Current Physical Therapy for Skin Scar Management: A Scoping Review
Abstract
1. Introduction
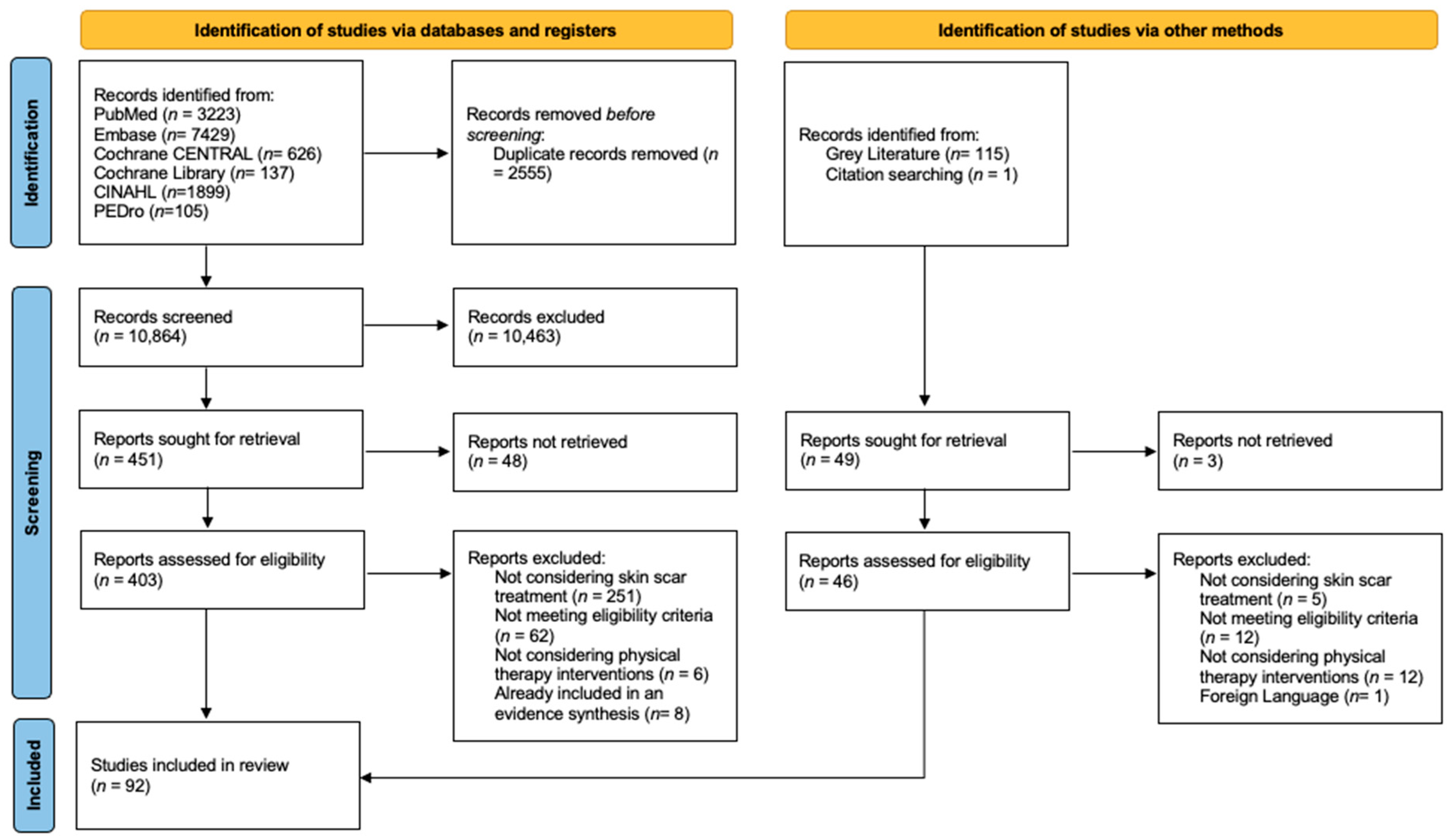
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Strategy
2.3. Study Selection and Data Extraction
3. Results
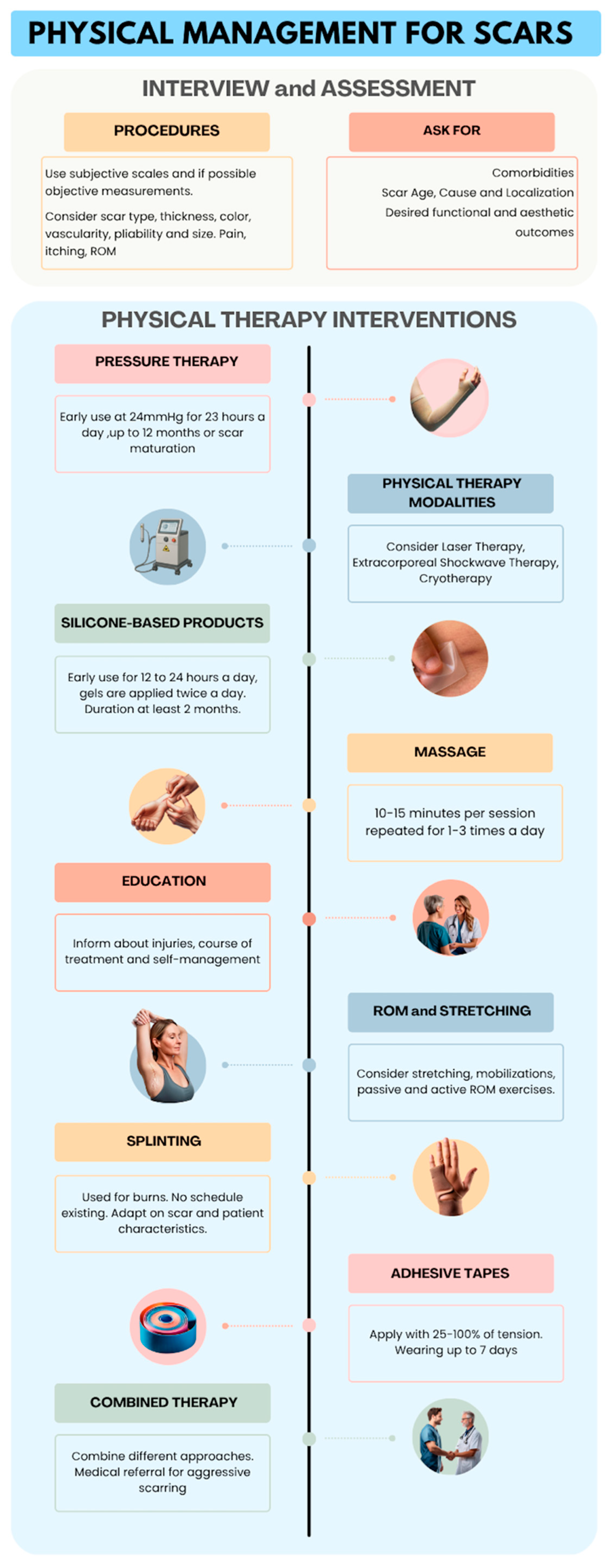
3.1. Assessment Methods
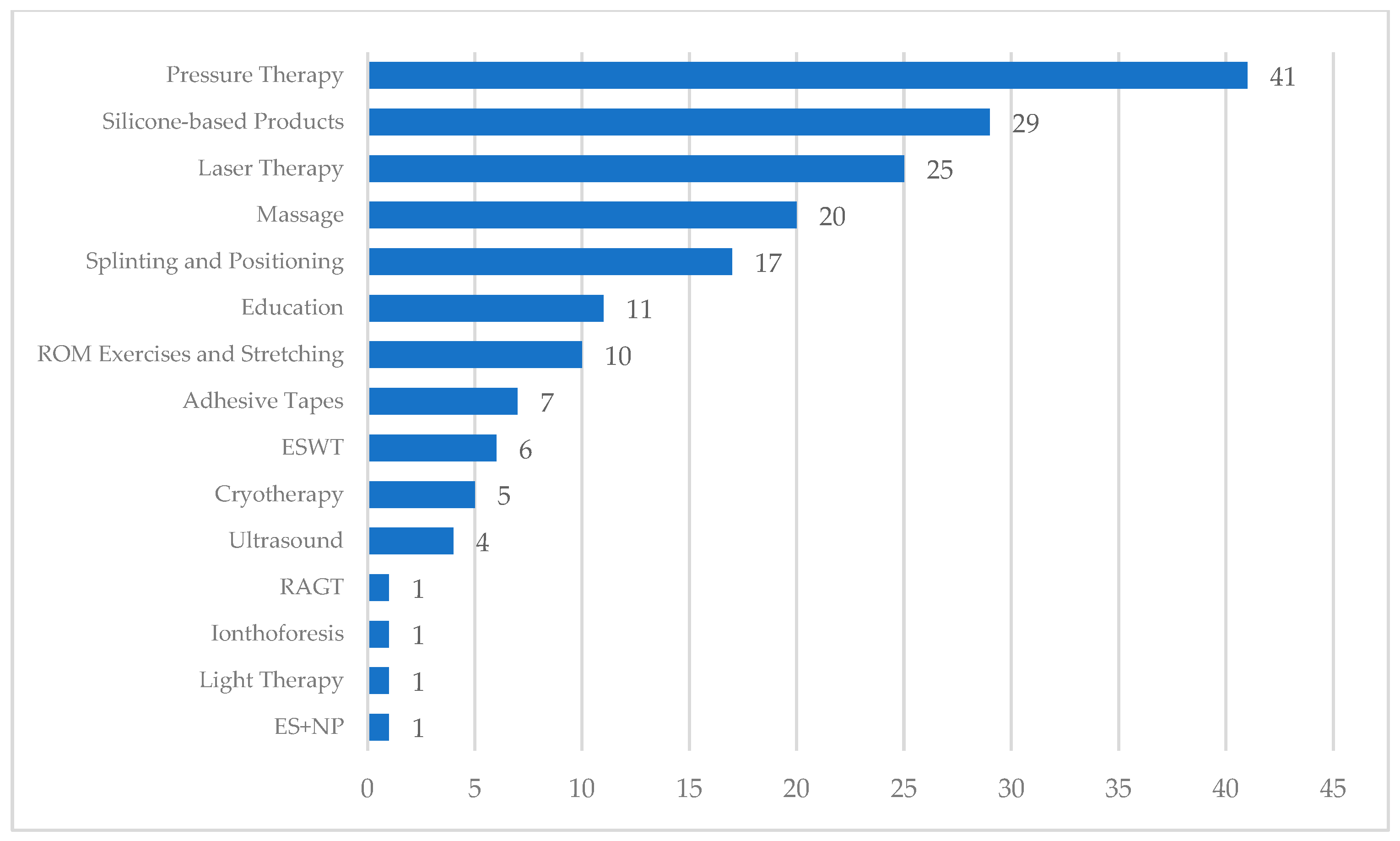
3.2. Interventions
3.3. Summary of Reported Effects
4. Discussion
4.1. Assessment Procedures
4.2. Pressure Therapy
4.3. Physical Modalities
4.3.1. Laser Therapy
4.3.2. Extracorporeal Shockwave Therapy
4.3.3. Cryotherapy
4.3.4. Other Modalities
4.4. Silicone-Based Products
4.5. Massage
4.6. Splinting
4.7. Education
4.8. Stretching and Mobilizations
4.9. Adhesive Tapes
4.10. Robot-Assisted Gait Training
4.11. Limitations
4.12. Implications for Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sund, B. New Developments in Wound Care; Clinica Reports: Hong Kong SAR, China, 2000. [Google Scholar]
- Bayat, A.; McGrouther, D.A.; Ferguson, M.W.J. Skin scarring. BMJ 2003, 326, 88–92. [Google Scholar] [CrossRef]
- Smolle, C.; Cambiaso-Daniel, J.; Forbes, A.A.; Wurzer, P.; Hundeshagen, G.; Branski, L.K.; Huss, F.; Kamolz, L.-P. Recent trends in burn epidemiology worldwide: A systematic review. Burns 2017, 43, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, R.; Akaishi, S. Endothelial dysfunction may play a key role in keloid and hypertrophic scar pathogenesis—Keloids and hypertrophic scars may be vascular disorders. Med. Hypotheses 2016, 96, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, R. Mechanobiology of Cutaneous Scarring. In Textbook on Scar Management: State of the Art Management and Emerging Technologies; Téot, L., Mustoe, T.A., Middelkoop, E., Gauglitz, G.G., Eds.; Springer: Cham, Germany, 2020. [Google Scholar]
- Seifert, O.; Mrowietz, U. Keloid scarring: Bench and bedside. Arch. Dermatol. Res. 2009, 301, 259–272. [Google Scholar] [CrossRef] [PubMed]
- Bock, O.; Schmid-Ott, G.; Malewski, P.; Mrowietz, U. Quality of life of patients with keloid and hypertrophic scarring. Arch. Dermatol. Res. 2006, 297, 433–438. [Google Scholar] [CrossRef]
- Anthonissen, M.; Daly, D.; Janssens, T.; Van den Kerckhove, E. The effects of conservative treatments on burn scars: A systematic review. Burns 2016, 42, 508–518. [Google Scholar] [CrossRef]
- Deflorin, C.; Hohenauer, E.; Stoop, R.; van Daele, U.; Clijsen, R.; Taeymans, J. Physical Management of Scar Tissue: A Systematic Review and Meta-Analysis. J. Altern. Complement. Med. 2020, 26, 854–865. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Godfrey, C.; McInerney, P.; Munn, Z. Chapter 11: Scoping Reviews. In JBI Manual for Evidence Synthesi; JBI: North Adelaide, Australia, 2020. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Serio, S.D.; Congiu, M.; Minnucci, S.; Scalise, V.; Mourad, F. Current Physical Therapy for Skin Scars Management: A Scoping Review Protocol. medRxiv 2024. [Google Scholar] [CrossRef]
