Unraveling the Easix Score: Its Association with Vasopressor Need in Critically Ill Septic Pediatric Hematology–Oncology Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
2.3. Definitions
2.4. Statistical Analysis
3. Results
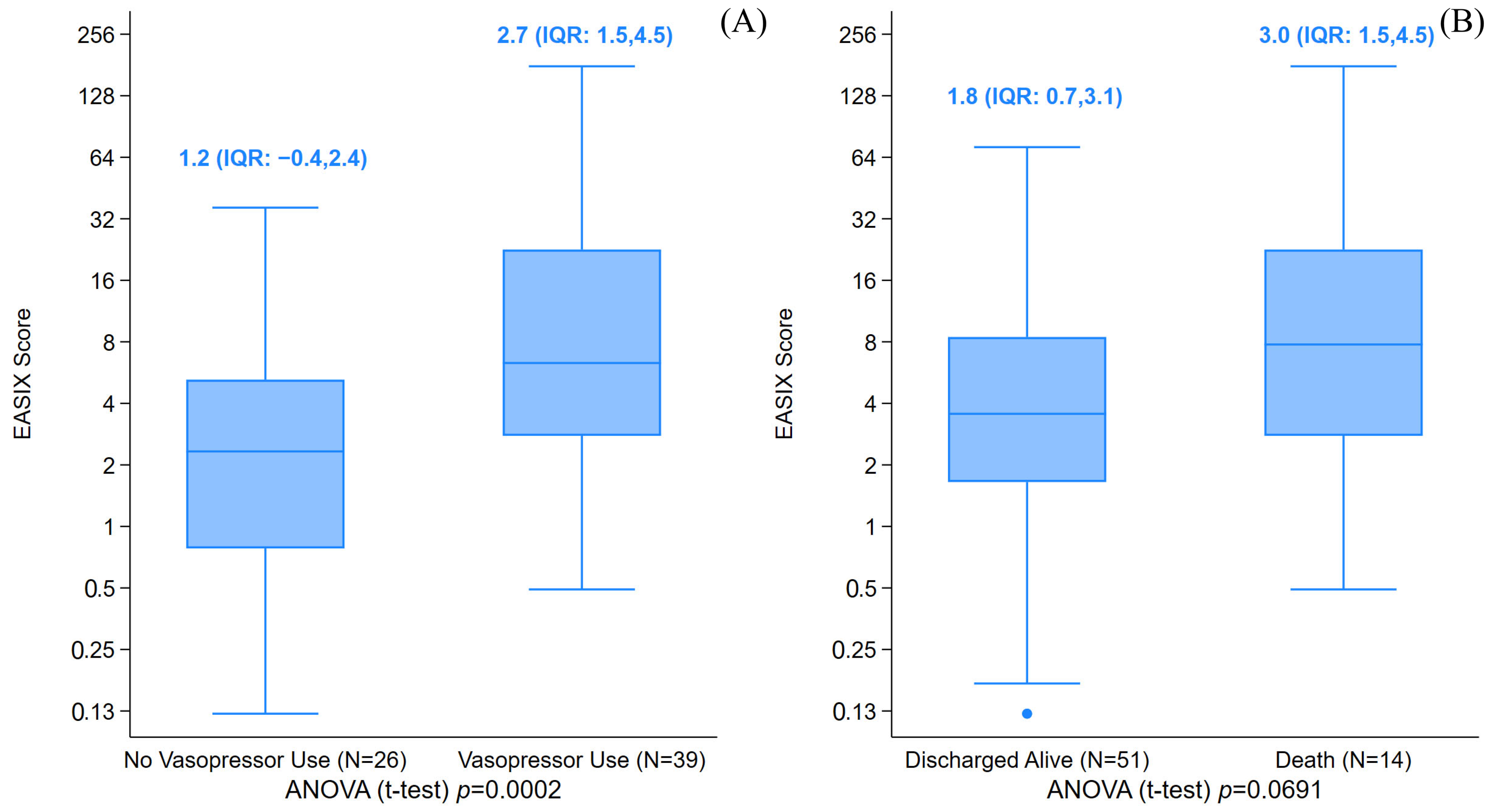
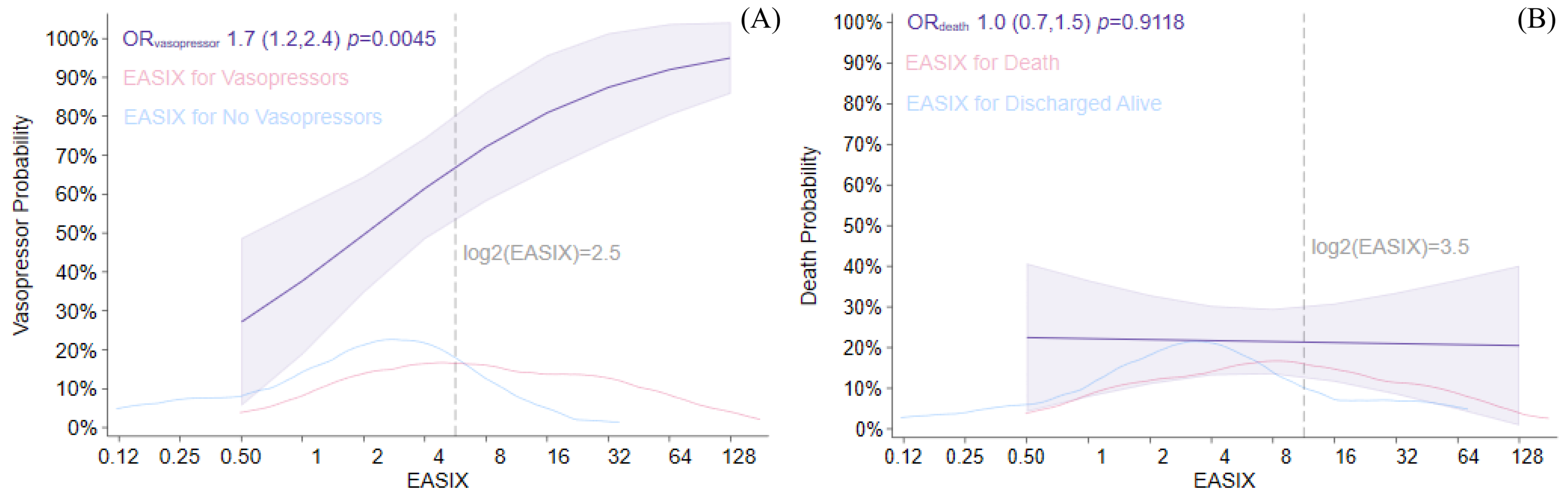
3.1. EASIX Score and Outcome
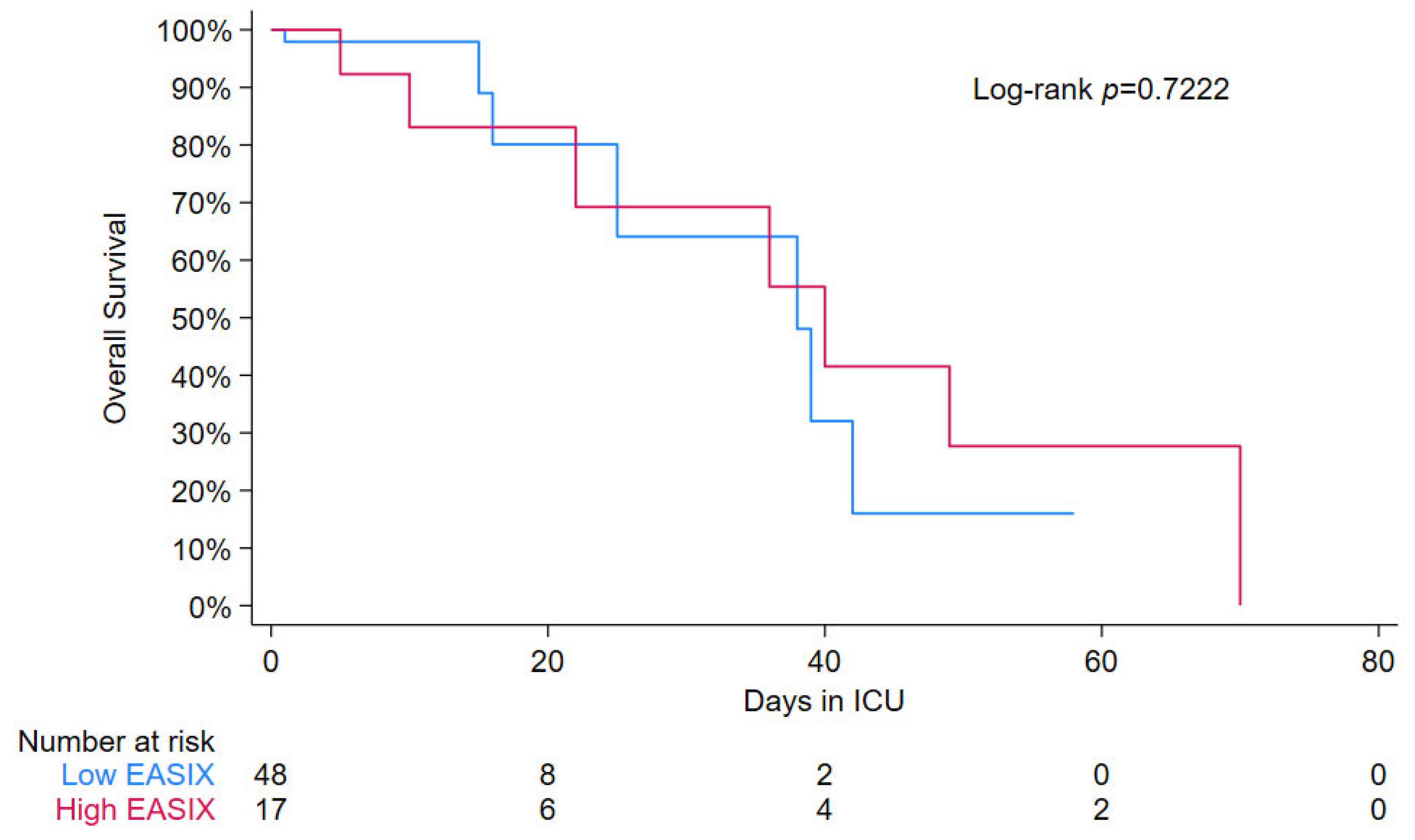
3.2. EASIX Score and Survival
3.3. EASIX Score Versus Modified EASIX Score
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| EASIX | Endothelial Activation and Stress Index |
| mEASIX | Modified Endothelial Activation and Stress Index |
| PHO | Pediatric hematology oncology |
| HCT | Hematopoietic cell transplant |
| RRT | Renal replacement therapy |
| ICU | Intensive care unit |
| LDH | Lactate dehydrogenase |
| OR | Odds ratio |
| AUC | Area under curve |
| ROC | Receiver operating characteristic |
| CRP | C-reactive protein |
| PIM | Pediatric Index of Mortality |
| PRISM | Pediatric Risk of Mortality |
| IMV | Invasive mechanical ventilation |
| ICD | International Classification of Diseases |
| CRS | Cytokine release syndrome |
| ICANS | Immune effector cell-associated neurotoxicity syndrome |
| CD19-CAR | CD19-directed chimeric antigen receptor |
| SOS | Sinusoidal obstruction syndrome |
References
- Agulnik, A. Management of septic shock in children with cancer-Common challenges and research priorities. J. Pediatr. 2023, 99, 101–104. [Google Scholar] [CrossRef]
- Palomo, M.; Diaz-Ricart, M.; Carbo, C.; Rovira, M.; Fernandez-Aviles, F.; Escolar, G.; Eissner, G.; Holler, E.; Carreras, E. The release of soluble factors contributing to endothelial activation and damage after hematopoietic stem cell transplantation is not limited to the allogeneic setting and involves several pathogenic mechanisms. Biol. Blood Marrow Transplant. 2009, 15, 537–546. [Google Scholar] [CrossRef]
