One Year After Mild COVID-19: Emotional Distress but Preserved Cognition in Healthcare Workers
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Neuropsychological Assessments
2.3. Emotional Measures and Subjective Complaints
2.4. Procedure
2.5. Statistical Analysis
3. Results
3.1. Descriptive Analysis
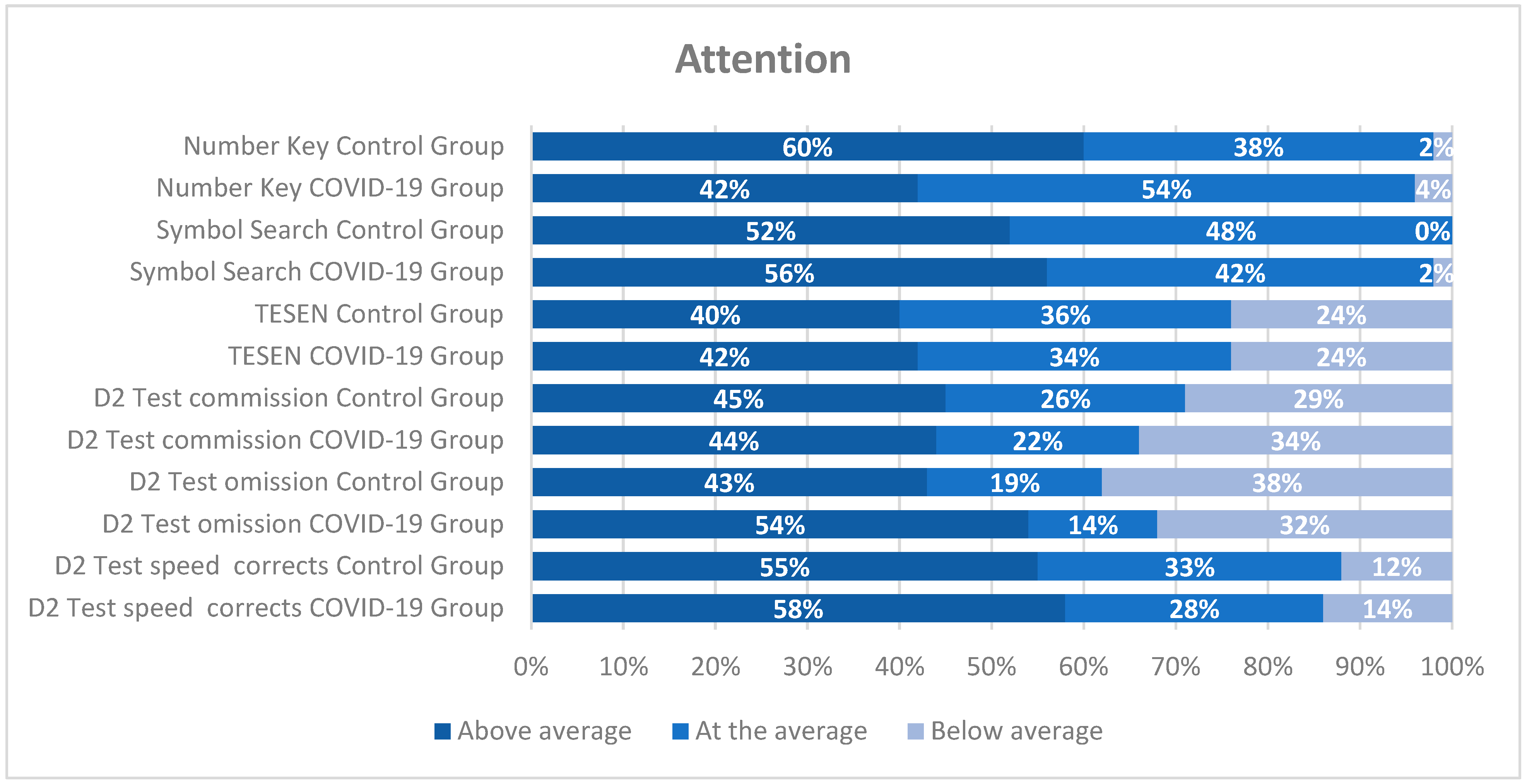
3.2. Analyses of Neuropsychological Measures
3.3. Analyses of Emotional Symptomatology and Subjective Complaints
3.4. Relationship Between Neuropsychological Tests and Emotional Symptomatology
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BADS | Behavioral Assessment of the Dysexecutive Syndrome |
| COVID-19 | Coronavirus Disease 2019 |
| CoVs | Coronavirus |
| HUFA | University Hospital Alcorcon Foundation |
| ISP-20 | Prefrontal Symptom Inventory |
| MBI | Maslach’s Burnout Inventory |
| MFE-30 | Failures in Everyday Life Questionnaire |
| MoCA | Montreal Cognitive Assessment |
| PCL | Post-Traumatic Stress Checklist–Civilian |
| PHQ-9 | Patient Health Questionnaire-9 |
| SARS-CoV-2 | Severe acute respiratory syndrome coronavirus 2 |
| SCL-90 | Symptom Checklist-90 |
| STAI | State-Trait Anxiety Inventory |
| TESEN | The Test of the Paths |
| TMT | Trail Making Test |
| WAIS-IV | Wechsler Intelligence Scale for Adults-IV |
| WMS-III | Wechsler Memory Scale III |
Appendix A
| Test/Subtest | Cognitive Function | Description |
|---|---|---|
| D2 Sustained Attention Test | Sustained and selective attention, processing speed | This test evaluates the ability to maintain attention and discriminate stimuli and provides concentration and processing speed indices. |
| TESEN (Test of the Paths, TMT-based) | Switching attention, cognitive flexibility | This test assesses task switching, sequential planning, and processing speed; errors and time in the task indicate flexibility efficiency. |
| Symbol Searching and Number Key (WAIS-IV) | Processing speed, visuomotor coordination | Processing speed and visual scanning are the abilities used to successfully accomplish these tests; the combined scores of both provide the Processing Speed Index. |
| Word Lists I and II, Faces I and II (WMS-III) | Verbal and visual memory | These instruments evaluate learning, retention, and recognition of verbal and visual information; they assess immediate and delayed memory. |
| Vocabulary (WAIS-IV) | Semantic memory, verbal reasoning | The vocabulary test is designed to evaluate verbal comprehension and semantic memory. |
| Rey–Osterrieth Complex Figure Test | Visuospatial construction, visual memory, planning | Through copying and recalling a complex figure, this test assesses visuospatial organization and memory. |
| Five Digit Test | Executive functions, inhibition, flexibility | This instrument measures inhibition and cognitive flexibility through four subtests: reading, counting, selection, and switching. It provides two indices: inhibition and flexibility. |
| Digit Span, Spatial Span, Letter–Number Sequencing (WMS-III) | Working memory | This test assesses verbal and visuospatial working memory through the ability to maintain and manipulate information. |
| Similarities (WAIS-IV) | Verbal reasoning, abstraction | This test assesses reasoning by comparing concepts and forming abstract judgments. |
| FAS Test | Verbal fluency | This test measures semantic word retrieval, spontaneous flexibility, and semantic memory organization. |
| Key Search and Zoo (BADS) | Planning, problem-solving, executive functions | This instrument evaluates successful strategies to find lost keys inside a closed space, presented as a square on a sheet of paper, as an evaluation of planning, behavioral monitoring, and problem-solving. |
References
- World Health Organization. A Clinical Case Definition of Post COVID-19 Condition by a Delphi Consensus; WHO: Geneva, Switzerland, 2024. [Google Scholar]
- Hu, B.; Guo, H.; Zhou, P.; Shi, Z.L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021, 19, 141–154. [Google Scholar] [CrossRef]
- Bailey, E.K.; Steward, K.A.; VandenBussche Jantz, A.B.; Kamper, J.E.; Mahoney, E.J.; Duchnick, J.J. Neuropsychology of COVID-19: Anticipated cognitive and mental health outcomes. Neuropsychology 2021, 35, 335–351. [Google Scholar] [CrossRef]
