Diagnostic Yield of the New Bárány Society Criteria for Pediatric Episodic Vestibular Syndrome
Abstract
1. Introduction
2. Materials and Methods
2.1. Clinical Study Design and Setting
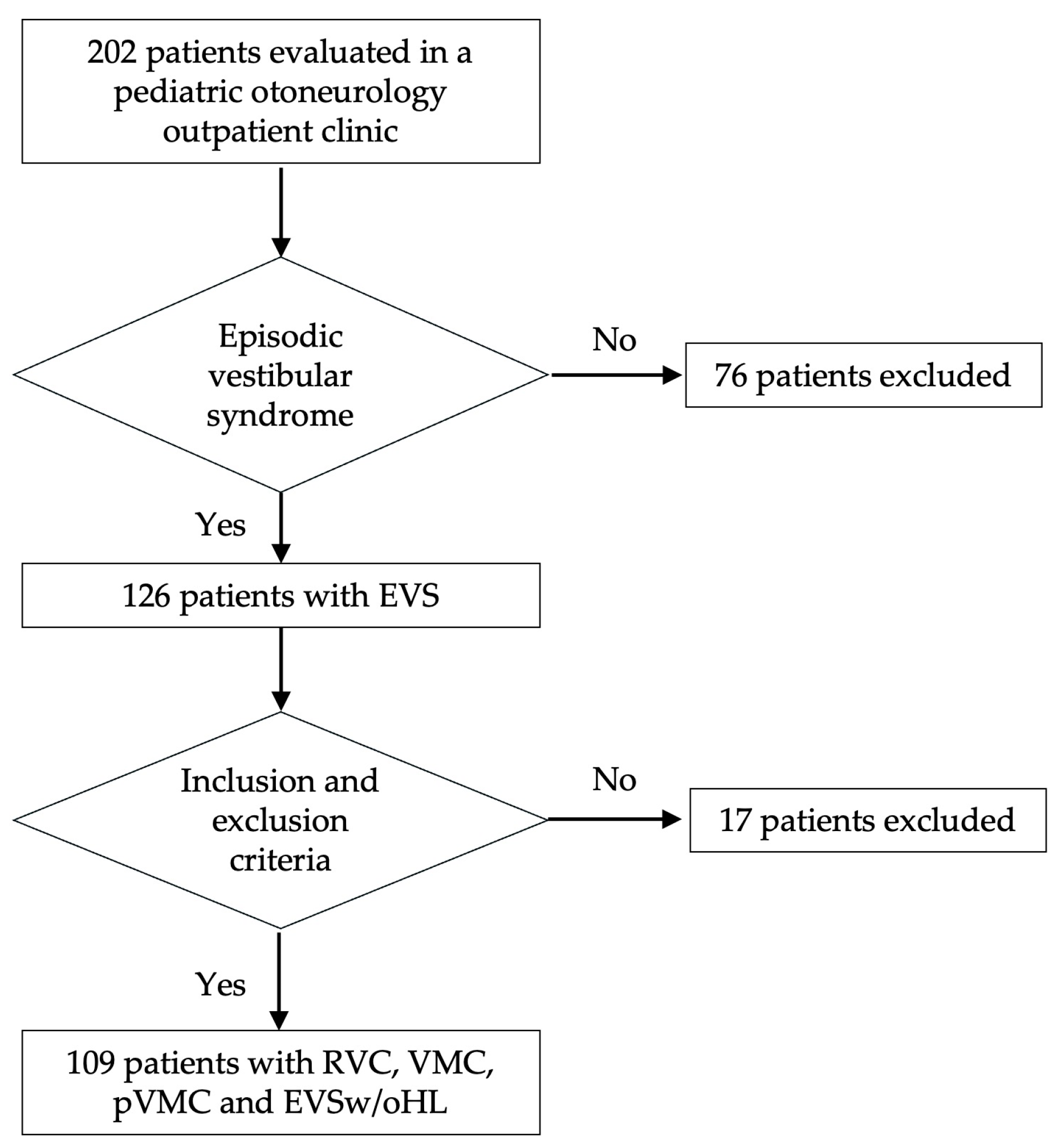
2.2. Patient Selection
2.3. Clinical Assessment
2.4. Inclusion Criteria
2.5. Exclusion Criteria
2.6. Data Collection
2.7. Statistical Analysis
2.8. Sample Size and Sampling Procedure
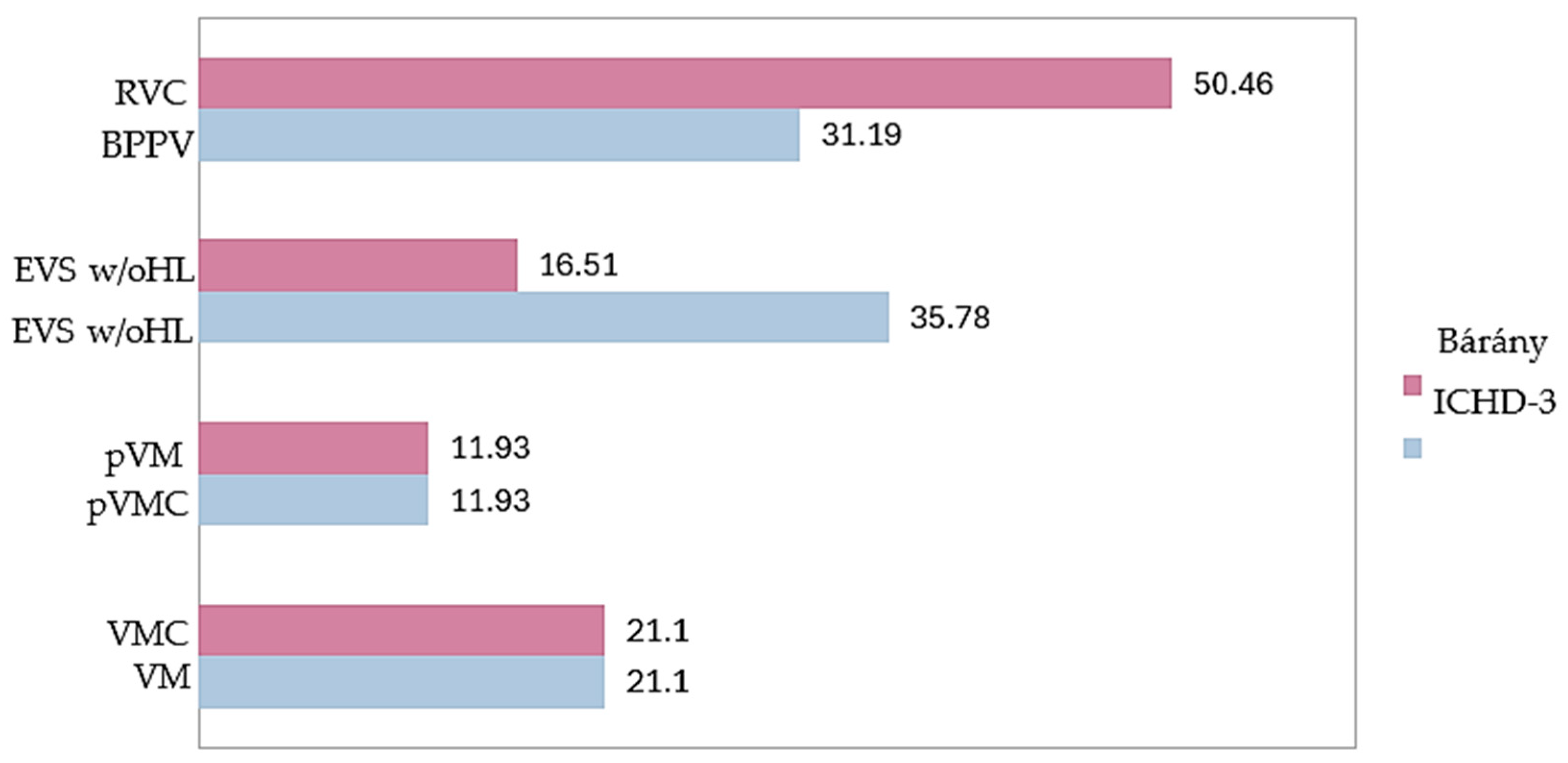
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BPPV | Benign paroxysmal positional vertigo |
| BPV | Benign paroxysmal vertigo |
| BPVC | Benign paroxismal vertigo of childhood |
| cVEMP | Cervical vestibular evoked myogenic potentials |
| EEG | Electroencephalogram |
| EVS | Episodic vestibular syndrome |
| EVSw/oHL | Episodic vestibular syndrome without hearing loss |
| ICHD-3 | International Classification of Headache Disorders |
| HIS | International Headache Society |
| MRI | Magnetic resonance imaging |
| oVEMP | Ocular vestibular evoked myogenic potentials |
| pVM | Probable vestibular migraine |
| pVMC | Probable vestibular migraine of childhood |
| RVC | Recurrent vertigo of childhood |
| VEMP | Vestibular evoked myogenic potentials |
| vHIT | Video head impulse test |
| VM | Vestibular migraine |
| VMC | Vestibular migraine of childhood |
Appendix A
| Vestibular Symptom | Duration of Episodes | Auditory Symptoms | Migraine | Number of Episodes | Plausible Diagnosis | |
|---|---|---|---|---|---|---|
| A1 | Vertigo | <1 min | No | No | 5 | RVC |
| A2 | Vertigo | <1 min | No | No | 10 | RVC |
| A3 | Vertigo | <1 min | No | No | 5 | RVC |
| A4 | Vertigo | <1 min | No | No | 5 | RVC |
| A5 | Vertigo | <1 min | No | No | 90 | RVC |
| A6 | Vertigo | <1 min | No | No | 7 | RVC |
| A7 | Vertigo | <1 min | No | No | 9 | RVC |
| A8 | Vertigo | <1 min | No | No | 100 | RVC |
| A9 | Vertigo | <1min | No | No | 8 | RVC |
| A10 | Vertigo | <1 min | No | No | 6 | RVC |
| A11 | Vertigo | <1 min | Yes | No | 8 | RVC |
| A12 | Vertigo | 5–20 min | Yes | No | 4 | RVC |
| A13 | Vertigo | <1 min | No | Yes | 12 | VMC |
| A14 | Unsteadiness | <1 min | No | Yes | 24 | VMC |
| A15 | Vertigo | <1 min | Yes | Yes | 90 | VMC |