- Palomo, M.; Diaz-Ricart, M.; Carbo, C.; Rovira, M.; Fernandez-Aviles, F.; Martine, C.; Ghita, G.; Escolar, G.; Carreras, E. Endothelial dysfunction after hematopoietic stem cell transplantation: Role of the conditioning regimen and the type of transplantation. Biol. Blood Marrow Transplant. 2010, 16, 985–993. [Google Scholar] [CrossRef] [PubMed]
- DeLeve, L.D.; Shulman, H.M.; McDonald, G.B. Toxic injury to hepatic sinusoids: Sinusoidal obstruction syndrome (veno-occlusive disease). Semin. Liver Dis. 2002, 22, 27–42. [Google Scholar] [CrossRef] [PubMed]
- Akwii, R.G.; Sajib, M.S.; Zahra, F.T.; Mikelis, C.M. Role of Angiopoietin-2 in Vascular Physiology and Pathophysiology. Cells 2019, 8, 471. [Google Scholar] [CrossRef]
- Reiss, Y.; Scholz, A.; Plate, K.H. The Angiopoietin—Tie System: Common Signaling Pathways for Angiogenesis, Cancer, and Inflammation. In Endothelial Signaling in Development and Disease; Schmidt, M.H.H., Liebner, S., Eds.; Springer: New York, NY, USA, 2015; pp. 313–328. [Google Scholar] [CrossRef]
- Jodele, S.; Davies, S.M.; Lane, A.; Khoury, J.; Dandoy, C.; Goebel, J.; Myers, K.; Grimley, M.; Bleesing, J.; El-Bietar, J.; et al. Diagnostic and risk criteria for HSCT-associated thrombotic microangiopathy: A study in children and young adults. Blood 2014, 124, 645–653. [Google Scholar] [CrossRef] [PubMed]
- Pedraza, A.; Salas, M.Q.; Rodríguez-Lobato, L.G.; Escribano-Serrat, S.; Suárez-Lledo, M.; Martínez-Cebrian, N.; Solano, M.T.; Arcarons, J.; Rosiñol, L.; Gutiérrez-García, G.; et al. Easix Score Correlates with Endothelial Dysfunction Biomarkers and Predicts Risk of Acute Graft-Versus-Host Disease After Allogeneic Transplantation. Transplant. Cell Ther. 2024, 30, 187.e1–187.e12. [Google Scholar] [CrossRef]