- Boldrini, M.; Canoll, P.; Klein, R.S. How COVID-19 affects the brain. JAMA Psychiatry 2021, 78, 682–683. [Google Scholar] [CrossRef]
- Zhao, S.; Toniolo, S.; Hampshire, A.; Husain, M. Effects of COVID-19 on cognition and brain health. Trends Cogn. Sci. 2023, 27, 1053–1067. [Google Scholar] [CrossRef] [PubMed]
- Maiese, A.; Manetti, A.C.; Bosetti, C.; Del Duca, F.; La Russa, R.; Frati, P.; Di Paolo, M.; Turillazzi, E.; Fineschi, V. SARS-CoV-2 and the brain: A review of neuropathology in COVID-19. Brain Pathol. 2021, 31, e13013. [Google Scholar] [CrossRef] [PubMed]
- Ollila, H.; Pihlaja, R.; Koskinen, S.; Tuulio Henriksson, A.; Salmela, V.; Tiainen, M.; Hokkanen, L. Long term cognitive functioning is impaired in ICU treated COVID-19 patients: A comprehensive neuropsychological study. Crit. Care 2022, 26, 92. [Google Scholar] [CrossRef] [PubMed]
- Becker, J.H.; Lin, J.J.; Doernberg, M.; Stone, K.; Navis, A.; Festa, J.R.; Wisnivesky, J.P. Assessment of Cognitive Function in Patients after COVID-19 Infection. JAMA Netw. Open 2021, 4, e2130645. [Google Scholar] [CrossRef]
- Daroische, R.; Hemminghyth, M.S.; Eilertsen, T.H.; Breitve, M.H.; Chwiszczuk, L.J. Cognitive impairment after COVID-19—A review on objective test data. Front. Neurol. 2021, 12, 699582. [Google Scholar] [CrossRef]
- Hampshire, A.; Trender, W.; Chamberlain, S.R.; Jolly, A.E.; Grant, J.E.; Patrick, F.; Mazibuko, N.; Williams, S.C.; Barnby, J.M.; Hellyer, P.; et al. Cognitive deficits in people who have recovered from COVID-19. EClinicalMedicine 2021, 39, 101044. [Google Scholar] [CrossRef]
- Ceban, F.; Ling, S.; Lui, L.M.W.; Lee, Y.; Gill, H.; Teopiz, K.M.; Rodrigues, N.B.; Subramaniapillai, M.; Di Vincenzo, J.D.; Cao, B.; et al. Fatigue and cognitive impairment in Post COVID-19 syndrome: A systematic review and meta analysis. Brain Behav. Immun. 2022, 101, 93–135. [Google Scholar] [CrossRef]
- Crivelli, L.; Palmer, K.; Calandri, I.; Guekht, A.; Beghi, E.; Carroll, W.; Frontera, J.; García-Azorín, D.; Westenberg, E.; Winkler, A.S.; et al. Changes in cognitive functioning after COVID-19: A systematic review and meta analysis. Alzheimer's Dement. 2022, 18, 1047–1066. [Google Scholar] [CrossRef]
- Tavares Júnior, J.W.L.; de Souza, A.C.C.; Borges, J.W.P.; Oliveira, D.N.; Siqueira Neto, J.I.; Sobreira Neto, M.A.; Braga-Neto, P. COVID-19 associated cognitive impairment: A systematic review. Cortex 2022, 152, 77–97. [Google Scholar] [CrossRef]
- Ferrucci, R.; Dini, M.; Rosci, C.; Capozza, A.; Groppo, E.; Reitano, M.R.; Allocco, E.; Poletti, B.; Brugnera, A.; Bai, F.; et al. One year cognitive follow up of COVID-19 hospitalized patients. Eur. J. Neurol. 2022, 29, 2006–2014. [Google Scholar] [CrossRef] [PubMed]
- Miskowiak, K.W.; Johnsen, S.; Sattler, S.M.; Nielsen, S.; Kunalan, K.; Rungby, J.; Lapperre, T.; Porsberg, C. Cognitive impairments four months after COVID-19 hospital discharge. Eur. Neuropsychopharmacol. 2021, 46, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Román, F.; Calandri, I.L.; Caridi, A.; Carosella, M.A.; Palma, P.A.; Llera, J.J.; Bartoloni, L.-C.; Sanz, P.; Mouchet, M.-E.; Fernandez-Díaz, P.-C.; et al. Consecuencias neurológicas y psiquiátricas a largo plazo (6 meses) en pacientes con COVID leve de la comunidad. J. Appl. Cogn. Neurosci. 2022, 3, e00264623. [Google Scholar] [CrossRef]
- Mattioli, F.; Stampatori, C.; Righetti, F.; Sala, E.; Tomasi, C.; De Palma, G. Neurological and cognitive sequelae of COVID-19: A four month follow up. J. Neurol. 2021, 268, 4422–4426. [Google Scholar] [CrossRef]
- Mazza, M.G.; Palladini, M.; De Lorenzo, R.; Magnaghi, C.; Poletti, S.; Furlan, R.; Ciceri, F.; Rovere-Querini, P.; Benedetti, F. Persistent psychopathology and neurocognitive impairment in COVID-19 survivors: Effect of inflammatory biomarkers at three month follow up. Brain Behav. Immun. 2021, 94, 138–147. [Google Scholar] [CrossRef] [PubMed]
- García Iglesias, J.J.; Gómez Salgado, J.; Martín Pereira, J.; Fagundo Rivera, J.; Ayuso Murillo, D.; Martínez Riera, J.R.; Ruiz Frutos, C. Impacto del SARS-CoV-2 en la salud mental de los profesionales sanitarios: Una revisión sistemática. Rev. Española Salud Pública 2020, 94, e202004011. [Google Scholar]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef]
