Long-Term Stability and Histologic Evaluation of Orthodontically Driven Osteogenesis (ODO): A Preliminary Retrospective Study
Abstract
1. Introduction
1.1. Periodontally Accelerated Osteogenic Orthodontics
1.2. Orthodontically Driven Osteogenesis
1.3. Rationale and Study Objectives
2. Materials and Methods
2.1. Study Design
2.2. Surgical Protocol
2.3. Orthodontic Protocol
- Initial assessment and diagnostic workflow. Following a thorough clinical evaluation, comprehensive diagnostic records were obtained. These included digital scans of the dental arches, standardized intraoral and extraoral photographs, and radiographic documentation consisting of both panoramic (orthopantomography) and lateral cephalometric radiographs. Based on these data, a detailed analysis of the malocclusion was performed, and a virtual three-dimensional treatment simulation was generated using the ClinCheck® Pro 6.0 software (Align Technology, San Jose, CA, USA). This digital setup allowed for precise visualization of tooth movement, prediction of occlusal outcomes, and assessment of arch form changes prior to the surgical phase.
- Treatment planning with the Invisalign® Comprehensive package—The “Comprehensive” aligner system (Align Technology, San Jose, CA, USA) was selected, as it provides flexibility for multi-phase treatments and the possibility of refinements when required. The planned orthodontic movements included dental arch expansion and coordination aimed at resolving crowding and achieving proper arch form alignment. The treatment protocol deliberately excluded interproximal enamel reduction (IPR) and tooth extractions, thereby favoring a non-invasive and expansion-based strategy consistent with the regenerative potential induced by ODO.
- Aligner wear protocol and compliance instructions—Patients were instructed to wear their aligners for 20–22 h per day, removing them only during meals and oral hygiene procedures. Aligner changes were scheduled on a 7-day basis to ensure a continuous and controlled force application, harmonized with the accelerated bone remodeling process induced by the surgical procedure. On average, each patient required approximately 30 aligners per arch to complete the active orthodontic phase. Patient adherence to the prescribed wear time was emphasized as a critical factor for the success of treatment, especially in the context of surgically accelerated orthodontic tooth movement.
- Retention strategy—Following completion of the active orthodontic therapy, a retention phase was implemented to maintain the achieved results and prevent relapse. Each patient was provided with a vacuum-formed retainer (VFR) tailored to their post-treatment dental arches. Patients were instructed to wear the retainers nightly on a long-term basis. This retention approach was chosen for its effectiveness, comfort, and minimal impact on oral hygiene, ensuring stability of the orthodontic results obtained after ODO.