- Muratore, E.; Gambuti, G.; Leardini, D.; Baccelli, F.; Venturelli, F.; Larcinese, L.; Gottardi, F.; Di Battista, A.; Belotti, T.; Prete, A.; et al. The EASIX score as a predictor of sinusoidal obstruction syndrome and nonrelapse mortality in paediatric patients receiving allogeneic haematopoietic stem cell transplantation. Bone Marrow Transplant. 2025, 60, 346–352. [Google Scholar] [CrossRef]
- Ince, C.; Mayeux, P.R.; Nguyen, T.; Gomez, H.; Kellum, J.A.; Ospina-Tascón, G.A.; Hernandez, G.; Murray, P.; De Backer, D. The Endothelium in Sepsis. Shock 2016, 45, 259–270. [Google Scholar] [CrossRef]
- Xu, H.B.; Ye, Y.; Xue, F.; Wu, J.; Suo, Z.; Zhang, H. Association Between Endothelial Activation and Stress Index and 28-Day Mortality in Septic ICU patients: A Retrospective Cohort Study. Int. J. Med. Sci. 2023, 20, 1165–1173. [Google Scholar] [CrossRef]
- Weiss, S.L.; Peters, M.J.; Alhazzani, W.; Agus, M.S.D.; Flori, H.R.; Inwald, D.P.; Nadel, S.; Schlapbach, L.J.; Tasker, R.C.; Argent, A.C.; et al. Surviving sepsis campaign international guidelines for the management of septic shock and sepsis-associated organ dysfunction in children. Intensive Care Med. 2020, 46, 10–67. [Google Scholar] [CrossRef]
- Di Nardo, M.; Ghafoor, S.; Szmit, Z.; Elbahlawan, L.; Rowan, C.M.; Agulnik, A.; Asperen, R.W.; Zinter, M.S.; Nellis, M.E.; Moody, K.; et al. International expert consensus statement on PICU admission and early critical care management for paediatric patients following haematopoietic cell transplant and immune effector cell therapy. Lancet Child. Adolesc. Health 2025, 9, 426–438. [Google Scholar] [CrossRef]
