Prevalence of the Os Supranaviculare: A Systematic Review with Meta-Analysis
Abstract
1. Introduction
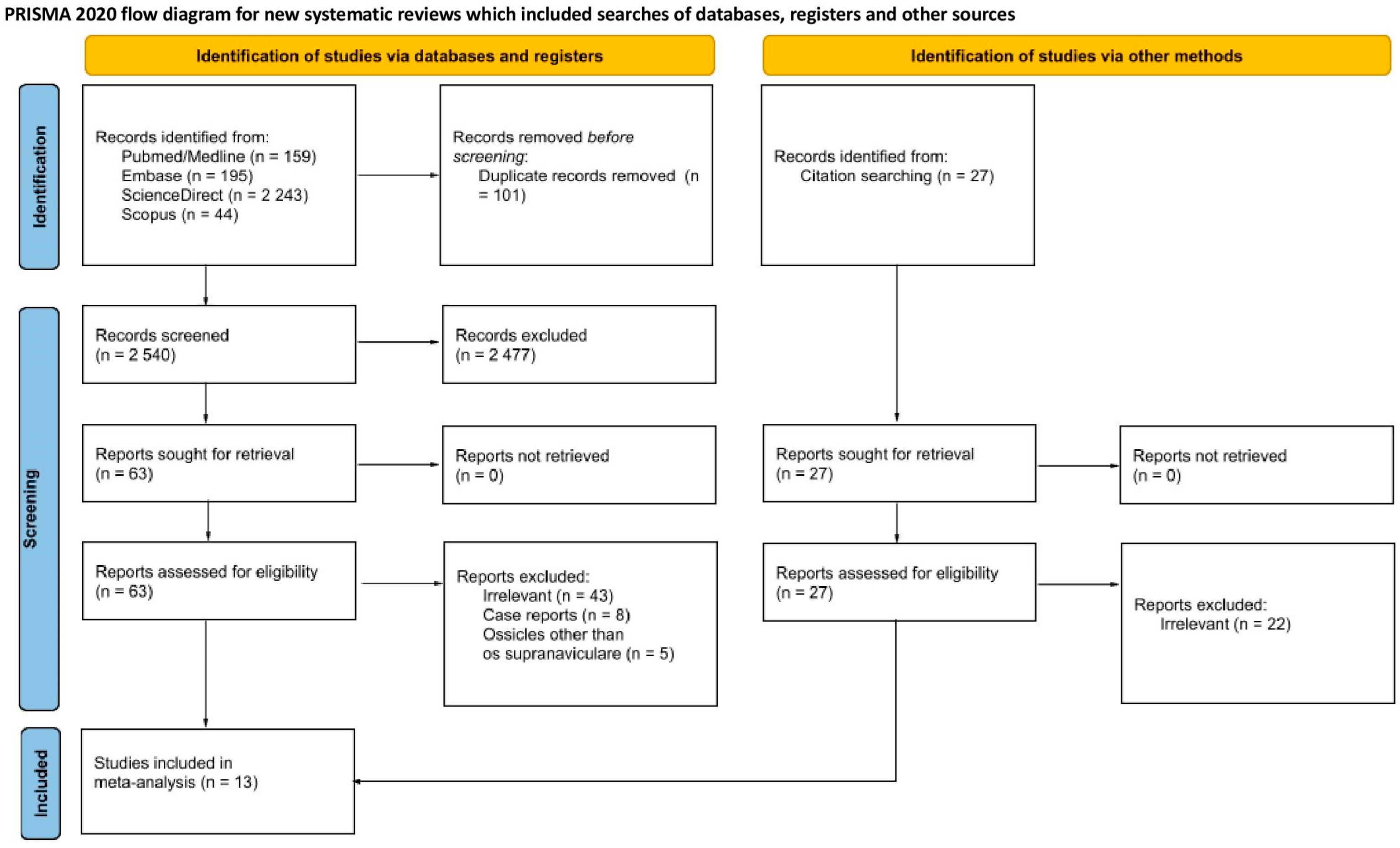
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Study Selection and Data Extraction
2.4. Quality Assessment
2.5. Statistical Analysis
3. Results
3.1. Study Characteristics
3.2. Quality Assessment
3.3. General Prevalence
3.4. Sex-Specific Prevalence
3.5. Geographical Distribution
3.6. Prevalence Based on Population Size
4. Discussion
4.1. Clinical Implications, Diagnosis and Treatment
4.2. Methodological Considerations and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| OSSN | Os Supranaviculare |
| NSF | Navicular Stress Fracture |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| CT | Computed Tomography |
| MRI | Magnetic Resonance Imaging |
| PPE | Pooled Prevalence Estimate |
| 95%CI | 95% Confidence Intervals |
| 95%PI | 95% Prediction Intervals |
| LFK index | Luis Furuya-Kanamori index |
References
- Coskun, N.; Yuksel, M.; Cevener, M.; Arican, R.Y.; Ozdemir, H.; Bircan, O.; Sindel, T.; Ilgi, S.; Sindel, M. Incidence of accessory ossicles and sesamoid bones in the feet: A radiographic study of the Turkish subjects. Surg. Radiol. Anat. 2009, 31, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Gottlieb, C.; Beranbaum, S.L. Pirie’s bone. Radiology 1950, 55, 423–424. [Google Scholar] [CrossRef]
- Candan, B.; Torun, E.; Dikici, R. The Prevalence of Accessory Ossicles, Sesamoid Bones, and Biphalangism of the Foot and Ankle: A Radiographic Study. Foot Ankle Orthop. 2022, 7, 24730114211068792. [Google Scholar] [CrossRef]
- Stolarz, K.; Osiowski, A.; Preinl, M.; Jasiewicz, B.; Taterra, D. The prevalence and anatomy of accessory navicular bone: A meta-analysis. Surg. Radiol. Anat. 2024, 46, 1731–1743. [Google Scholar] [CrossRef]
- Azawi, D.; Mahsouli, A.; Vanhoenacker, F. Os supranaviculare as a predisposing factor to navicular stress fractures. J. Belg. Soc. Radiol. 2021, 105, 81. [Google Scholar] [CrossRef]
- Kim, W.-J.; Jung, K.-J.; Yeo, E.-D.; Lee, H.-S.; Won, S.-H.; Lee, D.-W.; Ji, J.-Y.; Yoon, S.-J.; Hong, Y.-C. Treatment of Navicular Stress Fracture Accompanied by Os Supranaviculare: A Case Report. Medicina 2021, 58, 27. [Google Scholar] [CrossRef]
- Sugimoto, K.; Isomoto, S.; Miura, K.; Wakiyama, S.; Yoneda, A.; Taniguchi, A.; Tanaka, Y. Treatment of Symptomatic Os Supranaviculare in Athletes. Foot Ankle Int. 2024, 45, 593–600. [Google Scholar] [CrossRef]
