Perioperative Repercussions of Cannabis Use—Implications for GI Endoscopy Sedation
Abstract
1. Introduction
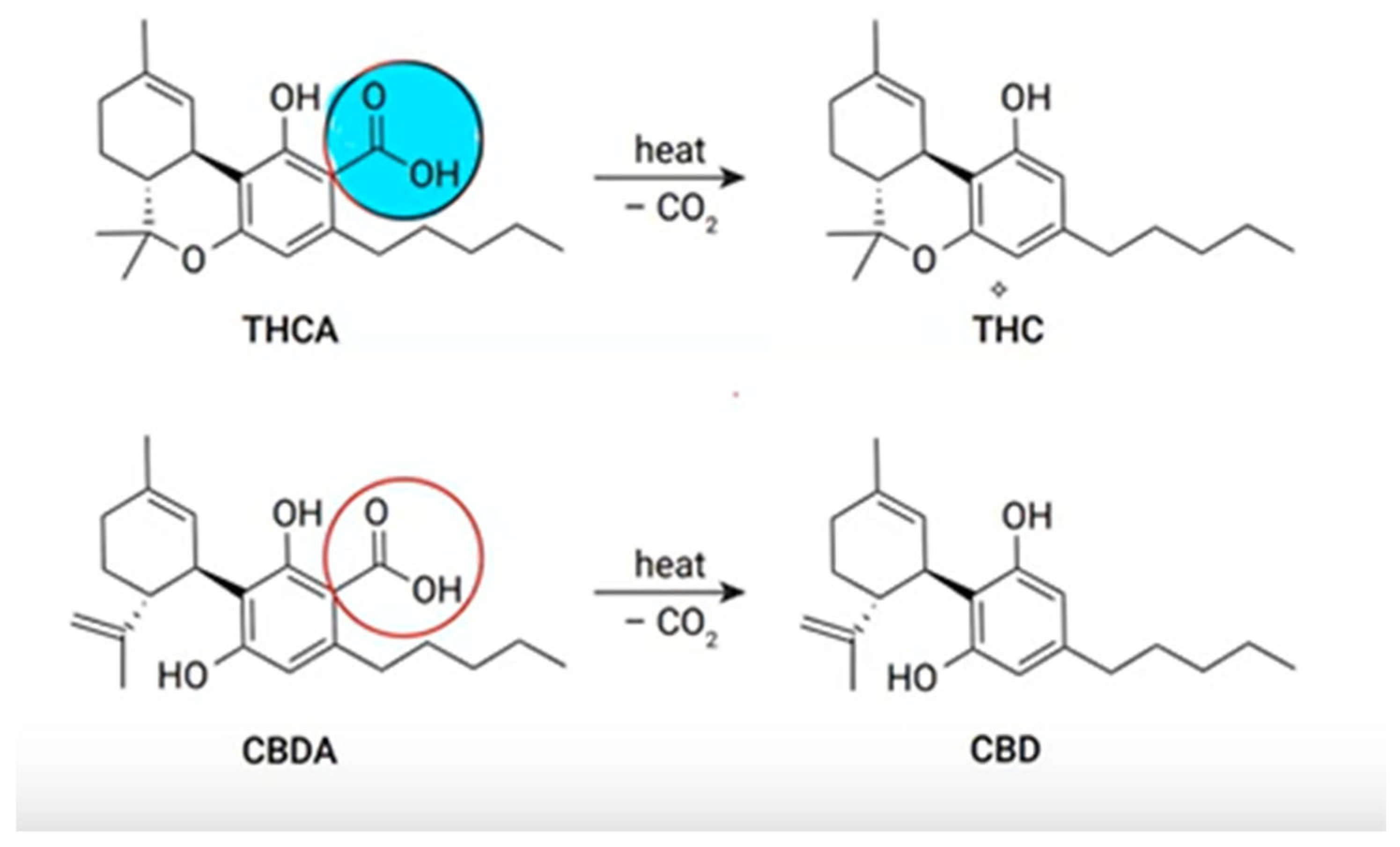
2. Chemistry of Cannabis and Their Products
3. Pharmacology
4. Extent of Marijuana Use in the USA
5. Clinical Uses
6. Sedation Management in Cannabis-Using Patients: Key Challenges
6.1. Acute Intoxication
6.2. Challenges with Sedation Administration
6.2.1. Sedation Requirements
6.2.2. Cardiovascular Adverse Events
6.2.3. Pulmonary Adverse Events
6.2.4. Gastric Emptying
6.2.5. Emergence from Anesthesia
6.2.6. Cannabinoid Hyperemesis Syndrome
6.2.7. Relevant Drug Interactions
7. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bodnar, R.J. Endogenous opiates and behavior: 2023. Peptides 2024, 179, 171268. [Google Scholar] [CrossRef]
- Sugiura, T.; Waku, K. Cannabinoid receptors and their endogenous ligands. J. Biochem. 2002, 132, 7–12. [Google Scholar] [CrossRef]
- Mackie, K. Cannabinoid receptors as therapeutic targets. Annu. Rev. Pharmacol. Toxicol. 2006, 46, 101–122. [Google Scholar] [CrossRef]
- What Are Cannabinoids? All About|Fundación CANNA: Scientific Studies and Cannabis Testing. Available online: https://www.fundacion-canna.es/en/cannabinoids (accessed on 30 May 2025).
- Cannabinoids—Alcohol and Drug Foundation. Available online: https://adf.org.au/drug-facts/cannabinoids/ (accessed on 31 May 2025).
- Cannabis (Marijuana) and Cannabinoids: What You Need To Know. NCCIH. Available online: https://www.nccih.nih.gov/health/cannabis-marijuana-and-cannabinoids-what-you-need-to-know (accessed on 31 May 2025).
- McGilveray, I.J. Pharmacokinetics of cannabinoids. Pain. Res. Manag. 2005, 10 (Suppl. A), 15A–22A. [Google Scholar] [CrossRef] [PubMed]
