Surgery Without Scalpel: Histotripsy as a Non-Invasive and Non-Thermal Modality for Liver Tumor Ablation
Abstract
1. Introduction
2. Histotripsy: Principles and Mechanism of Action
2.1. Acoustic Cavitation and Bubble Cloud Formation
2.2. Device and Pulse Parameters
2.3. Mechanical Tissue Fractionation and Disintegration
2.4. Biological and Immunological Implications
3. Preclinical and Clinical Evidence in Liver Oncology
3.1. Preclinical Evidence in Liver Oncology
3.2. Clinical Evidence in Liver Oncology
3.3. Contraindications for Using Histotripsy
3.4. Advantages over Traditional Therapies
3.5. Recommended Selection Criteria for Histotripsy in Liver Tumor Ablation
- Maximum Size and Number of Liver Tumors
- ii.
- Child–Pugh Grading for Eligibility
- iii.
- Tumor Location Within the Liver
- iv.
- Patient and Tumor Characteristics Modulating Immunomodulatory and Abscopal Effects
4. Challenges and Limitations
5. Future Directions and Research Priorities
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rumgay, H.; Arnold, M.; Ferlay, J.; Lesi, O.; Cabasag, C.J.; Vignat, J.; Laversanne, M.; McGlynn, K.A.; Soerjomataram, I. Global burden of primary liver cancer in 2020 and predictions to 2040. J. Hepatol. 2022, 77, 1598–1606. [Google Scholar] [CrossRef] [PubMed]
- Oh, J.H.; Jun, D.W. The latest global burden of liver cancer: A past and present threat. Clin. Mol. Hepatol. 2023, 29, 355–357. [Google Scholar] [CrossRef] [PubMed]
- Alawyia, B.; Constantinou, C. Hepatocellular Carcinoma: A Narrative Review on Current Knowledge and Future Prospects. Curr. Treat. Options Oncol. 2023, 24, 711–724. [Google Scholar] [CrossRef] [PubMed]
- Forner, A.; Reig, M.; Bruix, J. Hepatocellular carcinoma. Lancet 2018, 391, 1301–1314. [Google Scholar] [CrossRef]
- Villanueva, A. Hepatocellular Carcinoma. N. Engl. J. Med. 2019, 380, 1450–1462. [Google Scholar] [CrossRef]
- Vitale, A.; Romano, P.; Cillo, U.; Writing Group for the HE.RC.O.LE.S Collaborative Group; Writing Group for the ITA.LI.CA Collaborative Group; HE.RC.O.LE.S and ITA.LI.CA Collaborative Groups; Lauterio, A.; Sangiovanni, A.; Cabibbo, G.; Missale, G.; et al. Liver Resection vs Nonsurgical Treatments for Patients with Early Multinodular Hepatocellular Carcinoma. JAMA Surg. 2024, 159, 881. [Google Scholar] [CrossRef]
- Brown, Z.J.; Tsilimigras, D.I.; Ruff, S.M.; Mohseni, A.; Kamel, I.R.; Cloyd, J.M.; Pawlik, T.M. Management of Hepatocellular Carcinoma. JAMA Surg. 2023, 158, 410. [Google Scholar] [CrossRef]
