Technical Variations in Lateral Extra-Articular Tenodesis for Anterior Cruciate Ligament Reconstruction: A Systematic Review
Abstract
1. Introduction
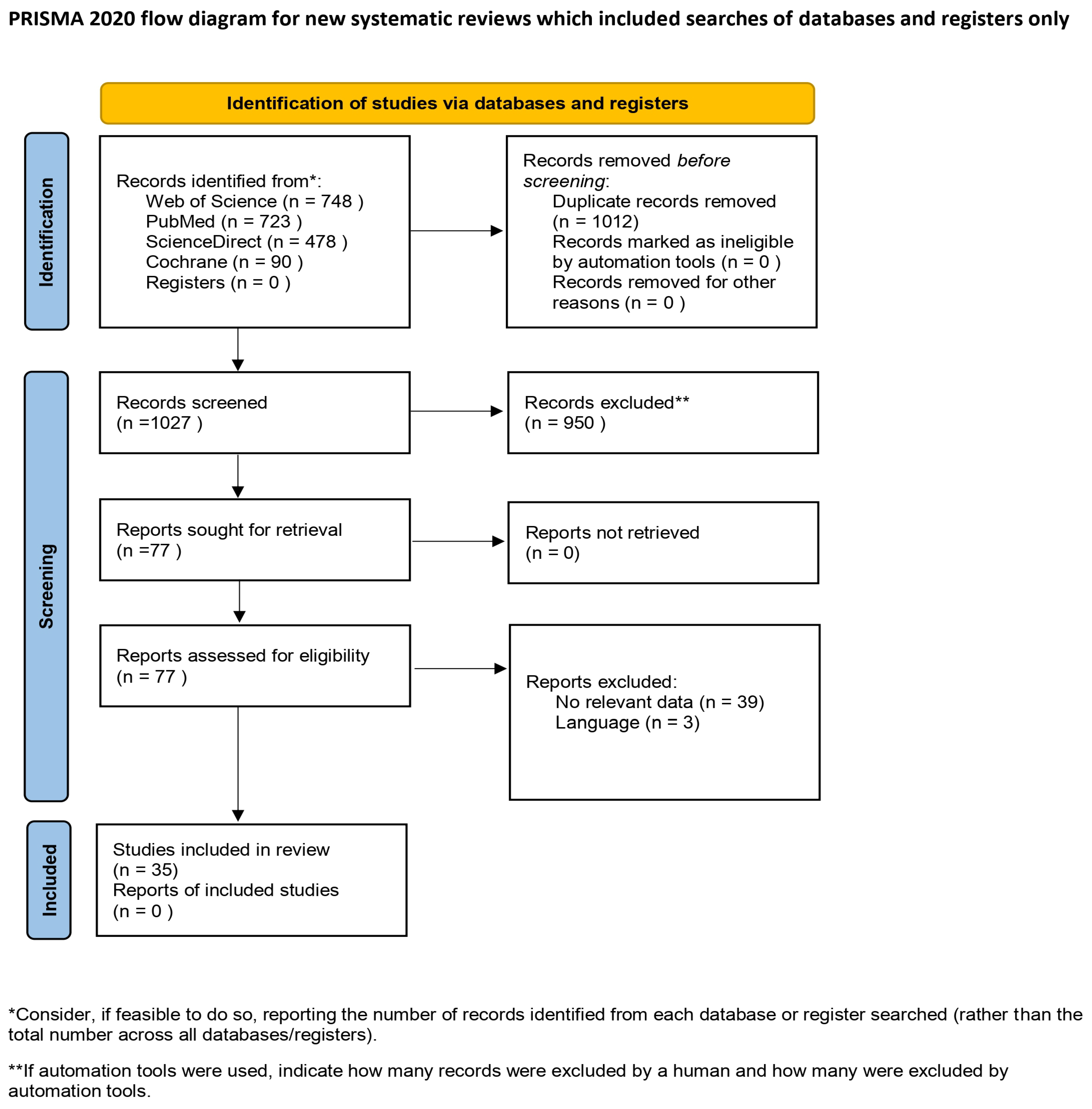
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Assessment
2.3. Data Extraction
2.4. Risk of Bias Assessment
3. Results
3.1. Surgical Technique
3.2. Femoral Attachment
3.3. Tibial Attachment
3.4. Fixation Method
3.5. Knee Angle During Fixation
3.6. Graft Type
3.7. Graft Tension
3.8. Summary of Key Patterns and Variations
4. Discussion
4.1. The Lemaire Procedure
4.2. The MacIntosh Procedure
4.3. The Other Procedures
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACL | Anterior cruciate ligament |
| ALC | Anterolateral complex |
| LCL | Lateral collateral ligament |
| ACLR | Anterior cruciate ligament reconstruction |
| LET | Lateral Extra-articular Tenodesis |
| PLCI | Posterolateral corner injury |
| LIS | Lateral intermuscular septum |
| iACLR | Isolated anterior cruciate ligament reconstruction |
| MACM | Arnold–Coker modification |
References
- Domnick, C.; Raschke, M.J.; Herbort, M. Biomechanics of the Anterior Cruciate Ligament: Physiology, Rupture and Reconstruction Techniques. World J. Orthop. 2016, 7, 82. [Google Scholar] [CrossRef]
- Roethke, L.; Braaten, J.; Rodriguez, A.; LaPrade, R. Revision Anterior Cruciate Ligament Reconstruction ACLR): Causes and How to Minimize Primary ACLR Failure. ABJS 2023, 11, 80–93. [Google Scholar] [CrossRef]
- Beynnon, B.D.; Johnson, R.J.; Abate, J.A.; Fleming, B.C.; Nichols, C.E. Treatment of Anterior Cruciate Ligament Injuries, Part I. Am. J. Sports Med. 2005, 33, 1579–1602. [Google Scholar] [CrossRef]
- Skinner, E.J.; Davis, D.D.; Varacallo, M. Segond Fracture. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Nazzal, E.M.; Keeling, L.E.; Ryan, P.M.; Herman, Z.J.; Hughes, J.D. The Role of Lateral Extra-Articular Tenodesis in Anterior Cruciate Ligament Reconstruction and Treatment of Rotatory Knee Instability: A Scoping Review. Curr. Rev. Musculoskelet. Med. 2023, 16, 235–245. [Google Scholar] [CrossRef]
- Claes, S.; Vereecke, E.; Maes, M.; Victor, J.; Verdonk, P.; Bellemans, J. Anatomy of the Anterolateral Ligament of the Knee. J. Anat. 2013, 223, 321–328. [Google Scholar] [CrossRef]
- Herbst, E.; Albers, M.; Burnham, J.M.; Fu, F.H.; Musahl, V. The Anterolateral Complex of the Knee. Orthop. J. Sports Med. 2017, 5, 2325967117730805. [Google Scholar] [CrossRef] [PubMed]
- Brockmeyer, M.; Orth, P.; Höfer, D.; Seil, R.; Paulsen, F.; Menger, M.D.; Kohn, D.; Tschernig, T. The Anatomy of the Anterolateral Structures of the Knee—A Histologic and Macroscopic Approach. Knee 2019, 26, 636–646. [Google Scholar] [CrossRef] [PubMed]
- Thein, R.; Boorman-Padgett, J.; Stone, K.; Wickiewicz, T.L.; Imhauser, C.W.; Pearle, A.D. Biomechanical Assessment of the Anterolateral Ligament of the Knee: A Secondary Restraint in Simulated Tests of the Pivot Shift and of Anterior Stability. J. Bone Jt. Surg. 2016, 98, 937–943. [Google Scholar] [CrossRef] [PubMed]
- Kwapisz, A.; Mollison, S.; McRae, S.; MacDonald, P. Lateral Extra-Articular Tenodesis with Proximal Staple Fixation. Arthrosc. Tech. 2019, 8, e821–e825. [Google Scholar] [CrossRef] [PubMed]
- Ferretti, A. Extra-Articular Reconstruction in the Anterior Cruciate Ligament Deficient Knee: A Commentary. Joints 2014, 2, 41–47. [Google Scholar]
- Filbay, S.R.; Grindem, H. Evidence-Based Recommendations for the Management of Anterior Cruciate Ligament (ACL) Rupture. Best. Pract. Res. Clin. Rheumatol. 2019, 33, 33–47. [Google Scholar] [CrossRef]
- Bernholt, D.L.; Kennedy, M.I.; Crawford, M.D.; DePhillipo, N.N.; LaPrade, R.F. Combined Anterior Cruciate Ligament Reconstruction and Lateral Extra-Articular Tenodesis. Arthrosc. Tech. 2019, 8, e855–e859. [Google Scholar] [CrossRef]
- Jesani, S.; Getgood, A. Modified Lemaire Lateral Extra-Articular Tenodesis Augmentation of Anterior Cruciate Ligament Reconstruction. JBJS Essent. Surg. Tech. 2019, 9, e41. [Google Scholar] [CrossRef]