- Kinoshita, T.; Hashimoto, Y.; Inui, K.; Sugama, R.; Sugimoto, T.; Akizuki, Y.; Nakamura, H. Male elite soccer players have a higher incidence of accessory ossicles in the foot and ankle. Int. Orthop. 2024, 48, 1049–1055. [Google Scholar] [CrossRef] [PubMed]
- Keles-Celik, N.; Kose, O.; Sekerci, R.; Aytac, G.; Turan, A.; Güler, F. Accessory Ossicles of the Foot and Ankle: Disorders and a Review of the Literature. Cureus 2017, 9, e1881. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
- Henry, B.M.; Marcinów, A.; Pękala, P.; Taterra, D.; Loukas, M.; Tubbs, R.S.; A Walocha, J.; Tomaszewski, K. Polish translation of the Anatomical Quality Assurance (AQUA) Checklist: New guidelines for reporting in original anatomical studies. Folia Med. Cracov. 2017, 57, 105–116. [Google Scholar] [PubMed]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.T.; Rothstein, H.R. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res. Synth. Methods 2010, 1, 97–111. [Google Scholar] [CrossRef]
- IntHout, J.; Ioannidis, J.P.A.; Rovers, M.M.; Goeman, J.J. Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open 2016, 6, e010247. [Google Scholar] [CrossRef] [PubMed]
- Henry, B.M.; Tomaszewski, K.A.; Walocha, J.A. Methods of Evidence-Based Anatomy: A guide to conducting systematic reviews and meta-analysis of anatomical studies. Ann. Anat. 2016, 205, 16–21. [Google Scholar] [CrossRef]
- Furuya-Kanamori, L.; Barendregt, J.J.; Doi, S.A.R. A new improved graphical and quantitative method for detecting bias in meta-analysis. Int. J. Evid.-Based Healthc. 2018, 16, 195–203. [Google Scholar] [CrossRef]
- Naing, L.; Winn, T. Practical Issues in Calculating the Sample Size for Prevalence Studies. Arch. Orofac. Sci. 2006, 1, 9–14. [Google Scholar]
- Tsuruta, T.; Shiokawa, Y.; Kato, A.; Matsumoto, T.; Yamazoe, Y.; Oike, T.; Sugiyama, T.; Saito, M. Radiological study of the accessory skeletal elements in the foot and ankle. J. Jpn. Orthop. Assoc. 1981, 55, 357–370. [Google Scholar] [CrossRef]
- Cilli, F.A.M. The incidence of accessory bones of the foot and their clinical significance. Acta Orthop. Traumatol. Turc. 2005, 36, 243–246. [Google Scholar]
- Bizarro, A.H. On sesamoid and supernumerary bones of the limbs. J. Anat. 1921, 55, 256–268. [Google Scholar] [PubMed]
- Capecchi, V.; Cicala, G.; Crisafulli, A. Le ossa soprannumerarie del piede (Parte I). Acta Orthop. Ital. 1964, 10, 9. [Google Scholar]
- Heimerzheim, A. Über einige akzessorische Fußwurzelknochen nebst ihrer chirurgischen Bedeutung. Langenbeck’s Arch. Surg. 1925, 190, 96–112. [Google Scholar] [CrossRef]