- Singal, A.G.; Llovet, J.M.; Yarchoan, M.; Mehta, N.; Heimbach, J.K.; Dawson, L.A.; Jou, J.H.; Kulik, L.M.; Agopian, V.G.; Marrero, J.A.; et al. AASLD Practice Guidance on prevention, diagnosis, and treatment of hepatocellular carcinoma. Hepatology 2023, 78, 1922–1965. [Google Scholar] [CrossRef]
- Wade, R.; South, E.; Anwer, S.; Sharif-Hurst, S.; Harden, M.; Fulbright, H.; Hodgson, R.; Dias, S.; Simmonds, M.; Rowe, I.; et al. Ablative and non-surgical therapies for early and very early hepatocellular carcinoma: A systematic review and network meta-analysis. Health Technol. Assess. 2023, 27, 1–172. [Google Scholar] [CrossRef]
- Johnson, B.W.; Wright, G.P. Regional therapies for the treatment of primary and metastatic hepatic tumors: A disease-based review of techniques and critical appraisal of current evidence. Am. J. Surg. 2019, 217, 541–545. [Google Scholar] [CrossRef]
- Tsilimigras, D.I.; Brodt, P.; Clavien, P.A.; Muschel, R.J.; D’Angelica, M.I.; Endo, I.; Parks, R.W.; Doyle, M.; de Santibañes, E.; Pawlik, T.M. Liver metastases. Nat. Rev. Dis. Primers 2021, 7, 27. [Google Scholar] [CrossRef] [PubMed]
- Rashidian, N.; Alseidi, A.; Kirks, R.C. Cancers Metastatic to the Liver. Surg. Clin. N. Am. 2020, 100, 551–563. [Google Scholar] [CrossRef] [PubMed]
- de Ridder, J.; de Wilt, J.H.W.; Simmer, F.; Overbeek, L.; Lemmens, V.; Nagtegaal, I. Incidence and origin of histologically confirmed liver metastases: An explorative case-study of 23,154 patients. Oncotarget 2016, 7, 55368–55376. [Google Scholar] [CrossRef] [PubMed]
- Kaur, H.; Hindman, N.M.; Al-Refaie, W.B.; Arif-Tiwari, H.; Cash, B.D.; Chernyak, V.; Farrell, J.; Grajo, J.R.; Horowitz, J.M.; McNamara, M.M.; et al. ACR Appropriateness Criteria® Suspected Liver Metastases. J. Am. Coll. Radiol. 2017, 14, S314–S325. [Google Scholar] [CrossRef]
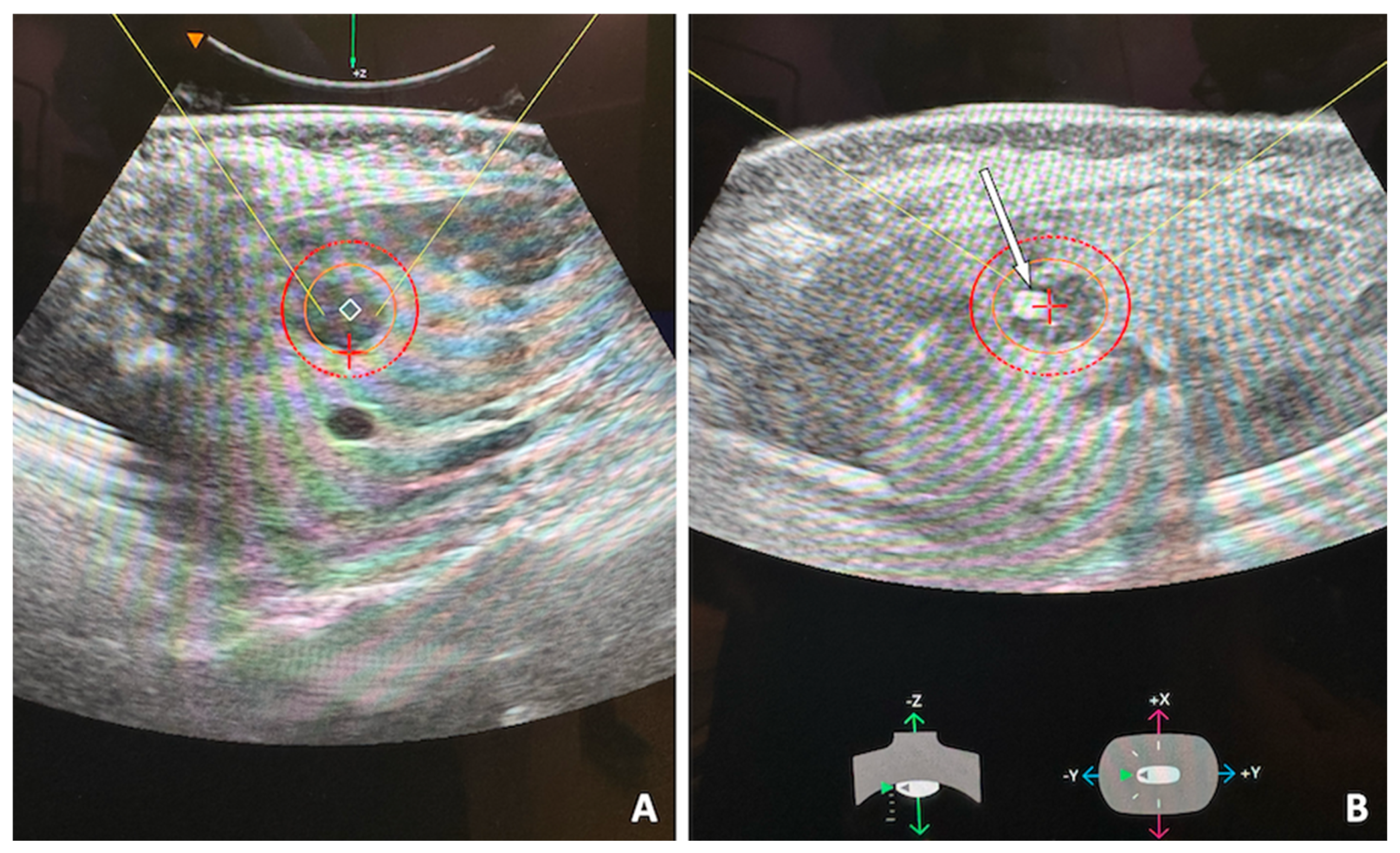
- Uysal, M.; Wehrle, C.J.; Satish, S.; Knott, E.; Hong, H.; Allkushi, E.; Schlegel, A.; Berber, E.; Aucejo, F.; Kim, J.; et al. Histotripsy of Liver Tumors: Patient Selection, Ethical Discussions, and How We Do It. Cancers 2025, 17, 1100. [Google Scholar] [CrossRef]
- Xu, Z.; Khokhlova, T.D.; Cho, C.S.; Khokhlova, V.A. Histotripsy: A Method for Mechanical Tissue Ablation with Ultrasound. Annu. Rev. Biomed. Eng. 2024, 26, 141–167. [Google Scholar] [CrossRef]
- Xu, Z.; Hall, T.L.; Vlaisavljevich, E.; Lee, F.T. Histotripsy: The first noninvasive, non-ionizing, non-thermal ablation technique based on ultrasound. Int. J. Hyperth. 2021, 38, 561–575. [Google Scholar] [CrossRef]