| A16 | Vertigo | <1 min | No | Yes | 40 | VMC |
| A17 | Dizziness | <1 min | No | Yes | 10 | VMC |
| A18 | Vertigo | <1 min | No | No | 4 | Vestibular paroxysmia |
References
- Brodsky, J.R.; Lipson, S.; Bhattacharyya, N. Prevalence of Pediatric Dizziness and Imbalance in the United States. Otolaryngol. Head. Neck Surg. 2020, 16, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Li, C.M.; Hoffman, H.J.; Ward, B.K.; Cohen, H.S.; Rine, R.M. Epidemiology of Dizziness and Balance Problems in Children in the United States: A Population-Based Study. J. Pediatr. 2016, 171, 240–247. [Google Scholar] [CrossRef] [PubMed]
- Gioacchini, F.M.; Alicandri-Ciufelli, M.; Kaleci, S.; Magliulo, G.; Re, M. Prevalence and Diagnosis of Vestibular Disorders in Children: A Review. Int. J. Pediatr. Otorhinolaryngol. 2014, 78, 718–724. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.D.; Kim, C.H.; Hong, S.M.; Kim, S.H.; Suh, M.W.; Kim, M.B.; Shim, D.B.; Chu, H.; Lee, N.H.; Kim, M.; et al. Prevalence of Vestibular and Balance Disorders in Children and Adolescents According to Age: A Multi-Center Study. Int. J. Pediatr. Otorhinolaryngol. 2017, 94, 36–39. [Google Scholar] [CrossRef]
- Wang, A.; Zhou, G.; Lipson, S.; Kawai, K.; Corcoran, M.; Brodsky, J.R. Multifactorial Characteristics of Pediatric Dizziness and Imbalance. Laryngoscope 2021, 131, E1308–E1314. [Google Scholar] [CrossRef]
- Davitt, M.; Delvecchio, M.T.; Aronoff, S.C. The Differential Diagnosis of Vertigo in Children: A Systematic Review of 2726 Cases. Pediatr. Emerg. Care. 2020, 36, 368–371. [Google Scholar] [CrossRef]
- Gao, F.; Gong, S.S. Vertigo and Dizziness in Child: A Clinical Analysis in 120 Cases. Zhonghua Nei Ke Za Zhi. 2024, 63, 680–685. [Google Scholar] [CrossRef]
- van de Berg, R.; Widdershoven, J.; Bisdorff, A.; Evers, S.; Wiener Vacher, S.; Cushing, S.L.; Mack, K.J.; Kim, J.S.; Jahn, K.; Strupp, M.; et al. Vestibular Migraine of Childhood and Recurrent Vertigo of Childhood: Diagnostic Criteria. J. Vestib. Res. 2021, 31, 1–9. [Google Scholar] [CrossRef]
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018, 38, 1–211. [Google Scholar] [CrossRef]
