Evaluation of the Diagnostic Accuracy of Serum Albumin and Globulin in Pyogenic Spondylitis
Abstract
1. Introduction
2. Materials and Methods
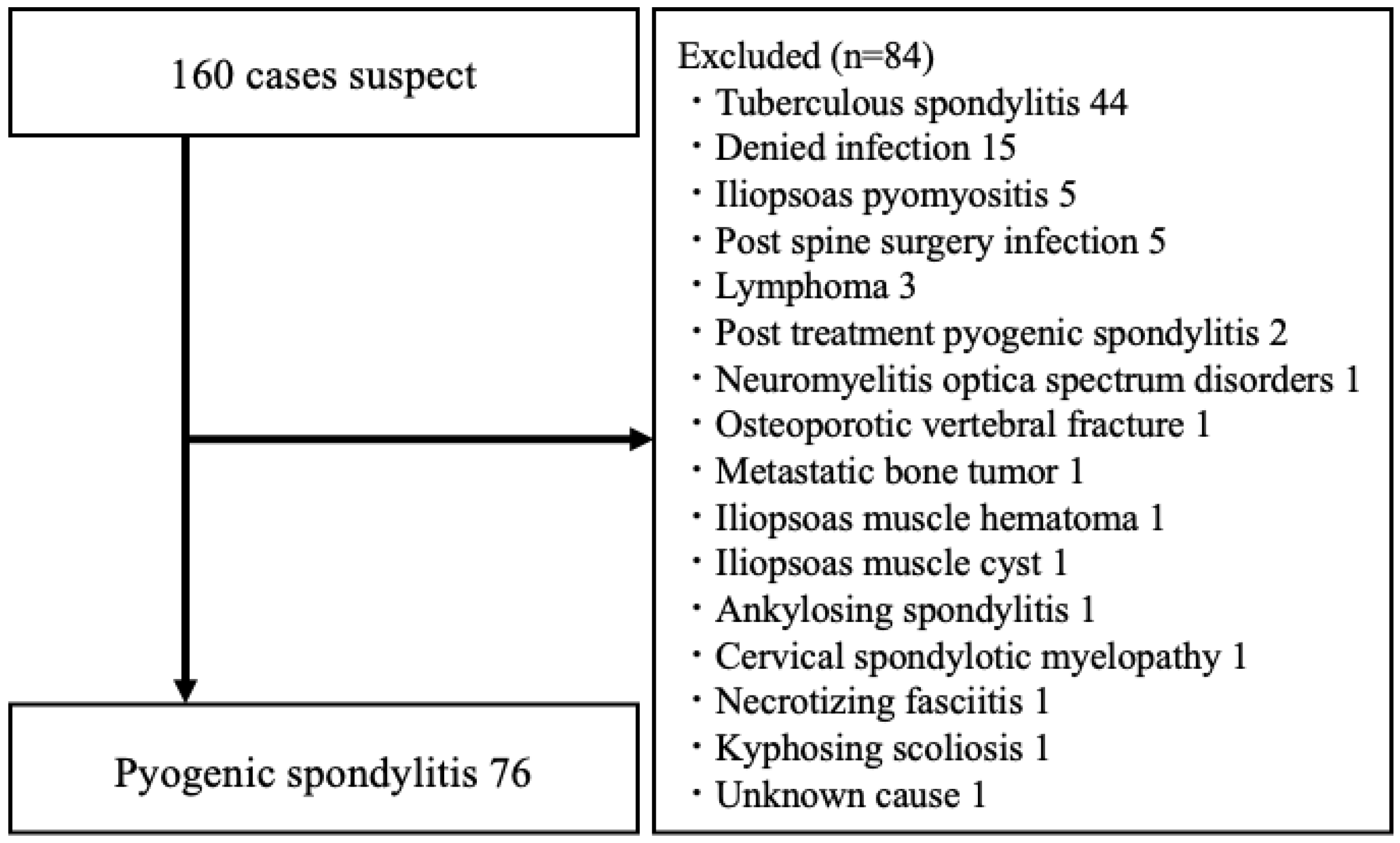
2.1. Patient Enrollment
2.2. Acquisition of Data
2.3. Serum Biomarkers
2.4. Statistical Analysis
3. Results
3.1. Comparison Between the Pyogenic Spondylitis and Control Groups
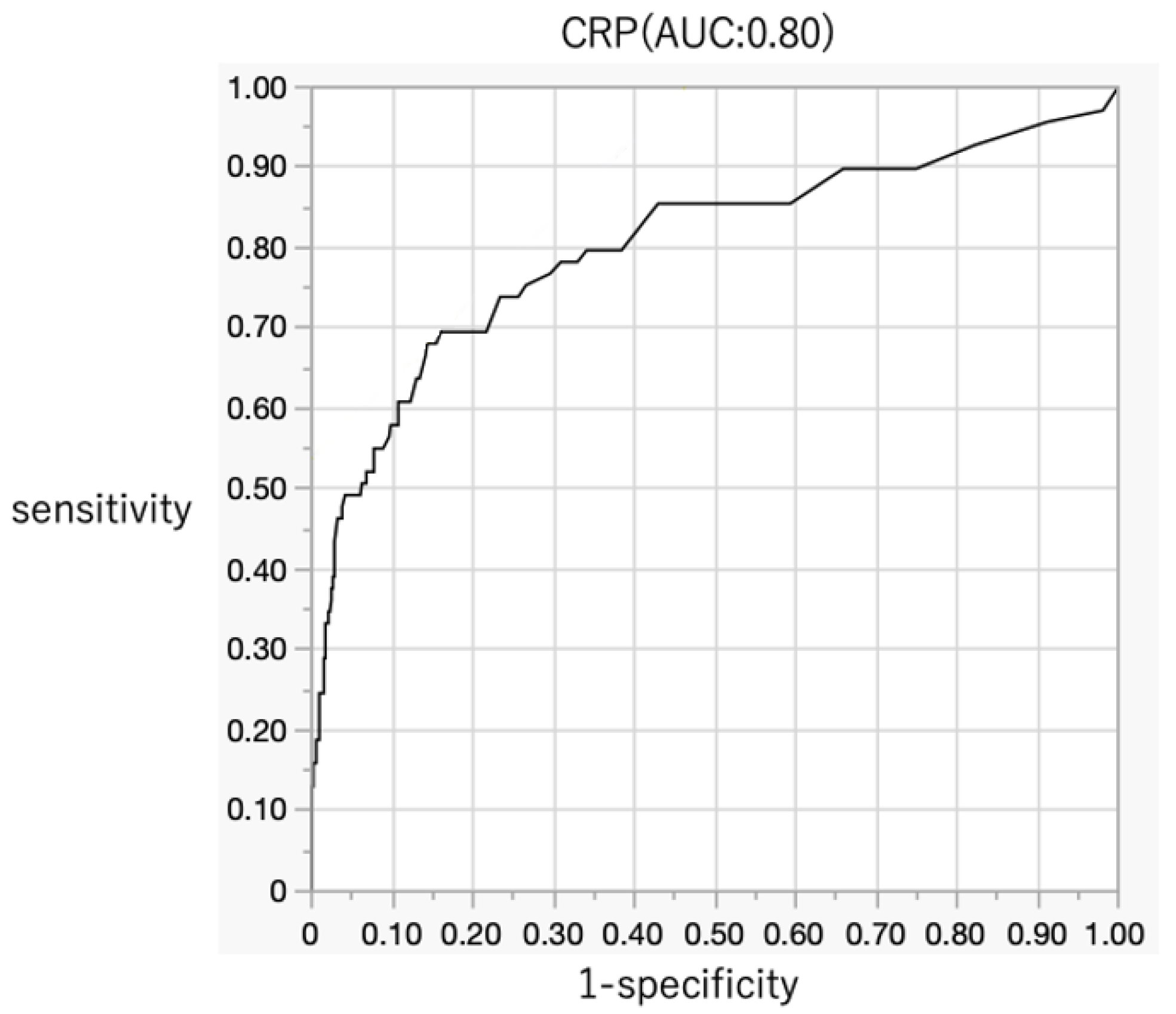
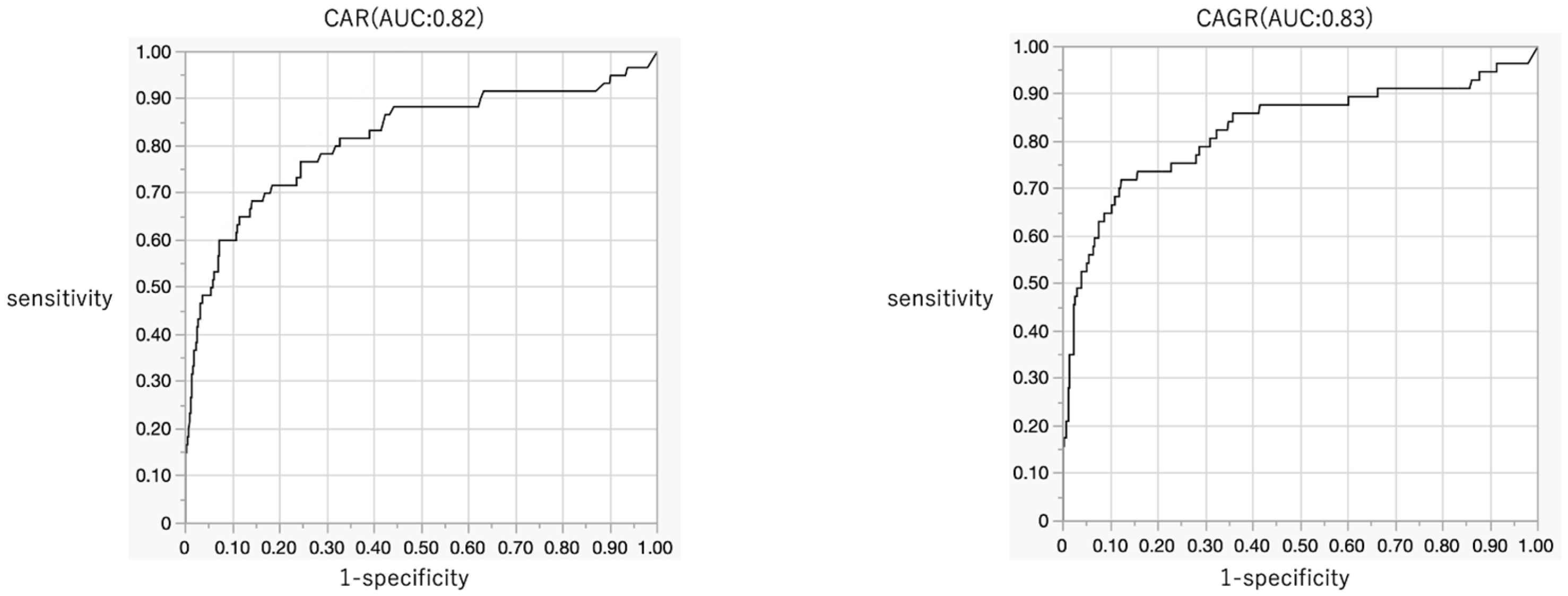
3.2. Diagnostic Accuracy of Serum Biomarkers for Pyogenic Spondylitis
3.3. Diagnostic Accuracy of Combination Biomarkers for Pyogenic Spondylitis
3.4. Multivariate Analysis for Pyogenic Spondylitis
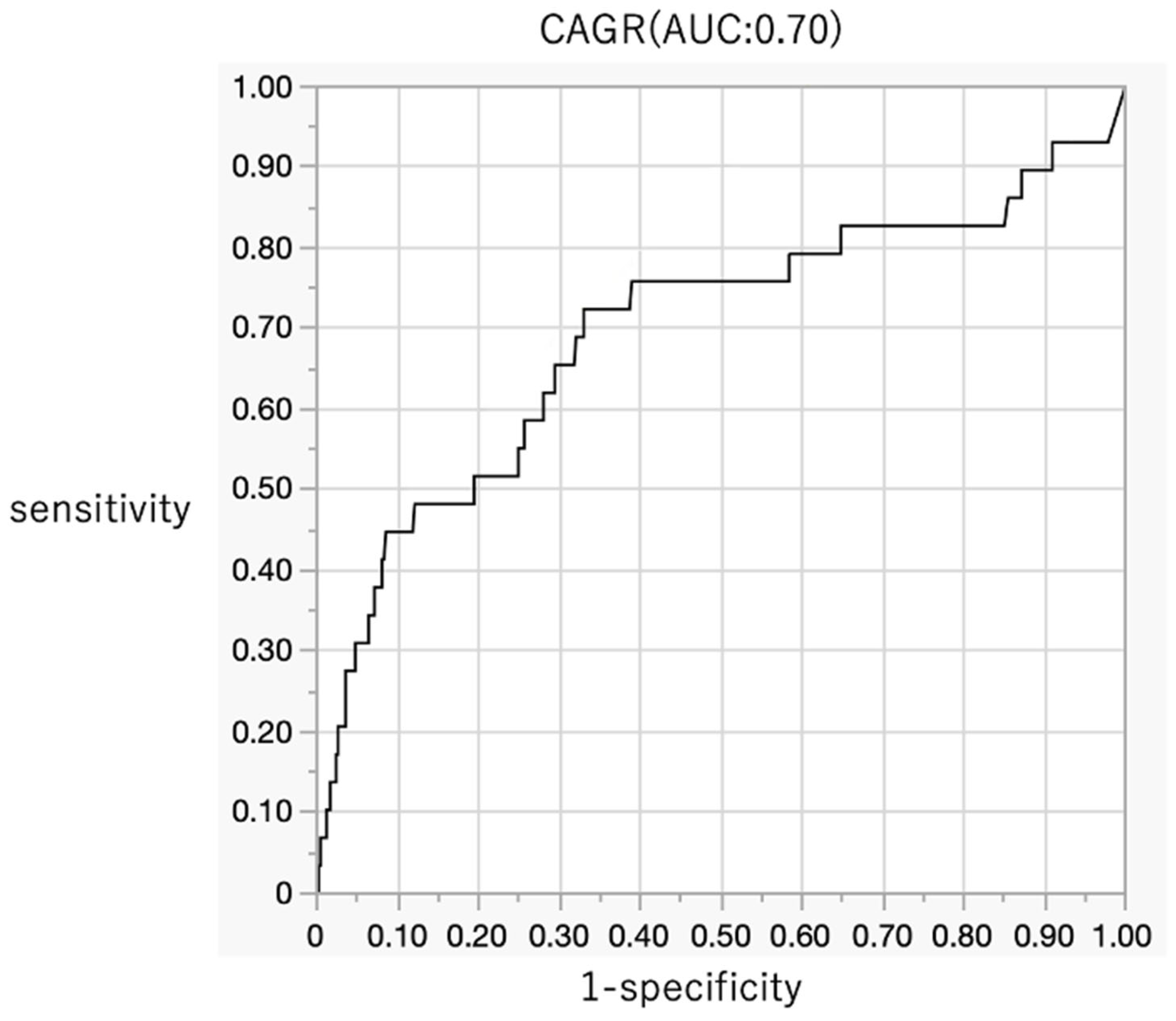
3.5. Comparison Between the Low-Inflammatory Pyogenic Spondylitis and Control Groups
3.6. Comparison Between the Culture-Positive Pyogenic Spondylitis and Control Groups
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ishimoto, Y.; Kawakami, M.; Curtis, E.; Cooper, C.; Harvey, N.C.; Westbury, L.; Teraguchi, M.; Horie, K.; Nakagawa, Y. The impact of lumbar spinal stenosis, knee osteoarthritis, and loss of lumbar lordosis on the quality of life: Findings from the Katsuragi Low Back Pain Study. Spine Surg. Relat. Res. 2019, 3, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Duarte, R.M.; Vaccaro, A.R. Spinal infection: State of the art and management algorithm. Eur. Spine J. 2013, 22, 2787–2799. [Google Scholar] [CrossRef] [PubMed]
- Butler, J.S.; Shelly, M.J.; Timlin, M.; Powderly, W.G.; O’Byrne, J.M. Nontuberculous pyogenic spinal infection in adults: A 12-year experience from a tertiary referral center. Spine 2006, 31, 2695–2700. [Google Scholar] [CrossRef] [PubMed]
- Nagashima, H.; Tanishima, S.; Tanida, A. Diagnosis and management of spinal infections. J. Orthop. Sci. 2018, 23, 8–13. [Google Scholar] [CrossRef]