- Williams, R.P.; Simon, J.C.; Khokhlova, V.A.; Sapozhnikov, O.A.; Khokhlova, T.D. The histotripsy spectrum: Differences and similarities in techniques and instrumentation. Int. J. Hyperth. 2023, 40, 2233720. [Google Scholar] [CrossRef]
- Bader, K.B.; Vlaisavljevich, E.; Maxwell, A.D. For Whom the Bubble Grows: Physical Principles of Bubble Nucleation and Dynamics in Histotripsy Ultrasound Therapy. Ultrasound Med. Biol. 2019, 45, 1056–1080. [Google Scholar] [CrossRef]
- Khokhlova, V.A.; Fowlkes, J.B.; Roberts, W.W.; Schade, G.R.; Xu, Z.; Khokhlova, T.D.; Hall, T.L.; Maxwell, A.D.; Wang, Y.N.; Cain, C.A. Histotripsy methods in mechanical disintegration of tissue: Towards clinical applications. Int. J. Hyperth. 2015, 31, 145–162. [Google Scholar] [CrossRef]
- Lundt, J.E.; Allen, S.P.; Shi, J.; Hall, T.L.; Cain, C.A.; Xu, Z. Non-invasive, Rapid Ablation of Tissue Volume Using Histotripsy. Ultrasound Med. Biol. 2017, 43, 2834–2847. [Google Scholar] [CrossRef]
- Mancia, L.; Vlaisavljevich, E.; Yousefi, N.; Rodriguez, M.; Ziemlewicz, T.J.; Lee, F.T.; Henann, D.; Franck, C.; Xu, Z.; Johnsen, E. Modeling tissue-selective cavitation damage. Phys. Med. Biol. 2019, 64, 225001. [Google Scholar] [CrossRef] [PubMed]
- Vlaisavljevich, E.; Maxwell, A.; Mancia, L.; Johnsen, E.; Cain, C.; Xu, Z. Visualizing the Histotripsy Process: Bubble Cloud–Cancer Cell Interactions in a Tissue-Mimicking Environment. Ultrasound Med. Biol. 2016, 42, 2466–2477. [Google Scholar] [CrossRef] [PubMed]
- Edsall, C.; Huynh, L.; Hall, T.L.; Vlaisavljevich, E. Bubble cloud characteristics and ablation efficiency in dual-frequency intrinsic threshold histotripsy. Phys. Med. Biol. 2023, 68, 225006. [Google Scholar] [CrossRef] [PubMed]
- Edsall, C.; Ham, E.; Holmes, H.; Hall, T.L.; Vlaisavljevich, E. Effects of frequency on bubble-cloud behavior and ablation efficiency in intrinsic threshold histotripsy. Phys. Med. Biol. 2021, 66, 225009. [Google Scholar] [CrossRef]
- Hendricks-Wenger, A.; Hutchison, R.; Vlaisavljevich, E.; Allen, I.C. Immunological Effects of Histotripsy for Cancer Therapy. Front. Oncol. 2021, 11, 681629. [Google Scholar] [CrossRef]
- Worlikar, T.; Hall, T.; Zhang, M.; Mendiratta-Lala, M.; Green, M.; Cho, C.S.; Xu, Z. Insights from in vivo preclinical cancer studies with histotripsy. Int. J. Hyperth. 2024, 41, 2297650. [Google Scholar] [CrossRef]
- Worlikar, T.; Vlaisavljevich, E.; Gerhardson, T.; Greve, J.; Wan, S.; Kuruvilla, S.; Lundt, J.; Ives, K.; Hall, T.; Welling, T.H.; et al. Histotripsy for Non-Invasive Ablation of Hepatocellular Carcinoma (HCC) Tumor in a Subcutaneous Xenograft Murine Model. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2018, 2018, 6064–6067. [Google Scholar] [CrossRef]