- Bisdorff, A.; Von Brevern, M.; Lempert, T.; Newman-Toker, D.E. Classification of vestibular symptoms: Towards an international classification of vestibular disorders. J. Vestib. Res. 2009, 19, 1–13. [Google Scholar] [CrossRef]
- Teggi, R.; Colombo, B.; Familiari, M.; Cangiano, I.; Bussi, M.; Filippi, M. Phenotypes, Bedside Examination, and Video Head Impulse Test in Vestibular Migraine of Childhood Compared with Probable Vestibular Migraine and Recurrent Vertigo in Childhood. Front. Pediatr. 2023, 11, 1152928. [Google Scholar] [CrossRef]
- Strupp, M.; Lopez Escamez, J.A.; Kim, J.S.; Straumann, D.; Jen, J.C.; Carey, J.; Bisdorff, A.; Brandt, T. Vestibular Paroxysmia: Diagnostic Criteria. J. Vestib. Res. 2016, 26, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Wu, Q.; Chen, J.; Wang, X.; Zhang, Y.; Liu, S.; Wang, L.; Shen, J.; Shen, M.; Tang, X.; et al. Characteristics of Vestibular Migraine, Probable Vestibular Migraine, and Recurrent Vertigo of Childhood in Caloric and Video Head Impulse Tests. Front. Neurol. 2022, 13, 1050282. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Du, Y.; Liu, X.; Xu, Z.; Wang, Y.; Ren, L.; Wu, Z. Vestibular Migraine and Recurrent Vertigo in Children: A Diagnostic Focus From a Tertiary Hospital Study. Pediatr. Neurol. 2024, 158, 86–93. [Google Scholar] [CrossRef]
- Dunker, K.; Schnabel, L.; Grill, E.; Filippopulos, F.M.; Huppert, D. Recurrent Vertigo of Childhood: Clinical Features and Prognosis. Front. Neurol. 2022, 13, 1022395. [Google Scholar] [CrossRef]
- Lorente Piera, J.; Pérez Fernández, N.; Blanco Pareja, M.; Manrique Huarte, R.; Larenas, M.P.; Serra, V.; Manrique, M. Can We Predict Emotional Disability in Pediatric Patients with Vertigo and Dizziness? Audiol. Res. 2024, 14, 701–713. [Google Scholar] [CrossRef]
- Haripriya, G.R.; Lepcha, A.; Augustine, A.M.; John, M.; Philip, A.; Mammen, M.D. Prevalence, Clinical Profile, and Diagnosis of Pediatric Dizziness in a Tertiary Care Hospital. Int. J. Pediatr. Otorhinolaryngol. 2021, 146, 110761. [Google Scholar] [CrossRef]
- Basser, L.S. Benign Paroxysmal Vertigo of Childhood: A Variety of Vestibular Neuronitis. Brain. 1964, 87, 141–152. [Google Scholar] [CrossRef]