- Akiyama, T.; Chikuda, H.; Yasunaga, H.; Horiguchi, H.; Fushimi, K.; Saita, K. Incidence and risk factors for mortality of vertebral osteomyelitis: A retrospective analysis using the Japanese diagnosis procedure combination database. BMJ Open 2013, 3, e002412. [Google Scholar] [CrossRef]
- Sato, K.; Yamada, K.; Yokosuka, K.; Yoshida, T.; Goto, M.; Matsubara, T.; Iwahashi, S.; Shimazaki, T.; Nagata, K.; Shiba, N.; et al. Pyogenic Spondylitis: Clinical Features, Diagnosis and Treatment. Kurume Med J. 2019, 65, 83–89. [Google Scholar] [CrossRef]
- Gupta, A.; Kowalski, T.J.; Osmon, D.R.; Enzler, M.; Steckelberg, J.M.; Huddleston, P.M.; Nassr, A.; Mandrekar, J.M.; Berbari, E.F. Long-term outcome of pyogenic vertebral osteomyelitis: A cohort study of 260 patients. Open Forum Infect. Dis. 2014, 1, ofu107. [Google Scholar] [CrossRef]
- Nolla, J.M.; Ariza, J.; Gómez-Vaquero, C.; Fiter, J.; Bermejo, J.; Valverde, J.; Escofet, D.R.; Gudiol, F. Spontaneous pyogenic vertebral osteomyelitis in nondrug users. Semin. Arthritis Rheum. 2002, 31, 271–278. [Google Scholar] [CrossRef]
- Zimmerli, W. Clinical practice. Vertebral osteomyelitis. N. Engl. J. Med. 2010, 362, 1022–1029. [Google Scholar] [CrossRef]
- Darouiche, R.O. Spinal epidural abscess. N. Engl. J. Med. 2006, 355, 2012–2020. [Google Scholar] [CrossRef]
- Mylona, E.; Samarkos, M.; Kakalou, E.; Fanourgiakis, P.; Skoutelis, A. Pyogenic vertebral osteomyelitis: A systematic review of clinical characteristics. Semin. Arthritis Rheum. 2009, 39, 10–17. [Google Scholar] [CrossRef]
- Choe, H.; Kobayashi, N.; Abe, K.; Hieda, Y.; Tezuka, T.; Inaba, Y. Evaluation of serum albumin and globulin in combination with C-reactive protein improves serum diagnostic accuracy for low-grade periprosthetic joint infection. J. Arthroplast. 2023, 38, 555–561. [Google Scholar] [CrossRef]
- Abe, K.; Choe, H.; Oba, M.; Tezuka, T.; Ike, H.; Kobayashi, N.; Inaba, Y. Inflammation and nutrition based screening tests for detection of infection in cases of rapid hip destruction. Sci. Rep. 2022, 12, 3586. [Google Scholar] [CrossRef]
