Association Between Cardiovascular Disease and Complete Edentulism in U.S. Adults
Abstract
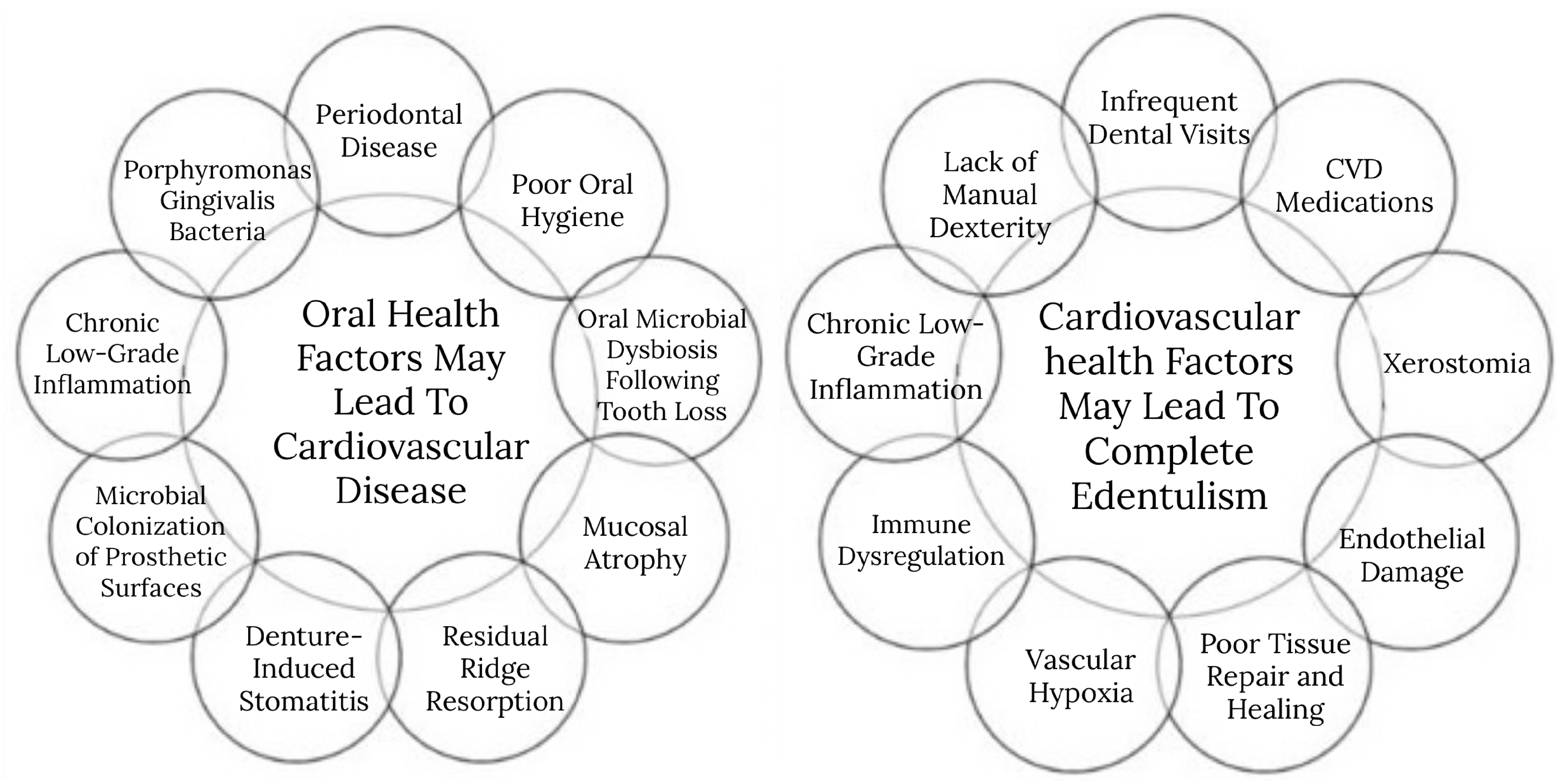
1. Introduction
2. Materials and Methods
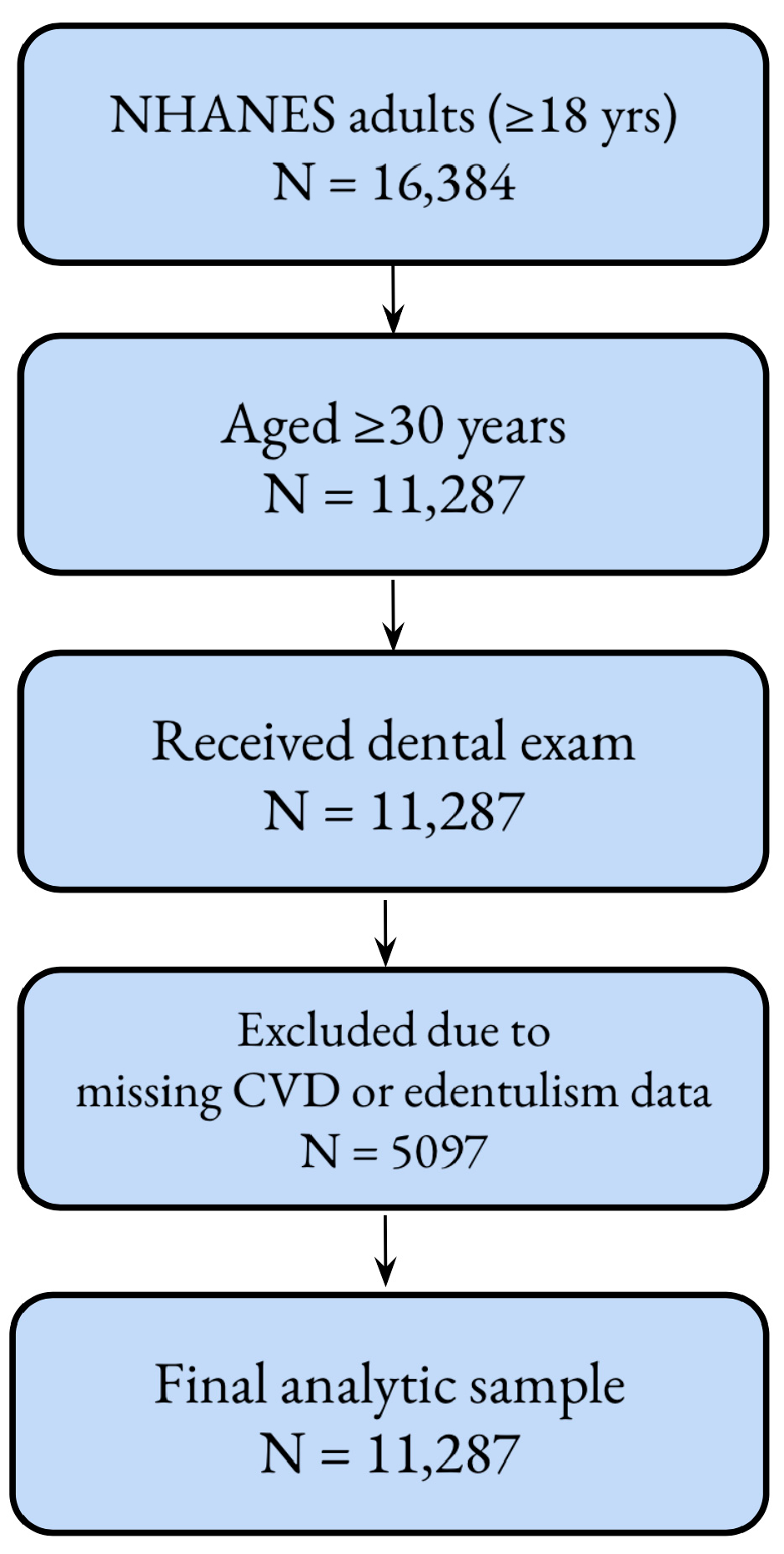
2.1. Study Population
2.2. Definition of the Dependent Variable: Complete Tooth Loss
2.3. Description of Independent Variable: CVD
2.4. Potential Confounding Variable
2.5. Statistical Methods
3. Results
4. Discussion
4.1. Limitations of Research
4.2. Future Perspectives
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CVD | Cardiovascular Disease |
| CHD | Coronary Heart Disease |
| MI | Myocardial Infarction |
| CHF | Congestive Heart Failure |
References
- Mendoza, M.F.; Anzelmo, M.A.; Suan, N.M.; Cuccia, C.S.; Lavie, C.J. More than Just a Toothache: Inflammatory Mechanisms Linking Periodontal Disease to Cardiovascular Disease and the Protective Impact of Cardiorespiratory Fitness. Biomedicines 2025, 13, 1512. [Google Scholar] [CrossRef]
- Watt, R.G.; Tsakos, G.; de Oliveira, C.; Hamer, M. Tooth Loss and Cardiovascular Disease Mortality Risk—Results from the Scottish Health Survey. PLoS ONE 2012, 7, e30797. [Google Scholar] [CrossRef]
- Bengtsson, V.W.; Persson, G.R.; Berglund, J.S.; Renvert, S. Periodontitis related to cardiovascular events and mortality: A long-time longitudinal study. Clin. Oral Investig. 2021, 25, 4085–4095. [Google Scholar] [CrossRef] [PubMed]
- American College of Prosthodontists. ACP Talking Points for Missing Teeth. 2015. Available online: https://www.prosthodontics.org/assets/1/7/ACP_Talking_points_for_Missing_Teeth_1-12-15.pdf (accessed on 20 May 2025).
- Holmstrup, P.; Damgaard, C.; Olsen, I.; Björn, K.; Allan, F.; Claus, H.; Nielsen, P.; Riis, H. Comorbidity of Periodontal Disease: Two Sides of the Same Coin? An Introduction for the Clinician. J. Oral Microbiol. 2017, 9, 1332710. [Google Scholar] [CrossRef] [PubMed]
- Romandini, M.; Baima, G.; Antonoglou, G.; Bueno, J.; Figuero, E.; Sanz, M. Periodontitis, Edentulism, and Risk of Mortality: A Systematic Review with Meta-Analyses. J. Dent. Res. 2021, 100, 37–49. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Gupta, A.; Peres, M.A.; Watt, R.G.; Tsakos, G.; Mathur, M.R. Association Between Tooth Loss and Hypertension Among a Primarily Rural Middle Aged and Older Indian Adult Population. J. Public Health Dent. 2016, 76, 198–205. [Google Scholar] [CrossRef]
- Taboza, Z.A.; Costa, K.L.; Silveira, V.R.; Furlaneto, F.A.; Montenegro, R., Jr.; Russell, S.; Dasanayake, A.; Rego, R.O. Periodontitis, edentulism and Glycemic Control in Patients with Type 2 Diabetes: A Cross-Sectional Study. BMJ Open Diabetes Res. Care 2018, 6, e000453. [Google Scholar] [CrossRef]
- Muñoz-Torres, F.J.; Mukamal, K.J.; Pai, J.K.; Willett, W.; Joshipura, K.J. Relationship between Tooth Loss and Peripheral Arterial Disease among Women. J. Clin. Periodontol. 2017, 44, 989–995. [Google Scholar] [CrossRef]
- Cheng, F.; Zhang, M.; Wang, Q.; Xu, H.; Dong, X.; Gao, Z.; Chen, J.; Wei, Y.; Qin, F. Tooth Loss and Risk of Cardiovascular Disease and Stroke: A Dose-Response Meta Analysis of Prospective Cohort Studies. PLoS ONE 2018, 13, e0194563. [Google Scholar] [CrossRef]
- Lee, H.J.; Choi, E.K.; Park, J.B.; Han, K.D.; Oh, S. Tooth Loss Predicts Myocardial Infarction, Heart Failure, Stroke, and Death. J. Dent. Res. 2019, 98, 164–170. [Google Scholar] [CrossRef]
- Goteiner, D.; Craig, R.G.; Ashmen, R.; Janal, M.N.; Eskin, B.; Lehrman, N. Endotoxin Levels are Associated with High-Density Lipoprotein, Triglycerides, and Troponin in Patients with Acute Coronary Syndrome and Angina: Possible Contributions from Periodontal Sources. J. Periodontol. 2008, 79, 2331–2339. [Google Scholar] [CrossRef] [PubMed]