- Lempert, T.; Olesen, J.; Furman, J.; Waterston, J.; Seemungal, B.; Carey, J.; Bisdorff, A.; Versino, M.; Evers, S.; Newman Toker, D. Vestibular Migraine: Diagnostic Criteria. J. Vestib. Res. 2012, 22, 167–172. [Google Scholar] [CrossRef]
- Patterson Gentile, C.; Szperka, C.L.; Hershey, A.D. Cluster Analysis of Migraine associated Symptoms (CAMS) in Youth: A Retrospective Cross sectional Multicenter Study. Headache 2024, 64, 1230–1243. [Google Scholar] [CrossRef]
- Balzanelli, C.; Spataro, D.; Redaelli de Zinis, L.O. Prevalence of Pediatric and Adolescent Balance Disorders: Analysis of a Mono-Institutional Series of 472 Patients. Children 2021, 8, 1056. [Google Scholar] [CrossRef] [PubMed]
- Saniasiaya, J.; Salim, R. Characteristics and Diagnostic Approach of Vestibular Migraine in Children and Adolescents: A Systematic Review. Auris Nasus Larynx. 2023, 50, 218–227. [Google Scholar] [CrossRef] [PubMed]
- Batuecas-Caletrío, A.; Martín-Sánchez, V.; Cordero-Civantos, C.; Guardado-Sánchez, L.; Marcos, M.R.; Fabián, A.H.; Benito González, J.J.; Santa Cruz-Ruiz, S. Is benign paroxysmal vertigo of childhood a migraine precursor? Eur. J. Paediatr. Neurol. 2013, 17, 397–400. [Google Scholar] [CrossRef] [PubMed]
- Jahn, K.; Langhagen, T.; Heinen, F. Vertigo and Dizziness in Children. Curr. Opin. Neurol. 2015, 28, 78–82. [Google Scholar] [CrossRef]
- Gurberg, J.; Tomczak, K.K.; Brodsky, J.R. Benign paroxysmal vertigo of childhood. Handb. Clin. Neurol. 2023, 198, 229–240. [Google Scholar] [CrossRef]
- Zhang, F.; Shen, J.; Zhu, Q.; Wang, L.; Ma, X.; He, B.; Yang, Y.; Wang, W.; Chen, X.; Zhang, Q.; et al. Evaluating Children with Vestibular Migraine Through Vestibular Test Battery: A Cross-Sectional Investigation. Front. Neurol. 2022, 13, 997217. [Google Scholar] [CrossRef]
- Gao, D.; Sun, X.; Shen, J.; Ma, X.; Wang, L.; Chen, X.; Yang, J.; Chen, J. Clinical Characteristics of Vestibular Evoked Myogenic Potentials in Children with Recurrent Vertigo of Childhood. Int. J. Pediatr. Otorhinolaryngol. 2022, 161, 111257. [Google Scholar] [CrossRef]
- Hwa, T.P.; Patel, V.; Field, E.; Windsor, A.; Spencer, L.M.; Caine, M.; O’Reilly, R.C. Asymmetric Ocular Vestibular Evoked Myogenic Potentials in Pediatric Vestibular Migraine. Otol. Neurotol. 2023, 44, 578–583. [Google Scholar] [CrossRef]