2.4. Radiological Evaluation
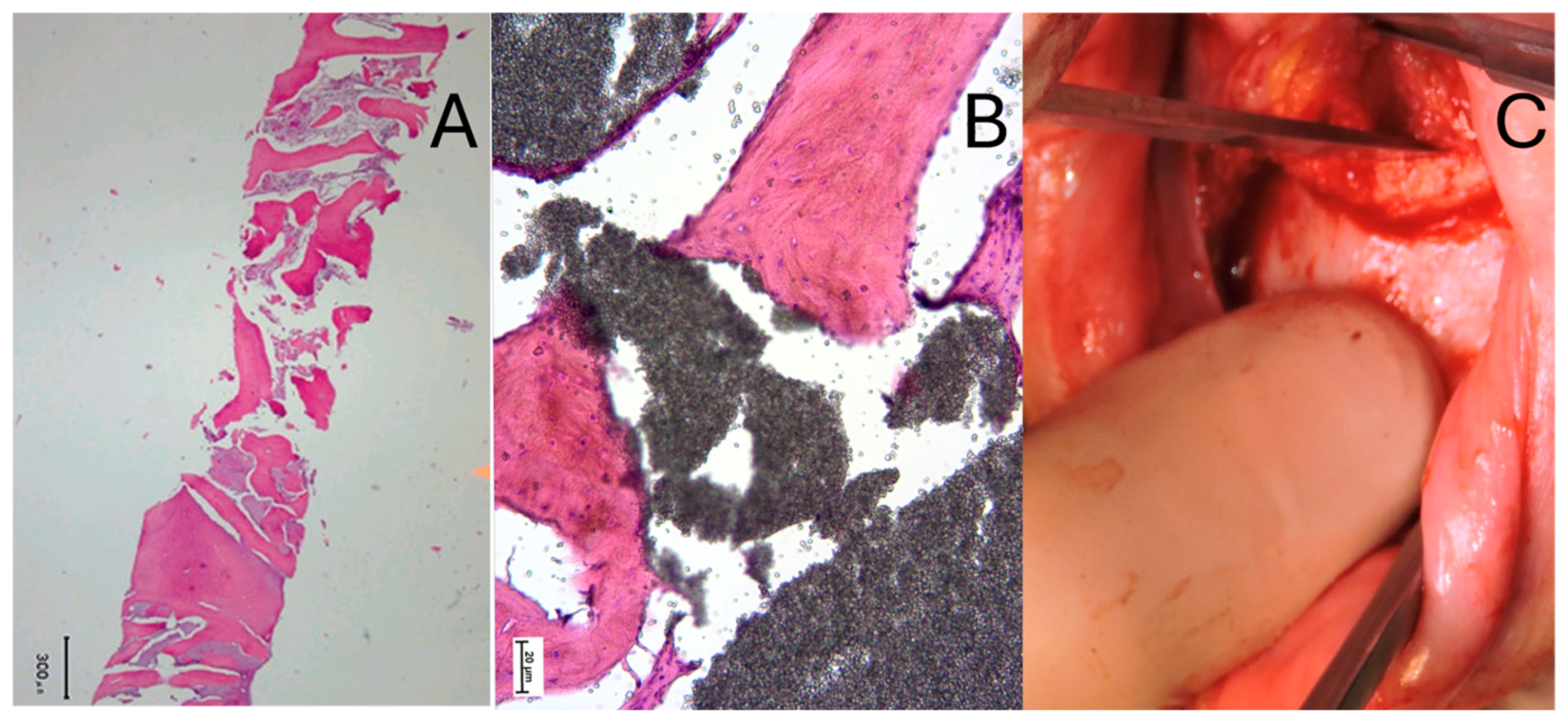
2.5. Histological Evaluation
3. Results
3.1. Radiological Outcomes
3.2. Histological Findings
4. Discussion
4.1. Periodontal Effects of Orthodontic Treatment
4.2. Insights from Orthodontically Driven Osteogenesis
4.3. Limitations and Strengths
4.4. Future Directions and Clinical Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Uzuner, F.D.; Darendeliler, N. Dentoalveolar surgery techniques combined with orthodontic treatment: A literature review. Eur. J. Dent. 2013, 7, 257–265. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wilcko, M.T.; Wilcko, W.M.; Bissada, N.F. An evidence-based analysis of periodontally accelerated orthodontic and osteogenic techniques: A synthesis of scientific perspective. Semin. Orthod. 2008, 14, 305–316. [Google Scholar] [CrossRef]
- Alsino, H.I.; Hajeer, M.Y.; Burhan, A.S.; Alkhouri, I.; Darwich, K. The Effectiveness of Periodontally Accelerated Osteogenic Orthodontics (PAOO) in Accelerating Tooth Movement and Supporting Alveolar Bone Thickness During Orthodontic Treatment: A Systematic Review. Cureus 2022, 14, e24985. [Google Scholar] [CrossRef] [PubMed]
- Al-Khalifa, K.S.; Baeshen, H.A. Micro-osteoperforations and Its Effect on the Rate of Tooth Movement: A Systematic Review. Eur. J. Dent. 2021, 15, 158–167. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kim, S.H.; Kim, I.; Jeong, D.M.; Chung, K.R.; Zadeh, H. Corticotomy-assisted decompensation for augmentation of the mandibular anterior ridge. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 720–731. [Google Scholar] [CrossRef]
- Bondemark, L. Interdental bone changes after orthodontic treatment: A 5-year longitudinal study. Am. J. Orthod. Dentofac. Orthop. 1998, 114, 25–31. [Google Scholar] [CrossRef]
- Janson, G.; Bombonatti, R.; Henriques, J.F. Comparative radiographic evaluation of the alveolar bone crest after orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 157–164. [Google Scholar] [CrossRef]
- Wang, B.; Shen, G.; Fang, B.; Yu, H.; Wu, Y. Augmented corticotomy-assisted presurgical orthodontics of class III malocclusions: A cephalometric and cone-beam computed tomography study. J. Craniofac. Surg. 2013, 24, 1886–1890. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, A.A.; Kolte, A.P.; Kolte, R.A.; Vaswani, V.; Shenoy, U.; Rathi, P. Comparative CBCT analysis of the changes in buccal bone morphology after corticotomy and micro-osteoperforations assisted orthodontic treatment—Case series with a split mouth design. Saudi Dent. J. 2019, 31, 58–65. [Google Scholar] [CrossRef]