- Nascimento, G.G.; Leite, F.R.; Conceição, D.A.; Ferrúa, C.P.; Singh, A.; Demarco, F.F. Is There a Relationship Between Obesity and Tooth Loss and Edentulism? A Systematic Review and Meta-Analysis. Obes. Rev. 2016, 17, 587–598. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.M.; Han, K.; Park, Y.G.; Park, J.B. Associations Between the Number of Natural Teeth and Renal Dysfunction. Medicine 2016, 95, e4681. [Google Scholar] [CrossRef] [PubMed]
- Barros, S.P.; Suruki, R.; Loewy, Z.G.; Beck, J.D.; Offenbacher, S. A Cohort Study of the Impact of Tooth Loss and Periodontal Disease on Respiratory Events Among COPD Subjects: Modulatory Role of Systemic Biomarkers of Inflammation. PLoS ONE 2013, 8, e68592. [Google Scholar] [CrossRef]
- Yoo, J.J.; Yoon, J.H.; Kang, M.J.; Kim, M.; Oh, N. The Effect of Missing Teeth on Dementia in Older People: A Nationwide Population-Based Cohort Study in South Korea. BMC Oral Health 2019, 19, 61. [Google Scholar] [CrossRef]
- Cademartori, M.G.; Gastal, M.T.; Nascimento, G.G.; Demarco, F.F.; Corrêa, M.B. Is Depression Associated with Oral Health Outcomes in Adults and Elders? A Systematic Review and Meta-Analysis. Clin. Oral Investig. 2018, 22, 2685–2702. [Google Scholar] [CrossRef]
- Saito, S.; Ohi, T.; Murakami, T.; Komiyama, T.; Miyoshi, Y.; Endo, K.; Satoh, M.; Asayama, K.; Inoue, R.; Kikuya, M.; et al. Association Between Tooth Loss and Cognitive Impairment in Community-Dwelling Older Japanese Adults: A 4-Year Prospective Cohort Study from the Ohasama Study. BMC Oral Health 2018, 18, 142. [Google Scholar] [CrossRef]
- Dembowska, E.; Jaroń, A.; Gabrysz-Trybek, E.; Bladowska, J.; Trybek, G. Evaluation of Common Factors of Periodontitis and Cardiovascular Disease in Patients with the Acute Coronary Syndrome. Int. J. Environ. Res. Public Health 2022, 19, 8139. [Google Scholar] [CrossRef]
- Dhungana, G.; Srisai, D.; Sampath, C.; Soliman, J.; Kelly, R.M.; Saleh, H.Y.; Sedik, A.; Raynes, E.; Ferguson, A.; Alluri, L.S.C.; et al. Unveiling the Molecular Crosstalk Between Periodontal and Cardiovascular Diseases: A Systematic Review. Dent. J. 2025, 13, 98. [Google Scholar] [CrossRef]
- Cardona-Mendoza, A.; Roa Molina, N.S.; Castillo, D.M.; Lafaurie, G.I.; Gualtero Escobar, D.F. Human Coronary Artery Endothelial Cell Response to Porphyromonas gingivalis W83 in a Collagen Three-Dimensional Culture Model. Microorganisms 2024, 12, 248. [Google Scholar] [CrossRef]
- Hashim, N.T.; Babiker, R.; Padmanabhan, V.; Ahmed, A.T.; Chaitanya, N.C.S.K.; Mohammed, R.; Priya, S.P.; Ahmed, A.; El Bahra, S.; Islam, M.S.; et al. The Global Burden of Periodontal Disease: A Narrative Review on Unveiling Socioeconomic and Health Challenges. Int. J. Environ. Res. Public Health 2025, 22, 624. [Google Scholar] [CrossRef] [PubMed]
- Bell, V.; Rodrigues, A.R.; Antoniadou, M.; Peponis, M.; Varzakas, T.; Fernandes, T. An Update on Drug–Nutrient Interactions and Dental Decay in Older Adults. Nutrients 2023, 15, 4900. [Google Scholar] [CrossRef] [PubMed]
- Schulze, A.; Kwast, S.; Pökel, C.; Busse, M. Assessment of the Relationship between Periodontitis and Cardiac Parameters in Patients with Early Chronic Heart Failure: A Cross-Sectional Study. J. Funct. Morphol. Kinesiol. 2024, 9, 52. [Google Scholar] [CrossRef] [PubMed]
- Rus, M.; Negruțiu, B.M.; Sava, C.N.; Pasca, G.; Andronie-Cioara, F.L.; Crisan, S.; Popescu, M.-I.; Staniș, C.E.; Judea Pusta, C. The Association Between Periodontal Disease and Acute Coronary Syndrome—A Clinical Analysis. J. Clin. Med. 2025, 14, 2447. [Google Scholar] [CrossRef]