| Clinical Entity | Diagnostic Criteria |
|---|---|
| RVC 1 | A. At least three episodes with vestibular symptoms of moderate or severe intensity, lasting between 1 min and 72 h B. None of the criteria B and C for vestibular migraine of childhood C. Age < 18 years D. Not better accounted for by another headache disorder, vestibular disorder, or other condition |
| VMC 2 | A. At least five episodes with vestibular symptoms of moderate or severe intensity, lasting between five minutes and 72 h B. A current or past history of migraine with or without aura C. At least half of episodes are associated with at least one of the following three migraine features: 1. Headache with at least two of the following four characteristics: (a) One-sided location (b) Pulsating quality (c) Moderate or severe pain intensity (d) Aggravation by routine physical activity 2. Photophobia and phonophobia 3. Visual aura D. Age < 18 years E. Not better accounted for by another headache disorder, vestibular disorder, or other condition |
| pVMC 3 | A. At least three episodes with vestibular symptoms of moderate or severe intensity, lasting between five minutes and 72 h B. Only one of the criteria B and C for vestibular migraine of childhood C. Age < 18 years D. Not better accounted for by another headache disorder, vestibular disorder, or other condition |
| BPV 4 | A. At least five attacks fulfilling criteria B and C B. Vertigo occurring without warning, maximal at onset, and resolving spontaneously after minutes to hours without loss of consciousness C. At least one of the following five associated symptoms or signs: 1. nystagmus 2. ataxia 3. vomiting 4. pallor 5. fearfulness D. Normal neurological examination and audiometric and vestibular functions between attacks E. Not attributed to another disorder. |