- Firth, A.D.; Bryant, D.M.; Litchfield, R.; McCormack, R.G.; Heard, M.; MacDonald, P.B.; Spalding, T.; Verdonk, P.C.M.; Peterson, D.; Bardana, D.; et al. Predictors of Graft Failure in Young Active Patients Undergoing Hamstring Autograft Anterior Cruciate Ligament Reconstruction with or without a Lateral Extra-Articular Tenodesis: The Stability Experience. Am. J. Sports Med. 2022, 50, 384–395. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Green, D.W.; Hidalgo Perea, S.; Brusalis, C.M.; Chipman, D.E.; Asaro, L.A.; Cordasco, F.A. A Modified Lemaire Lateral Extra-Articular Tenodesis in High-Risk Adolescents Undergoing Anterior Cruciate Ligament Reconstruction with Quadriceps Tendon Autograft: 2-Year Clinical Outcomes. Am. J. Sports Med. 2023, 51, 1441–1446. [Google Scholar] [CrossRef]
- Hantouly, A.T.; Ahmed, A.F.; Fermin, T.M.; Macchiarola, L.; Sideris, V.; Papakostas, E.; Hooghe, P.D.; Al-Khelaifi, K.; Olory, B.; Zikria, B. Short-Term Outcomes of Anterior Cruciate Ligament Reconstruction with or without Lateral Tenodesis or Anterolateral Ligament Reconstruction: A Retrospective Cohort. Int. Orthop. (SICOT) 2023, 47, 2991–2999. [Google Scholar] [CrossRef]
- Trichine, F.; Alsaati, M.; Chouteau, J.; Moyen, B.; Bouzitouna, M.; Maza, R. Patellar Tendon Autograft Reconstruction of the Anterior Cruciate Ligament with and without Lateral Plasty in Advanced-Stage Chronic Laxity. A Clinical, Prospective, Randomized, Single-Blind Study Using Passive Dynamic X-Rays. Knee 2014, 21, 58–65. [Google Scholar] [CrossRef] [PubMed]
- El-Azab, H.; Moursy, M.; Mohamed, M.A.; Elsayed, M. A Comparison of the Outcomes of Anterior Curciate Ligament Reconstruction with Large-Size Graft versus Reconstruction with Average-Size Graft Combined with Extraarticular Tenodesis. Injury 2023, 54, 976–982. [Google Scholar] [CrossRef] [PubMed]
- Joseph, L.; Demey, G.; Chamu, T.; Schmidt, A.; Germain, A.; Van Rooij, F.; Saffarini, M.; Dejour, D. Adding a Modified Lemaire Procedure to ACLR in Knees with Severe Rotational Knee Instability Does Not Compromise Isokinetic Muscle Recovery at the Time of Return-to-Play. J. Exp. Ortop. 2020, 7, 84. [Google Scholar] [CrossRef] [PubMed]
- Eggeling, L.; Drenck, T.C.; Frings, J.; Krause, M.; Korthaus, A.; Krukenberg, A.; Frosch, K.-H.; Akoto, R. Additional Lateral Extra-Articular Tenodesis in Revision ACL Reconstruction Does Not Influence the Outcome of Patients with Low-Grade Anterior Knee Laxity. Arch. Orthop. Trauma. Surg. 2022, 142, 291–299. [Google Scholar] [CrossRef]
- Minguell Monyart, J.; Moreira Borim, F.; Revertè Vinaixa, M.M.; Portas-Torres, I.; Pijoan Bueno, J.; Castellet Feliu, E.; Joshi Jubert, N. Allografts and Lateral Extra-Articular Tenodesis for Revision Anterior Cruciate Ligament Reconstruction: Enhanced Rotational Stability and Improved Functional Outcomes. Eur. J. Orthop. Surg. Traumatol. 2023, 33, 2579–2586. [Google Scholar] [CrossRef] [PubMed]
- Vadalà, A.P.; Iorio, R.; De Carli, A.; Bonifazi, A.; Iorio, C.; Gatti, A.; Rossi, C.; Ferretti, A. An Extra-Articular Procedure Improves the Clinical Outcome in Anterior Cruciate Ligament Reconstruction with Hamstrings in Female Athletes. Int. Orthop. (SICOT) 2013, 37, 187–192. [Google Scholar] [CrossRef]
- Gibbs, C.M.; Hughes, J.D.; Popchak, A.J.; Chiba, D.; Lesniak, B.P.; Anderst, W.J.; Musahl, V. Anterior Cruciate Ligament Reconstruction with Lateral Extraarticular Tenodesis Better Restores Native Knee Kinematics in Combined ACL and Meniscal Injury. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Feller, J.A.; Devitt, B.M.; Webster, K.E.; Klemm, H.J. Augmentation of Primary ACL Reconstruction with a Modified Ellison Lateral Extra-Articular Tenodesis in High-Risk Patients: A Pilot Study. Orthop. J. Sports Med. 2021, 9, 23259671211021351. [Google Scholar] [CrossRef]
- Viglietta, E.; Ponzo, A.; Monaco, E.; Iorio, R.; Drogo, P.; Andreozzi, V.; Conteduca, F.; Ferretti, A. ACL Reconstruction Combined with the Arnold-Coker Modification of the MacIntosh Lateral Extra-Articular Tenodesis: Long-Term Clinical and Radiological Outcomes. Am. J. Sports Med. 2022, 50, 404–414. [Google Scholar] [CrossRef] [PubMed]
- Marcacci, M.; Zaffagnini, S.; Giordano, G.; Iacono, F.; Lo Presti, M. Anterior Cruciate Ligament Reconstruction Associated with Extra-Articular Tenodesis: A Prospective Clinical and Radiographic Evaluation with 10- to 13-Year Follow-Up. Am. J. Sports Med. 2009, 37, 707–714. [Google Scholar] [CrossRef]