- Lunn, S.; Diaz, P.; O’Hearn, S.; Cahill, S.P.; Blake, A.; Narine, K.; Dyck, J.R.B. Human Pharmacokinetic Parameters of Orally Administered Δ9-Tetrahydrocannabinol Capsules Are Altered by Fed Versus Fasted Conditions and Sex Differences. Cannabis Cannabinoid Res. 2019, 4, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Lucas, C.J.; Galettis, P.; Schneider, J. The pharmacokinetics and the pharmacodynamics of cannabinoids. Br. J. Clin. Pharmacol. 2018, 84, 2477–2482. [Google Scholar] [CrossRef] [PubMed]
- ElSohly, M.A.; Stanford, D.F.; Harland, E.C.; Hikal, A.H.; Walker, L.A.; Little, T.L.; Rider, J.N.; Jones, A.B. Rectal bioavailability of delta-9-tetrahydrocannabinol from the hemisuccinate ester in monkeys. J. Pharm. Sci. 1991, 80, 942–945. [Google Scholar] [CrossRef]
- Massa, F.; Monory, K. Endocannabinoids and the gastrointestinal tract. J. Endocrinol. Invest. 2006, 29, 47–57. [Google Scholar]
- Oz, M.; Yang, K.-H.S.; Mahgoub, M.O. Effects of cannabinoids on ligand-gated ion channels. Front. Physiol. 2022, 13, 1041833. [Google Scholar] [CrossRef]
- Howlett, A.C.; Abood, M.E. CB1 and CB2 Receptor Pharmacology. Adv. Pharmacol. 2017, 80, 169–206. [Google Scholar] [CrossRef]
- Pintori, N.; Caria, F.; De Luca, M.A.; Miliano, C. THC and CBD: Villain versus Hero? Insights into Adolescent Exposure. Int. J. Mol. Sci. 2023, 24, 5251. [Google Scholar] [CrossRef]
- 2022 National Survey on Drug Use and Health (NSDUH) Releases|CBHSQ Data. Available online: https://www.samhsa.gov/data/data-we-collect/nsduh-national-survey-drug-use-and-health/national-releases/2022 (accessed on 2 June 2025).