| VM 5 | A. At least 5 episodes with vestibular symptoms of moderate or severe intensity, lasting 5 min to 72 h B. Current or previous history of migraine with or without aura according to the International Classification of Headache Disorders (ICHD) C. One or more migraine features with at least 50% of the vestibular episodes: 1. headache with at least two of the following characteristics: (a) one-sided location (b) pulsating quality, (c) moderate or severe pain intensity (d) aggravation by routine physical activity 2. photophobia and phonophobia 3. visual aura D. Not better accounted for by another vestibular or ICHD diagnosis |
| pVM 6 | A. At least 5 episodes with vestibular symptoms of moderate or severe intensity, lasting 5 min to 72 h. B. Only one of the criteria B and C for vestibular migraine is fulfilled (migraine history or migraine features during the episode). C. Not better accounted for by another vestibular or ICHD diagnosis. |
| Diagnostic Criterion | ICHD-3, 2018 | Bárány Society, 2021 |
|---|---|---|
| Minimum number of episodes | ≥5 (BPV and VM) | RVC and pVMC: ≥3 episodes VMC: ≥5 episodes |
| Duration of episodes | BPV: minutes to hours (no lower limit) VM: 5 min to 72 h | RVC: ≥1 min pVMC and VMC: ≥5 min to 72 h |
| Migraine history | VM: required BPV: not defined | VMC: required RVC: absent |
| Migraine features during episodes | VM: required (≥50% episodes) | VMC: required RVC: absent |
| Allowed symptoms | BPV: vertigo ± signs/other symptoms (nystagmus, ataxia, vomiting, pallor, fear) VM: specified vestibular symptoms | RVC: vestibular symptoms VMC, pVMC: specified vestibular symptoms |
| Age restrictions | BPV: <18 y VM: any age | All three (RVC, pVMC, VMC) apply <18 y |
| Terminology | BPV (childhood) pVMC and VM (all ages) | BPV replaced by RVC VMC and pVMC |
| RVC 1 N = 55 | VMC 2 N = 23 | pVMC 3 N = 13 | EVSw/oHL 4 N = 18 | p-Value | Post hoc Test ∆ | |
|---|---|---|---|---|---|---|
| Women CI 95% | 30 (54.55) 40.554–68.030 | 14 (60.87) 38.542–80.292 | 10 (76.92) 46.187–94.962 | 10 (55.56) 30.757–78.470 | 0.528 | |
| Onset (yrs) ** CI 95% | 10 (5) 8.201–10.090 | 10 (3) 9.895–11.931 | 12 (4) 9.037–12.809 | 10.5 (3) 8.151–11.515 | 0.131 | |
| Diagnosis (yrs) ** CI 95% | 11 (4) 8.939–10.843 | 12 (4) 10.992–12.834 | 13 (3) 9.977–14.177 | 11 (4) 8.913–12.309 | 0.044 | 1 vs. 2: p = 0.069 1 vs. 3: p = 0.083 |
| External vertigo * CI 95% | 41 (74.55) 60.997–85.330 | 16 (69.57) 47.080–86.790 | 12 (92.31) 63.970–99.805 | 13 (72.22) 46.520–90.305 | 0.479 | |