- Ibrahim, S.A.-R. Anterior Cruciate Ligament Reconstruction by Combined Intra-Articular (K. Lambert) and Extra-Articular Iliotibial Band Tenodesis (MacIntosh; Autologous Grafts). Med. Princ. Pract. 1999, 8, 1–5. [Google Scholar] [CrossRef]
- Declercq, J.; Schuurmans, M.; Tack, L.; Verhelst, C.; Truijen, J. Combined Lateral Extra-Articular Tenodesis and Anterior Cruciate Ligament Reconstruction: Risk of Osteoarthritis. Eur. J. Orthop. Surg. Traumatol. 2022, 33, 1075–1082. [Google Scholar] [CrossRef]
- Monaco, E.; Carrozzo, A.; Saithna, A.; Conteduca, F.; Annibaldi, A.; Marzilli, F.; Minucci, M.; Sonnery-Cottet, B.; Ferretti, A. Isolated ACL Reconstruction Versus ACL Reconstruction Combined with Lateral Extra-Articular Tenodesis: A Comparative Study of Clinical Outcomes in Adolescent Patients. Am. J. Sports Med. 2022, 50, 3244–3255. [Google Scholar] [CrossRef]
- Getgood, A.; Hewison, C.; Bryant, D.; Litchfield, R.; Heard, M.; Buchko, G.; Hiemstra, L.A.; Willits, K.R.; Firth, A.; MacDonald, P. No Difference in Functional Outcomes When Lateral Extra-Articular Tenodesis Is Added to Anterior Cruciate Ligament Reconstruction in Young Active Patients: The Stability Study. Arthrosc.: J. Arthrosc. Relat. Surg. 2020, 36, 1690–1701. [Google Scholar] [CrossRef]
- Heard, M.; Marmura, H.; Bryant, D.; Litchfield, R.; McCormack, R.; MacDonald, P.; Spalding, T.; Verdonk, P.; Peterson, D.; Bardana, D.; et al. No Increase in Adverse Events with Lateral Extra-Articular Tenodesis Augmentation of Anterior Cruciate Ligament Reconstruction—Results from the Stability Randomized Trial. J. ISAKOS 2023, 8, 246–254, Correction in: J. ISAKOS 2023, 8, 513. https://doi.org/10.1016/j.jisako.2023.09.006. [Google Scholar] [CrossRef]
- Farinelli, L.; Abermann, E.; Meena, A.; Ueblacker, P.; Hahne, J.; Fink, C. Return to Play and Pattern of Injury After ACL Rupture in a Consecutive Series of Elite UEFA Soccer Players. Orthop. J. Sports Med. 2023, 11, 23259671231153629. [Google Scholar] [CrossRef]
- Alm, L.; Drenck, T.C.; Frosch, K.-H.; Akoto, R. Lateral Extra-Articular Tenodesis in Patients with Revision Anterior Cruciate Ligament (ACL) Reconstruction and High-Grade Anterior Knee Instability. Knee 2020, 27, 1451–1457. [Google Scholar] [CrossRef] [PubMed]
- Jacquet, C.; Pioger, C.; Seil, R.; Khakha, R.; Parratte, S.; Steltzlen, C.; Argenson, J.-N.; Pujol, N.; Ollivier, M. Incidence and Risk Factors for Residual High-Grade Pivot Shift After ACL Reconstruction with or without a Lateral Extra-Articular Tenodesis. Orthop. J. Sports Med. 2021, 9, 23259671211003590. [Google Scholar] [CrossRef] [PubMed]
- Keizer, M.N.J.; Brouwer, R.W.; De Graaff, F.; Hoogeslag, R.A.G. Higher Return to Pre-Injury Type of Sports after Revision Anterior Ligament Reconstruction with Lateral Extra-Articular Tenodesis Compared to without Lateral Extra-Articular Tenodesis. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 1699–1703. [Google Scholar] [CrossRef]
- Borim, F.M.; Jubert, N.J.; Vinaixa, M.M.R.; Portas-Torres, I.; Bueno, J.P.; Mayayo, R.S.; Peiró, J.V.A.; Feliu, E.C.; Monyart, J.M. Good Rates of Return-to-Sport in Athletes after Revision Anterior Cruciate Ligament Reconstruction Using Autologous Patellar Tendon and Lateral Extra-Articular Tenodesis: A 2-Year Follow-up Prospective Study. Eur. J. Orthop. Surg. Traumatol. 2023, 33, 3125–3133. [Google Scholar] [CrossRef]
- Oni, O.O.A.; Crowder, E. A Comparison of Isokinetics and Muscle Strength Ratios Following Intra-Articular and Extra-Articular Reconstructions of the Anterior Cruciate Ligament. Injury 1996, 27, 195–197. [Google Scholar] [CrossRef]
- Alessio-Mazzola, M.; Formica, M.; Russo, A.; Sanguineti, F.; Capello, A.G.; Lovisolo, S.; Felli, L. Outcome after Combined Lateral Extra-Articular Tenodesis and Anterior Cruciate Ligament Revision in Professional Soccer Players. J. Knee Surg. 2019, 32, 906–910. [Google Scholar] [CrossRef]
- Christodoulou, N.A.; Sdrenias, C.V.; Tsaknis, R.N.; Mavrogenis, A.F.; Tsigginou, A.M. Reinforced Iliotibial Tenodesis for Chronic Anterolateral Instability of the Knee: A 6-Year Follow-Up/EDITORIAL COMMENT. Orthopedics 2005, 28, 472–478. [Google Scholar] [CrossRef] [PubMed]