- Rethlefsen, M.L.; Kirtley, S.; Waffenschmidt, S.; Ayala, A.P.; Moher, D.; Page, M.J.; Koffel, J.B. PRISMA-S: An extension to the PRISMA Statement for Reporting Literature Searches in Systematic Reviews. Syst. Rev. 2021, 10, 39. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Macintyre, L.; Baird, M. Pressure garments for use in the treatment of hypertrophic scars—A review of the problems associated with their use. Burns 2006, 32, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.-J.; Ko, J.-Y.; Chou, W.-Y.; Cheng, J.-H.; Kuo, Y.-R. Extracorporeal shockwave therapy for treatment of keloid scars. Wound Repair Regen. 2018, 26, 69–76. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Li-Tsang, C.W.P.; Zheng, Y.P.; Lau, J.C.M. A randomized clinical trial to study the effect of silicone gel dressing and pressure therapy on posttraumatic hypertrophic scars. J. Burn Care Res. 2010, 31, 448–457. [Google Scholar] [CrossRef]
- Lv, K.; Xia, Z. Chinese consensus panel on the prevention and treatment of scars Chinese expert consensus on clinical prevention and treatment of scar. Burn. Trauma 2018, 6, 27. [Google Scholar] [CrossRef] [PubMed]
- Kasch, M.C. Clinical management of scar tissue. Occup. Ther. Health Care 1988, 4, 37–52. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, R.; Akita, S.; Akaishi, S.; Aramaki-Hattori, N.; Dohi, T.; Hayashi, T.; Kishi, K.; Kono, T.; Matsumura, H.; Muneuchi, G.; et al. Diagnosis and Treatment of Keloids and Hypertrophic Scars-Japan Scar Workshop Consensus Document 2018. Burn. Trauma 2019, 7, 39. [Google Scholar] [CrossRef]
- Candy, L.H.Y.; Cecilia, L.-T.W.P.; Ping, Z.Y. Effect of different pressure magnitudes on hypertrophic scar in a Chinese population. Burns 2010, 36, 1234–1241. [Google Scholar] [CrossRef]
- Lumenta, D.B.; Siepmann, E.; Kamolz, L.-P. Internet-based survey on current practice for evaluation, prevention, and treatment of scars, hypertrophic scars, and keloids. Wound Repair Regen. 2014, 22, 483–491. [Google Scholar] [CrossRef]
- Hurren, J.S. Rehabilitation of the burned patient: James Laing Memorial Essay for 1993. Burns 1995, 21, 116–126. [Google Scholar] [CrossRef]
- Van den Kerckhove, E.; Stappaerts, K.; Fieuws, S.; Laperre, J.; Massage, P.; Flour, M.; Boeckx, W. The assessment of erythema and thickness on burn related scars during pressure garment therapy as a preventive measure for hypertrophic scarring. Burns 2005, 31, 696–702. [Google Scholar] [CrossRef]
- Li, P.; Li-Tsang, C.W.P.; Deng, X.; Wang, X.; Wang, H.; Zhang, Y.; Tan, Z.; He, C. The recovery of post-burn hypertrophic scar in a monitored pressure therapy intervention programme and the timing of intervention. Burns 2018, 44, 1451–1467. [Google Scholar] [CrossRef]