- Wu, H.; Pan, L.; Meng, Z.; Liu, H.; Yang, X.; Cao, Y. C-reactive protein (CRP)/albumin-to-globulin ratio (AGR) is a valuable test for diagnosing periprosthetic joint infection: A single-center retrospective study. J. Orthop. Traumatol. 2022, 23, 36. [Google Scholar] [CrossRef]
- Ji, W.; Liu, Z.; Lin, T. Diagnostic value of albumin/fibrinogen ratio and C-reactive protein/albumin/globulin ratio for periprosthetic joint infection: A retrospective study. PeerJ 2023, 11, e16662. [Google Scholar] [CrossRef]
- Moldovan, F. Role of Serum Biomarkers in Differentiating Periprosthetic Joint Infections from Aseptic Failures after Total Hip Arthroplasties. J. Clin. Med. 2024, 13, 5716. [Google Scholar] [CrossRef] [PubMed]
- Deng, L.; Wang, J.; Yang, G.-Y.; Hou, Y.-Z.; Li, K.-W.; Sun, B.; Wang, S.-H. Different biomarker ratios in peripheral blood have limited value in diagnosing periprosthetic joint infection after total joint arthroplasty: A single-center, retrospective study. BMC Musculoskelet. Disord. 2024, 25, 377. [Google Scholar] [CrossRef] [PubMed]
- Zhao, G.; Chen, J.; Wang, J.; Wang, S.; Xia, J.; Wei, Y.; Wu, J.; Huang, G.; Chen, F.; Shi, J.; et al. Predictive values of the postoperative neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and lymphocyte-to-monocyte ratio for the diagnosis of early periprosthetic joint infections: A preliminary study. J. Orthop. Surg. Res. 2020, 15, 571. [Google Scholar] [CrossRef] [PubMed]
- Inose, H.; Kobayashi, Y.; Yuasa, M.; Hirai, T.; Yoshii, T.; Okawa, A. Procalcitonin and Neutrophil Lymphocyte Ratio After Spinal Instrumentation Surgery. Spine 2019, 44, E1356–E1361. [Google Scholar] [CrossRef]
- Shang, G.; Fei, Z.; Xu, H.; Wang, Y.; Xiang, S. Globulin and albumin to globulin ratio precisely diagnose periprosthetic joint infection and determine the timing of second-stage reimplantation. J. Orthop. Surg. Res. 2022, 17, 12. [Google Scholar] [CrossRef]