- Qu, S.; Worlikar, T.; Felsted, A.E.; Ganguly, A.; Beems, M.V.; Hubbard, R.; Pepple, A.L.; Kevelin, A.A.; Garavaglia, H.; Dib, J.; et al. Non-thermal histotripsy tumor ablation promotes abscopal immune responses that enhance cancer immunotherapy. J. Immunother. Cancer 2020, 8, e000200. [Google Scholar] [CrossRef]
- Hendricks-Wenger, A.; Saunier, S.; Simon, A.; Grider, D.; Luyimbazi, D.; Allen, I.C.; Vlaisavljevich, E. Histotripsy for the Treatment of Cholangiocarcinoma in a Patient-Derived Xenograft Mouse Model. Ultrasound Med. Biol. 2022, 48, 293–303. [Google Scholar] [CrossRef]
- Hendricks-Wenger, A.; Weber, P.; Simon, A.; Saunier, S.; Coutermarsh-Ott, S.; Grider, D.; Vidal-Jove, J.; Allen, I.C.; Luyimbazi, D.; Vlaisavljevich, E. Histotripsy for the Treatment of Cholangiocarcinoma Liver Tumors: In Vivo Feasibility and Ex Vivo Dosimetry Study. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 2021, 68, 2953–2964. [Google Scholar] [CrossRef] [PubMed]
- Falk, K.L.; Laeseke, P.F.; Kisting, M.A.; Zlevor, A.M.; Knott, E.A.; Smolock, A.R.; Bradley, C.; Vlaisavljevich, E.; Lee, F.T., Jr.; Ziemlewicz, T.J. Clinical translation of abdominal histotripsy: A review of preclinical studies in large animal models. Int. J. Hyperth. 2023, 40, 2272065. [Google Scholar] [CrossRef] [PubMed]
- Knott, E.A.; Zlevor, A.M.; Hinshaw, J.L.; Laeseke, P.F.; Longhurst, C.; Frank, J.; Bradley, C.W.; Couillard, A.B.; Rossebo, A.E.; Xu, Z.; et al. A comparison study of microwave ablation vs. histotripsy for focal liver treatments in a swine model. Eur. Radiol. 2022, 33, 1050–1062. [Google Scholar] [CrossRef] [PubMed]
- Vidal-Jove, J.; Serres, X.; Vlaisavljevich, E.; Cannata, J.; Duryea, A.; Miller, R.; Merino, X.; Velat, M.; Kam, Y.; Bolduan, R.; et al. First-in-man histotripsy of hepatic tumors: The THERESA trial, a feasibility study. Int. J. Hyperth. 2022, 39, 1115–1123. [Google Scholar] [CrossRef]
- Wah, T.M.; Pech, M.; Thormann, M.; Serres, X.; Littler, P.; Stenberg, B.; Lenton, J.; Smith, J.; Wiggermann, P.; Planert, M.; et al. A Multi-centre, Single Arm, Non-randomized, Prospective European Trial to Evaluate the Safety and Efficacy of the HistoSonics System in the Treatment of Primary and Metastatic Liver Cancers (#HOPE4LIVER). Cardiovasc. Interv. Radiol. 2023, 46, 259–267. [Google Scholar] [CrossRef]
- Wehrle, C.J.; Burns, K.; Ong, E.; Couillard, A.; Parikh, N.D.; Caoili, E.; Kim, J.; Aucejo, F.; Schlegel, A.; Knott, E.; et al. The first international experience with histotripsy: A safety analysis of 230 cases. J. Gastrointest. Surg. 2025, 29, 102000. [Google Scholar] [CrossRef]