- World Health Organization. International Classification of Diseases 11th Revision (ICD-11); World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Arnsten, A.F.T.; Shanafelt, T. Physician distress and burnout: The neurobiological perspective. Mayo Clin. Proc. 2021, 96, 763–769. [Google Scholar] [CrossRef]
- Batra, K.; Singh, T.P.; Sharma, M.; Batra, R.; Schvaneveldt, N. Investigating the psychological impact of COVID-19 among healthcare workers: A meta analysis. Int. J. Environ. Res. Public Health 2020, 17, 9239. [Google Scholar] [CrossRef]
- Carmassi, C.; Dell’Oste, V.; Bui, E.; Foghi, C.; Bertelloni, C.A.; Atti, A.R.; Buselli, R.; Di Paolo, M.; Goracci, A.; Malacarne, P.; et al. The interplay between acute post traumatic stress, depressive and anxiety symptoms among healthcare workers during the COVID-19 emergency. J. Affect. Disord. 2022, 298, 209–216. [Google Scholar] [CrossRef]
- García Gómez, M.; Gherasim, A.M.; Roldán Romero, J.M.; Montoya Martínez, L.; Oliva Domínguez, J.; Escalona López, S. COVID-19 related temporary disability in healthcare workers in Spain during the four first pandemic waves. Prev. Med. Rep. 2024, 43, 102779. [Google Scholar] [CrossRef]
- Sylvain, R.; Gilbertson, H.; Carlson, J.M. Single session positive attention bias modification training enhances reward-related electrocortical responses in females. Int. J. Psychophysiol. 2020, 156, 10–17. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Brickenkamp, R.; Zillmer, E. Test de Atención d2 (D2 Test); TEA Ediciones: Madrid, Spain, 2002. [Google Scholar]
- Portellano, J.A.; Martínez-Arias, R. Test de los Senderos Para la Evaluación de las Funciones Ejecutivas; TEA Ediciones: Madrid, Spain, 2014. [Google Scholar]
- Reitan, R.M. Trail Making Test: Manual for Administration and Scoring; Reitan Neuropsychology Laboratory: Tucson, AZ, USA, 1992. [Google Scholar]
- Wechsler, D. WAIS-IV: Escala de Inteligencia de Wechsler Para Adultos-IV; Pearson: Madrid, Spain, 2012. [Google Scholar]
- Pereña, J.; Seisdedos, N.; Corral, S.; Arribas-Aguila, D.; Santamaría, P.; Sueiro, M. WMS-III. Wechsler Memory Scale-III (Spanish Adaptation); Pearson: Madrid, Spain, 2004. [Google Scholar]
- Wechsler, D. WMS-III: Escala de Memoria de Wechsler-III; Pearson: Madrid, Spain, 2004. [Google Scholar]
- Jerskey, B.A. Meyers JERey complex figure test. In Encyclopedia of Clinical Neuropsychology; Kreutzer, J.S., DeLuca, J., Caplan, B., Eds.; Springer: New York, NY, USA, 2011; pp. 2176–2179. [Google Scholar] [CrossRef]
- Sedó, M.A. Five Digit Test (Test de Los Cinco Dígitos); TEA Ediciones: Madrid, Spain, 2007. [Google Scholar]
- Patterson, J. F-A-S test. In Encyclopedia of Clinical Neuropsychology; Kreutzer, J.S., DeLuca, J., Caplan, B., Eds.; Springer: New York, NY, USA, 2011. [Google Scholar]
- Norris, G.; Tate, R.L. The Behavioural Assessment of the Dysexecutive Syndrome (BADS): Ecological, concurrent and construct validity. Neuropsychol. Rehabil. 2000, 10, 33–45. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Spielberger, C.D.; Gorsuch, R.L.; Lushene, R.E. Manual for the State-Trait Anxiety Inventory; Consulting Psychologists Press: Palo Alto, CA, USA, 1970. [Google Scholar]
- Derogatis, L.R. SCL-90-R: Administration, Scoring and Procedures Manual-II; Clinical Psychometric Research: Baltimore, MD, USA, 1992. [Google Scholar]
- Weathers, F.W.; Litz, B.T.; Herman, D.S.; Huska, J.A.; Keane, T.M. The PTSD Checklist (PCL); National Center for PTSD: San Antonio, TX, USA, 1993. [Google Scholar]
- Seisdedos, N. Manual MBI, Inventario Burnout de Maslach; TEA Ediciones: Madrid, Spain, 1997. [Google Scholar]
- Carrasco, P.M.; Peña, M.M.; Sueiro, M.J. The Memory Failures of Everyday Questionnaire (MFE-30): Internal consistency and reliability. Span. J. Psychol. 2012, 15, 768–776. [Google Scholar] [CrossRef]
- Pedrero-Pérez, E.J.; Ruiz-Sánchez de León, J.M. Quejas subjetivas de memoria, personalidad y sintomatología prefrontal en adultos jóvenes. Rev. Neurol. 2013, 57, 289–296. [Google Scholar] [CrossRef]
