Comparison of Radiographic Stress Views in Detecting Scapholunate Ligament Injuries: A Cadaveric Model Study
Abstract
1. Introduction
2. Current Diagnostic Challenges and Limitations
2.1. The Role of MRI
2.2. The Role of Arthroscopy: Gold Standard with Significant Limitations
2.3. Critical Need for Improved Diagnostic Methods
2.4. Study Rationale and Significance
3. Methodology
3.1. Study Design and Ethical Considerations
3.2. Specimen Selection and Preparation
3.3. Anatomical Verification and Baseline Assessment
3.4. Scapholunate Ligament Transection Protocol
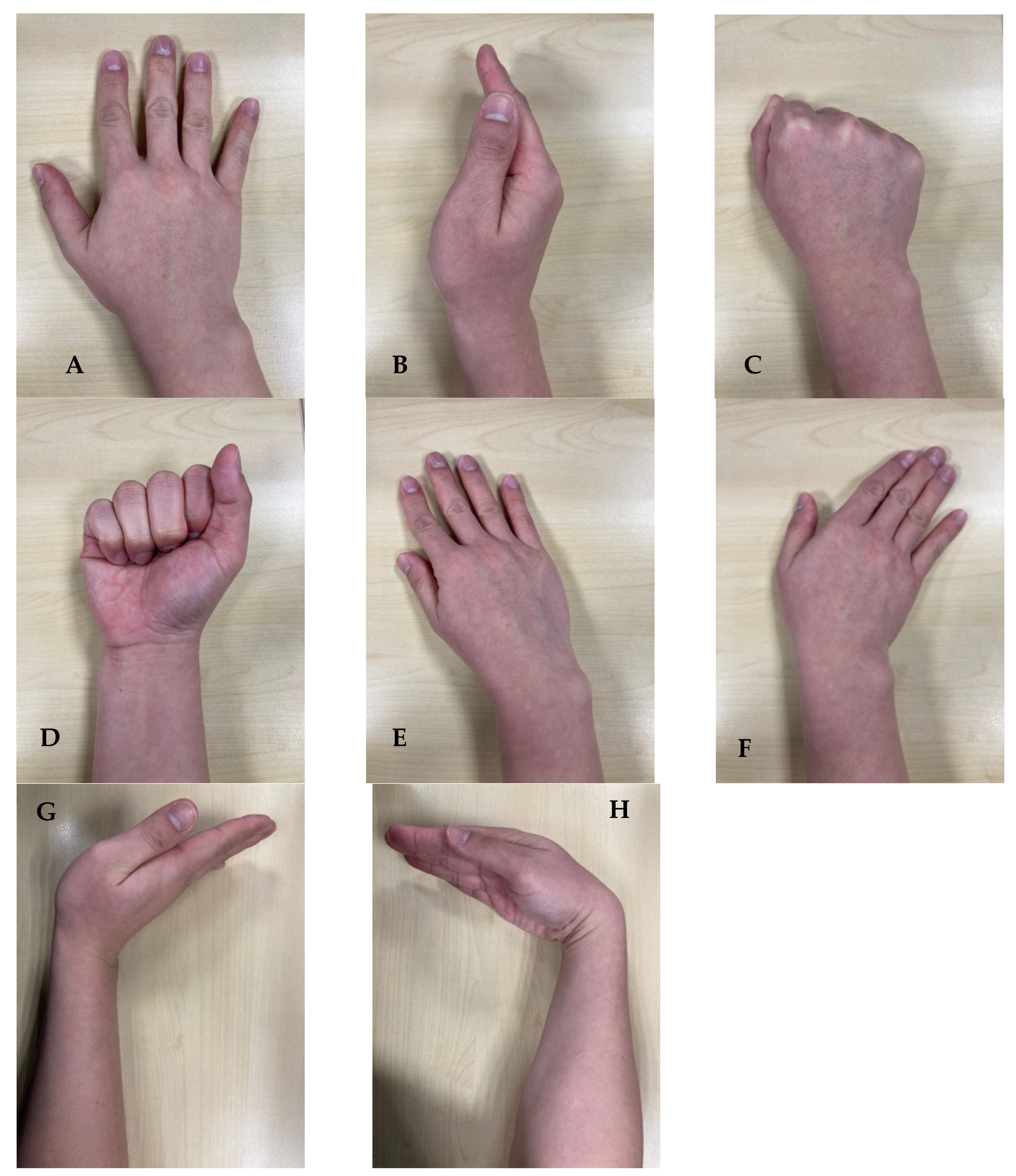
3.5. Radiographic Positioning and Imaging Protocol
3.6. Radiographic Technique and Image Acquisition
3.7. Measurement Methodology and Data Collection
3.8. Statistical Analysis and Data Management
3.9. Quality Assurance and Validation Measures
4. Results
4.1. Specimen Demographics and Characteristics
4.2. Scapholunate Gap Measurements Across Radiographic Positions
4.3. Lateral Radiographic Findings and Scapholunate Angle Analysis
4.4. Inter-Specimen Variability and Response Patterns
4.5. Statistical Significance and Effect Size Analysis
- -
- PA wrist extension vs. PA neutral: p = 0.006, Cohen’s d = 1.24 (large effect)
- -
- AP clenched fist vs. AP neutral: p = 0.036, Cohen’s d = 0.89 (large effect)
- -
- PA wrist flexion vs. PA neutral: p < 0.001, Cohen’s d = −2.31 (large effect, reduction)
- -
- PA radial deviation vs. PA neutral: p = 0.003, Cohen’s d = −1.18 (large effect, reduction)
4.6. Measurement Reliability and Quality Assurance