- Higashikawa, T.; Okuro, M.; Ishigami, K.; Mae, K.; Sangen, R.; Mizuno, T.; Usuda, D.; Saito, A.; Kasamaki, Y.; Fukuda, A.; et al. Procalcitonin and albumin as prognostic biomarkers in elderly patients with a risk of bacterial infection. J. Int. Med. Res. 2018, 46, 2606–2614. [Google Scholar] [CrossRef]
- Man, S.L.C.; Chau, W.W.; Chung, K.Y.; Ho, K.K.W. Hypoalbuminemia and obesity class II are reliable predictors of peri-prosthetic joint infection in patient undergoing elective total knee arthroplasty. Knee Surg. Relat. Res. 2020, 32, 21. [Google Scholar] [CrossRef]
- Tanaka, T.; Narazaki, M.; Kishimoto, T. IL-6 in inflammation, immunity, and disease. Cold Spring Harb. Perspect. Biol. 2014, 6, a016295. [Google Scholar] [CrossRef] [PubMed]
- Fulks, M.; Stout, R.L.; Dolan, V.F. Serum globulin predicts all-cause mortality for life insurance applicants. J. Insur. Med. 2014, 44, 93–98. [Google Scholar] [PubMed]
- Ye, Y.; Chen, W.; Gu, M.; Xian, G.; Pan, B.; Zheng, L.; Zhang, Z.; Sheng, P. Serum globulin and albumin to globulin ratio as potential diagnostic biomarkers for periprosthetic joint infection: A retrospective review. J. Orthop. Surg. Res. 2020, 15, 459. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Zhou, H.; Jiang, R.; Qian, Z.; Wang, F.; Cao, L. Globulin, the albumin-to-globulin ratio, and fibrinogen perform well in the diagnosis of periprosthetic joint infection. BMC Musculoskelet. Disord. 2021, 22, 583. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, T.; Fang, Y.; Wang, M.; Liu, W.; Zhao, J.; Wang, B.; Wu, Z.; Lv, Y.; Wu, R. Clinical significance of serum albumin/globulin ratio in patients with pyogenic liver abscess. Front. Surg. 2021, 8, 677799. [Google Scholar] [CrossRef]
- Li, K.; Fu, W.; Bo, Y.; Zhu, Y. Effect of albumin-globulin score and albumin to globulin ratio on survival in patients with heart failure: A retrospective cohort study in China. BMJ Open 2018, 8, e022960. [Google Scholar] [CrossRef]