- Nijakowski, K.; Jankowski, J.; Gruszczyński, D.; Surdacka, A. Salivary Alterations of Myeloperoxidase in Patients with Systemic Diseases: A Systematic Review. Int. J. Mol. Sci. 2023, 24, 12078. [Google Scholar] [CrossRef]
- Angjelova, A.; Jovanova, E.; Polizzi, A.; Laganà, L.; Santonocito, S.; Ragusa, R.; Isola, G. Impact of Periodontitis on Endothelial Risk Dysfunction and Oxidative Stress Improvement in Patients with Cardiovascular Disease. J. Clin. Med. 2024, 13, 3781. [Google Scholar] [CrossRef]
- Murray, P.E.; Coffman, J.A.; Garcia-Godoy, F. Oral Pathogens’ Substantial Burden on Cancer, Cardiovascular Diseases, Alzheimer’s, Diabetes, and Other Systemic Diseases: A Public Health Crisis—A Comprehensive Review. Pathogens 2024, 13, 1084. [Google Scholar] [CrossRef]
- Dash, G.; Mishra, L.; Singh, N.R.; Behera, R.; Misra, S.R.; Kumar, M.; Sokolowski, K.; Agarwal, K.; Behera, S.K.; Mishra, S.; et al. Prevalence and Quality of Endodontic Treatment in Patients with Cardiovascular Disease and Associated Risk Factors. J. Clin. Med. 2022, 11, 6046. [Google Scholar] [CrossRef]
- González-Ramírez, J.; Martínez-Coronilla, G.; López-Rocha, L.D.; Leija-Montoya, A.G.; Hernández-Díazcouder, A.; Fontes-Garcia, Z.; Silva-Mancilla, M.; Sánchez-Muñoz, F. Acute Myocardial Infarction and Periodontitis: Importance of Awareness and Prevention in Latin America. Appl. Sci. 2022, 12, 3131. [Google Scholar] [CrossRef]
- Casanova-Rosado, A.J.; Casanova-Rosado, J.F.; Minaya-Sánchez, M.; Robles-Minaya, J.L.; Casanova-Sarmiento, J.A.; Márquez-Corona, M.d.L.; Pontigo-Loyola, A.P.; Isla-Granillo, H.; Mora-Acosta, M.; Márquez-Rodríguez, S.; et al. Association of Edentulism with Various Chronic Diseases in Mexican Elders 60+ Years: Results of a Population-Based Survey. Healthcare 2021, 9, 404. [Google Scholar] [CrossRef]
- Janket, S.-J.; Kunhipurayil, H.H.; Tamimi, F.; Surakka, M.; Li, H.; Van Dyke, T.E.; Meurman, J.H. Edentulism or Poor Oral Hygiene: Which Is the Stronger Predictor for All-Cause Mortality? J. Clin. Med. 2025, 14, 371. [Google Scholar] [CrossRef] [PubMed]
- Szerszeń, M.; Górski, B.; Kowalski, J. Clinical Condition of the Oral Cavity in the Adult Polish Population below 70 Years of Age after Myocardial Infarction—A Case–Control Study. Int. J. Environ. Res. Public Health 2022, 19, 7265. [Google Scholar] [CrossRef] [PubMed]
- Czerniuk, M.R.; Surma, S.; Romańczyk, M.; Nowak, J.M.; Wojtowicz, A.; Filipiak, K.J. Unexpected Relationships: Periodontal Diseases: Atherosclerosis–Plaque Destabilization? From the Teeth to a Coronary Event. Biology 2022, 11, 272. [Google Scholar] [CrossRef] [PubMed]
- Cacciatore, S.; Spadafora, L.; Bernardi, M.; Galli, M.; Betti, M.; Perone, F.; Nicolaio, G.; Marzetti, E.; Martone, A.M.; Landi, F.; et al. Management of Coronary Artery Disease in Older Adults: Recent Advances and Gaps in Evidence. J. Clin. Med. 2023, 12, 5233. [Google Scholar] [CrossRef]
- National Center for Health Statistics. About the National Health and Nutrition Examination Survey. Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/nchs/nhanes/about/ (accessed on 11 December 2024).
- American Association of Oral and Maxillofacial Surgeons. Edentulism. MyOMS. Available online: https://myoms.org/what-we-%20do/dental-implant-surgery/edentulism/ (accessed on 11 December 2024).
- Shahi, S.; Farhoudi, M.; Dizaj, S.M.; Sharifi, S.; Sadigh-Eteghad, S.; Goh, K.W.; Ming, L.C.; Dhaliwal, J.S.; Salatin, S. The Link between Stroke Risk and Orodental Status—A Comprehensive Review. J. Clin. Med. 2022, 11, 5854. [Google Scholar] [CrossRef]