- Leimbach, G. Beiträge zur Kenntnis der inkonstanten Skeletelemente des Tarsus. (Akzessorische Fußwurzelknochen.). Arch. Orthop. Trauma. Surg. 1937, 38, 431–448. [Google Scholar] [CrossRef]
- Schönekeß, P. Anomalien der Fusswurzelknochen. 1935; pp. 1–20. [Google Scholar]
- Tsuruta, T. NMSMOYMS. About the inconstant skeletal elements of the foot. Mie Med. J. 1968, 55, 357–370. [Google Scholar]
- Shands, A.R.; Durham, N.C. The accessory bones of the foot—An X-Ray study of the feet of 1054 patients. South Med. Surg. 1931, 93, 326–334. [Google Scholar]
- Ochs, B.M. Prävalenzbestimmung von Akzessorischen Skelettelementen im Bereich der Fußwurzel und des Oberen Sprunggelenks Beim Erwachsenen. Doctoral Dissertation, Charité—Universitätsmedizin Berlin, Berlin, Germany, 2021. [Google Scholar]
- Kalbouneh, H.; Alajoulin, O.; Shawaqfeh, J.; Mustafa, A.; Jaber, S.; Zaben, S.; Zapen, J.; Alsalem, M. Accessory ossicles in the region of the foot and ankle: An epidemiologic survey in a jordanian population. Medicina 2021, 57, 1178. [Google Scholar] [CrossRef]
- Preinl, M.; Osiowski, A.; Stolarz, K.; Osiowski, M.; Taterra, D. Prevalence and clinical aspects of os trigonum: A meta-analysis. Anat. Sci. Int. 2024, 100, 287–297. [Google Scholar] [CrossRef]
- Preinl, M.; Osiowski, A.; Osiowski, M.; Baran, K.; Stolarz, K.; Jasiewicz, B.; Taterra, D. Clinical aspects and epidemiology of os peroneum: A meta-analysis. Anat. Sci. Int. 2025, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Osiowski, A.; Preinl, M.; Osiowski, M.; Baran, K.; Jasiewicz, B.; Taterra, D. The prevalence and clinical considerations of Os Vesalianum Pedis: A meta-analysis. Foot Ankle Surg. 2025; in press. [Google Scholar] [CrossRef] [PubMed]
- Mellado, J.M.; Ramos, A.; Salvadó, E.; Camins, A.; Danús, M.; Saurí, A. Accessory ossicles and sesamoid bones of the ankle and foot: Imaging findings, clinical significance and differential diagnosis. Eur. Radiol. 2003, 13 (Suppl. S6), L164–L177. [Google Scholar] [CrossRef]
- Miller, T.T. Painful accessory bones of the foot. Semin. Musculoskelet. Radiol. 2002, 6, 153–161. [Google Scholar] [CrossRef]
- Chiu, N.-T.; Jou, I.-M.; Lee, B.-F.; Yao, W.-J.; Tu, D.-G.; Wu, P.-S. Symptomatic and Asymptomatic Accessory Navicular Bones: Findings of Tc-99m MDP Bone Scintigraphy. Clin. Radiol. 2000, 55, 353–355. [Google Scholar] [CrossRef]
- Uslu, M.; Arıcan, M.; Erdoğmuş, B. A Rare Case of Os Supranaviculare or Pirie’s Bone in the Pediatric Patient: A Case Report. Foot Ankle Online J. 2012, 5, 1–3. [Google Scholar] [CrossRef]