- Czerwińska, A.; Pawłowski, T. Cognitive dysfunctions in depression—Significance, description and treatment prospects. Psychiatr Pol. 2020, 54, 453–466. [Google Scholar] [CrossRef] [PubMed]
- Diana, L.; Regazzoni, R.; Sozzi, M.; Piconi, S.; Borghesi, L.; Lazzaroni, E.; Basilico, P.; Aliprandi, A.; Bolognini, N.; Bonardi, D.R.; et al. Monitoring cognitive and psychological alterations in COVID-19 patients: A longitudinal neuropsychological study. J. Neurol. Sci. 2023, 444, 120511. [Google Scholar] [CrossRef]
- Blazhenets, G.; Schroeter, N.; Bormann, T.; Thurow, J.; Wagner, D.; Frings, L.; Weiller, C.; Meyer, P.T.; Dressing, A.; Hosp, J.A. Slow but evident recovery from neocortical dysfunction and cognitive impairment in a series of chronic COVID-19 patients. J. Nucl. Med. 2021, 62, 910–915. [Google Scholar] [CrossRef]
- Cecchetti, G.; Agosta, F.; Canu, E.; Basaia, S.; Barbieri, A.; Cardamone, R.; Bernasconi, M.P.; Castelnovo, V.; Cividini, C.; Cursi, M.; et al. Cognitive, EEG, and MRI features of COVID-19 survivors: A 10-month study. J. Neurol. 2022, 269, 3400–3412. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, J.; Gerardo, B.; Santana, I.; Simões, M.R.; Freitas, S. The assessment of cognitive reserve: A systematic review of the most used quantitative measurement methods of cognitive reserve for aging. Front. Psychol. 2022, 13, 847186. [Google Scholar] [CrossRef]
- Vance, D.E.; Bail, J.; Enah, C.; Palmer, J.; Hoenig, A. The impact of employment on cognition and cognitive reserve: Implications across diseases and aging. Nurs. Res. Rev. 2016, 6, 61–71. [Google Scholar] [CrossRef]
- Foreman, L.; Child, B.; Saywell, I.; Collins-Praino, L.; Baetu, I. Cognitive reserve moderates the effect of COVID-19 on cognition: A systematic review and meta-analysis of individual participant data. Neurosci. Biobehav. Rev. 2025, 171, 106067. [Google Scholar] [CrossRef]
- Panico, F.; Luciano, S.M.; Sagliano, L.; Santangelo, G.; Trojano, L. Cognitive reserve and coping strategies predict the level of perceived stress during COVID-19 pandemic: A cross-sectional study. Pers. Individ. Differ. 2022, 190, 111703. [Google Scholar] [CrossRef]
- Favaretto, E.; Bedani, F.; Brancati, G.E.; De Berardis, D.; Giovannini, S.; Scarcella, L.; Martiadis, V.; Martini, A.; Pampaloni, I.; Perugi, G.; et al. Synthesising 30 years of clinical experience and scientific insight on affective temperaments in psychiatric disorders: State of the art. J. Affect. Disord. 2024, 362, 406–415. [Google Scholar] [CrossRef]
- Rock, P.L.; Roiser, J.P.; Riedel, W.J.; Blackwell, A.D. Cognitive impairment in depression: A systematic review and meta-analysis. Psychol. Med. 2014, 44, 2029–2040. [Google Scholar] [CrossRef]
- Usala, P.D.; Hertzog, C. Evidence of differential stability of state and trait anxiety in adults. J. Pers. Soc. Psychol. 1991, 60, 471–479. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.E.C.; Ling, M.; Boyd, L.; Olsson, C.; Sheen, J. The prevalence of probable mental health disorders among hospital healthcare workers during COVID-19: A systematic review and meta-analysis. J. Affect. Disord. 2023, 330, 329–345. [Google Scholar] [CrossRef] [PubMed]
- Bueno Ferrán, M.; Barrientos-Trigo, S. Caring for the caregiver: The emotional impact of the coronavirus epidemic on nurses and other health professionals. Enferm. Clin. 2021, 31 (Suppl. 1), S35–S39. [Google Scholar] [CrossRef] [PubMed]
- Koutsimani, P.; Montgomery, A. Burnout and cognitive functioning: Are we underestimating the role of visuospatial functions? Front. Psychiatry 2022, 13, 775606. [Google Scholar] [CrossRef] [PubMed]
- Acheson, D.T.; Gresack, J.E.; Risbrough, V.B. Hippocampal dysfunction effects on context memory: Possible etiology for posttraumatic stress disorder. Neuropharmacology 2012, 62, 674–685. [Google Scholar] [CrossRef]
- Bakusic, J.; Schaufeli, W.; Claes, S.; Godderis, L. Stress, burnout and depression: A systematic review on DNA methylation mechanisms. J. Psychosom. Res. 2017, 92, 34–44. [Google Scholar] [CrossRef]
- Boniol, M.; McIsaac, M.; Xu, L.; Wuliji, T.; Diallo, K.; Campbell, J. Gender Equity in the Health Workforce: Analysis of 104 Countries. World Health Organization. 2019. Available online: https://iris.who.int/handle/10665/311314 (accessed on 16 August 2025).