| Internal vertigo * CI 95% | 4 (7.27) 2.017–17.587 | 3 (13.04) 2.775–33.589 | 2 (15.38) 1.921–45.447 | 0 (0) | 0.292 | |
| Dizziness * CI 95% | 11 (20) 10.430–32.973 | 7 (30.43) 13.210–52.919 | 1 (7.69) 0.195–36.030 | 5 (27.78) 9.694–53.480 | 0.397 | |
| Unsteadiness * CI 95% | 19 (34.55) 22.237–48.581 | 13 (56.52) 34.494–76.809 | 3 (23.08) 5.038–53.813 | 16 (33.33) 13.343–59.007 | 0.188 | |
| Posit. vertigo * CI 95% | 3 (5.45) 1.139–15.124 | 1 (4.35) 0.110–21.949 | 2 (15.38) 1920–45.447 | 3 (16.67) 3.579–41.418 | 0.243 | |
| Visual vertigo * CI 95% | 1 (1.82) 0.046–9.719 | 0 (0) | 2 (15.38) 1.921–45.447 | 1 (5.56) 0.141–27.294 | 0.082 | |
| Hearing loss * CI 95% | 2 (3.64) 0.443–12.526 | 0 (0) | 1 (7.69) 0.019–36.030 | 1 (5.56) 0.141–27.294 | 0.549 | |
| Tinnitus * CI 95% | 11 (20) 10.430–32.973 | 5 (21.74) 7.460–43.703 | 4 (30.77) 9.092–61.426 | 3 (16.67) 3.579–41.418 | 0.796 | |
| Ear fullness * CI 95% | 3 (5.45) 1.140–15.124 | 3 (13.04) 2.775–33.589 | 1 (7.69) 0.194–36.030 | 0 (0) | 0.374 | |
| Headache * CI 95% | 22 (40) 27.023–54.093 | 23 (100) 85.181–100 | 13 (100) 75.295–100 | 10 (55.56) 30.747–78.470 | 0.000 | 2 vs. 4: p = 0.003 2 vs. 1: p = 0.000 3 vs. 1: p = 0.000 3 vs. 4: p = 0.058 |
| Migraine * CI 95% | 0 (0) | 23 (100) 85.181–100 | 9 (69.23) 38.574–90.908 | 5 (27.78) 9.695–53.480 | 0.000 | 2 vs. 4: p = 0.000 2 vs. 1: p = 0.000 3 vs. 1: p = 0.000 4 vs. 1: p = 0.003 |
| Nausea * CI 95% | 21 (38.18) 25.409–52.273 | 10 (43.48) 23.191–65.505 | 9 (69.23) 38.574–90.908 | 4 (22.22) 6.409–47.637 | 0.072 | |
| Vomiting * CI 95% | 13 (23.64) 13.228–37.020 | 8 (34.78) 16.376–57.266 | 7 (53.85) 25.135–80.777 | 0 (0) | 0.002 | 2 vs. 4: p = 0.034 3 vs. 4: p = 0.004 |
| FH migraine * CI 95% | 23 (41.82) 28.654–55.894 | 19 (82.61) 61.122–95.049 | 9 (69.23) 38.574–90.908 | 11 (61.11) 35.745–82.701 | 0.006 | 2 vs. 1: p = 0.007 |
| FH HL * CI 95% | 10 (18.18) 9.080–30.905 | 3 (13.04) 2.775–33.589 | 0 (0) | 3 (16.67) 3.579–41.418 | 0.457 | |
| FH vertigo * CI 95% | 22 (40) 27.023–54.093 | 6 (26.09) 10.229–48.405 | 2 (15.38) 1.921–45.447 | 2 (11.11) 1.375–34.712 | 0.075 |
| RVC 1 N = 55 | VMC 2 N = 23 | pVMC 3 N = 13 | EVSw/oHL 4 N = 18 | |