- Zwelling, L.; Gunther, S.F.; Hockstein, E. Removal of os supranaviculare from a runner’s painful foot: A case report. Am. J. Sports Med. 1978, 6, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Heckman, J.D.; McLean, M.R. Fractures of the lateral process of the talus. Clin. Orthop. Relat. Res. 1985, 199, 108–113. [Google Scholar] [CrossRef]
- Pavlov, H.; Torg, J.S.; Freiberger, R.H. Tarsal navicular stress fractures: Radiographic evaluation. Radiology 1983, 148, 641–645. [Google Scholar] [CrossRef] [PubMed]
- Ingalls, J.; Wissman, R. The os supranaviculare and navicular stress fractures. Skeletal. Radiol. 2011, 40, 937–941. [Google Scholar] [CrossRef]
- Drexelius, K.; Bartolomei, J.; Shu, A.; Hunt, K.J. Os supranaviculare and navicular osteochondral lesion contributing to the development of a navicular stress fracture in an adolescent male athlete: Case report. J. ISAKOS: Jt. Disord. Orthop. Sports Med. 2022, 8, 128–134. [Google Scholar] [CrossRef]
- Bayramoğlu, A.; Demiryürek, D.; Firat, A.; Oznur, A.; Ozsoy, M.H. Differential diagnosis in a professional basketball player with foot pain: Is it an avulsion fracture or an os supranaviculare? Jt. Dis. Relat. Surg. 2009, 20, 59–61. [Google Scholar] [PubMed]



| Author, Year | Origin of the Study | Diagnostic Modality | Prevalence Reporting Format (per Foot/per Patient) | Number of Feet Examined | Number of Feet with OSSN |
|---|---|---|---|---|---|
| Bizarro, 1921 [19] | England | X-ray | Per foot | 100 | 1 |
| Candan, 2022 [3] | Turkey | X-ray | Per foot | 1651 | 6 |
| Capecchi, 1964 [20] | Italy | X-ray | Per foot | 2155 | 6 |
| Cilli, 2005 [18] | Turkey | X-ray | Per foot | 464 | 3 |
| Coskun, 2009 [1] | Turkey | X-ray | Per foot | 1968 | 19 |
| Heimerzheim, 1925 [21] | England | X-ray | Per foot | 1800 | 12 |
| Kalbouneh, 2021 [27] | Jordan | X-ray | Per foot | 1000 | 7 |
| Leimbah, 1937 [22] | Germany | X-ray | Per foot | 500 | 8 |
| Ochs, 2021 [26] | Germany | X-ray | Per foot | 1820 | 43 |
| Schönekeß, 1935 [23] | Germany | X-ray | Per foot | 1324 | 18 |
| Shands, 1931 [25] | USA | X-ray | Per foot | 1054 | 5 |
| Tsuruta, 1968 [24] | Japan | X-ray | Per foot | 1449 | 16 |
| Tsuruta, 1981 [17] | Japan | X-ray | Per foot | 3460 | 35 |
| Risk of Bias | |||||
|---|---|---|---|---|---|
| Author, Year | Objective(S) and Study Characteristics | Study Design | Methodology Characterization | Descriptive Anatomy | Reporting of Results |
| Bizarro, 1921 [19] | LOW | UNCLEAR | LOW | LOW | LOW |
| Candan, 2022 [3] | LOW | LOW | LOW | LOW | LOW |
| Capecchi, 1964 [20] | LOW | HIGH | HIGH | LOW | LOW |
| Cilli, 2005 [18] | LOW | LOW | LOW | LOW | LOW |