- Legnani, C.; Borgo, E.; Macchi, V.; Ventura, A. Restoring Rotational Stability Following Anterior Cruciate Ligament Surgery: Single-Bundle Reconstruction Combined with Lateral Extra-Articular Tenodesis versus Double-Bundle Reconstruction. J. Comp. Eff. Res. 2022, 11, 729–736. [Google Scholar] [CrossRef] [PubMed]
- Guy, S.; Fayard, J.-M.; Saithna, A.; Bahroun, S.; Ferreira, A.; Carrozzo, A.; De Jesus, S.; Bulle, S.; Vieira, T.D.; Sonnery-Cottet, B. Risk of Graft Rupture After Adding a Lateral Extra-Articular Procedure at the Time of ACL Reconstruction: A Retrospective Comparative Study of Elite Alpine Skiers from the French National Team. Am. J. Sports Med. 2022, 50, 1609–1617. [Google Scholar] [CrossRef]
- Legnani, C.; Boisio, F.; Borgo, E.; Ventura, A. Autograft for Anterior Cruciate Ligament Revision Surgery: Lateral Extra-Articular Tenodesis in Skeletally Mature Patients under 25 Years of Age. Orthopäde 2019, 48, 858–861. [Google Scholar] [CrossRef] [PubMed]
- Zanna, L.; Niccolò, G.; Matteo, I.; Malone, J.; Roberto, C.; Fabrizio, M. Clinical Outcomes and Return to Sport after Single-Stage Revision Anterior Cruciate Ligament Reconstruction by Bone-Patellar Tendon Autograft Combined with Lateral Extra-Articular Tenodesis. Eur. J. Orthop. Surg. Traumatol. 2022, 33, 1811–1819. [Google Scholar] [CrossRef]
- Grassi, A.; Pizza, N.; Andrea Lucidi, G.; Macchiarola, L.; Mosca, M.; Zaffagnini, S. Anatomy, Magnetic Resonance and Arthroscopy of the Popliteal Hiatus of the Knee: Normal Aspect and Pathological Conditions. EFORT Open Rev. 2021, 6, 61–74. [Google Scholar] [CrossRef]
- Guzzini, M.; Mazza, D.; Fabbri, M.; Lanzetti, R.; Redler, A.; Iorio, C.; Monaco, E.; Ferretti, A. Extra-Articular Tenodesis Combined with an Anterior Cruciate Ligament Reconstruction in Acute Anterior Cruciate Ligament Tear in Elite Female Football Players. Int. Orthop. (SICOT) 2016, 40, 2091–2096. [Google Scholar] [CrossRef] [PubMed]
- Chiba, D.; Gale, T.; Nishida, K.; Suntaxi, F.; Lesniak, B.P.; Fu, F.H.; Anderst, W.; Musahl, V. Lateral Extra-Articular Tenodesis Contributes Little to Change In Vivo Kinematics After Anterior Cruciate Ligament Reconstruction: A Randomized Controlled Trial. Am. J. Sports Med. 2021, 49, 1803–1812. [Google Scholar] [CrossRef]
- Ventura, A.; Legnani, C.; Boisio, F.; Borgo, E.; Peretti, G.M. The Association of Extra-Articular Tenodesis Restores Rotational Stability More Effectively Compared to Contralateral Hamstring Tendon Autografts ACL Reconstruction Alone in Patients Undergoing ACL Revision Surgery. Orthop. Traumatol. Surg. Res. 2021, 107, 102739. [Google Scholar] [CrossRef]
- Getgood, A.M.J.; Bryant, D.M.; Litchfield, R.; Heard, M.; McCormack, R.G.; Rezansoff, A.; Peterson, D.; Bardana, D.; MacDonald, P.B.; Verdonk, P.C.M.; et al. Lateral Extra-Articular Tenodesis Reduces Failure of Hamstring Tendon Autograft Anterior Cruciate Ligament Reconstruction: 2-Year Outcomes from the STABILITY Study Randomized Clinical Trial. Am. J. Sports Med. 2020, 48, 285–297. [Google Scholar] [CrossRef]
- Mahmoud, A.; Torbey, S.; Honeywill, C.; Myers, P. Lateral Extra-Articular Tenodesis Combined with Anterior Cruciate Ligament Reconstruction Is Effective in Knees with Additional Features of Lateral, Hyperextension, or Increased Rotational Laxity: A Matched Cohort Study. Arthrosc. J. Arthrosc. Relat. Surg. 2022, 38, 119–124. [Google Scholar] [CrossRef]
- Grassi, A.; Costa, G.G.; Cialdella, S.; Lo Presti, M.; Neri, M.P.; Zaffagnini, S. The 90-Day Readmission Rate after Single-Bundle ACL Reconstruction Plus LET: Analysis of 2,559 Consecutive Cases from a Single Institution. J. Knee Surg. 2021, 34, 978–986. [Google Scholar] [CrossRef]
- McAleese, T.; Murgier, J.; Cavaignac, E.; Devitt, B.M. A Review of Marcel Lemaire’s Original Work on Lateral Extra-Articular Tenodesis. J. ISAKOS 2024, 9, 431–437. [Google Scholar] [CrossRef] [PubMed]
- Ferretti, A.; Monaco, E.; Ponzo, A.; Basiglini, L.; Iorio, R.; Caperna, L.; Conteduca, F. Combined Intra-Articular and Extra-Articular Reconstruction in Anterior Cruciate Ligament–Deficient Knee: 25 Years Later. Arthrosc. J. Arthrosc. Relat. Surg. 2016, 32, 2039–2047. [Google Scholar] [CrossRef]