- Quader, Z.S. Routes of Marijuana Use—Behavioral Risk Factor Surveillance System, 22 U.S. States and Two Territories, 2022. MMWR Morb. Mortal. Wkly. Rep. 2025, 74, 198–204. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, E.C.; Tsien, R.W.; Whalley, B.J.; Devinsky, O. Cannabinoids and Epilepsy. Neurotherapeutics 2015, 12, 747–768. [Google Scholar] [CrossRef]
- Sirbu, C.-A.; Georgescu, R.; Pleşa, F.C.; Paunescu, A.; Marilena Ţânţu, M.; Nicolae, A.C.; Caloianu, I.; Mitrica, M. Cannabis and Cannabinoids in Multiple Sclerosis: From Experimental Models to Clinical Practice-A Review. Am. J. Ther. 2023, 30, e220–e231. [Google Scholar] [CrossRef] [PubMed]
- Rosager, E.V.; Møller, C.; Sjögren, M. Treatment studies with cannabinoids in anorexia nervosa: A systematic review. Eat. Weight. Disord. Stud. Anorex. Bulim. Obes. 2021, 26, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Novack, G.D. Cannabinoids for treatment of glaucoma. Curr. Opin. Ophthalmol. 2016, 27, 146–150. [Google Scholar] [CrossRef]
- Braun, I.M.; Bohlke, K.; Abrams, D.I.; Anderson, H.; Balneaves, L.G.; Bar-Sela, G.; Bowles, D.W.; Chai, P.R.; Damani, A.; Gupta, A.; et al. Cannabis and Cannabinoids in Adults with Cancer: ASCO Guideline. J. Clin. Oncol. 2024, 42, 1575–1593. [Google Scholar] [CrossRef]
- Urbi, B.; Corbett, J.; Hughes, I.; Owusu, M.A.; Thorning, S.; Broadley, S.A.; Sabet, A.; Heshmat, S. Effects of Cannabis in Parkinson’s Disease: A Systematic Review and Meta-Analysis. J. Park. Dis. 2022, 12, 495–508. [Google Scholar] [CrossRef]
- Akinyemi, E.; Randhawa, G.; Longoria, V.; Zeine, R. Medical Marijuana Effects in Movement Disorders, Focus on Huntington Disease; A Literature Review. J. Pharm. Pharm. Sci. 2020, 23, 389–395. [Google Scholar] [CrossRef]
- Cao, C.; Li, Y.; Liu, H.; Bai, G.; Mayl, J.; Lin, X.; Sutherland, K.; Nabar, N.; Cai, J. The potential therapeutic effects of THC on Alzheimer’s disease. J. Alzheimer’s Dis. 2014, 42, 973–984. [Google Scholar] [CrossRef]
- Mosley, P.E.; Webb, L.; Suraev, A.; Hingston, L.; Turnbull, T.; Foster, K.; Ballard, E.; Gomes, L.; Mohan, A.; Sachdev, P.S.; et al. Tetrahydrocannabinol and Cannabidiol in Tourette Syndrome. NEJM Evid. 2023, 2, EVIDoa2300012. [Google Scholar] [CrossRef]
- Skelley, J.W.; Deas, C.M.; Curren, Z.; Ennis, J. Use of cannabidiol in anxiety and anxiety-related disorders. J. Am. Pharm. Assoc. 2020, 60, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Paulus, V.; Billieux, J.; Benyamina, A.; Karila, L. Cannabidiol in the context of substance use disorder treatment: A systematic review. Addict. Behav. 2022, 132, 107360. [Google Scholar] [CrossRef] [PubMed]
- Davies, C.; Bhattacharyya, S. Cannabidiol as a potential treatment for psychosis. Ther. Adv. Psychopharmacol. 2019, 9, 2045125319881916. [Google Scholar] [CrossRef] [PubMed]
- Kluger, B.M.; Huang, A.P.; Miyasaki, J.M. Cannabinoids in movement disorders. Park. Relat. Disord. 2022, 102, 124–130. [Google Scholar] [CrossRef]