- Izzo, F.; Granata, V.; Grassi, R.; Fusco, R.; Palaia, R.; Delrio, P.; Carrafiello, G.; Azoulay, D.; Petrillo, A.; Curley, S.A. Radiofrequency Ablation and Microwave Ablation in Liver Tumors: An Update. Oncologist 2019, 24, e990–e1005. [Google Scholar] [CrossRef]
- Mendiratta-Lala, M.; Wiggermann, P.; Pech, M.; Serres-Créixams, X.; White, S.B.; Davis, C.; Ahmed, O.; Parikh, N.D.; Planert, M.; Thormann, M.; et al. The #HOPE4LIVER Single-Arm Pivotal Trial for Histotripsy of Primary and Metastatic Liver Tumors. Radiology 2024, 312, e233051. [Google Scholar] [CrossRef]
- Mauch, S.C.; Zlevor, A.M.; Knott, E.A.; Couillard, A.B.; Periyasamy, S.; Williams, E.C.; Swietlik, J.F.; Laeseke, P.F.; Zhang, X.; Xu, Z.; et al. Hepatic and Renal Histotripsy in an Anticoagulated Porcine Model. J. Vasc. Interv. Radiol. 2023, 34, 386–394.e2. [Google Scholar] [CrossRef]
- Sandilos, G.; Butchy, M.V.; Koneru, M.; Gongalla, S.; Sensenig, R.; Hong, Y.K. Histotripsy—Hype or hope? Review of innovation and future implications. J. Gastrointest. Surg. 2024, 28, 1370–1375. [Google Scholar] [CrossRef]
- Künzli, B.M.; Abitabile, P.; Maurer, C.A. Radiofrequency ablation of liver tumors: Actual limitations and potential solutions in the future. World J. Hepatol. 2011, 3, 8. [Google Scholar] [CrossRef]
- Huang, H. Influence of blood vessel on the thermal lesion formation during radiofrequency ablation for liver tumors. Med. Phys. 2013, 40, 073303. [Google Scholar] [CrossRef] [PubMed]
- Osada, T.; Jiang, X.; Zhao, Y.; Chen, M.; Kreager, B.C.; Wu, H.; Kim, H.; Ren, J.; Snyder, J.; Zhong, P.; et al. The use of histotripsy as intratumoral immunotherapy beyond tissue ablation—The rationale for exploring the immune effects of histotripsy. Int. J. Hyperth. 2023, 40, 2263672. [Google Scholar] [CrossRef] [PubMed]
- Imran, K.M.; Ganguly, A.; Paul, T.; Powar, M.; Vlaisavljevich, E.; Cho, C.S.; Allen, I.C. Magic bubbles: Utilizing histotripsy to modulate the tumor microenvironment and improve systemic anti-tumor immune responses. Int. J. Hyperth. 2023, 40, 2244206. [Google Scholar] [CrossRef] [PubMed]
- Pepple, A.L.; Guy, J.L.; McGinnis, R.; Felsted, A.E.; Song, B.; Hubbard, R.; Worlikar, T.; Garavaglia, H.; Dib, J.; Chao, H.; et al. Spatiotemporal local and abscopal cell death and immune responses to histotripsy focused ultrasound tumor ablation. Front. Immunol. 2023, 14, 1012799. [Google Scholar] [CrossRef]