- Parfitt, A.M.; Drezner, M.K.; Glorieux, F.H.; Kanis, J.A.; Malluche, H.; Meunier, P.J.; Ott, S.M.; Recker, R.R. Bone histomorphometry: Standardization of nomenclature, symbols, and units. Report of the ASBMR Histomorphometry Nomenclature Committee. J. Bone Miner Res. 1987, 2, 595–610. [Google Scholar] [CrossRef]
- Brugnami, F.; Caiazzo, A.; Meuli, S. Orthodontically Driven Osteogenesis, 2nd ed.; Wiley-Blackwell: Hoboken, NJ, USA, 2024; ISBN 978-1-119-70056-2. [Google Scholar]
- Brugnami, F.; Caiazzo, A.; Mehra, P. Tunnel Regenerative Corticotomy (TURC): A modified approach in surgically-assisted orthodontics. J. Oral. Biol. Craniofac. Res. 2021, 11, 63–65. [Google Scholar] [CrossRef] [PubMed]
- Lund, H.; Gröndahl, K.; Gröndahl, H.G. Cone beam computed tomography evaluations of marginal alveolar bone before and after orthodontic treatment combined with premolar extractions. Eur. J. Oral Sci. 2012, 120, 201–211. [Google Scholar] [CrossRef] [PubMed]
- Renkema, A.M.; Fudalej, P.S.; Renkema, A.A. Gingival labial recessions in orthodontically treated and untreated individuals: A case—Control study. J. Clin. Periodontol. 2013, 40, 631–639. [Google Scholar] [CrossRef] [PubMed]
- Staufer, K.; Landmesser, H. Effects of crowding in the lower anterior segment- a risk evaluation depending upon the degree of crowding. J. Orofac. Orthop. 2004, 65, 13–25. [Google Scholar] [CrossRef]
- Sarikaya, S.; Haydar, B.; Ciğer, S.; Ariyürek, M. Changes in alveolar bone thickness due to retraction of anterior teeth. Am. J. Orthod. Dentofac. Orthop. 2002, 122, 15–26. [Google Scholar] [CrossRef]
- Hollender, L.; Rönnerman, A.; Thilander, B. Root resorption, marginal bone support and clinical crown length in orthodontically treated patients. Eur. J. Orthod. 1980, 2, 197–205. [Google Scholar] [CrossRef]
- Choi, Y.J.; Chung, C.J.; Kim, K.H. Periodontal consequences of mandibular incisor proclination during presurgical orthodontic treatment in Class III malocclusion patients. Angle Orthod. 2015, 85, 427–433. [Google Scholar] [CrossRef]
- Fuhrmann, R. Three-dimensional interpretation of periodontal lesions and remodeling during orthodontic treatment. Part. III. J. Orofac. Orthop. 1996, 57, 224–237. [Google Scholar] [CrossRef]
- Apalimova, A.; Roselló, À.; Jané-Salas, E.; Arranz-Obispo, C.; Marí-Roig, A.; López-López, J. Corticotomy in orthodontic treatment: Systematic review. Heliyon 2020, 6, e04013. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chen, Z.; Zhou, H.; Zhang, K.; Wang, X.; Zhong, L.; Hou, Y.; Chen, Y. The clinical efficacy of periodontally accelerated osteogenic orthodontics in patients with bone fenestration and dehiscence: A retrospective study. Head. Face Med. 2022, 18, 40. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jiang, J.; Wu, J.; Yu, W.; Yu, J.; Xiong, Q.; Liu, D.; Xiong, Z.; Feng, J.; Xuan, D. Comparative evaluation of periodontally accelerated osteogenic orthodontics (PAOO) versus traditional camouflage orthodontic treatment in adult patients with skeletal class III malocclusion. BMC Oral Health 2024, 24, 1479. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mandelaris, G.A.; Neiva, R.; Chambrone, L. Cone-Beam Computed Tomography and Interdisciplinary Dentofacial Therapy: An American Academy of Periodontology Best Evidence Review Focusing on Risk Assessment of the Dentoalveolar Bone Changes Influenced by Tooth Movement. J. Periodontol. 2017, 88, 960–977. [Google Scholar] [CrossRef]
- Picanço, P.R.; Valarelli, F.P.; Cançado, R.H.; de Freitas, K.M.; Picanço, G.V. Comparison of the changes of alveolar bone thickness in maxillary incisor area in extraction and non-extraction cases: Computerized tomography evaluation. Dent. Press. J. Orthod. 2013, 18, 91–98. [Google Scholar] [CrossRef]
- Engelking, G.; Zachrisson, B.U. Effects of incisor repositioning on monkey periodontium after expansion through the cortical plate. Am. J. Orthop. 1982, 82, 23–32. [Google Scholar] [CrossRef]
- Bhattacharya, P.; Bhattacharya, H.; Anjum, A.; Bhandari, R.; Agarwal, D.K.; Gupta, A.; Ansar, J. Assessment of Corticotomy Facilitated Tooth Movement and Changes in Alveolar Bone Thickness—A CT Scan Study. J. Clin. Diagn. Res. 2014, 8, ZC26-30. [Google Scholar]

| Distance from CEJ | 3 mm | 5 mm | 7 mm | |||
|---|---|---|---|---|---|---|
| Time | T1 | T2 | T1 | T2 | T1 | T2 |
| Measurements (mm) | 1.93 | 1.91 | 2.15 | 2.14 | 3.19 | 3.16 |
| Mean (mm) | 0.55 | 0.53 | 0.62 | 0.63 | 0.86 | 0.86 |
| (±Standard deviation) | 0.88 | 0.88 | 0.95 | 0.95 | 0.89 | 0.89 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brugnami, F.; Meuli, S.; Ventura, V.; Gentile, D. Long-Term Stability and Histologic Evaluation of Orthodontically Driven Osteogenesis (ODO): A Preliminary Retrospective Study. J. Clin. Med. 2025, 14, 6896. https://doi.org/10.3390/jcm14196896
Brugnami F, Meuli S, Ventura V, Gentile D. Long-Term Stability and Histologic Evaluation of Orthodontically Driven Osteogenesis (ODO): A Preliminary Retrospective Study. Journal of Clinical Medicine. 2025; 14(19):6896. https://doi.org/10.3390/jcm14196896
Chicago/Turabian StyleBrugnami, Federico, Simonetta Meuli, Valentina Ventura, and Davide Gentile. 2025. "Long-Term Stability and Histologic Evaluation of Orthodontically Driven Osteogenesis (ODO): A Preliminary Retrospective Study" Journal of Clinical Medicine 14, no. 19: 6896. https://doi.org/10.3390/jcm14196896
APA StyleBrugnami, F., Meuli, S., Ventura, V., & Gentile, D. (2025). Long-Term Stability and Histologic Evaluation of Orthodontically Driven Osteogenesis (ODO): A Preliminary Retrospective Study. Journal of Clinical Medicine, 14(19), 6896. https://doi.org/10.3390/jcm14196896