- Perelli, S.; Gelber, P.E.; Morales-Avalos, R.; Ronco, S.; Torres-Claramunt, R.; Espregueira-Mendes, J.; Monllau, J.C. Isolated Lateral Extra-Articular Tenodesis in ACL-Deficient Knees: In Vivo Knee Kinematics and Clinical Outcomes. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3212–3220. [Google Scholar] [CrossRef]
- Aga, C.; Kartus, J.-T.; Lind, M.; Lygre, S.H.L.; Granan, L.-P.; Engebretsen, L. Risk of Revision Was Not Reduced by a Double-Bundle ACL Reconstruction Technique: Results from the Scandinavian Registers. Clin. Orthop. Relat. Res. 2017, 475, 2503–2512. [Google Scholar] [CrossRef]
- Lagae, K.C.; Robberecht, J.; Athwal, K.K.; Verdonk, P.C.M.; Amis, A.A. ACL Reconstruction Combined with Lateral Monoloop Tenodesis Can Restore Intact Knee Laxity. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 1159–1168. [Google Scholar] [CrossRef] [PubMed]
- Noyes, F.R.; Chen, R.C.; Barber-Westin, S.D.; Potter, H.G. Greater Than 10-Year Results of Red-White Longitudinal Meniscal Repairs in Patients 20 Years of Age or Younger. Am. J. Sports Med. 2011, 39, 1008–1017. [Google Scholar] [CrossRef] [PubMed]
- Buerba, R.A.; Zaffagnini, S.; Kuroda, R.; Musahl, V. ACL Reconstruction in the Professional or Elite Athlete: State of the Art. J. ISAKOS 2021, 6, 226–236. [Google Scholar] [CrossRef]
- Meynard, P.; Pelet, H.; Angelliaume, A.; Legallois, Y.; Lavignac, P.; De Bartolo, R.; Fabre, T.; Costes, S. ACL Reconstruction with Lateral Extra-Articular Tenodesis Using a Continuous Graft: 10-Year Outcomes of 50 Cases. Orthop. Traumatol. Surg. Res. 2020, 106, 929–935. [Google Scholar] [CrossRef]
- Getgood, A.; Brown, C.; Lording, T.; Amis, A.; Claes, S.; Geeslin, A.; Musahl, V.; ALC Consensus Group. The Anterolateral Complex of the Knee: Results from the International ALC Consensus Group Meeting. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 166–176. [Google Scholar] [CrossRef]
- Slette, E.L.; Mikula, J.D.; Schon, J.M.; Marchetti, D.C.; Kheir, M.M.; Turnbull, T.L.; LaPrade, R.F. Biomechanical Results of Lateral Extra-Articular Tenodesis Procedures of the Knee: A Systematic Review. Arthrosc. J. Arthrosc. Relat. Surg. 2016, 32, 2592–2611. [Google Scholar] [CrossRef]
- Pavão, D.M.; Cruz, R.S.; De Faria, J.L.R.; De Sousa, E.B.; Barretto, J.M. Modified Lemaire Lateral Tenodesis Associated with an Intra-Articular Reconstruction Technique with Bone-Tendon-Bone Graft Using an Adjustable Fixation Mechanism. Arthrosc. Tech. 2019, 8, e733–e740. [Google Scholar] [CrossRef]
- Neri, T.; Cadman, J.; Beach, A.; Grasso, S.; Dabirrahmani, D.; Putnis, S.; Oshima, T.; Devitt, B.; Coolican, M.; Fritsch, B.; et al. Lateral Tenodesis Procedures Increase Lateral Compartment Pressures More than Anterolateral Ligament Reconstruction, When Performed in Combination with ACL Reconstruction: A Pilot Biomechanical Study. J. ISAKOS 2021, 6, 66–73. [Google Scholar] [CrossRef]
- Koukoulias, N.E.; Dimitriadis, T.; Vasiliadis, A.V.; Germanou, E.; Boutovinos, A.-P. ACL Reconstruction and Modified Lemaire Tenodesis Utilizing Common Suspensory Femoral Fixation. Arthrosc. Tech. 2022, 11, e2185–e2193. [Google Scholar] [CrossRef]
- Christel, P.; Djian, P. [Anterio-lateral extra-articular tenodesis of the knee using a short strip of fascia lata]. Rev. Chir. Orthop. Reparatrice Appar. Mot. 2002, 88, 508–513. [Google Scholar] [PubMed]
- Maffulli, N.; Oliviero, A. Review of Jones (1963) on ‘Reconstruction of the Anterior Cruciate Ligament. A Technique Using the Central One-Third of the Patellar Ligament’. J. ISAKOS 2019, 4, 338–344. [Google Scholar] [CrossRef]
- Schlichte, L.M.; Aitchison, A.H.; Green, D.W.; Cordasco, F.A. Modified Lemaire Lateral Extra-Articular Tenodesis in the Pediatric Patient: An Adjunct to Anterior Cruciate Ligament Reconstruction. Arthrosc. Tech. 2020, 9, e111–e116. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, N.; Monketh, J.; Volpin, A. Clinical and Mechanical Outcomes in Isolated Anterior Cruciate Ligament Reconstruction vs Additional Lateral Extra-Articular Tenodesis or Anterolateral Ligament Reconstruction. World J. Orthop. 2022, 13, 662–675. [Google Scholar] [CrossRef]