| Variables | Percentage or Mean (SD) | Group Effect | ||
|---|---|---|---|---|
| Control Group | COVID-19 Group | Statistic t or χ2 | p-Value | |
| Age (years) | 44.24 (11.23) | 45.18 (10.49) | −0.415 | 0.679 |
| Education | 0.393 | 0.822 | ||
| Intermediate studies (%) | 33.3 | 32.0 | ||
| Advanced vocational qualification (%) | 4.8 | 8.0 | ||
| University studies (%) | 61.9 | 60.0 | ||
| Profession | 7.640 | 0.054 | ||
| Physician (%) | 16.7 | 6.0 | ||
| Nurse (%) | 54.8 | 80.0 | ||
| Physiotherapist (%) | 14.3 | 4.0 | ||
| Other (%) | 14.3 | 10.0 | ||
| Time since COVID-19 symptoms (months) | - | 13 (3.82) | ||
| COVID-19 Symptoms | ||||
| Fever (%) | - | 72.0 | ||
| Dry cough (%) | - | 66.0 | ||
| Tiredness (%) | - | 90.0 | ||
| Aches and pains (%) | - | 78.0 | ||
| Sore throat (%) | - | 52.0 | ||
| Diarrhea (%) | - | 32.0 | ||
| Conjunctivitis (%) | - | 6.0 | ||
| Headache (%) | - | 84.0 | ||
| Loss of smell (%) | - | 70.0 | ||
| Loss of taste (%) | - | 64.0 | ||
| Dysgeusia (%) | - | 34.0 | ||
| Skin rash or loss of pain (%) | - | 14.0 | ||
| Difficulty breathing or feeling shortness of breath (%) | - | 48.0 | ||
| Chest pain or pressure (%) | - | 46.0 | ||
| Inability to speak or move (%) | - | 8.0 | ||
| Vomiting or nausea (%) | - | 22.0 | ||
| Itchy skin (%) | - | 12.0 | ||
| Feeling dizzy (%) | - | 32.0 | ||
| Syncope (%) | - | 4.0 | ||
| Confusion (%) | - | 10.0 | ||
| Neuropsychological Tests | COVID-19 Group | Control Group | Statistics (df = 1.90) |
|---|---|---|---|
| Attention | |||
| D2 Test | |||
| Scanning speed | 432.38 (87.494) | 434.83 (81.874) | F = 0.018, p = 0.895 |
| Scanning accuracy | 170.10 (43.239) | 165.55 (38.952) | F = 0.277, p = 0.600 |
| Omission | 12.52 (10.300) | 17.31 (14.146) | F = 3.516, p = 0.064 |
| Commission | 7.90 (4.807) | 2.45 (4.915) | F = 1.957, p = 0.165 |
| Effectiveness index | 412.48 (82.240) | 406.93 (86.358) | F = 0.099, p = 0.753 |
| Concentration index | 162.18 (37.307) | 163.10 (40.975) | F = 0.013, p = 0.911 |
| Max | 36.96 (6.114) | 36.76 (5.656) | F = 0.026, p = 0.873 |
| Min | 25.14 (7.709) | 24.40 (6.950) | F = 0.227, p = 0.635 |
| Variation index | 12.04 (4.882) | 12.36 (5.093) | F = 0.093, p = 0.762 |
| TESEN | |||
| Path 1 execution | 27.01 (7.695) | 28.67 (5.549) | F = 1.357, p = 0.247 |
| Path 1 speed | 92.88 (25.749) | 86.21 (20.290) | F = 1.849, p = 0.177 |
| Path 1 accuracy | 98.59 (2.840) | 98.98 (2.473) | F = 0.499, p = 0.482 |
| Path 2 execution | 25.01 (6.653) | 26.56 (6.200) | F = 1.305, p = 0.256 |
| Path 2 speed | 99.46 (25.565) | 94.36 (29.597) | F = 0.787, p = 0.377 |
| Path 2 accuracy | 98.33 (3.039) | 98.23 (3.553) | F = 0.018, p = 0.893 |
| Path 3 execution | 18.31 (4.567) | 18.89 (4.371) | F = 0.388, p = 0.535 |
| Path 3 speed | 106.54 (36.249) | 99.81 (25.072) | F = 1.032, p = 0.312 |
| Path 3 accuracy | 95.96 (10.791) | 95.69 (7.221) | F = 0.018, p = 0.894 |
| Path 4 execution | 15.88 (19.016) | 14.39 (4.271) | F = 0.250, p = 0.619 |
| Path 4 speed | 144.02 (3.759) | 139.19 (40.697) | F = 0.027, p = 0.555 |
| Path 4 accuracy | 95.51 (13.201) | 98.04 (3.387) | F = 1.468, p = 0.229 |
| Total execution | 19.57 (4.591) | 20.94 (4.24) | F = 2.193, p = 0.142 |
| Total speed | 432.81 (128.36) | 418.62 (104.04) | F = 0.331, p = 0.567 |
| Total accuracy | 97.54 (4.125) | 97.83 (2.846) | F = 0.151, p = 0.699 |
| Symbol search | 37.25 (8.411) | 37.78 (8.568) | F = 0.084, p = 0.773 |
| Number Key | 75.26 (14.151) | 79.36 (17.072) | F = 1.585, p = 0.211 |
| Memory | |||
| Word List I | |||
| Score 1 recall | 6.62 (1.398) | 6.67 (1.509) | F = 0.024, p = 0.878 |
| Total recall score | 35.80 (5.063) | 36.10 (4.674) | F = 0.083, p = 0.774 |
| Interference 1 | 0.92 (1.441) | 0.81 (2.027) | F = 0.093, p = 0.761 |
| Learning | 3.72 (1.371) | 3.95 (1.738) | F = 0.514, p = 0.475 |
| Interference 2 | 1.14 (1.552) | 1.21 (1.353) | F = 0.059, p = 0.809 |
| Word List II | |||