- Brahmbhatt, Y.; Zak, M.; Alhajri, R.; Almulla, N.; Alqallaf, S.; Alkandari, A.; Alsaleh, S.; Alqaderi, H. Association Between Ethylene Oxide Exposure and Complete Edentulism in United States Adults. Life 2025, 15, 740. [Google Scholar] [CrossRef]
- Iacob, S.; Chisnoiu, R.M.; Zaharia, A.; Bălaj, M.G.; Iosa, A.E.; Condor, A.-M.; Chisnoiu, A.; Buduru, S.D.; Kui, A. Correlation Between Type of Edentulism, Age, Socioeconomic Status and General Health. J. Clin. Med. 2025, 14, 3924. [Google Scholar] [CrossRef]
- Gabiec, K.; Bagińska, J.; Łaguna, W.; Rodakowska, E.; Kamińska, I.; Stachurska, Z.; Dubatówka, M.; Kondraciuk, M.; Kamiński, K.A. Factors Associated with Tooth Loss in General Population of Bialystok, Poland. Int. J. Environ. Res. Public Health 2022, 19, 2369. [Google Scholar] [CrossRef]
- D’Orto, B.; Tetè, G.; Nagni, M.; Visconti, R.F.; Polizzi, E.; Gherlone, E.F. Full Arch Implant-Prosthetic Rehabilitation in Patients with Cardiovascular Diseases: A 7-Year Follow-Up Prospective Single Cohort Study. J. Clin. Med. 2024, 13, 924. [Google Scholar] [CrossRef]
- Bassani, B.; Cucchiara, M.; Butera, A.; Kayali, O.; Chiesa, A.; Palano, M.T.; Olmeo, F.; Gallazzi, M.; Dellavia, C.P.B.; Mortara, L.; et al. Neutrophils’ Contribution to Periodontitis and Periodontitis-Associated Cardiovascular Diseases. Int. J. Mol. Sci. 2023, 24, 15370. [Google Scholar] [CrossRef]
- Sadek, K.M.; El Moshy, S.; Radwan, I.A.; Rady, D.; Abbass, M.M.S.; El-Rashidy, A.A.; Dörfer, C.E.; Fawzy El-Sayed, K.M. Molecular Basis beyond Interrelated Bone Resorption/Regeneration in Periodontal Diseases: A Concise Review. Int. J. Mol. Sci. 2023, 24, 4599. [Google Scholar] [CrossRef]
- Ferrara, E.; D’Albenzio, A.; Bassignani, J.; Di Tanna, I.; Murmura, G.; Balice, G. The Periodontal–Cardiovascular Disease Association: Molecular Mechanisms and Clinical Implications. Int. J. Mol. Sci. 2025, 26, 7710. [Google Scholar] [CrossRef]
- Deng, Y.; Xiao, J.; Ma, L.; Wang, C.; Wang, X.; Huang, X.; Cao, Z. Mitochondrial Dysfunction in Periodontitis and Associated Systemic Diseases: Implications for Pathomechanisms and Therapeutic Strategies. Int. J. Mol. Sci. 2024, 25, 1024. [Google Scholar] [CrossRef] [PubMed]
- Saha, S.; Sachivkina, N.; Lenchenko, E.; Pilshchikova, O.; Muraev, A. Activation of the Nrf2 Signaling Pathway as a Therapeutic Strategy Against Periodontal Disease: A Narrative Review. Dent. J. 2025, 13, 314. [Google Scholar] [CrossRef] [PubMed]
- Bhuyan, R.; Bhuyan, S.K.; Mohanty, J.N.; Das, S.; Juliana, N.; Juliana, I.F. Periodontitis and Its Inflammatory Changes Linked to Various Systemic Diseases: A Review of Its Underlying Mechanisms. Biomedicines 2022, 10, 2659. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, A.B.; Pizziolo, P.G.; Clemente, L.M.; Aguiar, H.C.; Poker, B.d.C.; Silva, A.A.M.e.; Makrakis, L.R.; Fifolato, M.A.; Souza, G.C.; Oliveira, V.d.C.; et al. Strategies for Preventing and Treating Oral Mucosal Infections Associated with Removable Dentures: A Scoping Review. Antibiotics 2024, 13, 273. [Google Scholar] [CrossRef]
- Desai, J.P.; Nair, R.U. Oral Health Factors Related to Rapid Oral Health Deterioration among Older Adults: A Narrative Review. J. Clin. Med. 2023, 12, 3202. [Google Scholar] [CrossRef]
- Cristina, N.M.; Lucia, D. Nutrition and Healthy Aging: Prevention and Treatment of Gastrointestinal Diseases. Nutrients 2021, 13, 4337. [Google Scholar] [CrossRef]