- Scott, H.F.; Brilli, R.J.; Paul, R.; Macias, C.G.; Niedner, M.; Depinet, H.; Richardson, T.; Riggs, R.; Gruhler, H.; Larsen, G.Y.; et al. Evaluating Pediatric Sepsis Definitions Designed for Electronic Health Record Extraction and Multicenter Quality Improvement. Crit. Care Med. 2020, 48, e916–e926. [Google Scholar] [CrossRef]
- Luft, T.; Benner, A.; Jodele, S.; Dandoy, C.E.; Storb, R.; Gooley, T.; Sandmaier, B.M.; Becker, N.; Radujkovic, A.; Dreger, P.; et al. EASIX in patients with acute graft-versus-host disease: A retrospective cohort analysis. Lancet Haematol. 2017, 4, e414–e423. [Google Scholar] [CrossRef] [PubMed]
- Zińczuk, A.; Rorat, M.; Simon, K.; Jurek, T. EASIX, Modified EASIX and Simplified EASIX as an Early Predictor for Intensive Care Unit Admission and Mortality in Severe COVID-19 Patients. J. Pers. Med. 2022, 12, 1022. [Google Scholar] [CrossRef]
- Sanchez-Escamilla, M.; Flynn, J.; Devlin, S.; Maloy, M.; Fatmi, S.A.; Tomas, A.A.; Escribano-Serrat, S.; Ponce, D.; Sauter, C.S.; Giralt, S.A.; et al. EASIX score predicts inferior survival after allogeneic hematopoietic cell transplantation. Bone Marrow Transplant. 2023, 58, 498–505. [Google Scholar] [CrossRef] [PubMed]
- Dolmatova, E.V.; Wang, K.; Mandavilli, R.; Griendling, K.K. The effects of sepsis on endothelium and clinical implications. Cardiovasc. Res. 2021, 117, 60–73. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhang, X.; Zhang, M.; Guo, R.; Zhang, Y.; Pu, Y.; Zhu, H.; Liu, P.; Zhang, Y.; He, X.; et al. Modified EASIX scores predict severe CRS/ICANS in patients with acute myeloid leukemia following CLL1 CAR-T cell therapy. Ann. Hematol. 2024, 103, 969–980. [Google Scholar] [CrossRef]