5. Discussion
5.1. Key Contributions and Clinical Significance
5.2. Study Limitations and Methodological Considerations
5.3. Future Research Directions and Clinical Validation
5.4. Clinical Recommendations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Berger, R.A. The gross and histologic anatomy of the scapholunate interosseous ligament. J. Hand Surg. 1996, 21, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Rajan, P.V.; Day, C.S. Scapholunate Interosseous Ligament Anatomy and Biomechanics. J. Hand Surg. 2015, 40, 1692–1702. [Google Scholar] [CrossRef] [PubMed]
- Kuo, C.E.; Wolfe, S.W. Scapholunate instability: Current concepts in diagnosis and management. J. Hand Surg. 2008, 33, 998–1013. [Google Scholar] [CrossRef] [PubMed]
- Esplugas, M.; Garcia-Elias, M.; Lluch, A.; Llusá Pérez, M. Role of muscles in the stabilization of ligament-deficient wrists. J. Hand Ther. Off. J. Am. Soc. Hand Ther. 2016, 29, 166–174. [Google Scholar] [CrossRef]
- Trail, I.A.; Stanley, J.K.; Hayton, M.J. Twenty Questions on Carpal Instability. J. Hand Surg. 2007, 32, 240–255. [Google Scholar] [CrossRef]
- Padmore, C.E.; Stoesser, H.; Langohr, G.D.G.; Johnson, J.A.; Suh, N. Carpal Kinematics following Sequential Scapholunate Ligament Sectioning. J. Wrist Surg. 2019, 08, 124–131. [Google Scholar] [CrossRef]
- Beutel, B.G.; Konstanty, J.; Beeker, R.W.; Rehman, U.H. Carpal Ligament Instability. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: http://www.ncbi.nlm.nih.gov/books/NBK557729/ (accessed on 21 September 2025).