- Tang, X.; Xu, Q.; Yang, S.; Huang, X.; Wang, L.; Huang, F.; Luo, J.; Zhou, X.; Wu, A.; Mei, Q.; et al. Toll-like Receptors and Thrombopoiesis. Int. J. Mol. Sci. 2023, 24, 1010. [Google Scholar] [CrossRef]
| Group | Pyogenic Spondylitis | Control | p Value |
|---|---|---|---|
| Number of patients | 76 | 531 | |
| Age; mean (range) | 65 (38–86) | 71 (29–96) | <0.0001 |
| Proportion of male patients | 68.4% | 54.1% | 0.0191 |
| Comorbidities | 37 (48.7%) | 20 (3.8%) | <0.0001 |
| Category | Markers | Pyogenic Spondylitis | Control | p Value |
|---|---|---|---|---|
| Nutritional markers | Albumin, g/dL | 3.6 (0.9) | 4.2 (0.4) | <0.0001 |
| Total protein, g/dL | 7.1 (0.8) | 7.1 (0.5) | 0.3003 | |
| Globulin, g/dL | 3.5 (0.8) | 2.9 (0.4) | <0.0001 | |
| AGR | 1.1 (0.5) | 1.5 (0.3) | <0.0001 | |
| Inflammatory markers | C-reactive protein, mg/dL | 4.7 (8.8) | 0.3 (0.8) | <0.0001 |
| CAR | 1.8 (4) | 0.1 (0.2) | <0.0001 | |
| CAGR | 7 (15) | 0.2 (0.8) | <0.0001 | |
| Hematologic markers | White blood cell count, /μL | 7924 (3606) | 6469 (1942) | 0.0006 |
| N count, /μL | 5182 (3242) | 3985 (1576) | 0.0019 | |
| L count, /μL | 1463 (568) | 1683 (638) | 0.0085 | |
| M count, /μL | 529 (258) | 480 (176) | 0.5268 | |
| Platelet count, 104/μL | 29.4 (12.9) | 22.6 (6.1) | <0.0001 | |
| NLR | 4.1 (3.8) | 2.6 (2.3) | <0.0001 | |
| PLR | 250.4 (190.9) | 158.6 (90.1) | <0.0001 |
| Category | Markers | AUC (95% CI) | Cut-Off | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|---|---|---|
| Nutritional | Albumin, g/dL | 0.70 (0.61–0.78) | 3.7 1 | 0.52 | 0.88 | 0.39 | 0.93 |
| Globulin, g/dL | 0.77 (0.69–0.84) | 3.2 1 | 0.66 | 0.81 | 0.31 | 0.95 | |
| AGR | 0.77 (0.68–0.84) | 1.2 1 | 0.61 | 0.87 | 0.38 | 0.94 | |
| Inflammatory | C-reactive protein, mg/dL | 0.80 (0.73–0.86) | 0.3 1 | 0.68 | 0.86 | 0.38 | 0.95 |
| CAR | 0.82 (0.73–0.88) | 0.1 1 | 0.68 | 0.86 | 0.39 | 0.95 | |
| CAGR | 0.83 (0.74–0.89) | 0.3 1 | 0.72 | 0.88 | 0.43 | 0.96 | |
| Hematologic | White blood cell count, /μL | 0.62 (0.55–0.69) | 7800 1 | 0.42 | 0.80 | 0.23 | 0.91 |