- Ogawa, R.; Dohi, T.; Tosa, M.; Aoki, M.; Akaishi, S. The Latest Strategy for Keloid and Hypertrophic Scar Prevention and Treatment: The Nippon Medical School (NMS) Protocol. J. Nippon Med. Sch. 2021, 88, 2–9. [Google Scholar] [CrossRef]
- Dardas, A.; Bae, G.H.; Yule, A.; Wright, J.; Straughn, N.; Day, C.S. Acetic acid iontophoresis for recalcitrant scarring in post-operative hand patients. J. Hand Ther. 2014, 27, 44–48. [Google Scholar] [CrossRef] [PubMed]
- Omranifard, M.; Rasti, M. Comparing the effects of conventional method, pulse dye laser and erbium laser for the treatment of hypertrophic scars in Iranian patients. J. Res. Med. Sci. 2007, 12, 277–281. [Google Scholar]
- Taudorf, E.H.; Haedersdal, M. Early non-ablative fractional laser improves the appearance of punch biopsy scar—A clinical report. J. Eur. Acad. Dermatol. Venereol. JEADV 2016, 30, 550–552. [Google Scholar] [CrossRef]
- Elshazly, M.; Ahmed, A.A.; Sarhan, M.A. Effect of Combining Vacuum Massage and Shock Wave Therapy on the Post Burn Scar. Int. J. Curr. Res. Rev. 2021, 13, 68–72. [Google Scholar] [CrossRef]
- Mowafy, Z.M.E.; Elgohary, H.M.; Hassan, K.M.; Mohamed, K.E.S. Effect of Cryotherpy on Hypertrophic Scar. Eur. J. Mol. Clin. Med. 2021, 8, 1184–1191. [Google Scholar]
- Elrashid, N.A.A.; Sanad, D.A.; Mahmoud, N.F.; Hamada, H.A.; Abdelmoety, A.M.; Kenawy, A.M. Effect of orange polarized light on post burn pediatric scar: A single blind randomized clinical trial. J. Phys. Ther. Sci. 2018, 30, 1227–1231. [Google Scholar] [CrossRef][Green Version]
- Freitas, C.P.; Melo, C.; Alexandrino, A.M.; Noites, A. Efficacy of low-level laser therapy on scar tissue. J. Cosmet. Laser Ther. 2013, 15, 171–176. [Google Scholar] [CrossRef]
- Manuskiatti, W.; Fitzpatrick, R.E.; Goldman, M.P. Energy density and numbers of treatment affect response of keloidal and hypertrophic sternotomy scars to the 585-nm flashlamp-pumped pulsed-dye laser. J. Am. Acad. Dermatol. 2001, 45, 557–565. [Google Scholar] [CrossRef] [PubMed]
- Alsharnoubi, J.; Shoukry, K.E.-S.; Fawzy, M.W.; Mohamed, O. Evaluation of scars in children after treatment with low-level laser. Lasers Med. Sci. 2018, 33, 1991–1995. [Google Scholar] [CrossRef] [PubMed]
- Ward, R.S.; Hayes-Lundy, C.; Reddy, R.; Brockway, C.; Mills, P.; Saffle, J.R. Evaluation of topical therapeutic ultrasound to improve response to physical therapy and lessen scar contracture after burn injury. J. Burn Care Rehabil. 1994, 15, 74–79. [Google Scholar] [CrossRef] [PubMed]
- Saggini, R.; Saggini, A.; Spagnoli, A.M.; Dodaj, I.; Cigna, E.; Maruccia, M.; Soda, G.; Bellomo, R.G.; Scuderi, N. Extracorporeal Shock Wave Therapy: An Emerging Treatment Modality for Retracting Scars of the Hands. Ultrasound Med. Biol. 2016, 42, 185–195. [Google Scholar] [CrossRef]