- Pliefke, J.; Stengel, D.; Rademacher, G.; Mutze, S.; Ekkernkamp, A.; Eisenschenk, A. Diagnostic accuracy of plain radiographs and cineradiography in diagnosing traumatic scapholunate dissociation. Skelet. Radiol. 2008, 37, 139–145. [Google Scholar] [CrossRef]
- Zhou, J.Y.; Jodah, R.; Joseph, L.P.; Yao, J. Scapholunate Ligament Injuries. J. Hand Surg. Glob. Online 2024, 6, 245–267. [Google Scholar] [CrossRef]
- Frankel, V.H. The Terry-Thomas sign. Clin. Orthop. Relat. Res. 1977, 321–322. [Google Scholar] [CrossRef]
- Kader, N.; Arshad, M.S.; Chajed, P.K.; Makki, D.; Naikoti, K.; Temperley, D.; Murali, S.R. Evaluating Accuracy of Plain Magnetic Resonance Imaging or Arthrogram versus Wrist Arthroscopy in the Diagnosis of Scapholunate Interosseous Ligament Injury. J. Hand Microsurg. 2022, 14, 298–303. [Google Scholar] [CrossRef]
- Rachunek, K.; Springer, F.; Barczak, M.; Kolbenschlag, J.; Daigeler, A.; Medved, F. An algorithmic diagnostic approach to scapholunate ligament injuries based on comparison of X-ray examinations and arthroscopy in 414 patients. J. Plast. Reconstr. Aesthetic Surg. 2022, 75, 3293–3303. [Google Scholar] [CrossRef]
- Said, J.; Baker, K.; Fernandez, L.; Komatsu, D.E.; Gould, E.; Hurst, L.C. The Optimal Location to Measure Scapholunate Diastasis on Screening Radiographs. Hand 2018, 13, 671–677. [Google Scholar] [CrossRef]
- Lee, S.K.; Desai, H.; Silver, B.; Dhaliwal, G.; Paksima, N. Comparison of radiographic stress views for scapholunate dynamic instability in a cadaver model. J. Hand Surg. 2011, 36, 1149–1157. [Google Scholar] [CrossRef]
- Manton, G.L.; Schweitzer, M.E.; Weishaupt, D.; Morrison, W.B.; Osterman, A.L.; Culp, R.W.; Shabshin, N. Partial Interosseous Ligament Tears of the Wrist: Difficulty in Utilizing Either Primary or Secondary MRI Signs. J. Comput. Assist. Tomogr. 2001, 25, 671–676. [Google Scholar] [CrossRef]
- Shahabpour, M.; Staelens, B.; Van Overstraeten, L.; De Maeseneer, M.; Boulet, C.; De Mey, J.; Scheerlinck, T. Advanced imaging of the scapholunate ligamentous complex. Skelet. Radiol. 2015, 44, 1709–1725. [Google Scholar] [CrossRef]
- Zhang, M.; Yip, S.W.Y.; Wu, S.; Yeung, D.K.W.; Griffith, J.F. Direct traction MR imaging of the wrist: Practical experience. Skelet. Radiol. 2025, 54, 1407–1415. [Google Scholar] [CrossRef]
- Luitjens, J.; Hesse, N.; Rübenthaler, J.; Schmitt, R.; Gassert, F. Comparison of MRI and MR Arthrography for the Detection of Scapholunate Ligament Injuries: A Cost-Effectiveness Analysis. Osteoarthr. Cartil. 2023, 31, S246–S247. [Google Scholar] [CrossRef]
- Kitay, A.; Wolfe, S.W. Scapholunate instability: Current concepts in diagnosis and management. J. Hand Surg. 2012, 37, 2175–2196. [Google Scholar] [CrossRef]
- Geissler, W.B.; Freeland, A.E.; Savoie, F.H.; McIntyre, L.W.; Whipple, T.L. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J. Bone Jt. Surg. 1996, 78, 357–365. [Google Scholar] [CrossRef]
- van Wijk, L.; van der Heijden, B.; Souer, J.S.; Hovius, S.E.R.; Colaris, J.W.; Hand Wrist Study Group*. The role of diagnostic wrist arthroscopy in suspected scapholunate ligament injury: A cohort study of 324 patients. Bone Jt. Open 2025, 6, 312–320. [Google Scholar] [CrossRef]
- Beredjiklian, P.K.; Bozentka, D.J.; Leung, Y.L.; Monaghan, B.A. Complications of wrist arthroscopy. J. Hand Surg. 2004, 29, 406–411. [Google Scholar] [CrossRef]
- Sennwald, G. Diagnostic arthroscopy: Indications and interpretation of findings. J. Hand Surg. 2001, 26, 241–246. [Google Scholar] [CrossRef]