| Recall | 9.04 (2.466) | 9.02 (2.342) | F = 0.001, p = 0.974 |
| Recognition | 23.39 (1.169) | 23.17 (1.305) | F = 0.726, p = 0.396 |
| Faces I | 40.87 (3.512) | 40.60 (3.787) | F = 0.128, p = 0.721 |
| Faces II | 102.65 (15.806) | 100.55 (7.765) | F = 0.619, p = 0.433 |
| Vocabulary | 36.24 (9.317) | 34.00 (9.904) | F = 1.246, p = 0.267 |
| Rey–Osterrieth Complex Figure | |||
| Copy | 33.15 (4.136) | 32.77 (3.239) | F = 0.229, p = 0.633 |
| Copy time | 125.40 (38.970) | 137.52 (43.747) | F = 1.975, p = 0.163 |
| Recovery | 18.06 (5.985) | 18.45 (6.288) | F = 0.094, p = 0.760 |
| Recovery time | 109.84 (37.433) | 117.20 (43.584) | F = 0.750, p = 0.389 |
| Executive Functions | |||
| FAS Test | |||
| F (Words/min) | 18.04 (4.256) | 19.60 (3.749) | F = 3.299, p = 0.073 |
| A (Words/min) | 15.76 (4.461) | 16.31 (3.646) | F = 0.408, p = 0.525 |
| S (Words/min) | 15.18 (4.308) | 15.60 (3.722) | F = 0.240, p = 0.626 |
| Semantics (Words/min) | 63.18 (11.208) | 66.93 (10.778) | F = 2.644, p = 0.107 |
| Five Digit Test | |||
| Reading | 20.14 (3.417) | 19.74 (3.507) | F = 0.308, p = 0.580 |
| Counting | 21.88 (3.409) | 21.19 (3.430) | F = 0.929, p = 0.338 |
| Choosing | 31.96 (5.525) | 30.52 (5.438) | F = 1.565, p = 0.214 |
| Shifting | 41.30 (8.812) | 39.07 (7.270) | F = 1.709, p = 0.194 |
| Inhibition | 11.82 (5.054) | 10.95 (5.860) | F = 0.582, p = 0.448 |
| Flexibility | 21.16 (7.950) | 19.26 (7.398) | F = 1.385, p = 0.242 |
| Spatial Span | |||
| Forward | 8.60 (1.841) | 8.71 (1.672) | F = 0.096, p = 0.758 |
| Backward | 8.22 (1.962) | 7.95 (1.766) | F = 0.465, p = 0.497 |
| Total | 17.00 (3.812) | 16.62 (2.946) | F = 0.279, p = 0.599 |
| Letter–Number Sequencing | 19.12 (2.344) | 19.69 (2.552) | F = 1.247, p = 0.267 |
| Digit Span | |||
| Forward | 9.00 (1.959) | 8.69 (2.089) | F = 0.536, p = 0.466 |
| Forward Span | 6.06 (1.168) | 5.93 (1.237) | F = 0.274, p = 0.602 |
| Backward | 8.28 (2.286) | 8.29 (1.798) | F = 0.000, p = 0.990 |
| Backward Span | 4.62 (1.244) | 4.67 (1.052) | F = 0.037, p = 0.848 |
| Increasing | 8.46 (2.279) | 8,79 (2.280) | F = 0.466, p = 0.496 |
| Increasing Span | 5.84 (1.695) | 6.29 (2.351) | F = 1.111, p = 0.295 |
| Total | 25.76 (5.286) | 25.76 (4.616) | F = 0.000, p = 0.999 |
| Similarities | 21.88 (4.914) | 19.93 (4.566) | F = 3.838, p = 0.053 |
| Key Search | 10.80 (3.774) | 11.52 (3.487) | F = 0.900, p = 0.345 |
| Key Search time | 60.42 (61.305) | 58.26 (57.274) | F = 0.030, p = 0.863 |
| Zoo Test Total | 11.10 (3.898) | 11.40 (3.964) | F = 0.137, p = 0.712 |
| Emotional Measures | COVID-19 Group | Control Group | Statistics (df = 1.90) |
|---|---|---|---|
| STAI-State | 25.08 (4.923) | 24.67 (5.664) | F = 0.113, p = 0.738 |
| STAI-Trait | 26.52 (5.578) | 24.07 (5.110) | F = 4.746, p = 0.032 |
| PHQ-9 | 8.06 (5.482) | 7.71 (4.994) | F = 1.748, p = 0.190 |
| MBI | 11.32 (5.156) | 12.05 (6.231) | F = 1.079, p = 0.541 |
| PCL | 34.58 (11.500) | 34.55 (17.429) | F = 0.639, p = 0.426 |
| MFE-30 | 14.42 (8.442) | 13.76 (8.678) | F = 1.303, p = 0.992 |
| ISP-20 | 15.72 (11.644) | 14.76 (12.689) | F = 0.057, p = 0.812 |
| SCL-90-R | 78.32 (56.750) | 69.50 (64.569) | F = 0.008, p = 0.927 |
| Somatizations | 1.01 (0.783) | 1.70 (5.025) | F = 0.245, p = 0.622 |
| Obsessions and compulsions | 1.28 (0.868) | 2.45 (10.078) | F = 0.097, p = 0.756 |
| Interpersonal sensitivity | 0.84 (0.773) | 0.58 (0.556) | F = 0.909, p = 0.343 |
| Depression | 1.13 (0.881) | 0.81 (0.768) | F = 0.822, p = 0.367 |
| Anxiety | 0.69 (0.642) | 0.68 (0.782) | F = 0.674, p = 0.414 |
| Hostility | 0.68 (0.705) | 0.41 (0.671) | F = 1.433, p = 0.235 |
| Phobic anxiety | 0.27 (0.426) | 0.32 (0.535) | F = 1.618, p = 0.207 |
| Paranoid ideation | 0.66 (0.809) | 0.37 (0.562) | F = 1.925, p = 0.169 |
| Psychoticism | 0.42 (0.620) | 0.26 (0.362) | F = 2.988, p = 0.141 |
| Global severity index | 0.84 (0.647) | 0.67 (0.628) | F = 0.176, p = 0.676 |