| N count, /μL | 0.63 (0.54–0.71) | 3680 1 | 0.73 | 0.51 | 0.17 | 0.93 | |
| L count, /μL | 0.60 (0.53–0.67) | 1700 1 | 0.72 | 0.47 | 0.18 | 0.91 | |
| Platelet count, 104/μL | 0.68 (0.61–0.75) | 27.0 1 | 0.53 | 0.78 | 0.25 | 0.92 | |
| NLR | 0.69 (0.61–0.75) | 2.0 1 | 0.84 | 0.48 | 0.18 | 0.96 | |
| PLR | 0.67 (0.59–0.75) | 208 1 | 0.51 | 0.83 | 0.33 | 0.91 |
| Category | Variable | OR | 95% CI | p Value |
|---|---|---|---|---|
| Age | 0.93 | 0.90–0.97 | 0.0005 | |
| Comorbidities | 16.98 | 6.31–45.73 | <0.0001 | |
| Nutritional markers | Albumin, g/dL | 0.24 | 0.03–2.12 | 0.1974 |
| Globulin, g/dL | 6.1 | 0.43–97.02 | 0.1905 | |
| AGR | 5.99 | 0.01–2395.08 | 0.5796 | |
| Inflammatory markers | C-reactive protein, mg/dL | 0.63 | 0.13–1.32 | 0.4404 |
| CAGR | 1.53 | 0.91–5.73 | 0.3283 | |
| Hematologic markers | NLR | 1.06 | 0.85–1.26 | 0.5843 |
| PLR | 1.00 | 0.995–1.003 | 0.8819 |
| Category | Markers | Low-Inflammatory Pyogenic Spondylitis | Control | p Value |
|---|---|---|---|---|
| Nutritional markers | Albumin, g/dL | 4.0 (0.8) | 4.2 (0.4) | 0.1193 |
| Total protein, g/dL | 7.3 (0.6) | 7.1 (0.5) | 0.0293 | |
| Globulin, g/dL | 3.3 (1.0) | 2.8 (0.4) | 0.0012 | |
| AGR | 1.3 (0.4) | 1.5 (0.3) | 0.0044 | |
| Inflammatory markers | C-reactive protein, mg/dL | 0.24 (0.22) | 0.13 (0.18) | 0.0023 |
| CAR | 0.073 (0.069) | 0.03 (0.05) | 0.0006 | |
| CAGR | 0.29 (0.33) | 0.1 (0.2) | 0.0004 | |
| Hematologic markers | White blood cell count, /μL | 6303 (1622) | 6380 (1890) | 0.6551 |
| N count, /μL | 4149 (1275) | 3907 (1514) | 0.1254 | |
| L count, /μL | 1482 (527) | 1698 (633) | 0.0541 | |
| M count, /μL | 437 (152) | 473 (172) | 0.2099 | |
| Platelet count, 104/μL | 25.5 (8.6) | 22.5 (6) | 0.0108 | |
| NLR | 8759 (6743) | 85,636 (87,653) | 0.0027 | |
| PLR | 193.5 (99.7) | 154.4 (79.7) | 0.0192 |
| Category | Markers | AUC (95% CI) | Cut-Off | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|---|---|---|