- Ng, A.W.H.; Chan, J.Y.S.; Griffith, J.F.; Ng, I.S.H.; Tse, W.L.; Ng, S.S.H. Imaging of dorsal wrist pain. Quant. Imaging Med. Surg. 2024, 14, 6945–6962. [Google Scholar] [CrossRef]
- Sikora, S.K.; Tham, S.K.; Harvey, J.N.; Garcia-Elias, M.; Goldring, T.; Rotstein, A.H.; Ek, E.T. The Twist X-ray: A Novel Test for Dynamic Scapholunate Instability. J. Wrist Surg. 2019, 8, 61–65. [Google Scholar] [CrossRef]
- Slater, R.R.; Szabo, R.M.; Bay, B.K.; Laubach, J. Dorsal intercarpal ligament capsulodesis for scapholunate dissociation: Biomechanical analysis in a cadaver model. J. Hand Surg. 1999, 24, 232–239. [Google Scholar] [CrossRef]
- Davis, C.A.; Culp, R.W.; Hume, E.L.; Osterman, A.L. Reconstruction of the scapholunate ligament in a cadaver model using a bone-ligament-bone autograft from the foot. J. Hand Surg. 1998, 23, 884–892. [Google Scholar] [CrossRef]
- Dunn, M.J.; Johnson, C. Static scapholunate dissociation: A new reconstruction technique using a volar and dorsal approach in a cadaver model. J. Hand Surg. 2001, 26, 749–754. [Google Scholar] [CrossRef]
- Pilla, N.I.; Koroneos, Z.A.; Dunleavy, M.L.; Vaughn, N.H.; Lewis, G.S.; Payatakes, A.H. A Biomechanical Comparison of Three Current Scapholunate Reconstruction Methods. J. Hand Surg. Glob. Online 2025, 7, 100701. [Google Scholar] [CrossRef]
- Dornberger, J.E.; Rademacher, G.; Mutze, S.; Eisenschenk, A.; Stengel, D. Accuracy of simple plain radiographic signs and measures to diagnose acute scapholunate ligament injuries of the wrist. Eur. Radiol. 2015, 25, 3488–3498. [Google Scholar] [CrossRef]
- Qualls, A.C.; Fox, W.B.; Merchant, A. Comprehensive Review on the Use of Fresh Frozen Cadavers in Procedural Skill Training of Medical Students. Int. J. Surg. Educ. 2024. [Google Scholar] [CrossRef]
- Iwanaga, J.; Obata, K.; Kato, T.; Samrid, R.; Lesser, E.R.; Cardona, J.J.; Kikuchi, K.; Kim, C.Y.; Ono, K.; D’ANtoni, A.; et al. What Is the Appropriate Sample Size in Human Cadaveric Studies? A Quantitative Review of 770 Articles. Clin. Anat. 2025. [Google Scholar] [CrossRef]
- Lopez-Valdes, F.J.; Mascareñas Brito, A.; Agnew, A.M.; Cripton, P.; Kerrigan, J.; Masouros, S.; Schmitt, K.-U.; Siegmund, G. The ethics, applications, and contributions of cadaver testing in injury prevention research. Traffic Inj. Prev. 2024, 25, 1115–1128. [Google Scholar] [CrossRef]
- Larsen, C.F.; Mathiesen, F.K.; Lindequist, S. Measurements of carpal bone angles on lateral wrist radiographs. J. Hand Surg. 1991, 16, 888–893. [Google Scholar] [CrossRef]
- Garcia-Elias, M.; Lluch, A.L.; Stanley, J.K. Three-ligament tenodesis for the treatment of scapholunate dissociation: Indications and surgical technique. J. Hand Surg. 2006, 31, 125–134. [Google Scholar] [CrossRef]
- Pridgen, B.; von Rabenau, L.; Luan, A.; Gu, A.J.; Wang, D.S.; Langlotz, C.; Chang, J.; Do, B. Automatic Detection of Perilunate and Lunate Dislocations on Wrist Radiographs Using Deep Learning. Plast. Reconstr. Surg. 2024, 153, 1138e–1141e. [Google Scholar] [CrossRef]
- van Kampen, R.J.; Henk Coert, J.; Moran, S.L. Mid-term outcomes of three commonly used surgical reconstructions for scapholunate instability. J. Hand Surg. 2024, 49, 852–858. [Google Scholar] [CrossRef]
- Rosvall, F.; Hagert, E.; Gustafson, P.; Andersson, J.K. Clinical and Socioeconomic Effects of Misdiagnosed Wrist Ligament Injuries. J. Wrist Surg. 2025, 14, 34–41. [Google Scholar] [CrossRef]