| Positive discomfort index | 1.66 (0.575) | 1.76 (0.612) | F = 3.672, p = 0.059 |
| Total positive symptoms | 41.78 (21.076) | 34.02 (23.912) | F = 0.856, p = 0.357 |
| Emotional Tests | STAI State | STAI Trait | PHQ-9 | MBI | PCL | MFE-30 | ISP20 | SCL-90-R |  |
| Neuropsychological tests | |||||||||
| Attention | |||||||||
| D2 Test | |||||||||
| Scanning speed | −0.040 | −0.023 | 0.038 | −0.105 | −0.131 | 0.037 | 0.048 | −0.086 | |
| Scanning accuracy | 0.001 | 0.005 | 0.028 | −0.115 | −0.080 | 0.007 | 0.009 | −0.068 | |
| Omission | −0.084 | 0.015 | 0.005 | −0.034 | −0.015 | 0.101 | 0.126 | −0.010 | |
| Commission | 0.002 | 0.066 | −0.057 | −0.038 | 0.017 | −0.067 | −0.044 | −0.006 | |
| Effectiveness index | 0.000 | −0.140 | 0.061 | −0.205 * | −0.133 | 0.009 | 0.033 | −0.103 | |
| Concentration index | 0.000 | −0.027 | 0.057 | −0.104 | −0.093 | 0.040 | 0.030 | −0.069 | |
| Max | −0.073 | 0.058 | 0.141 | −0.104 | −0.027 | 0.113 | 0.105 | 0.002 | |
| Min | −0.104 | −0.050 | −0.101 | −0.207 * | −0.201 * | −0.137 | −0.006 | −0.163 | |
| Variation index | 0.078 | 0.137 | 0.328 ** | 0.199 | 0.273 ** | 0.328 ** | 0.147 | 0.249 * | |
| TESEN | |||||||||
| Path 1 execution | −0.024 | −0.057 | 0.008 | −0.179 | −0.088 | −0.123 | −0.039 | −0.125 | |
| Path 1 speed | −0.003 | 0.086 | 0.067 | 0.177 | 0.113 | 0.110 | 0.061 | 0.132 | |
| Path 1 accuracy | 0.024 | 0.059 | 0.092 | 0.024 | 0.068 | 0.013 | −0.051 | −0.085 | |
| Path 2 execution | 0.031 | −0.152 | −0.039 | −0.188 | −0.209 * | −0.237 * | −0.145 | −0.182 | |
| Path 2 speed | −0.038 | 0.125 | 0.037 | 0.215 * | 0.178 | 0.176 | 0.137 | 0.146 | |
| Path 2 accuracy | 0.134 | −0.112 | −0.161 | 004 | −0.001 | −0.093 | −0.087 | −0.064 | |
| Path 3 execution | 0.027 | −0.016 | 0.134 | −0.053 | 0.053 | 0.105 | 0.018 | −0.026 | |
| Path 3 speed | −0.089 | −0.001 | −0.091 | 0.075 | −0.049 | −0.080 | 0.004 | 0.085 | |
| Path 3 accuracy | −0.038 | −0.008 | 0.028 | 0.064 | 0.074 | 0.096 | 0.079 | 0.079 | |
| Path 4 execution | 0.100 | −0.035 | 0.189 | −0.003 | 0.151 | 0.247 * | 0.135 | 0.118 | |
| Path 4 speed | 0.046 | 0.204 * | 0.039 | 0.275 ** | 0.176 | 0.079 | 0.169 | 0.217 * | |
| Path 4 accuracy | 0.055 | 0.050 | 0.015 | −0.013 | 0.010 | −0.031 | −0.044 | −0.068 | |
| Total execution | −0.022 | −0.128 | 0.022 | −0.225 * | −0.124 | −0.100 | −0.104 | −0.168 | |
| Total speed | −0.013 | 0.121 | 0.037 | 0.228 * | 0.133 | 0.106 | 0.104 | 0.183 | |
| Total accuracy | 0.031 | 0.006 | −0.033 | 0.032 | 0.046 | −0.007 | −0.042 | −0.044 | |
| Symbol Search | 0.121 | −0.001 | 0.049 | −0.053 | −0.012 | 0.005 | 0.051 | 0.022 | |
| Number Key | 0.079 | 0.059 | −0.048 | 0.016 | −0.138 | −0.076 | −0.021 | −0.056 | |
| Memory | |||||||||
| Word List I | |||||||||
| Score 1 recall | −0.044 | 0.030 | −0.043 | −0.129 | −0.077 | −0.147 | −0.091 | −0.167 | |
| Total recall score | −0.087 | 0.143 | 0.078 | 0.007 | 0.003 | 0.003 | 0.022 | −0.081 | |
| Interference 1 | −0.130 | −0.047 | −0.126 | −0.175 | −0.130 | −0.164 | −0.100 | −0.095 | |
| Learning | −0.034 | 0.126 | 0.150 | 0.177 | 0.064 | 0.155 | 0.072 | 0.097 | |
| Interference 2 | −0.082 | 0.078 | 0.112 | 0.117 | 0.192 | 0.043 | 0.014 | 0.112 | |
| Word List II | |||||||||
| Recall | −0.010 | 0.111 | 0.020 | −0.007 | −0.096 | 0.026 | −0.026 | −0.095 | |
| Recognition | 0.070 | 0.141 | 0.167 | 0.078 | 0.067 | 0.184 | 0.170 | 0.101 | |
| Faces I | −0.013 | −0.006 | 0.011 | −0.170 | −0.112 | 0.050 | −0.005 | −0.036 | |
| Faces II | 0.031 | 0.104 | 0.128 | 0.130 | 0.134 | 0.031 | 0.060 | 0.094 | |
| Vocabulary | −0.022 | 0.048 | −0.225 * | −0.149 | −0.183 | −0.125 | −0.091 | −0.242 * | |
| Rey–Osterrieth Complex Figure | |||||||||
| Copy | −0.179 | −0.016 | −0.041 | −0.036 | −0.161 | −0.096 | −0.110 | −0.178 | |
| Copy time | −0.018 | 0.023 | 0.026 | 0.261 * | 0.141 | 0.064 | −0.024 | 0.098 | |
| Recovery | −0.161 | −0.155 | −0.046 | −0.217 * | −0.294 * | −0.101 | −0.167 | −0.261 * | |