| Nutritional | Total protein, g/dL | 0.61 (0.50–0.72) | 7.3 1 | 0.63 | 0.65 | 0.10 | 0.96 |
| Globulin, g/dL | 0.68 (0.56–0.78) | 3.0 1 | 0.66 | 0.63 | 0.11 | 0.96 | |
| AGR | 0.66 (0.53–0.77) | 1.2 1 | 0.41 | 0.89 | 0.20 | 0.96 | |
| Inflammatory | C-reactive protein, mg/dL | 0.65 (0.54–0.75) | 0.1 1 | 0.71 | 0.60 | 0.11 | 0.97 |
| CAR | 0.68 (0.56–0.79) | 0.02 1 | 0.77 | 0.58 | 0.12 | 0.97 | |
| CAGR | 0.70 (0.56–0.80) | 0.1 1 | 0.72 | 0.67 | 0.13 | 0.97 | |
| Hematologic | Platelet count, 104/μL | 0.63 (0.53–0.72) | 23.3 1 | 0.66 | 0.57 | 0.10 | 0.96 |
| NLR | 0.66 (0.58–0.74) | 2.0 1 | 0.81 | 0.49 | 0.11 | 0.97 | |
| PLR | 0.62 (0.51–0.72) | 209 1 | 0.42 | 0.85 | 0.19 | 0.99 |
| Category | Markers | Culture-Positive Pyogenic Spondylitis | Control | p Value |
|---|---|---|---|---|
| Nutritional markers | Albumin, g/dL | 3.5 (0.9) | 4.2 (0.4) | <0.0001 |
| Total protein, g/dL | 7.2 (0.7) | 7.1 (0.5) | 0.3285 | |
| Globulin, g/dL | 3.7 (0.9) | 2.9 (0.4) | <0.0001 | |
| AGR | 1.0 (0.4) | 1.5 (0.3) | <0.0001 | |
| Inflammatory markers | C-reactive protein, mg/dL | 5.3 (9.9) | 0.3 (0.8) | <0.0001 |
| CAR | 1.8 (3.5) | 0.1 (0.2) | <0.0001 | |
| CAGR | 7.7 (15) | 0.2 (0.8) | <0.0001 | |
| Hematologic markers | White blood cell count, /μL | 8272 (3774) | 6469 (1942) | 0.0004 |
| N count, /μL | 5633 (3772) | 3985 (1576) | 0.0018 | |
| L count, /μL | 1450 (549) | 1683 (638) | 0.0297 | |
| M count, /μL | 547 (280) | 480 (176) | 0.4961 | |
| Platelet count, 104/μL | 31.5 (15.1) | 22.6 (6.1) | <0.0001 | |
| NLR | 4.7 (4.6) | 2.6 (2.3) | <0.0001 | |
| PLR | 276.2 (223.8) | 158.6 (90.1) | <0.0001 |
| Category | Markers | AUC (95% CI) | Cut-Off | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|---|---|---|
| Nutritional | Albumin, g/dL | 0.75 (0.63–0.84) | 3.7 1 | 0.62 | 0.88 | 0.31 | 0.97 |
| Globulin, g/dL | 0.81 (0.71–0.89) | 3.5 1 | 0.59 | 0.91 | 0.34 | 0.97 | |
| AGR | 0.81 (0.70–0.89) | 0.1 1 | 0.71 | 0.88 | 0.32 | 0.98 | |