| Coskun, 2009 [1] | LOW | LOW | LOW | LOW | LOW |
| Heimerzheim, 1925 [21] | UNCLEAR | LOW | UNCLEAR | UNCLEAR | LOW |
| Kalbouneh, 2021 [27] | LOW | LOW | LOW | LOW | LOW |
| Leimbah, 1937 [22] | LOW | LOW | UNCLEAR | UNCLEAR | LOW |
| Ochs, 2021 [26] | LOW | LOW | LOW | LOW | LOW |
| Schönekeß, 1935 [23] | LOW | UNCLEAR | LOW | LOW | LOW |
| Shands, 1931 [25] | UNCLEAR | LOW | LOW | LOW | LOW |
| Tsuruta, 1968 [24] | LOW | LOW | UNCLEAR | LOW | LOW |
| Tsuruta, 1981 [17] | LOW | LOW | UNCLEAR | LOW | LOW |
| Category | Subgroup | Number of Studies (Number of Feet) | Number of OSSN | Prevalence (95%CI); (95%PI) | I2 (95%CI) | Cochran’s Q; p-Value |
|---|---|---|---|---|---|---|
| General | 13 (18,745) | 179 | 0.88% (0.62–1.24%); (0.26–2.97%) | 78.41% (63.59–87.20%) | 55.59; p < 0.001 | |
| Sex | Males | 3 (2986) | 25 | 0.87% (0.58–1.32%); - | 7.75% (0.00–90.40%) | 2.17; p = 0.338 |
| Females | 3 (3125) | 23 | 0.48% (0.14–1.64%); - | 68.80% (0.00–90.93%) | 6.41; p = 0.041 | |
| Origin | Asia | 6 (9992) | 86 | 0.87% (0.66–1.13%); (0.47–1.61%) | 28.58% (0.00–70.65%) | 7.00; p = 0.221 |
| Europe | 6 (7699) | 88 | 1.04% (0.55–1.96%); (0.12–8.32%) | 85.53% (70.47–92.91%) | 34.55; p < 0.001 | |
| Sample size | Insufficient (<1521 feet) | 7 (5891) | 58 | 1.02% (0.75–1.39%); (0.54–1.94%) | 22.58% (0.00–65.51%) | 7.75; p = 0.257 |
| Sufficient (>1521 feet) | 6 (12,854) | 121 | 0.79% (0.44–1.42%); (0.10–6.02%) | 89.48% (79.76–94.53%) | 47.52; p < 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Osiowski, M.; Osiowski, A.; Preinl, M.; Fibiger, G.; Majka, K.; Jasiewicz, B.; Taterra, D. Prevalence of the Os Supranaviculare: A Systematic Review with Meta-Analysis. J. Clin. Med. 2025, 14, 5934. https://doi.org/10.3390/jcm14175934
Osiowski M, Osiowski A, Preinl M, Fibiger G, Majka K, Jasiewicz B, Taterra D. Prevalence of the Os Supranaviculare: A Systematic Review with Meta-Analysis. Journal of Clinical Medicine. 2025; 14(17):5934. https://doi.org/10.3390/jcm14175934
Chicago/Turabian StyleOsiowski, Maksymilian, Aleksander Osiowski, Maciej Preinl, Grzegorz Fibiger, Katarzyna Majka, Barbara Jasiewicz, and Dominik Taterra. 2025. "Prevalence of the Os Supranaviculare: A Systematic Review with Meta-Analysis" Journal of Clinical Medicine 14, no. 17: 5934. https://doi.org/10.3390/jcm14175934
APA StyleOsiowski, M., Osiowski, A., Preinl, M., Fibiger, G., Majka, K., Jasiewicz, B., & Taterra, D. (2025). Prevalence of the Os Supranaviculare: A Systematic Review with Meta-Analysis. Journal of Clinical Medicine, 14(17), 5934. https://doi.org/10.3390/jcm14175934