- Leszczynski, R.; da Silva, C.A.; Pinto, A.C.P.N.; Kuczynski, U.; da Silva, E.M. Laser therapy for treating hypertrophic and keloid scars. Cochrane Database Syst. Rev. 2022, 9, CD011642. [Google Scholar] [CrossRef]
- Seago, M.; Shumaker, P.R.; Spring, L.K.; Alam, M.; Al-Niaimi, F.; Rox Anderson, R.; Artzi, O.; Bayat, A.; Cassuto, D.; Chan, H.H.; et al. Laser Treatment of Traumatic Scars and Contractures: 2020 International Consensus Recommendations. Lasers Surg. Med. 2020, 52, 96–116. [Google Scholar] [CrossRef]
- Ebid, A.A.; Ibrahim, A.R.; Omar, M.T.; El Baky, A.M.A. Long-term effects of pulsed high-intensity laser therapy in the treatment of post-burn pruritus: A double-blind, placebo-controlled, randomized study. Lasers Med. Sci. 2017, 32, 693–701. [Google Scholar] [CrossRef]
- Yang, Y.; Kang, J.; Jiang, T.; Schmitz, C.; Weng, C.; Zhang, L. Safety and efficacy of treating post-burn pathological scars with extracorporeal shock wave therapy: A meta-analysis of randomised controlled trials. Wound Repair Regen. 2022, 30, 595–607. [Google Scholar] [CrossRef] [PubMed]
- Nicoletti, G.; Perugini, P.; Bellino, S.; Capra, P.; Malovini, A.; Jaber, O.; Tresoldi, M.; Faga, A. Scar Remodeling with the Association of Monopolar Capacitive Radiofrequency, Electric Stimulation, and Negative Pressure. Photomed. Laser Surg. 2017, 35, 246–258. [Google Scholar] [CrossRef]
- Deng, H.; Tan, T.; Luo, G.; Tan, J.; Li-Tsang, C.W.P. Vascularity and Thickness Changes in Immature Hypertrophic Scars Treated With a Pulsed Dye Laser. Lasers Surg. Med. 2020, 53, 914–921. [Google Scholar] [CrossRef]
- Edwards, J. Hypertrophic scar management. Br. J. Nurs. 2022, 31, S24–S31. [Google Scholar] [CrossRef]
- Karagoz, H.; Yuksel, F.; Ulkur, E.; Evinc, R. Comparison of efficacy of silicone gel, silicone gel sheeting, and topical onion extract including heparin and allantoin for the treatment of postburn hypertrophic scars. Burns 2009, 35, 1097–1103. [Google Scholar] [CrossRef]
- Sadat-Ali, M.; AlMousa, S.A.; AlTabash, K.W.; Abotaleb, M.M.; Al Anii, F.M.; AlOmran, A.S. Phyto-Extracts and Silicone Gel (JUMI) in Reduction of Surgical Scar Post-joint Arthroplasty. A Randomized Control Trial. Open Med. Chem. J. 2023, 17. [Google Scholar] [CrossRef]
- O’Brien, L.; Jones, D.J. Silicone gel sheeting for preventing and treating hypertrophic and keloid scars. Cochrane Database Syst. Rev. 2013, 2013, CD003826. [Google Scholar] [CrossRef]
- Jiang, Q.; Chen, J.; Tian, F.; Liu, Z. Silicone gel sheeting for treating hypertrophic scars. Cochrane Database Syst. Rev. 2021, 9, CD013357. [Google Scholar] [CrossRef]
- Eishi, K.; Bae, S.-J.; Ogawa, F.; Hamasaki, Y.; Shimizu, K.; Katayama, I. Silicone gel sheets relieve pain and pruritus with clinical improvement of keloid: Possible target of mast cells. J. Dermatol. Treat. 2003, 14, 248–252. [Google Scholar] [CrossRef] [PubMed]