- Rotaru, M.; Singeap, A.-M.; Ciobica, A.; Huiban, L.; Stanciu, C.; Romila, L.; Burlui, V.; Mavroudis, I.; Trifan, A. Oral Health and “Modern” Digestive Diseases: Pathophysiologic and Etiologic Factors. Biomedicines 2024, 12, 1854. [Google Scholar] [CrossRef]
- Azzolino, D.; Carnevale-Schianca, M.; Bottalico, L.; Colella, M.; Felicetti, A.; Perna, S.; Terranova, L.; Garcia-Godoy, F.; Rondanelli, M.; Passarelli, P.C.; et al. The Oral–Gut Microbiota Axis as a Mediator of Frailty and Sarcopenia. Nutrients 2025, 17, 2408. [Google Scholar] [CrossRef]
- Alfakry, H.; Malle, E.; Koyani, C.N.; Pussinen, P.J.; Sorsa, T. Neutrophil proteolytic activation cascades: A possible mechanistic link between chronic periodontitis and coronary heart disease. Innate Immun. 2015, 22, 85–99. [Google Scholar] [CrossRef] [PubMed]
- Irwandi, R.A.; Chiesa, S.T.; Hajishengallis, G.; Papayannopoulos, V.; Deanfield, J.E.; D’Aiuto, F. The Roles of Neutrophils Linking Periodontitis and Atherosclerotic Cardiovascular Diseases. Front. Immunol. 2022, 13, 915081. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Saxena, A.; Yan, W.; Uriarte, S.M.; Siqueira, R.; Li, X. The impact of aging on neutrophil functions and the contribution to periodontitis. Int. J. Oral Sci. 2025, 17, 10. [Google Scholar] [CrossRef] [PubMed]
- Celik, D.; Kantarci, A. Vascular Changes and Hypoxia in Periodontal Disease as a Link to Systemic Complications. Pathogens 2021, 10, 1280. [Google Scholar] [CrossRef]
- Eldzharov, A.; Kabaloeva, D.; Nemeryuk, D.; Goncharenko, A.; Gatsalova, A.; Ivanova, E.; Kostritskiy, I.; Carrouel, F.; Bourgeois, D. Evaluation of Microcirculation, Cytokine Profile, and Local Antioxidant Protection Indices in Periodontal Health, and Stage II, Stage III Periodontitis. J. Clin. Med. 2021, 10, 1262. [Google Scholar] [CrossRef]
- Messina, B.M.; Grippaudo, C.; Polizzi, A.; Blasi, A.; Isola, G. The Key Role of Porphyromonas gingivalis in the Pathogenesis of Periodontitis Linked with Systemic Diseases. Appl. Sci. 2025, 15, 6847. [Google Scholar] [CrossRef]
- Mei, F.; Xie, M.; Huang, X.; Long, Y.; Lu, X.; Wang, X.; Chen, L. Porphyromonas gingivalis and Its Systemic Impact: Current Status. Pathogens 2020, 9, 944. [Google Scholar] [CrossRef]
- Park, H.-J.; Kim, Y.; Kim, M.-K.; Park, H.-R.; Kim, H.-J.; Bae, S.-K.; Bae, M.-K. Infection of Porphyromonas gingivalis Increases Phosphate-Induced Calcification of Vascular Smooth Muscle Cells. Cells 2020, 9, 2694. [Google Scholar] [CrossRef]
- Ramírez Martínez-Acitores, L.; Hernández Ruiz de Azcárate, F.; Casañas, E.; Serrano, J.; Hernández, G.; López-Pintor, R.M. Xerostomia and Salivary Flow in Patients Taking Antihypertensive Drugs. Int. J. Environ. Res. Public Health 2020, 17, 2478. [Google Scholar] [CrossRef]
- Pająk-Łysek, E.; Polak, M.; Kopeć, G.; Podolec, M.; Desvarieux, M.; Pająk, A.; Zarzecka, J. Associations Between Pharmacotherapy for Cardiovascular Diseases and Periodontitis. Int. J. Environ. Res. Public Health 2021, 18, 770. [Google Scholar] [CrossRef]
- Chan, A.K.Y.; Tamrakar, M.; Jiang, C.M.; Lo, E.C.M.; Leung, K.C.M.; Chu, C.-H. Common Medical and Dental Problems of Older Adults: A Narrative Review. Geriatrics 2021, 6, 76. [Google Scholar] [CrossRef] [PubMed]
- Religioni, U.; Barrios-Rodríguez, R.; Requena, P.; Borowska, M.; Ostrowski, J. Enhancing Therapy Adherence: Impact on Clinical Outcomes, Healthcare Costs, and Patient Quality of Life. Medicina 2025, 61, 153. [Google Scholar] [CrossRef] [PubMed]