- Getgood, A.; Bryant, D.; Firth, A.; Stability Group. The Stability Study: A Protocol for a Multicenter Randomized Clinical Trial Comparing Anterior Cruciate Ligament Reconstruction with and without Lateral Extra-Articular Tenodesis in Individuals Who Are at High Risk of Graft Failure. BMC Musculoskelet. Disord. 2019, 20, 216. [Google Scholar] [CrossRef] [PubMed]
- Orduna, S. Lateral Extraarticular Tenodesis in Combination with ACL Reconstruction: Indications, Technique Description. GJOR 2019, 1. [Google Scholar] [CrossRef]
- Bertoia, J.T.; Urovitz, E.P.; Richards, R.R.; Gross, A.E. Anterior Cruciate Reconstruction Using the MacIntosh Lateral-Substitution over-the-Top Repair. J. Bone Jt. Surg. Am. 1985, 67, 1183–1188. [Google Scholar] [CrossRef]
- Abusleme, S.; Strömbäck, L.; Caracciolo, G.; Zamorano, H.; Cheyre, J.; Vergara, F.; Yañez, R. Lateral Extra-Articular Tenodesis: A Technique with an Iliotibial Band Strand without Implants. Arthrosc. Tech. 2021, 10, e85–e89. [Google Scholar] [CrossRef] [PubMed]
| Author | Year | Country | Study Design | Level of Evidence | Type of Study | Number of Subjects | Male | Female | Mean Age |
|---|---|---|---|---|---|---|---|---|---|
| Green et al. [17] | 2023 | USA | Case series | 4 | Retrospective | 48 | 27 | 21 | 14.2 |
| Hantouly et al. [18] | 2023 | Qatar | Cohort study | 3 | Retrospective | 100 | 94 | 6 | 28.15 |
| Trichine et al. [19] | 2013 | Algieria | Randomized trial | 1 | Prospective | 120 | 120 | 0 | 28.15 |
| Mahmoud et al. [51] | 2021 | Australia | Matched cohort study | 3 | Retrospective | 72 | 55 | 17 | 25 |
| El-Azab et al. [20] | 2023 | Egypt, Austria | Randomized Comparative Study | 1 | Prospective | 100 | 73 | 27 | 27.5 |
| Joseph et al. [21] | 2020 | France, Switzerland | Comparative study | 3 | Retrospective | 87 | 57 | 30 | 29.7 |
| Eggeling et al. [22] | 2021 | Germany | Cohort study | 3 | Retrospective | 78 | 48 | 30 | 28.7 |
| Monyart et al. [23] | 2023 | Spain | Case series | 4 | Prospective | 46 | 31 | 15 | 36.3 |
| Vadalà et al. [24] | 2012 | Italy | Comparative study | 3 | Prospective | 60 | 0 | 60 | 27 |
| Gibbs et al. [25] | 2021 | USA, Japan | Cohort study | 3 | Retrospective | 20 | 12 | 8 | 20.8 |
| Feller et al. [26] | 2021 | Australia | Case series | 4 | Retrospective | 25 | 21 | 4 | 8.5 |
| Viglietta et al. [27] | 2021 | Italy | Cohort study | 3 | Retrospective | 164 | 126 | 38 | 27.3 |
| Marcacci et al. [28] | 2009 | Italy | Case series | 4 | Retrospective | 60 | 45 | 15 | - |
| Ibrahim et al. [29] | 1999 | Kuwait | Case series | 4 | Retrospective | 153 | 153 | 0 | 23.7 |
| Declercq et al. [30] | 2021/22 | Belgium | Case series | 4 | Retrospective | 86 | 69 | 17 | 26.1 |
| Monaco et al. [31] | 2022 | Italy | Cohort study | 3 | Retrospective | 111 | 69 | 42 | 16.2 |
| Getgood et al. [32] | 2020 | Canada | Randomized Controlled Trial | 1 | Retrospective | 356 | 154 | 202 | 18.9 |
| Heard et al. [33] | 2023 | Canada | Randomized Clinical Trial | 1 | Prospective | 618 | 302 | 316 | 18.9 |
| Farinelli et al. [34] | 2023 | Austria | Case series | 4 | Retrospective | 27 | 27 | 0 | 23.15 |
| Alm et al. [35] | 2020 | Germany | Case series | 4 | Retrospective | 73 | 39 | 34 | 31 |
| Jacquet et al. [36] | 2021 | France | Cohort study | 3 | Retrospective | 266 | 190 | 76 | 30.4 |
| Keizer et al. [37] | 2022 | Netherlands | Cohort study | 3 | Retrospective | 78 | 57 | 21 | 29.3 |
| Borim et al. [38] | 2023 | Spain | Case series | 4 | Prospective | 19 | 9 | 10 | 27.7 |
| Oni & Crowder [39] | 1996 | UK | Randomized Controlled Trial | 1 | Prospective | 32 | 26 | 6 | - |
| Alessio-Mazzola et al. [40] | 2019 | Italy | Case series | 4 | Retrospective | 24 | 24 | 0 | 23.8 |
| Christodoulou et al. [41] | 2005 | Greece | Case series | 4 | Retrospective | 52 | 47 | 5 | 41 |
| Legnani et al. [42] | 2022 | Italy | Case series | 4 | Retrospective | 36 | 22 | 14 | 27.6 |
| Guy et al. [43] | 2022 | France | Cohort study | 3 | Retrospective | 81 | 45 | 36 | 22.5 |
| Legnani et al. [44] | 2019 | Italy | Case series | 4 | Retrospective | 9 | 7 | 2 | 23.3 |
| Zanna et al. [45] | 2023 | Italy | Case series | 4 | Retrospective | 17 | 14 | 3 | 26.4 |
| Grassi et al. [46] | 2021 | Italy | Case series | 4 | Retrospective | 2559 | 2009 | 550 | 30.9 |