- Mohammed, S.Y.M.; Leis, K.; Mercado, R.E.; Castillo, M.M.S.; Miranda, K.J.; Carandang, R.R. Effectiveness of Cannabidiol to Manage Chronic Pain: A Systematic Review. Pain. Manag. Nurs. 2024, 25, e76–e86. [Google Scholar] [CrossRef]
- Shah, S.; Schwenk, E.S.; Sondekoppam, R.V.; Clarke, H.; Zakowski, M.; Rzasa-Lynn, R.S.; Yeung, B.; Nicholson, K.; Schwartz, G.; Hooten, W.M.; et al. ASRA Pain Medicine consensus guidelines on the management of the perioperative patient on cannabis and cannabinoids. Reg. Anesth. Pain. Med. 2023, 48, 97–117. [Google Scholar] [CrossRef]
- Schmid, Y.; Galicia, M.; Vogt, S.B.; Liechti, M.E.; Burillo-Putze, G.; Dargan, P.I.; Dines, A.M.; Giraudon, I.; Heyerdahl, F.; Hovda, K.E.; et al. Differences in clinical features associated with cannabis intoxication in presentations to European emergency departments according to patient age and sex. Clin. Toxicol. 2022, 60, 912–919. [Google Scholar] [CrossRef]
- Marcotte, T.D.; Umlauf, A.; Grelotti, D.J.; Sones, E.G.; Mastropietro, K.F.; Suhandynata, R.T.; Huestis, M.A.; Grant, I.; Fitzgerald, R.L. Evaluation of Field Sobriety Tests for Identifying Drivers Under the Influence of Cannabis. JAMA Psychiatry 2023, 80, 914–923. [Google Scholar] [CrossRef]
- Vandrey, R.; Herrmann, E.S.; Mitchell, J.M.; Bigelow, G.E.; Flegel, R.; LoDico, C.; Cone, E.J. Pharmacokinetic Profile of Oral Cannabis in Humans: Blood and Oral Fluid Disposition and Relation to Pharmacodynamic Outcomes. J. Anal. Toxicol. 2017, 41, 83–99. [Google Scholar] [CrossRef]
- Kesner, A.J.; Lovinger, D.M. Cannabis use, abuse, and withdrawal: Cannabinergic mechanisms, clinical, and preclinical findings. J. Neurochem. 2021, 157, 1674–1696. [Google Scholar] [CrossRef] [PubMed]
- Imasogie, N.; Rose, R.V.; Wilson, A. High quantities: Evaluating the association between cannabis use and propofol anesthesia during endoscopy. PLoS ONE 2021, 16, e0248062. [Google Scholar] [CrossRef] [PubMed]
- Ripperger, D.; Atte, A.; Ritto, F. Cannabis Users Require More Anesthetic Agents for General Anesthesia in Ambulatory Oral and Maxillofacial Surgery Procedures. J. Oral Maxillofac. Surg. 2023, 81, 1460–1465. [Google Scholar] [CrossRef]
- Flisberg, P.; Paech, M.J.; Shah, T.; Ledowski, T.; Kurowski, I.; Parsons, R. Induction dose of propofol in patients using cannabis. Eur. J. Anaesthesiol. 2009, 26, 192–195. [Google Scholar] [CrossRef]
- Bornemann-Cimenti, H.; Lang-Illievich, K.; Neuwersch-Sommeregger, S.; Lang, J.; Danninger, T.; Hammer, S.; Szilagyi, I.-S.; Klivinyi, C. Effect of cannabinoid consumption on propofol dosage: A systematic review and meta-analysis. Br. J. Anaesth. 2025, 134, 875–878. [Google Scholar] [CrossRef]
- Baker, M.B.; Binda, D.D.; Nozari, A.; Kennedy, J.M.; Dienes, E.; Baker, W.E. Quantitative Analysis of Propofol Dosage in Cannabis Users: A Systematic Review and Meta-Analysis. J. Clin. Med. 2025, 14, 858. [Google Scholar] [CrossRef]
- Reed, C. Cannabis Users Require More Sedation for Endoscopy. DDW. 21 May 2022. Available online: https://ddw.org/cannabis-users-require-more-sedation-for-endoscopy/ (accessed on 4 June 2025).