|---|---|---|---|---|
| <1 min * CI 95% | 0 (0) | 0 (0) | 0 (0) | 17 (94.44) 72.706–99.860 |
| 1–5 min * CI 95% | 30 (54.55) 40.554–68.030 | 0 (0) | 0 (0) | 0 (0) |
| 5–20 min * CI 95% | 10 (18.18) 9.070–30.905 | 9 (39.13) 19.708–61.458 | 10 (76.92) 46.187–94.962 | 1 (5.56) 0.140–27.294 |
| 20–60 min * CI 95% | 6 (10.91) 4.110–22.471 | 5 (21.74) 7.460–43.703 | 0 (0) | 0 (0) |
| >60 min * CI 95% | 9 (16.36) 7.767–28.803 | 9 (39.13) 19.708–61.458 | 3 (23.08) 5.038–53.813 | 0 (0) |
| EVSw/oHL 1 N = 18 | |
|---|---|
| Nº episodes * | 24.28 (19) |
| Dizziness ** | 1 (5.56) |
| Unsteadiness ** | 1 (5.56) |
| Vertigo ** | 16 (88.89) |
| Duration of episodes ** | |
| <1 min | 17 (94.44) |
| 5–20 min | 1 (5.56) |
| Plausible diagnosis ** | |
| RVC | 12 (66.67) |
| VMC | 5 (27.78) |
| Vestibular paroxysmia | 1 (5.56) |
| Auditory symptoms ** | 3 (16.67) |
| Migraine ** | 5 (27.78) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rey-Berenguel, M.; Vallecillo-Zorrilla, J.; Burgueño-Uriarte, E.K.; Olvera-Porcel, M.d.C.; Espinosa-Sanchez, J.M. Diagnostic Yield of the New Bárány Society Criteria for Pediatric Episodic Vestibular Syndrome. J. Clin. Med. 2025, 14, 5971. https://doi.org/10.3390/jcm14175971
Rey-Berenguel M, Vallecillo-Zorrilla J, Burgueño-Uriarte EK, Olvera-Porcel MdC, Espinosa-Sanchez JM. Diagnostic Yield of the New Bárány Society Criteria for Pediatric Episodic Vestibular Syndrome. Journal of Clinical Medicine. 2025; 14(17):5971. https://doi.org/10.3390/jcm14175971
Chicago/Turabian StyleRey-Berenguel, Mar, Javier Vallecillo-Zorrilla, Edith Karelly Burgueño-Uriarte, María del Carmen Olvera-Porcel, and Juan Manuel Espinosa-Sanchez. 2025. "Diagnostic Yield of the New Bárány Society Criteria for Pediatric Episodic Vestibular Syndrome" Journal of Clinical Medicine 14, no. 17: 5971. https://doi.org/10.3390/jcm14175971
APA StyleRey-Berenguel, M., Vallecillo-Zorrilla, J., Burgueño-Uriarte, E. K., Olvera-Porcel, M. d. C., & Espinosa-Sanchez, J. M. (2025). Diagnostic Yield of the New Bárány Society Criteria for Pediatric Episodic Vestibular Syndrome. Journal of Clinical Medicine, 14(17), 5971. https://doi.org/10.3390/jcm14175971