- Van den Kerckhove, E.; Stappaerts, K.; Boeckx, W.; Van den Hof, B.; Monstrey, S.; Van der Kelen, A.; De Cubber, J. Silicones in the rehabilitation of burns: A review and overview. Burns 2001, 27, 205–214. [Google Scholar] [CrossRef] [PubMed]
- Zhang, E.W.; Li-Tsang, C.W.P.; Li, T.M.H.; Huang, L.; Cheung, K.-K. Smart Scar Care Pad: An Innovated Silicone-Based Insert That Improved Severe Hypertrophic Scar by Integrating Optimal Pressure and Occlusion Effects. Adv. Wound Care 2020, 9, 564–575. [Google Scholar] [CrossRef]
- Kong, C.-G.; Kim, G.-H.; Kim, D.-W.; In, Y. The effect of topical scar treatment on postoperative scar pain and pruritus after total knee arthroplasty. Arch. Orthop. Trauma Surg. 2014, 134, 555–559. [Google Scholar] [CrossRef]
- Westra, I.; Pham, H.; Niessen, F.B. Topical Silicone Sheet Application in the Treatment of Hypertrophic Scars and Keloids. J. Clin. Aesthetic Dermatol. 2016, 9, 28–35. [Google Scholar]
- Tawfik, A.M.; Othman, E.M.; Kenawy, A.M.; AboElnour, N.H. Effectiveness of kinesio taping versus deep friction massage on post burn hypertrophic scar. Curr. Sci. Int. 2018, 7, 775–784. [Google Scholar]
- Roh, Y.S.; Seo, C.H.; Jang, K.U. Effects of a skin rehabilitation nursing program on skin status, depression, and burn-specific health in burn survivors. Rehabil. Nurs. J. 2010, 35, 65–69. [Google Scholar] [CrossRef]
- Roh, Y.S.; Cho, H.; Oh, J.O.; Yoon, C.J. Effects of skin rehabilitation massage therapy on pruritus, skin status, and depression in burn survivors. J. Korean Acad. Nurs. 2007, 37, 221–226. [Google Scholar] [CrossRef]
- Poddighe, D.; Ferriero, G.; Corna, S.; Bravini, E.; Sartorio, F.; Vercelli, S. Effects of soft tissue mobilisation on subacute adherent linear scars: A single-group intervention study. J. Wound Care 2024, 33, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Scott, H.C.; Robinson, L.S.; Brown, T. Scar massage as an intervention for post-surgical scars: A practice survey of Australian hand therapists. Hand Ther. 2024, 29, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Donnelly, C.J.; Wilton, J. The Effect of Massage to Scars on Active Range of Motion and Skin Mobility. Br. J. Hand Ther. 2002, 7, 5–11. [Google Scholar] [CrossRef]
- Asadullah, M.; Khan, A.; Shakil-ur-Rehman, S.; Danish, K.F.; Sibtain, F. Role of Early Range of Motion Exercises in Reduction of Scar Formation and Prevention of Contracture in Sub-acute Stage of Burn Patients. J. Islam. Int. Med. Coll. JIIMC 2013, 8, 10–14. [Google Scholar]
- Abdalla, A.M.; Mohamed, H.S.; I Saafan, K.; Elnour, N.H.A. Comparative study between effects of kinesio taping and Contractubex phonophoresis on post-burn hypertrophic scar characteristics. Egypt. J. Hosp. Med. 2023, 91, 3846–3849. [Google Scholar] [CrossRef]
- Karwacińska, J.; Kiebzak, W.; Stepanek-Finda, B.; Kowalski, I.M.; Protasiewicz-Fałdowska, H.; Trybulski, R.; Starczyńska, M. Effectiveness of Kinesio Taping on hypertrophic scars, keloids and scar contractures. Pol. Ann. Med. 2012, 19, 50–57. [Google Scholar] [CrossRef]