- King, D.D.; Gill, C.J.; Cadieux, C.S.; Singh, N. The role of stigma in cannabis use disclosure: An exploratory study. Harm Reduct. J. 2024, 21, 21. [Google Scholar] [CrossRef]
- Jeffers, A.M.; Glantz, S.; Byers, A.L.; Keyhani, S. Association of Cannabis Use with Cardiovascular Outcomes Among US Adults. J. Am. Heart Assoc. 2024, 13, e030178. [Google Scholar] [CrossRef]
- Goel, A.; McGuinness, B.; Jivraj, N.K.; Wijeysundera, D.N.; Mittleman, M.A.; Bateman, B.T.; Clarke, H.; Kotra, L.P.; Ladha, K.S. Cannabis Use Disorder and Perioperative Outcomes in Major Elective Surgeries: A Retrospective Cohort Analysis. Anesthesiology 2020, 132, 625–635. [Google Scholar] [CrossRef] [PubMed]
- Mukamal, K.J.; Maclure, M.; Muller, J.E.; Mittleman, M.A. An Exploratory Prospective Study of Marijuana Use and Mortality Following Acute Myocardial Infarction. Am. Heart J. 2008, 155, 465–470. [Google Scholar] [CrossRef]
- Mittleman, M.A.; Lewis, R.A.; Maclure, M.; Sherwood, J.B.; Muller, J.E. Triggering myocardial infarction by marijuana. Circulation 2001, 103, 2805–2809. [Google Scholar] [CrossRef]
- Ghasemiesfe, M.; Ravi, D.; Casino, T.; Korenstein, D.; Keyhani, S. Acute Cardiovascular Effects of Marijuana Use. J. Gen. Intern. Med. 2020, 35, 969–974. [Google Scholar] [CrossRef] [PubMed]
- Ravi, D.; Ghasemiesfe, M.; Korenstein, D.; Cascino, T.; Keyhani, S. Associations Between Marijuana Use and Cardiovascular Risk Factors and Outcomes: A Systematic Review. Ann. Intern. Med. 2018, 168, 187–194. [Google Scholar] [CrossRef] [PubMed]
- van Amsterdam, J.; van den Brink, W. Cannabis Use Variations and Myocardial Infarction: A Systematic Review. J. Clin. Med. 2024, 13, 5620. [Google Scholar] [CrossRef]
- Chambers, J.; Keyhani, S.; Ling, P.M.; Hoggatt, K.J.; Hasin, D.; Nguyen, N.; Woods, A.; Ryder, A.; Cohen, B.E. Perceptions of Safety of Daily Cannabis vs. Tobacco Smoking and Secondhand Smoke Exposure, 2017–2021. JAMA Netw. Open 2023, 6, e2328691. [Google Scholar] [CrossRef]
- Tashkin, D.P. Smoked marijuana as a cause of lung injury. Monaldi Arch. Chest Dis. 2005, 63, 93–100. [Google Scholar] [CrossRef]
- Janssen, F.; Braun, M.; Dröge, J.; Brüggmann, D.; Groneberg, D.A. Comparison Between Smoked Tobacco and Medical Cannabis Cigarettes Concerning Particulate Matter. Cannabis Cannabinoid Res. 2024, 9, 1492–1499. [Google Scholar] [CrossRef]
- Tan, W.C.; Lo, C.; Jong, A.; Xing, L.; FitzGerald, M.J.; Vollmer, W.M.; Buist, S.A.; Sin, D.D. Marijuana and chronic obstructive lung disease: A population-based study. CMAJ Can. Med. Assoc. J. 2009, 180, 814–820. [Google Scholar] [CrossRef] [PubMed]
- Tan, C.; Hatam, N.; Treasure, T. Bullous disease of the lung and cannabis smoking: Insufficient evidence for a causative link. J. R. Soc. Med. 2006, 99, 77–80. [Google Scholar] [CrossRef]
- Lehrer, S.; Rheinstein, P.H. Association of cannabis with chronic obstructive pulmonary disease and COVID--19 infection. Chronic Dis. Transl. Med. 2022, 8, 238–241. [Google Scholar] [CrossRef]