- Pennisi, M.; Sanchez-Escamilla, M.; Flynn, J.R.; Shouval, R.; Alarcon Tomas, A.; Silverberg, M.L.; Batlevi, C.; Brentjens, R.J.; Dahi, P.B.; Devlin, S.M.; et al. Modified EASIX predicts severe cytokine release syndrome and neurotoxicity after chimeric antigen receptor T cells. Blood Adv. 2021, 5, 3397–3406. [Google Scholar] [CrossRef] [PubMed]
- Zandaki, D.; Selukar, S.; Bi, Y.; Li, Y.; Zinsky, M.; Bonifant, C.L.; Epperly, R.; Keerthi, D.; Triplett, B.M.; Gottschalk, S.; et al. EASIX and m-EASIX predict CRS and ICANS in pediatric and AYA patients after CD19-CAR T-cell therapy. Blood Adv. 2025, 9, 270–279. [Google Scholar] [CrossRef]
- Fernández-Sarmiento, J.; Molina, C.F.; Salazar-Pelaez, L.M.; Flórez, S.; Alarcón-Forero, L.C.; Sarta, M.; Hernández-Sarmiento, R.; Villar, J.C. Biomarkers of Glycocalyx Injury and Endothelial Activation are Associated with Clinical Outcomes in Patients with Sepsis: A Systematic Review and Meta-Analysis. J. Intensive Care Med. 2023, 38, 95–105. [Google Scholar] [CrossRef] [PubMed]

| Low EASIX | High EASIX | Total | p-Value | |
|---|---|---|---|---|
| N | 42 (64.6%) | 23 (35.4%) | 65 (100.0%) | |
| Sex | ||||
| Female | 17 (40.5%) | 15 (65.2%) | 32 (49.2%) | 0.072 |
| Male | 25 (59.5%) | 8 (34.8%) | 33 (50.8%) | |
| Race | ||||
| White | 27 (64.3%) | 15 (65.2%) | 42 (64.6%) | 0.800 |
| Black | 9 (21.4%) | 6 (26.1%) | 15 (23.1%) | |
| Other | 6 (14.3%) | 2 (8.7%) | 8 (12.3%) | |
| Diagnosis Group | ||||
| Hematologic Malignancy | 31 (73.8%) | 15 (65.2%) | 46 (70.8%) | 0.608 |
| Benign Hematologic Disease | 6 (14.3%) | 3 (13.0%) | 9 (13.8%) | |
| Solid Tumor | 5 (11.9%) | 5 (21.7%) | 10 (15.4%) | |
| Age at ICU Admission (y) | 14.5 [10.8] | 15.1 [10.1] | 14.9 [9.9] | 0.641 |
| HCT | ||||
| No | 24 (57.1%) | 10 (43.5%) | 34 (52.3%) | 0.313 |
| Yes | 18 (42.9%) | 13 (56.5%) | 31 (47.7%) | |
| Sepsis After ICU Admission | ||||
| No | 36 (85.7%) | 17 (73.9%) | 53 (81.5%) | 0.319 |