- González-Zamora, M.; Ambrosio, N.; González, R.; Anguita, P.; Molina, A.; Herrera, D.; Sanz, M.; Marín, F.; Anguita-Gámez, M.; Ferrandis, R.; et al. Perioperative/Periprocedural Antithrombotic Management in Oral Health Procedures. A Prospective Observational Study. Dent. J. 2025, 13, 196. [Google Scholar] [CrossRef] [PubMed]
- Boccatonda, A.; Frisone, A.; Lorusso, F.; Bugea, C.; Di Carmine, M.; Schiavone, C.; Cocco, G.; D’Ardes, D.; Scarano, A.; Guagnano, M.T. Perioperative Management of Antithrombotic Therapy in Patients Who Undergo Dental Procedures: A Systematic Review of the Literature and Network Meta-Analysis. Int. J. Environ. Res. Public Health 2023, 20, 5293. [Google Scholar] [CrossRef]
- Chu, S.; Chu, C.H.; Chan, A.K.Y. Behavioural Change Interventions for Preventing Periodontal Disease in Older Adults: A Literature Review. Geriatrics 2025, 10, 97. [Google Scholar] [CrossRef]
- Chan, A.K.Y.; Tsang, Y.C.; Jiang, C.M.; Leung, K.C.M.; Lo, E.C.M.; Chu, C.H. Diet, Nutrition, and Oral Health in Older Adults: A Review of the Literature. Dent. J. 2023, 11, 222. [Google Scholar] [CrossRef]
| Independent Variable | With Dentition (n) | % | Complete Tooth Loss (n) | % | Total (n) | p Value | |
|---|---|---|---|---|---|---|---|
| Heart Disease * | No heart disease | 8583 | 84.5 | 1378 | 6.42 | 9961 | <0.0001 |
| Have heart disease | 941 | 7.33 | 385 | 1.76 | 1326 | ||
| Heart Attack (Myocardial Infarction (MI)) | Yes | 356 | 2.78 | 165 | 0.78 | 521 | <0.0001 |
| No | 9155 | 89.06 | 1593 | 7.42 | 10,748 | ||
| Coronary Heart Disease (CHD) | Yes | 349 | 3.08 | 160 | 0.74 | 509 | <0.0001 |
| No | 9147 | 88.78 | 1590 | 7.39 | 10,737 | ||
| Congestive Heart Failure (CHF) | Yes | 271 | 1.8 | 144 | 0.58 | 415 | <0.0001 |
| No | 9229 | 90.02 | 1616 | 7.61 | 10,845 | ||
| Stroke | Yes | 346 | 2.37 | 136 | 0.64 | 482 | <0.0001 |
| No | 9167 | 89.46 | 1624 | 7.52 | 10,791 | ||
| Gender | Male | 6963 | 42.21 | 2486 | 6.65 | 9449 | 0.5345 |
| Female | 7329 | 44.36 | 2447 | 6.78 | 9776 | ||
| Race/Ethnicity | Hispanic | 4065 | 15.14 | 1351 | 2.72 | 5416 | 0.00017 |
| White | 4474 | 52.46 | 1742 | 7.41 | 6216 | ||
| Black | 3221 | 10.22 | 1023 | 1.67 | 4244 | ||
| Asian | 1747 | 4.83 | 463 | 0.75 | 2210 | ||
| Others | 785 | 3.92 | 354 | 0.87 | 1139 | ||
| Age (in years) | 19–44 | 4345 | 32.54 | 455 | 1.38 | 4800 | <0.0001 |
| 45–59 | 2376 | 18.66 | 339 | 1.56 | 2715 | ||
| Above 60 | 3061 | 18.07 | 990 | 3.14 | 4051 | ||
| Education Level | 0–11 | 1931 | 10.8 | 550 | 2.13 | 2481 | <0.0001 |
| HS/Ged | 2118 | 21.46 | 443 | 2.48 | 2561 | ||
| >HS | 5466 | 59.58 | 762 | 3.55 | 6228 | ||
| Ratio of Family | <100%FPL | 2889 | 69.58 | 1263 | 30.42 | 4152 | |
| 100–99%FPL | 3564 | 74.46 | 1222 | 25.54 | 4786 | <0.0001 | |
| 200–399%FPL | 3382 | 77.18 | 1000 | 22.82 | 4382 | ||
| 400% + FPL | 2886 | 79.68 | 736 | 20.32 | 3622 | ||
| BMI | Underweight | 1877 | 7.61 | 1288 | 4.39 | 3165 | <0.0001 |
| Normal | 4268 | 26.16 | 453 | 1.97 | 4721 | ||
| Overweight | 3648 | 24.58 | 409 | 2.09 | 4057 | ||
| Obese | 4355 | 30.68 | 463 | 2.52 | 4818 | ||
| Diabetes | Yes | 1365 | 7.38 | 384 | 1.24 | 1749 | 0.0976 |
| No | 12,647 | 78.54 | 3737 | 10.99 | 16,384 | ||
| Borderline | 273 | 1.67 | 58 | 0.17 | 331 | ||
| Composite | ||||
|---|---|---|---|---|
| Covariate | Prevalence Ratio | Confidence Interval | p Value | |
| Lower | Upper | |||
| Heart attack (MI) * | 1.55 | 1.225 | 1.980 | 0.001 |
| Sex (reference: male) | 1.03 | 0.878 | 1.224 | 0.657 |
| Age (reference: 30–44) | ||||
| 45–59 | 2.10 | 1.558 | 2.848 | <0.001 |
| >60 | 3.70 | 2.576 | 5.326 | <0.001 |
| Education (reference: <high school) | ||||
| High school/GED | 0.70 | 0.580 | 0.859 | 0.001 |
| >High school | 0.46 | 0.380 | 0.556 | <0.001 |