- Barjaktarevic, I.; Cooper, C.B.; Shing, T.; Buhr, R.G.; Hoffman, E.A.; Woodruff, P.G.; Drummond, M.B.; Kanner, R.E.; Han, M.K.; Hansel, N.N.; et al. Impact of Marijuana Smoking on COPD Progression in a Cohort of Middle-Aged and Older Persons. Chronic Obs. Pulm. Dis. 2023, 10, 234–247. [Google Scholar] [CrossRef]
- Marijuana and Surgery. ACS. Available online: https://www.facs.org/for-patients/preparing-for-surgery/marijuana-and-surgery/ (accessed on 10 June 2025).
- Alexander, J.C.; Joshi, G.P. A review of the anesthetic implications of marijuana use. Proc. Bayl. Univ. Med. Cent. 2019, 32, 364–371. [Google Scholar] [CrossRef]
- Papatheodorou, S.I.; Buettner, H.; Rice, M.B.; Mittleman, M.A. Recent Marijuana Use and Associations with Exhaled Nitric Oxide and Pulmonary Function in Adults in the United States. Chest 2016, 149, 1428–1435. [Google Scholar] [CrossRef]
- Crowley, K.; Kiraga, Ł.; Miszczuk, E.; Skiba, S.; Banach, J.; Latek, U.; Mendel, M.; Chłopecka, M. Effects of Cannabinoids on Intestinal Motility, Barrier Permeability, and Therapeutic Potential in Gastrointestinal Diseases. Int. J. Mol. Sci. 2024, 25, 6682. [Google Scholar] [CrossRef]
- McCallum, R.W.; Soykan, I.; Sridhar, K.R.; Ricci, D.A.; Lange, R.C.; Plankey, M.W. Delta-9-tetrahydrocannabinol delays the gastric emptying of solid food in humans: A double-blind, randomized study. Aliment. Pharmacol. Ther. 1999, 13, 77–80. [Google Scholar] [CrossRef]
- Casajuana Kögel, C.; Balcells-Olivero, M.M.; López-Pelayo, H.; Miquel, L.; Teixidó, L.; Colom, J.; Nutt, D.J.; Rehm, J.; Gual, A. The Standard Joint Unit. Drug Alcohol. Depend. 2017, 176, 109–116. [Google Scholar] [CrossRef]
- Cammarano, C.A.; Villaluz, J.E. A Reason to Rethink Fasting Guidelines? Marijuana-Induced Gastroparesis and the Implications for Aspiration Risk in the Nil Per Os (NPO) Patient: A Case Report. Am. J. Case Rep. 2021, 22, e934187. [Google Scholar] [CrossRef] [PubMed]
- Camilleri, M. Cannabinoids and Gastrointestinal Motility: Pharmacology, Clinical Effects and Potential Therapeutics in Humans. Neurogastroenterol. Motil. 2018, 30, e13370. [Google Scholar] [CrossRef] [PubMed]
- Amoroso, K.; Chiapparelli, E.; Zhu, J.; Guven, A.E.; Shue, J.; Sama, A.A.; Girardi, F.P.; Cammisa, F.P.; Hughes, A.P.; Soffin, E.M. The Association Between Preoperative Cannabis Use and Anxiety, Pain Scores and Opioid Consumption in Patients Undergoing Spinal Fusion: A Retrospective Cohort Study. Glob. Spine J. 2025, 21925682251327986. [Google Scholar] [CrossRef] [PubMed]
- Echeverria-Villalobos, M.; Fabian, C.A.; Mitchell, J.G.; Mazzotta, E.; Fiorda Diaz, J.C.; Noon, K.; Weaver, T.E. Cannabinoids and General Anesthetics: Revisiting Molecular Mechanisms of Their Pharmacological Interactions. Anesth. Analg. 2025, 140, 1401–1413. [Google Scholar] [CrossRef] [PubMed]
- Suhre, W.; O’Reilly-Shah, V.; Van Cleve, W. Cannabis use is associated with a small increase in the risk of postoperative nausea and vomiting: A retrospective machine-learning causal analysis. BMC Anesth. 2020, 20, 115. [Google Scholar] [CrossRef]