| Inflammatory | C-reactive protein, mg/dL | 0.84(0.74–0.90) | 0.4 1 | 0.76 | 0.86 | 0.29 | 0.98 |
| CAR | 0.84 (0.73–0.91) | 0.1 1 | 0.74 | 0.86 | 0.30 | 0.97 | |
| CAGR | 0.84 (0.73–0.91) | 0.3 1 | 0.76 | 0.88 | 0.32 | 0.98 | |
| Hematologic | White blood cell count, /μL | 0.66 (0.56–0.75) | 7800 1 | 0.49 | 0.80 | 0.16 | 0.95 |
| N count, /μL | 0.66 (0.55–0.76) | 5421 1 | 0.42 | 0.86 | 0.20 | 0.95 | |
| L count, /μL | 0.60 (0.51–0.69) | 1588 1 | 0.66 | 0.53 | 0.12 | 0.94 | |
| Platelet count, 104/μL | 0.71 (0.61–0.79) | 30.5 1 | 0.40 | 0.91 | 0.26 | 0.95 | |
| NLR | 0.70 (0.61–0.78) | 2.2 1 | 0.82 | 0.52 | 0.12 | 0.97 | |
| PLR | 0.69 (0.58–0.78) | 195 1 | 0.59 | 0.77 | 0.20 | 0.95 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mitsui, H.; Choe, H.; Shimoda, M.; Yamane, H.; Hieda, Y.; Abe, K.; Ito, Y.; Ike, H.; Kumagai, K.; Kobayashi, N.; et al. Evaluation of the Diagnostic Accuracy of Serum Albumin and Globulin in Pyogenic Spondylitis. J. Clin. Med. 2025, 14, 6001. https://doi.org/10.3390/jcm14176001
Mitsui H, Choe H, Shimoda M, Yamane H, Hieda Y, Abe K, Ito Y, Ike H, Kumagai K, Kobayashi N, et al. Evaluation of the Diagnostic Accuracy of Serum Albumin and Globulin in Pyogenic Spondylitis. Journal of Clinical Medicine. 2025; 14(17):6001. https://doi.org/10.3390/jcm14176001
Chicago/Turabian StyleMitsui, Hideo, Hyonmin Choe, Masashi Shimoda, Hironori Yamane, Yuta Hieda, Koki Abe, Yohei Ito, Hiroyuki Ike, Ken Kumagai, Naomi Kobayashi, and et al. 2025. "Evaluation of the Diagnostic Accuracy of Serum Albumin and Globulin in Pyogenic Spondylitis" Journal of Clinical Medicine 14, no. 17: 6001. https://doi.org/10.3390/jcm14176001
APA StyleMitsui, H., Choe, H., Shimoda, M., Yamane, H., Hieda, Y., Abe, K., Ito, Y., Ike, H., Kumagai, K., Kobayashi, N., & Inaba, Y. (2025). Evaluation of the Diagnostic Accuracy of Serum Albumin and Globulin in Pyogenic Spondylitis. Journal of Clinical Medicine, 14(17), 6001. https://doi.org/10.3390/jcm14176001