- Pahk, K.J.; Shin, C.H.; Bae, I.Y.; Yang, Y.; Kim, S.H.; Pahk, K.; Kim, H.; Oh, S.J. Boiling Histotripsy-induced Partial Mechanical Ablation Modulates Tumour Microenvironment by Promoting Immunogenic Cell Death of Cancers. Sci. Rep. 2019, 9, 9050. [Google Scholar] [CrossRef]
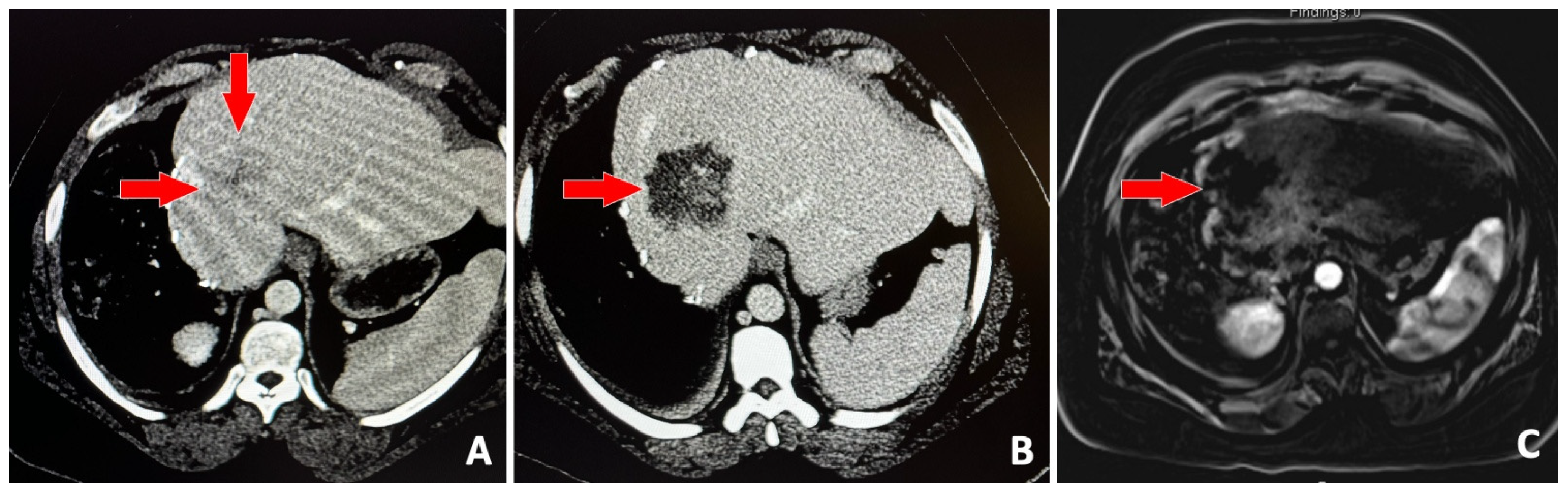
- Vidal-Jove, J.; Serres-Creixams, X.; Ziemlewicz, T.J.; Cannata, J.M. Liver Histotripsy Mediated Abscopal Effect-Case Report. IEEE Trans. Ultrason. Ferroelectr. Freq. Control. 2021, 68, 3001–3005. [Google Scholar] [CrossRef] [PubMed]
- Raman, A.P.; Kotlarz, P.L.; Giff, A.E.; Goundry, K.A.; Laeseke, P.; Koepsel, E.M.K.; Alhamami, M.; Daye, D. Breaking Barriers with Sound: The Implementation of Histotripsy in Cancer. Cancers 2025, 17, 2548. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Carstensen, E.L.; Gracewski, S.; Dalecki, D. The search for cavitation in vivo. Ultrasound Med. Biol. 2000, 26, 1377–1385. [Google Scholar] [CrossRef]
- Church, C.C. A theoretical study of acoustic cavitation produced by ‘positive-only’ and ‘negative-only’ pressure waves in relation to in vivo studies. Ultrasound Med. Biol. 2003, 29, 319–330. [Google Scholar] [CrossRef]
- Miller, D.L. Mechanisms for Induction of Pulmonary Capillary Hemorrhage by Diagnostic Ultrasound: Review and Consideration of Acoustical Radiation Surface Pressure. Ultrasound Med. Biol. 2016, 42, 2743–2757. [Google Scholar] [CrossRef]
- Petrella, L.I.; Maggi, L.E.; Souza, R.M.; Alvarenga, A.V.; Costa-Félix, R.P.B. Influence of subcutaneous fat in surface heating of ultrasonic diagnostic transducers. Ultrasonics 2014, 54, 1476–1479. [Google Scholar] [CrossRef] [PubMed]
- Heinitz, S.; Müller, J.; Jenderka, K.V.; Schlögl, H.; Stumvoll, M.; Blüher, M.; Blank, V.; Karlas, T. The application of high-performance ultrasound probes increases anatomic depiction in obese patients. Sci. Rep. 2023, 13, 16297. [Google Scholar] [CrossRef] [PubMed]
- Worlikar, T.; Mendiratta-Lala, M.; Vlaisavljevich, E.; Hubbard, R.; Shi, J.; Hall, T.L.; Cho, C.S.; Lee, F.T.; Greve, J.; Xu, Z. Effects of Histotripsy on Local Tumor Progression in an in vivo Orthotopic Rodent Liver Tumor Model. BME Front. 2020, 2020, 9830304. [Google Scholar] [CrossRef] [PubMed]
- Eigner, E.; Malshy, K.; Bandari, J.; Fazaa, N.; Nsair, A.; Hines, L.; Atallah, M.; Joseph, J.V.; Rappold, P.M. Histotripsy in the Management of RCC: A New Frontier in Focused Therapies. Clin. Genitourin. Cancer 2025, 23, 102360. [Google Scholar] [CrossRef]