- Bathula, P.P.; Maciver, M.B. Cannabinoids in Treating Chemotherapy-Induced Nausea and Vomiting, Cancer-Associated Pain, and Tumor Growth. Int. J. Mol. Sci. 2023, 25, 74. [Google Scholar] [CrossRef]
- Abrams, D.I. Cannabis, Cannabinoids and Cannabis-Based Medicines in Cancer Care. Integr. Cancer Ther. 2022, 21, 1–11. [Google Scholar] [CrossRef]
- Tramèr, M.R.; Carroll, D.; Campbell, F.A.; Reynolds, D.J.M.; Moore, R.A.; McQuay, H.J. Cannabinoids for control of chemotherapy induced nausea and vomiting: Quantitative systematic review. BMJ 2001, 323, 16. [Google Scholar] [CrossRef]
- Sankar-Maharaj, S.; Chen, D.; Hariharan, S. Postoperative Shivering Among Cannabis Users at a Public Hospital in Trinidad, West Indies. J. Perianesth Nurs. 2018, 33, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Fleming, J.E.; Lockwood, S. Cannabinoid Hyperemesis Syndrome. Fed. Pr. 2017, 34, 33–36. [Google Scholar]
- Galli, J.A.; Sawaya, R.A.; Friedenberg, F.K. Cannabinoid hyperemesis syndrome. Curr. Drug Abus. Rev. 2011, 4, 241–249. [Google Scholar] [CrossRef] [PubMed]
- Costales, B.; Lu, Y.; Young-Wolff, K.C.; Cotton, D.M.; Campbell, C.I.; Iturralde, E.; Sterling, S.A. Prevalence and trends of suspected cannabinoid hyperemesis syndrome over an 11-year period in Northern California: An electronic health record study. Drug Alcohol. Depend. 2024, 263, 112418. [Google Scholar] [CrossRef] [PubMed]
- Habboushe, J.; Rubin, A.; Liu, H.; Hoffman, R.S. The Prevalence of Cannabinoid Hyperemesis Syndrome Among Regular Marijuana Smokers in an Urban Public Hospital. Basic Clin. Pharmacol. Toxicol. 2018, 122, 660–662. [Google Scholar] [CrossRef]
- Soh, J.; Kim, Y.; Shen, J.; Kang, M.; Chaudhry, S.; Chung, T.H.; Kim, S.H.; Hwang, Y.; Lim, D.; Khattak, A.; et al. Trends of emergency department visits for cannabinoid hyperemesis syndrome in Nevada: An interrupted time series analysis. PLoS ONE 2024, 19, e0303205. [Google Scholar] [CrossRef]
- Damkier, P.; Lassen, D.; Christensen, M.M.H.; Madsen, K.G.; Hellfritzsch, M.; Pottegård, A. Interaction between warfarin and cannabis. Basic. Clin. Pharmacol. Toxicol. 2019, 124, 28–31. [Google Scholar] [CrossRef]
- Yamreudeewong, W.; Wong, H.K.; Brausch, L.M.; Pulley, K.R. Probable interaction between warfarin and marijuana smoking. Ann. Pharmacother. 2009, 43, 1347–1353. [Google Scholar] [CrossRef] [PubMed]
- Paduch, M.; Thomason, A.R. Potential Drug Interactions Between Cannabinoids and Its Derivatives and Oral Anticoagulants. Hosp. Pharm. 2022, 57, 188–192. [Google Scholar] [CrossRef] [PubMed]
- Greger, J.; Bates, V.; Mechtler, L.; Gengo, F. A Review of Cannabis and Interactions with Anticoagulant and Antiplatelet Agents. J. Clin. Pharmacol. 2020, 60, 432–438. [Google Scholar] [CrossRef] [PubMed]
| Attribute | Implication/s | References | Notes |
|---|---|---|---|