| Recovery time | 0.039 | 0.090 | −0.035 | −0.002 | −0.016 | −0.101 | −0.196 | −0.127 | |
| Executive Functions | |||||||||
| FAS Test | |||||||||
| F (Words/min) | −0.007 | −0.016 | −0.090 | −0.042 | −0.049 | −0.073 | −0.058 | −0.063 | |
| A (Words/min) | −0.053 | −0.104 | −0.168 | −0.022 | −0.087 | −0.012 | −0.056 | −0.094 | |
| S (Words/min) | −0.040 | −0.092 | −0.108 | −0.157 | −0.114 | −0.073 | −0.118 | −0.170 | |
| Semantics (words/3min) | −0.047 | −0.098 | −0.182 | −0.127 | −0.217 * | −0.065 | −0.093 | −0.209 * | |
| Five Digit Test | |||||||||
| Reading | −0.161 | 0.043 | 0.159 | −0.053 | 0.138 | −0.020 | −0.060 | 0.047 | |
| Counting | −0.113 | 0.071 | 0.188 | −0.021 | 0.131 | −0.029 | −0.023 | 0.074 | |
| Choosing | −0.059 | 0.068 | 0.067 | −0.010 | 0.065 | 0.035 | 0.123 | 0.063 | |
| Shifting | −0.036 | −0.053 | −0.015 | 0.056 | 0.067 | 0.027 | 0.049 | 0.105 | |
| Inhibition | 0.066 | 0.064 | −0.004 | 0.067 | 0.011 | 0.072 | 0.177 | 0.064 | |
| Flexibility | 0.027 | −0.083 | −0.096 | 0.070 | −0.001 | 0.030 | 0.074 | 0.081 | |
| Spatial Span | |||||||||
| Forward | −0.029 | −0.077 | 0.030 | −0.026 | −0.020 | −0.040 | 0.017 | −0.042 | |
| Backward | −0.064 | −0.068 | −0.027 | −0.279 ** | −0.167 | −0.035 | −0.114 | −0.263 * | |
| Total | −0.030 | −0.039 | −0.017 | −0.186 | −0.109 | −0.069 | −0.038 | −0.179 | |
| Letter–Number Sequencing | 0.069 | −0.092 | 0.026 | −0.101 | −0.074 | 0.043 | −0.053 | −0.116 | |
| Digit Span | |||||||||
| Forward | 0.040 | −0.106 | −0.156 | −0.257 * | −0.104 | −0.098 | −0.144 | −0.198 | |
| Forward Span | 0.016 | −0.124 | −0.221 * | −0.279 ** | −0.132 | −0.132 | −0.211 * | −0.235 * | |
| Backward | 0.011 | −0.111 | −0.050 | −0.110 | −0.055 | −0.059 | −0.084 | −0.102 | |
| Backward Span | 0.024 | −0.97 | −0.020 | −0.057 | −0.047 | −0.046 | −0.111 | −0.095 | |
| Increasing | −0.081 | −0.274 ** | −0.060 | −0.159 | −0.091 | 0.010 | −0.048 | −0.147 | |
| Increasing Span | 0.035 | −0.240 * | −0.004 | −0.109 | −0.017 | 0.115 | −0.062 | −0.074 | |
| Total | −0.012 | −0.209 * | −0.109 | −0.224 * | −0.106 | −0.061 | −0.116 | −0.190 | |
| Similarities | 0.071 | −0.036 | −0.148 | −0.063 | −0.141 | 0.007 | 0.047 | −0.096 | |
| Key Search | 0.091 | 0.068 | −0.019 | 0.044 | −0.108 | 0.029 | 0.070 | −0.056 | |
| Key Search Time | −0.154 | −0.120 | 0.046 | 0.056 | 0.061 | 0.044 | −0.042 | 0.021 | |
| Zoo Test Total | 0.081 | 0.177 | −0.007 | 0.163 | −0.051 | −0.125 | 0.061 | −0.022 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peláez, I.; Martínez-Íñigo, D.; Fernandes-Magalhaes, R.; De Lahoz, M.E.; del Pino, A.B.; Pérez-Aranda, S.; García-Romero, A.; Soldic, D.; Mercado, F. One Year After Mild COVID-19: Emotional Distress but Preserved Cognition in Healthcare Workers. J. Clin. Med. 2025, 14, 6007. https://doi.org/10.3390/jcm14176007
Peláez I, Martínez-Íñigo D, Fernandes-Magalhaes R, De Lahoz ME, del Pino AB, Pérez-Aranda S, García-Romero A, Soldic D, Mercado F. One Year After Mild COVID-19: Emotional Distress but Preserved Cognition in Healthcare Workers. Journal of Clinical Medicine. 2025; 14(17):6007. https://doi.org/10.3390/jcm14176007
Chicago/Turabian StylePeláez, Irene, David Martínez-Íñigo, Roberto Fernandes-Magalhaes, María E. De Lahoz, Ana Belén del Pino, Sonia Pérez-Aranda, Alejandro García-Romero, Dino Soldic, and Francisco Mercado. 2025. "One Year After Mild COVID-19: Emotional Distress but Preserved Cognition in Healthcare Workers" Journal of Clinical Medicine 14, no. 17: 6007. https://doi.org/10.3390/jcm14176007
APA StylePeláez, I., Martínez-Íñigo, D., Fernandes-Magalhaes, R., De Lahoz, M. E., del Pino, A. B., Pérez-Aranda, S., García-Romero, A., Soldic, D., & Mercado, F. (2025). One Year After Mild COVID-19: Emotional Distress but Preserved Cognition in Healthcare Workers. Journal of Clinical Medicine, 14(17), 6007. https://doi.org/10.3390/jcm14176007