| Guzzini et al. [47] | 2016 | Italy | Case series | 4 | Retrospective | 16 | 0 | 16 | 26.4 |
| Chiba et al. [48] | 2021 | USA | Randomized Controlled Trial | 1 | Prospective | 18 | 11 | 7 | 20.45 |
| Ventura et al. [49] | 2021 | Italy | Case series | 3 | Retrospective | 24 | 19 | 5 | 30.35 |
| Getgood et al. [50] | 2020 | Canada | Randomized Controlled Trial | 1 | Prospective | 618 | 297 | 321 | 18.9 |
| Author | Type of Technique | Femoral Attachment | Tibial Attachment | Fixation Method | Knee Angle During Fixation |
|---|---|---|---|---|---|
| Green et al. [17] | modified Lemaire | proximal and posterior to the lateral femoral epicondyle | Gerdy’s Tubercle | Sutures | 30° flexion |
| Hantouly et al. [18] | modified Lemaire | 3 cm higher to gastrocnemius insertion in the posterior third of the femur | Gerdy’s Tubercle | Sutures/Staples/Anchor | 30° flexion |
| Trichine et al. [19] | Christel | Lateral femoral condyle | Gerdy’s Tubercle | Interference screw | 90° flexion, 10° external rotation |
| Mahmoud et al. [51] | MacIntosh | ITB | Gerdy’s Tubercle | Sutures | 50° flexion |
| El-Azab et al. [20] | modified Lemaire | distal ridge of Kaplan’s fibers | n/a | Interference screw | n/a |
| Joseph et al. [21] | modified Lemaire | n/a | Gerdy’s Tubercle | Interference screw | |
| Eggeling et al. [22] | Modified Lemaire | 1 cm proximal and posterior to the lateral epicondyle | Gerdy’s Tubercle | Interference screw | 45° flexion |
| Monyart et al. [23] | modified Lemaire | n/a | n/a | n/a | n/a |
| Vadalà et al. [24] | Macintosh modified by Coker–Arnold | n/a | Gerdy’s Tubercle | Sutures | n/a |
| Gibbs et al. [25] | modified Lemaire | proximal and posterior to the lateral femoral epicondyle | Gerdy’s Tubercle | Staples | Between 60° and 70° flexion |
| Feller et al. [26] | modified Ellison | ITT strip passed deep to the LCL from proximal to distal and reattached to Gerdy’s tubercle | Gerdy’s Tubercle | Sutures/Anchor | Between 60° and 70° flexion |
| Viglietta et al. [27] | MacIntosh modified by Coker–Arnold | n/a | Gerdy’s Tubercle | Sutures | 90° flexion, external rotation |
| Marcacci et al. [28] | Marcacci | Lateral femoral condyle | Gerdy’s Tubercle | Staples | 90° flexion |
| Ibrahim et al. [29] | MacIntosh | n/a | Gerdy’s Tubercle | Sutures | 90° flexion |
| Declercq et al. [30] | MacIntosh modified by Coker–Arnold/modified Lemaire | ITB | Gerdy’s Tubercle | Sutures/Anchor | 30° flexion, maximal external rotation |
| Monaco et al. [31] | MacIntosh modified by Coker–Arnold | ITB | Gerdy’s Tubercle | Sutures | 90° flexion, external rotation |
| Getgood et al. [32] | modified Lemaire | Distal femur anteriorly to the intermuscular septum and proximally to the femoral attachment site of the FCL | Gerdy’s Tubercle | Staples | Between 60° and 70° flexion |
| Heard et al. [33] | modified Lemaire | n/a | n/a | Sutures | Between 60° and 70° flexion |
| Farinelli et al. [34] | modified Ellison | ITT strip passed deep to the LCL from proximal to distal and reattached to Gerdy’s tubercle | Gerdy’s Tubercle | Sutures/Anchor | n/a |
| Alm et al. [35] | modified Lemaire | 1 cm proximal and posterior to the lateral epicondyle | Gerdy’s Tubercle | Sutures/K-wire | 45° flexion |
| Jacquet et al. [36] | modified Lemaire | Distal femur anteriorly to the intermuscular septum and proximally to the femoral attachment site of the FCL | Gerdy’s Tubercle | Interference screw | 20° flexion |
| Keizer et al. [37] | modified Lemaire | n/a | n/a | Interference screw | 20° flexion |
| Borim et al. [38] | modified Lemaire | n/a | n/a | n/a | n/a |
| Oni & Crowder [39] | Lemaire | Lateral femoral condyle | n/a | Sutures | 60° flexion, maximal external rotation |
| Alessio-Mazzola et al. [40] | MacIntosh modified by Coker–Arnold | ITB | Gerdy’s Tubercle | Sutures | 90° flexion, 30° external rotation |
| Christodoulou et al. [41] | MacIntosh | Lateral femoral epicondyle | Gerdy’s Tubercle | Titanium screw with a serrated polyethylene washer | 60° flexion, 5° external rotation |
| Legnani et al. [42] | MacIntosh modified by Coker–Arnold | ITB | n/a | Sutures | n/a |
| Guy et al. [43] | modified Lemaire | Modified Lemaire fixation | n/a | Bioabsorbable screw | Full extension |