- Luetkens, K.S.; Kunz, A.S.; Paul, M.M.; Hölscher-Doht, S.; Huflage, H.; Heidenreich, J.F.; Müller, L.; Bley, T.A.; Schmitt, R.; Grunz, J.-P. Gantry-free cone-beam CT arthrography for diagnosis of scapholunate ligament injuries: Accelerating the preoperative work-up in acute wrist trauma. Eur. Radiol. 2025, 35, 4562–4570. [Google Scholar] [CrossRef]
- Ajmera, P.; Gandikota, G.; Kharat, A. Artificial Intelligence in Hand and Wrist Imaging: Enhancing Diagnostics and Workflow; Springer: Berlin/Heidelberg, Germany, 2025; pp. 1–15. [Google Scholar] [CrossRef]
- Kantarcı, M.; Aydın, S.; Oğul, H.; Kızılgöz, V. New imaging techniques and trends in radiology. Diagn. Interv. Radiol. 2025. [Google Scholar] [CrossRef]
- Copeland, J.; Byerly, D.W. Wrist Imaging. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Teule, E.H.S.; Hummelink, S.; Kumaş, A.; Buckens, C.F.M.; Sechopoulos, I.; van der Heijden, E.P.A. Automatic analysis of the scapholunate distance using 4DCT imaging: Normal values in the healthy wrist. Clin. Radiol. 2024, 79, e1040–e1048. [Google Scholar] [CrossRef]
- Saran, S.; Pellakuru, S.R.; Shah, A.B.; Wu, F.; Botchu, R. Interventions of the Hand and Wrist; Springer: Berlin/Heidelberg, Germany, 2025; pp. 1–27. [Google Scholar] [CrossRef]
- Alanen, M.; Aspinen, S.; Höglund, T.; Sippo, R.; Waris, E. Computer-aided three-dimensional analysis of carpal alignment in scaphoid nonunion advanced collapse wrists: A comparative study with scapholunate advanced collapse and healthy wrists. BMC Musculoskelet. Disord. 2025, 26, 423. [Google Scholar] [CrossRef]
- Alrehily, F.A. Assessing the inter-observer and intra-observer reliability of radiographic measurements for size-specific dose estimates. BMC Med. Imaging 2024, 24, 209. [Google Scholar] [CrossRef]
- Hermena, S.; Zabaglo, M. Wrist Arthrogram. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]

| Cadaver | Hand Side | Sex | Age |
|---|---|---|---|
| 1 | Lt | Female | 58 |
| 2 | Lt | Male | 71 |
| 3 | Rt | Male | 53 |
| 4 | Rt | Male | 78 |
| 5 | Lt | Male | 39 |
| 6 | Lt | Male | 69 |
| 7 | Rt | Male | 54 |
| 8 | Lt | Male | 53 |
| 9 | Lt | Male | 54 |
| Mean | 58.78 | ||
| Standard Deviation | 11.87 |
| Radiographic View | Mean SL Gap (mm) | SD (mm) | p-Value vs. Neutral PA |
|---|---|---|---|
| PA Neutral | 2.11 | 0.63 | — |
| AP Clenched Fist | 2.32 | 1.07 | 0.036 * |
| PA Clenched Fist | 1.94 | 0.64 | 0.14 |
| PA Ulnar Deviation | 2.11 | 0.94 | 0.11 |
| PA Radial Deviation | 1.08 | 0.52 | 0.003 * |
| PA Wrist Flexion | 0.47 | 0.44 | <0.001 * |
| PA Wrist Extension | 2.68 | 0.84 | 0.006 * |
| Lateral (SL Angle, °) | 58.8° | 9.8° | — |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Omar, U.F.; Ng, J.; Sim, W.P.; Rajaratnam, V. Comparison of Radiographic Stress Views in Detecting Scapholunate Ligament Injuries: A Cadaveric Model Study. J. Clin. Med. 2025, 14, 6764. https://doi.org/10.3390/jcm14196764
Omar UF, Ng J, Sim WP, Rajaratnam V. Comparison of Radiographic Stress Views in Detecting Scapholunate Ligament Injuries: A Cadaveric Model Study. Journal of Clinical Medicine. 2025; 14(19):6764. https://doi.org/10.3390/jcm14196764
Chicago/Turabian StyleOmar, Usama Farghaly, Jingwen Ng, Wei Ping Sim, and Vaikunthan Rajaratnam. 2025. "Comparison of Radiographic Stress Views in Detecting Scapholunate Ligament Injuries: A Cadaveric Model Study" Journal of Clinical Medicine 14, no. 19: 6764. https://doi.org/10.3390/jcm14196764
APA StyleOmar, U. F., Ng, J., Sim, W. P., & Rajaratnam, V. (2025). Comparison of Radiographic Stress Views in Detecting Scapholunate Ligament Injuries: A Cadaveric Model Study. Journal of Clinical Medicine, 14(19), 6764. https://doi.org/10.3390/jcm14196764