- Gannon, J.; Imran, K.M.; Hendricks-Wenger, A.; Edwards, M.; Covell, H.; Ruger, L.; Singh, N.; Nagai-Singer, M.; Tintera, B.; Eden, K.; et al. Ultrasound-guided noninvasive pancreas ablation using histotripsy: Feasibility study in an in vivo porcine model. Int. J. Hyperth. 2023, 40, 2247187. [Google Scholar] [CrossRef]
- Schuster, T.G.; Wei, J.T.; Hendlin, K.; Jahnke, R.; Roberts, W.W. Histotripsy Treatment of Benign Prostatic Enlargement Using the Vortx Rx System: Initial Human Safety and Efficacy Outcomes. Urology 2018, 114, 184–187. [Google Scholar] [CrossRef]
| Study Name | Phase | n Patients | Tumor Types | Technical Success | Major Complications |
|---|---|---|---|---|---|
| Vidal-Jove et al., 2022 [34] | I | 8 | HCC, metastases | 100% | 0% |
| Wah et al., 2023 [35] | I/II | 44 tumors | HCC, CRLM, others | 95% | 7% |
| Wehrle et al., 2025 [36] | — | 230 | Broad spectrum | High (implied) | 1.3% |
| Category | Contraindications |
|---|---|
| Imaging Limitations | Deep tumors, overlying gas, obesity |
| Coagulopathy | Severe thrombocytopenia, uncorrectable coagulopathy |
| Tumor Type | Diffuse/infiltrative tumors, extensive liver burden |
| Liver Function | Advanced dysfunction (e.g., Child–Pugh class C) |
| Anatomical Risk | Tumors near GI tract, gallbladder |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paramythiotis, D.; Tsavdaris, D.; Tsavdaris, G.; Hatzidakis, A.; Psarras, K.; Mekras, A.; Georgiades, C.; Michalopoulos, A. Surgery Without Scalpel: Histotripsy as a Non-Invasive and Non-Thermal Modality for Liver Tumor Ablation. J. Clin. Med. 2025, 14, 6391. https://doi.org/10.3390/jcm14186391
Paramythiotis D, Tsavdaris D, Tsavdaris G, Hatzidakis A, Psarras K, Mekras A, Georgiades C, Michalopoulos A. Surgery Without Scalpel: Histotripsy as a Non-Invasive and Non-Thermal Modality for Liver Tumor Ablation. Journal of Clinical Medicine. 2025; 14(18):6391. https://doi.org/10.3390/jcm14186391
Chicago/Turabian StyleParamythiotis, Daniel, Dimitrios Tsavdaris, Georgios Tsavdaris, Adam Hatzidakis, Kyriakos Psarras, Alexandros Mekras, Christos Georgiades, and Antonios Michalopoulos. 2025. "Surgery Without Scalpel: Histotripsy as a Non-Invasive and Non-Thermal Modality for Liver Tumor Ablation" Journal of Clinical Medicine 14, no. 18: 6391. https://doi.org/10.3390/jcm14186391
APA StyleParamythiotis, D., Tsavdaris, D., Tsavdaris, G., Hatzidakis, A., Psarras, K., Mekras, A., Georgiades, C., & Michalopoulos, A. (2025). Surgery Without Scalpel: Histotripsy as a Non-Invasive and Non-Thermal Modality for Liver Tumor Ablation. Journal of Clinical Medicine, 14(18), 6391. https://doi.org/10.3390/jcm14186391