| Legnani et al. [44] | MacIntosh modified by Coker–Arnold | Lateral femoral epicondyle | Gerdy’s Tubercle | Sutures | n/a |
| Zanna et al. [45] | MacIntosh modified by Coker–Arnold | Lateral femoral epicondyle | Gerdy’s Tubercle | Sutures | 90° flexion |
| Grassi et al. [46] | Marcacci | Lateral femoral condyle | Gerdy s Tubercle | Staples | Between 60° and 70° flexion |
| Guzzini et al. [47] | MacIntosh modified by Coker–Arnold | Lateral femoral epicondyle | Gerdy s Tubercle | Sutures | n/a |
| Chiba et al. [48] | modified Lemaire | Lateral femoral epicondyle | Gerdy’s Tubercle | Staples | Between 60° and 70° flexion |
| Ventura et al. [49] | MacIntosh modified by Coker–Arnold | ITB | n/a | Sutures | 20° flexion |
| Getgood et al. [50] | modified Lemaire | Lateral femoral condyle | n/a | Staples | Between 60° and 70° flexion |
| Author | Graft Type | Graft Tension During Fixation |
|---|---|---|
| Green et al. [17] | ITB 8 cm × 1 cm | n/a |
| Hantouly et al. [18] | ITB 10–15 cm × 1 cm | n/a |
| Trichine et al. [19] | ITB 7.5 cm × 1.2 cm | high manual tension |
| Mahmoud et al. [51] | ITB 12–15 cm | physiological tension |
| El-Azab et al. [20] | n/a | n/a |
| Joseph et al. [21] | ITB 8 cm × 1 cm | n/a |
| Eggeling et al. [22] | ITB 6–8 cm × 0.6–0.8 cm | n/a |
| Monyart et al. [23] | n/a | n/a |
| Vadalà et al. [24] | ITB | n/a |
| Gibbs et al. [25] | ITB | moderate manual tension approx. 20 N |
| Feller et al. [26] | ITB | n/a |
| Viglietta et al. [27] | ITB 13 cm × 1 cm | n/a |
| Marcacci et al. [28] | n/a | n/a |
| Ibrahim et al. [29] | ITB 15 cm × 1 cm | n/a |
| Declercq et al. [30] | ITB 6–8 cm × 1 cm | n/a |
| Monaco et al. [31] | ITB 13 cm × 1 cm | n/a |
| Getgood et al. [32] | ITB 8 cm × 1 cm | minimal tension |
| Heard et al. [33] | ITB 8 cm × 1 cm | taut; <20 N |
| Farinelli et al. [34] | n/a | n/a |
| Alm et al. [35] | ITB 6–8 cm × 0.6–0.8 cm | n/a |
| Jacquet et al. [36] | ITB 8 cm × 1 cm | n/a |
| Keizer et al. [37] | n/a | n/a |
| Borim et al. [38] | n/a | n/a |
| Oni & Crowder [39] | ITB 15 cm × 5 cm made into a tube | n/a |
| Alessio-Mazzola et al. [40] | ITB 10 cm × 1 cm | n/a |
| Christodoulou et al. [41] | ITB 8–10 cm × 1.3–1.6 cm | n/a |
| Legnani et al. [42] | ITB | n/a |
| Guy et al. [43] | n/a | n/a |
| Legnani et al. [44] | ITB 8–10 cm × 1 cm | n/a |
| Zanna et al. [45] | ITB 10 cm × 1 cm | n/a |
| Grassi et al. [46] | Semitendinosus and gracilis | n/a |
| Guzzini et al. [47] | ITB 10 cm × 1 cm | n/a |
| Chiba et al. [48] | ITB 8 cm × 1 cm | moderate manual tension approx. 20 N |
| Ventura et al. [49] | ITB | high manual tension |
| Getgood et al. [50] | ITB 8 cm × 1 cm | minimal tension |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zabrzyński, J.; Turoń, B.; Kwapisz, A.; Boutsiadis, A.; Zabrzyńska, M.; Sokołowski, M.; Majchrzak, B.; Adamczyk, M.; Kellett, K.; Huri, G. Technical Variations in Lateral Extra-Articular Tenodesis for Anterior Cruciate Ligament Reconstruction: A Systematic Review. J. Clin. Med. 2025, 14, 6510. https://doi.org/10.3390/jcm14186510
Zabrzyński J, Turoń B, Kwapisz A, Boutsiadis A, Zabrzyńska M, Sokołowski M, Majchrzak B, Adamczyk M, Kellett K, Huri G. Technical Variations in Lateral Extra-Articular Tenodesis for Anterior Cruciate Ligament Reconstruction: A Systematic Review. Journal of Clinical Medicine. 2025; 14(18):6510. https://doi.org/10.3390/jcm14186510
Chicago/Turabian StyleZabrzyński, Jan, Bartosz Turoń, Adam Kwapisz, Achilles Boutsiadis, Maria Zabrzyńska, Maciej Sokołowski, Bartosz Majchrzak, Michalina Adamczyk, Katie Kellett, and Gazi Huri. 2025. "Technical Variations in Lateral Extra-Articular Tenodesis for Anterior Cruciate Ligament Reconstruction: A Systematic Review" Journal of Clinical Medicine 14, no. 18: 6510. https://doi.org/10.3390/jcm14186510
APA StyleZabrzyński, J., Turoń, B., Kwapisz, A., Boutsiadis, A., Zabrzyńska, M., Sokołowski, M., Majchrzak, B., Adamczyk, M., Kellett, K., & Huri, G. (2025). Technical Variations in Lateral Extra-Articular Tenodesis for Anterior Cruciate Ligament Reconstruction: A Systematic Review. Journal of Clinical Medicine, 14(18), 6510. https://doi.org/10.3390/jcm14186510