| Poverty (reference: <100% FPL) | ||||
| 100–199% FPL | 0.93 | 0.740 | 1.178 | 0.554 |
| 200–399% FPL | 0.58 | 0.427 | 0.809 | 0.002 |
| 400% + FPL | 0.42 | 0.294 | 0.609 | <0.001 |
| Race (reference: Hispanic) | ||||
| Non-Hispanic White | 1.44 | 1.045 | 2.009 | 0.027 |
| Non-Hispanic Black | 1.50 | 1.109 | 2.051 | 0.010 |
| Non-Hispanic Asian | 1.77 | 1.198 | 2.624 | 0.006 |
| Other | 2.17 | 1.448 | 3.264 | <0.001 |
| Diabetes (reference: No Diabetes) | ||||
| Yes | 1.10 | 0.884 | 1.385 | 0.361 |
| Borderline | 1.09 | 0.729 | 1.654 | 0.641 |
| BMI (reference: Underweight) | ||||
| Normal | 0.75 | 0.298 | 1.893 | 0.533 |
| Overweight | 0.86 | 0.333 | 2.251 | 0.762 |
| Obese | 0.78 | 0.316 | 1.955 | 0.594 |
| Composite | ||||
|---|---|---|---|---|
| Covariate | Prevalence Ratio | Confidence Interval | p Value | |
| Lower | Upper | |||
| Heart Disease * | 1.53 | 1.280 | 1.842 | <0.001 |
| Sex (reference: male) | 1.03 | 0.879 | 1.215 | 0.676 |
| Age (reference: 30–44) | ||||
| 45–59 | 2.07 | 1.537 | 2.796 | <0.001 |
| >60 | 3.52 | 2.458 | 5.052 | <0.001 |
| Education (reference: <high school) | ||||
| High school/GED | 0.71 | 0.582 | 0.866 | 0.001 |
| >High school | 0.46 | 0.382 | 0.559 | <0.001 |
| Poverty (reference: <100% FPL) | ||||
| 100–199% FPL | 0.93 | 0.741 | 1.168 | 0.554 |
| 200–399% FPL | 0.59 | 0.431 | 0.813 | 0.002 |
| 400% + FPL | 0.43 | 0.301 | 0.619 | <0.001 |
| Race (reference: Hispanic) | ||||
| Non-Hispanic White | 1.41 | 1.016 | 1.962 | 0.040 |
| Non-Hispanic Black | 1.46 | 1.073 | 1.997 | 0.018 |
| Non-Hispanic Asian | 1.76 | 1.189 | 2.629 | 0.006 |
| Other | 2.14 | 1.413 | 3.242 | 0.001 |
| Diabetes (reference: No Diabetes) | ||||
| Yes | 1.06 | 0.851 | 1.335 | 0.562 |
| Borderline | 1.04 | 0.698 | 1.575 | 0.812 |
| BMI (reference: Underweight) | ||||
| Normal | 0.75 | 0.298 | 1.885 | 0.529 |
| Overweight | 0.85 | 0.329 | 2.232 | 0.746 |
| Obese | 0.77 | 0.313 | 1.915 | 0.569 |
| Composite | ||||
|---|---|---|---|---|
| Covariate | Prevalence Ratio | Confidence Interval | p Value | |
| Lower | Upper | |||
| Coronary Heart Disease | 1.44 | 1.132 | 1.853 | 0.004 |
| Sex (reference: male) | 1.02 | 0.872 | 1.210 | 0.739 |
| Age (reference: 30–44) | ||||
| 45–59 | 2.12 | 1.572 | 2.872 | <0.001 |
| >60 | 3.73 | 2.598 | 5.75 | <0.001 |
| Education (reference: <high school) | ||||
| High school/GED | 0.71 | 0.585 | 0.884 | 0.003 |
| >High school | 0.46 | 0.378 | 0.567 | <0.001 |
| Poverty (reference: <100% FPL) | ||||
| 100–199% FPL | 0.94 | 0.748 | 1.184 | 0.595 |
| 200–399% FPL | 0.58 | 0.425 | 0.809 | 0.002 |
| 400% + FPL | 0.42 | 0.294 | 0.605 | <0.001 |
| Race (reference: Hispanic) | ||||
| Non-Hispanic White | 1.43 | 1.025 | 2.001 | 0.036 |
| Non-Hispanic Black | 1.51 | 1.110 | 2.066 | 0.010 |
| Non-Hispanic Asian | 1.77 | 1.199 | 2.618 | 0.005 |
| Other | 2.22 | 1.468 | 3.356 | <0.001 |
| Diabetes (reference: No Diabetes) | ||||
| Yes | 1.11 | 0.877 | 1.408 | 0.367 |
| Borderline | 1.05 | 0.697 | 1.610 | 0.779 |
| BMI (reference: Underweight) | ||||
| Normal | 0.74 | 0.296 | 1.890 | 0.528 |
| Overweight | 0.85 | 0.325 | 2.225 | 0.734 |
| Obese | 0.78 | 0.315 | 1.959 | 0.596 |
| Composite | ||||
|---|---|---|---|---|
| Covariate | Prevalence Ratio | Confidence Interval | p Value | |
| Lower | Upper | |||
| Congestive Heart Failure | 1.58 | 1.216 | 2.067 | 0.001 |
| Sex (reference: male) | 1.01 | 0.862 | 1.193 | 0.858 |
| Age (reference: 30–44) | ||||
| 45–59 | 2.12 | 1.577 | 2.868 | <0.001 |
| >60 | 3.78 | 2.612 | 5.482 | <0.001 |
| Education (reference: <high school) | ||||