| Yes | 6 (14.3%) | 6 (26.1%) | 12 (18.5%) | |
| Vasopressor Use | ||||
| No | 23 (54.8%) | 3 (13.0%) | 26 (40.0%) | 0.001 * |
| Yes | 19 (45.2%) | 20 (87.0%) | 39 (60.0%) | |
| Death | ||||
| No | 35 (83.3%) | 16 (69.6%) | 51 (78.5%) | 0.221 |
| Yes | 7 (16.7%) | 7 (30.4%) | 14 (21.5%) | |
| Any Infection | ||||
| No | 16 (39.0%) | 4 (17.4%) | 20 (31.2%) | 0.095 |
| Yes | 25 (61.0%) | 19 (82.6%) | 44 (68.8%) | |
| Bacterial Infection | ||||
| No | 24 (58.5%) | 6 (26.1%) | 30 (46.9%) | 0.019 * |
| Yes | 17 (41.5%) | 17 (73.9%) | 34 (53.1%) | |
| Viral Infection | ||||
| No | 33 (80.5%) | 22 (95.7%) | 55 (85.9%) | 0.140 |
| Yes | 8 (19.5%) | 1 (4.3%) | 9 (14.1%) | |
| Fungal Infection | ||||
| No | 41 (100.0%) | 22 (95.7%) | 63 (98.4%) | 0.359 |
| Yes | 0 (0.0%) | 1 (4.3%) | 1 (1.6%) | |
| IMV | ||||
| No | 30 (73.2%) | 11 (47.8%) | 41 (64.1%) | 0.059 |
| Yes | 11 (26.8%) | 12 (52.2%) | 23 (35.9%) | |
| RRT | ||||
| No | 37 (88.1%) | 14 (60.9%) | 51 (78.5%) | 0.024 * |
| Yes | 5 (11.9%) | 9 (39.1%) | 14 (21.5%) | |
| Lactated Ringer’s | ||||
| No | 12 (28.6%) | 6 (26.1%) | 18 (27.7%) | 1.000 |
| Yes | 30 (71.4%) | 17 (73.9%) | 47 (72.3%) | |
| ICU Length of Stay (d) | 2.0 [10.0] | 7.0 [20.0] | 2.0 [15.0] | 0.024 * |
| Hospital Length of Stay (d) | 24.5 [36.0] | 33.0 [37.0] | 27.0 [37.5] | 0.029 * |
| Platelet Count (103/mm3) | 79.0 [119.0] | 17.0 [37.0] | 45.0 [104.0] | <0.001 * |
| C-Reactive Protein (mg/dL) | 7.7 [13.1] | 16.3 [19.1] | 11.2 [18.7] | 0.022 * |
| LDH (U/L) | 288.5 [310.0] | 363.0 [1615.0] | 314.0 [417.0] | 0.063 |
| Creatinine (mg/dL) | 0.5 [0.4] | 0.8 [0.9] | 0.5 [0.4] | 0.002 * |
| PIM2 | −3.0 [0.4] | −3.0 [1.8] | −3.0 [1.5] | 0.428 |
| PRISM3 | 5.5 [7.5] | 14.0 [14.0] | 8.0 [11.0] | 0.004 * |
| Vasopressor Use Log2-EASIX > 2.5 | Death Log2-EASIX > 3.5 | |