- Cho, Y.S.; Joo, S.Y.; Seo, C.H. Effect of robot-assisted gait training on the biomechanical properties of burn scars: A single-blind, randomized controlled trial. Burn. Trauma 2022, 10, tkac026. [Google Scholar] [CrossRef]
- Edgar, D.; Brereton, M. Rehabilitation after burn injury. BMJ 2004, 329, 343–345. [Google Scholar] [CrossRef] [PubMed]
- Helm, P.A.; Head, M.D.; Pullium, G.; O’Brien, M.; Cromes, G.F. Burn rehabilitation-a team approach. Surg. Clin. N. Am. 1978, 58, 1263–1278. [Google Scholar] [CrossRef]
- Johnson, C.L. Physical therapists as scar modifiers. Phys. Ther. 1984, 64, 1381–1387. [Google Scholar] [CrossRef] [PubMed]
- Williams, T.; Berenz, T. Postburn Upper Extremity Occupational Therapy. Hand Clin. 2017, 33, 293–304. [Google Scholar] [CrossRef]
- Procter, F. Rehabilitation of the burn patient. Indian J. Plast. Surg. Off. Publ. Assoc. Plast. Surg. India 2010, 43, S101–S113. [Google Scholar] [CrossRef]
- Jones, L. Scar Management in Hand Therapy–Is our Practice Evidence Based? Br. J. Hand Ther. 2005, 10, 40–46. [Google Scholar] [CrossRef]
- Ripper, S.; Renneberg, B.; Landmann, C.; Weigel, G.; Germann, G. Adherence to pressure garment therapy in adult burn patients. Burns 2009, 35, 657–664. [Google Scholar] [CrossRef]
- Helm, P.A.; Kevorkian, C.G.; Lushbaugh, M.; Pullium, G.; Head, M.D.; Cromes, G.F. Burn injury: Rehabilitation management in 1982. Arch. Phys. Med. Rehabil. 1982, 63, 6–16. [Google Scholar] [CrossRef]
- Pessina, M.A.; Ellis, S.M. Burn management. Rehabilitation. Nurs. Clin. N. Am. 1997, 32, 365–374. [Google Scholar] [CrossRef]
- Chapman, T.T. Burn scar and contracture management. J. Trauma 2007, 62, S8. [Google Scholar] [CrossRef]
- Teot, L.; Otman, S.; Brancati, A.; Mittermayr, R. Burn scar treatment. In Handbook of Burns: Reconstruction and Rehabilitation; Kamolz, L.-P., Jeschke, M.G., Horch, R.E., Küntscher, M., Brychta, P., Eds.; Springer: Berlin/Heidelberg, Germany, 2012; pp. 55–67. [Google Scholar]
- Yohannan, S.K.; Ronda-Velez, Y.; Henriquez, D.A.; Hunter, H.; Tufaro, P.A.; Marren, M.; Sher, M.; Gorga, D.I.; Yurt, R.W. Burn survivors’ perceptions of rehabilitation. Burns 2012, 38, 1151–1156. [Google Scholar] [CrossRef] [PubMed]
- Smith, F.R. Causes of and treatment options for abnormal scar tissue. J. Wound Care 2005, 14, 49–52. [Google Scholar] [CrossRef] [PubMed]
- Williams, F.; Knapp, D.; Wallen, M. Comparison of the characteristics and features of pressure garments used in the management of burn scars. Burns 1998, 24, 329–335. [Google Scholar] [CrossRef]
- Van den Kerckhove, E.; Anthonissen, M. Compression Therapy and Conservative Strategies in Scar Management After Burn Injury. In Textbook on Scar Management: State of the Art Management and Emerging Technologies; Téot, L., Mustoe, T.A., Middelkoop, E., Gauglitz, G.G., Eds.; Springer: Cham, Germany, 2020. [Google Scholar]