| High school/GED | 0.70 | 0.574 | 0.864 | 0.001 |
| >High school | 0.45 | 0.374 | 0.559 | <0.001 |
| Poverty (reference: <100% FPL) | ||||
| 100–199% FPL | 0.93 | 0.739 | 1.169 | 0.523 |
| 200–399% FPL | 0.58 | 0.425 | 0.809 | 0.002 |
| 400% + FPL | 0.42 | 0.295 | 0.607 | <0.001 |
| Race (reference: Hispanic) | ||||
| Non-Hispanic White | 1.45 | 1.041 | 2.019 | 0.029 |
| Non-Hispanic Black | 1.48 | 1.087 | 2.026 | 0.015 |
| Non-Hispanic Asian | 1.75 | 1.185 | 2.602 | 0.007 |
| Other | 2.25 | 1.494 | 3.407 | <0.001 |
| Diabetes (reference: No Diabetes) | ||||
| Yes | 1.10 | 0.872 | 1.391 | 0.403 |
| Borderline | 1.04 | 0.690 | 1.578 | 0.831 |
| BMI (reference: Underweight) | ||||
| Normal | 0.75 | 0.299 | 1.910 | 0.544 |
| Overweight | 0.86 | 0.329 | 2.256 | 0.756 |
| Obese | 0.78 | 0.315 | 1.933 | 0.582 |
| Composite | ||||
|---|---|---|---|---|
| Covariate | Prevalence Ratio | Confidence Interval | p Value | |
| Lower | Upper | |||
| Stroke | 1.46 | 1.133 | 1.898 | 0.005 |
| Sex (reference: male) | 1.01 | 0.860 | 1.198 | 0.858 |
| Age (reference: 30–44) | ||||
| 45–59 | 2.13 | 1.583 | 2.872 | <0.001 |
| >60 | 3.80 | 2.636 | 5.486 | <0.001 |
| Education (reference: <high school) | ||||
| High school/GED | 0.70 | 0.574 | 0.864 | 0.001 |
| >High school | 0.46 | 0.378 | 0.560 | <0.001 |
| Poverty (reference: <100% FPL) | ||||
| 100–199% FPL | 0.93 | 0.743 | 1.179 | 0.565 |
| 200–399% FPL | 0.58 | 0.426 | 0.811 | 0.002 |
| 400% + FPL | 0.42 | 0.296 | 0.607 | <0.001 |
| Race (reference: Hispanic) | ||||
| Non-Hispanic White | 1.45 | 1.046 | 2.027 | 0.027 |
| Non-Hispanic Black | 1.49 | 1.095 | 2.047 | 0.013 |
| Non-Hispanic Asian | 1.78 | 1.204 | 2.646 | 0.005 |
| Other | 2.24 | 1.480 | 3.404 | <0.001 |
| Diabetes (reference: No Diabetes) | ||||
| Yes | 1.10 | 0.878 | 1.384 | 0.387 |
| Borderline | 1.04 | 0.703 | 1.565 | 0.807 |
| BMI (reference: Underweight) | ||||
| Normal | 0.73 | 0.292 | 1.825 | 0.490 |
| Overweight | 0.83 | 0.322 | 2.162 | 0.701 |
| Obese | 0.76 | 0.310 | 1.898 | 0.556 |
| Composite | ||||
|---|---|---|---|---|
| Covariate | Prevalence Ratio | Confidence Interval | p Value | |
| Lower | Upper | |||
| Heart Disease * | 1.53 | 1.280 | 1.842 | <0.001 |
| Heart Attack (MI) | 1.55 | 0.878 | 1.224 | 0.657 |
| Coronary Heart Disease | 1.44 | 1.132 | 1.853 | 0.004 |
| Congestive Heart Failure | 1.58 | 1.216 | 2.067 | 0.001 |
| Stroke | 1.46 | 1.133 | 1.898 | 0.005 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alyahya, S.; Hamoud, B.; Alqattan, A.; Almasoud, M.; Almehjan, Y.; Alajmi, R.; Alhazmi, H.; Alqaderi, H. Association Between Cardiovascular Disease and Complete Edentulism in U.S. Adults. J. Clin. Med. 2025, 14, 6035. https://doi.org/10.3390/jcm14176035
Alyahya S, Hamoud B, Alqattan A, Almasoud M, Almehjan Y, Alajmi R, Alhazmi H, Alqaderi H. Association Between Cardiovascular Disease and Complete Edentulism in U.S. Adults. Journal of Clinical Medicine. 2025; 14(17):6035. https://doi.org/10.3390/jcm14176035
Chicago/Turabian StyleAlyahya, Saud, Basel Hamoud, Ali Alqattan, Masoud Almasoud, Yousef Almehjan, Rashed Alajmi, Hesham Alhazmi, and Hend Alqaderi. 2025. "Association Between Cardiovascular Disease and Complete Edentulism in U.S. Adults" Journal of Clinical Medicine 14, no. 17: 6035. https://doi.org/10.3390/jcm14176035
APA StyleAlyahya, S., Hamoud, B., Alqattan, A., Almasoud, M., Almehjan, Y., Alajmi, R., Alhazmi, H., & Alqaderi, H. (2025). Association Between Cardiovascular Disease and Complete Edentulism in U.S. Adults. Journal of Clinical Medicine, 14(17), 6035. https://doi.org/10.3390/jcm14176035