|---|---|---|
| OR (95% CI) p-value | 6.9 (1.7, 27.8) p = 0.007 | 2.1 (0.4, 10.7) p = 0.351 |
| Sensitivity | 77% | 57% |
| Specificity | 50% | 94% |
| Positive Predictive Value | 70% | 73% |
| Negative Predictive Value | 59% | 89% |
| Correctly Classified | 66% | 86% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elbahlawan, L.; Khiami, M.; Blackshear, C.; Ghafoor, S.; Schaller, A.; Johnson, S.; Maron, G.; Datta, R.; Qudeimat, A.; McArthur, J. Unraveling the Easix Score: Its Association with Vasopressor Need in Critically Ill Septic Pediatric Hematology–Oncology Patients. J. Clin. Med. 2025, 14, 7105. https://doi.org/10.3390/jcm14197105
Elbahlawan L, Khiami M, Blackshear C, Ghafoor S, Schaller A, Johnson S, Maron G, Datta R, Qudeimat A, McArthur J. Unraveling the Easix Score: Its Association with Vasopressor Need in Critically Ill Septic Pediatric Hematology–Oncology Patients. Journal of Clinical Medicine. 2025; 14(19):7105. https://doi.org/10.3390/jcm14197105
Chicago/Turabian StyleElbahlawan, Lama, Majd Khiami, Chad Blackshear, Saad Ghafoor, Alexandra Schaller, Sherry Johnson, Gabriela Maron, Raktima Datta, Amr Qudeimat, and Jennifer McArthur. 2025. "Unraveling the Easix Score: Its Association with Vasopressor Need in Critically Ill Septic Pediatric Hematology–Oncology Patients" Journal of Clinical Medicine 14, no. 19: 7105. https://doi.org/10.3390/jcm14197105
APA StyleElbahlawan, L., Khiami, M., Blackshear, C., Ghafoor, S., Schaller, A., Johnson, S., Maron, G., Datta, R., Qudeimat, A., & McArthur, J. (2025). Unraveling the Easix Score: Its Association with Vasopressor Need in Critically Ill Septic Pediatric Hematology–Oncology Patients. Journal of Clinical Medicine, 14(19), 7105. https://doi.org/10.3390/jcm14197105






