 0.045 | 0.369 | 0.145 |
| Finger Flexors | 0.798 | <0.001 | 0.602 | 0.011 |
| Finger Abductors | 0.658 | 0.002 | 0.217 | 0.402 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pérez-Nombela, S.; Merino-Andrés, J.; Gómez-Soriano, J.; Álvarez-Rodríguez, M.; Ceruelo-Abajo, S.; López-Muñoz, P.; Palomo-Carrión, R.; de los Reyes-Guzmán, A. Is It Feasible to Apply a Virtual Box and Block Test in Children with Unilateral Cerebral Palsy?: A Pilot Study. J. Clin. Med. 2025, 14, 391. https://doi.org/10.3390/jcm14020391
Pérez-Nombela S, Merino-Andrés J, Gómez-Soriano J, Álvarez-Rodríguez M, Ceruelo-Abajo S, López-Muñoz P, Palomo-Carrión R, de los Reyes-Guzmán A. Is It Feasible to Apply a Virtual Box and Block Test in Children with Unilateral Cerebral Palsy?: A Pilot Study. Journal of Clinical Medicine. 2025; 14(2):391. https://doi.org/10.3390/jcm14020391
Chicago/Turabian StylePérez-Nombela, Soraya, Javier Merino-Andrés, Julio Gómez-Soriano, María Álvarez-Rodríguez, Silvia Ceruelo-Abajo, Purificación López-Muñoz, Rocío Palomo-Carrión, and Ana de los Reyes-Guzmán. 2025. "Is It Feasible to Apply a Virtual Box and Block Test in Children with Unilateral Cerebral Palsy?: A Pilot Study" Journal of Clinical Medicine 14, no. 2: 391. https://doi.org/10.3390/jcm14020391
APA StylePérez-Nombela, S., Merino-Andrés, J., Gómez-Soriano, J., Álvarez-Rodríguez, M., Ceruelo-Abajo, S., López-Muñoz, P., Palomo-Carrión, R., & de los Reyes-Guzmán, A. (2025). Is It Feasible to Apply a Virtual Box and Block Test in Children with Unilateral Cerebral Palsy?: A Pilot Study. Journal of Clinical Medicine, 14(2), 391. https://doi.org/10.3390/jcm14020391