- Liu, Y.; Xiong, X.; Cao, N.; Zhao, Y. Diagnosis and Treatment of Keloid: Method Summary and Effect Evaluation. Clin. Cosmet. Investig. Dermatol. 2023, 16, 3775–3783. [Google Scholar] [CrossRef]
- Deitch, E.A.; Wheelahan, T.M.; Rose, M.P.; Clothier, J.; Cotter, J. Hypertrophic burn scars: Analysis of variables. J. Trauma 1983, 23, 895–898. [Google Scholar] [CrossRef]
- Bharadia, S.K.; Burnett, L.; Gabriel, V. Hypertrophic Scar. Phys. Med. Rehabil. Clin. N. Am. 2023, 34, 783–798. [Google Scholar] [CrossRef] [PubMed]
- Alster, T.S.; Tanzi, E.L. Hypertrophic scars and keloids: Etiology and management. Am. J. Clin. Dermatol. 2003, 4, 235–243. [Google Scholar] [CrossRef]
- Gauglitz, G.G. Long-Term Pathophysiology and Consequences of a Burn Including Scarring, HTS, Keloids and Scar Treatment, Rehabilitation, Exercise. In Burn Care and Treatment: A Practical Guide; Jeschke, M.G., Kamolz, L.-P., Shahrokhi, S., Eds.; Springer: Vienna, Austria, 2013; pp. 157–165. [Google Scholar] [CrossRef]
- Atiyeh, B.S. Nonsurgical management of hypertrophic scars: Evidence-based therapies, standard practices, and emerging methods. Aesthetic Plast. Surg. 2007, 31, 468–492; discussion 493–494. [Google Scholar] [CrossRef] [PubMed]
- Wittgruber, G.; Parvizi, D.; Koch, H. Nonsurgical therapy for postoperative hypertrophic scars. Eur. Surg. 2012, 44, 74–78. [Google Scholar] [CrossRef]
- Son, D.; Harijan, A. Overview of surgical scar prevention and management. J. Korean Med. Sci. 2014, 29, 751–757. [Google Scholar] [CrossRef]
- Jensen, L.L.; Parshley, P.F. Postburn Scar Contractures: Histology and Effects of Pressure Treatment. J. Burn Care Rehabil. 1984, 5, 119–123. [Google Scholar] [CrossRef]
- Roques, C. Pressure therapy to treat burn scars. Wound Repair Regen 2002, 10, 122–125. [Google Scholar] [CrossRef]
- Serghiou, M.; Cowan, A.; Whitehead, C. Rehabilitation after a burn injury. Clin. Plast. Surg. 2009, 36, 675–686. [Google Scholar] [CrossRef]
- Young, A.W.; Dewey, W.S.; King, B.T. Rehabilitation of Burn Injuries: An Update. Phys. Med. Rehabil. Clin. N. Am. 2019, 30, 111–132. [Google Scholar] [CrossRef]
- Masanovic, M.G.; Téot, L. Scar Contractures. In Textbook on Scar Management: State of the Art Management and Emerging Technologies; Téot, L., Mustoe, T.A., Middelkoop, E., Gauglitz, G.G., Eds.; Springer: Cham, Germany, 2020. [Google Scholar]
- Shirakami, E.; Yamakawa, S.; Hayashida, K. Strategies to prevent hypertrophic scar formation: A review of therapeutic interventions based on molecular evidence. Burn. Trauma 2020, 8, tkz003. [Google Scholar] [CrossRef]
- Rayner, K. The use of pressure therapy to treat hypertrophic scarring. J. Wound Care 2000, 9, 151–153. [Google Scholar] [CrossRef]