| Sedation requirements | Increased requirements for propofol, midazolam, ketamine, and fentanyl Greater oxygen requirements, increased need for bag–mask ventilation with oral airway insertion Higher propofol dose to achieve successful LMA insertion | [36,37,38,39,40,41,42] | Related to airway irritation (LMA insertion), altered central nervous system sensitivity and receptor-level adaptations. Related to the amount, duration, frequency, and route of cannabis intake |
| Cardiovascular adverse events | Increased risk of adverse cardiovascular events including CHD, MI. Stroke; related to amount and duration of exposure. Risk of triggering a myocardial infarction elevated 4.8-fold within one hour of smoking marijuana compared with periods of nonuse. | [43,44,45,46,47,48,49] | Supporting evidence is mainly retrospective. Currently insufficient evidence to cancel or delay a procedure based on history of cannabis use |
| Pulmonary adverse events | Concurrent use of marijuana and tobacco associated with a higher risk of respiratory symptoms and COPD, after adjusting for age, asthma, and comorbidities, compared with tobacco smoking alone. Long-term effects include chronic cough, sputum production, histopathologic evidence of widespread airway inflammation and injury | [50,51,52,53,54,55,56,57,58,59] | A definitive cause effect relationship between cannabis smoking and COPD is lacking |
| Gastric emptying | THC significantly delays gastric emptying of solid food compared with placebo. | [60,61,62,63,64] | Insufficient evidence to make definitive recommendations |
| Emergence from anesthesia | Daily cannabis users often experience higher postoperative pain scores. In those showing features of acute cannabis intoxication, emergence is delayed and less smooth. Postoperative shivering is more common among cannabis users. | [65,66,67,68,69,70,71] | Supporting evidence is mainly retrospective |
| Cannabinoid hyperemesis syndrome | Mainly seen in ER. A history of CHS indicates chronic cannabis use. CHS might be an indication for EGD. | [72,73,74,75,76] | CHS does not respond to standard antiemetics |
| Drug Interactions | THC inhibits the CYP2C9-mediated metabolism of warfarin. Cannabidiol inhibits an isoenzyme responsible for the transformation of clopidogrel to its active thiol metabolite | [77,78,79,80] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goudra, B.; Green, M. Perioperative Repercussions of Cannabis Use—Implications for GI Endoscopy Sedation. J. Clin. Med. 2025, 14, 7028. https://doi.org/10.3390/jcm14197028
Goudra B, Green M. Perioperative Repercussions of Cannabis Use—Implications for GI Endoscopy Sedation. Journal of Clinical Medicine. 2025; 14(19):7028. https://doi.org/10.3390/jcm14197028
Chicago/Turabian StyleGoudra, Basavana, and Michael Green. 2025. "Perioperative Repercussions of Cannabis Use—Implications for GI Endoscopy Sedation" Journal of Clinical Medicine 14, no. 19: 7028. https://doi.org/10.3390/jcm14197028
APA StyleGoudra, B., & Green, M. (2025). Perioperative Repercussions of Cannabis Use—Implications for GI Endoscopy Sedation. Journal of Clinical Medicine, 14(19), 7028. https://doi.org/10.3390/jcm14197028