- Rabello, F.B.; Souza, C.D.; Farina Júnior, J.A. Update on hypertrophic scar treatment. Clinics 2014, 69, 565–573. [Google Scholar] [CrossRef]
- Aguilera-Sáez, J.; Muñoz, P.; Serracanta, J.; Monte, A.; Barret, J.P. Extracorporeal shock wave therapy role in the treatment of burn patients. A systematic literature review. Burns 2020, 46, 1525–1532. [Google Scholar] [CrossRef]
- Chowdhury, B.; Kassir, M.; Salas-Alanis, J.; Nistico, S.; Galadari, H.; Fritz, K.; Salavastru, C.; Blicharz, L.; Goldust, M. Laser in surgical scar clearance: An update review. J. Cosmet. Dermatol. 2021, 20, 3808–3811. [Google Scholar] [CrossRef]
- Sorkin, M.; Cholok, D.; Levi, B. Scar Management of the Burned Hand. Hand Clin. 2017, 33, 305–315. [Google Scholar] [CrossRef]
- Wright, P.C. Fundamentals of acute burn care and physical therapy management. Phys. Ther. 1984, 64, 1217–1231. [Google Scholar] [CrossRef]
- Edger-Lacoursière, Z.; Deziel, E.; Nedelec, B. Rehabilitation interventions after hand burn injury in adults: A systematic review. Burns 2023, 49, 516–553. [Google Scholar] [CrossRef]
- Dewey, W.S.; Richard, R.L.; Parry, I.S. Positioning, splinting, and contracture management. Phys. Med. Rehabil. Clin. N. Am. 2011, 22, 229–247. [Google Scholar] [CrossRef] [PubMed]
- Harden, N.G.; Luster, S.H. Rehabilitation considerations in the care of the acute burn patient. Crit. Care Nurs. Clin. N. Am. 1991, 3, 245–253. [Google Scholar] [CrossRef]
- Asghari Amrei, S.; Ayatollahi, H.; Salehi, S.H. A Smartphone Application for Burn Self-care. J. Burn Care Res. 2020, 41, 384–389. [Google Scholar] [CrossRef]
- Toscano, D.; Arena, D.; Sarzi, L.; Stella, M.; Depetris, N.; Massazza, G. Scar taping. Burns Open 2021, 5, 218–221. [Google Scholar] [CrossRef]
- Vercelli, S.; Ferriero, G.; Sartorio, F.; Cisari, C.; Bravini, E. Clinimetric properties and clinical utility in rehabilitation of postsurgical scar rating scales: A systematic review. Int. J. Rehabil. Res. 2015, 38, 279–286. [Google Scholar] [CrossRef] [PubMed]
- Legemate, C.M.; Middelkoop, E.; Carrière, M.E.; van Zuijlen, P.P.M.; van Baar, M.E.; van der Vlies, C.H.; Hycon Study Group. The minimal important change (MIC) and minimal clinically important difference (MCID) of the patient and observer scar assessment scale (POSAS) 2.0. Burns 2024, 50, 2070–2076. [Google Scholar] [CrossRef]
- Deng, H.; Li-Tsang, C.W.P. Measurement of vascularity in the scar: A systematic review. Burns 2019, 45, 1253–1265. [Google Scholar] [CrossRef] [PubMed]
- Schoch, D.; Sommer, R.; Augustin, M.; Ständer, S.; Blome, C. Patient-Reported Outcome Measures in Pruritus: A Systematic Review of Measurement Properties. J. Investig. Dermatol. 2017, 137, 2069–2077. [Google Scholar] [CrossRef]
- Jang, Y.H.; Kim, S.M.; Eun, D.H.; Park, K.D.; Park, G.-H.; Kim, B.-S.; Li, K.; Park, C.O.; Kim, H.O.; Kim, H.S.; et al. Validity and reliability of itch assessment scales for chronic pruritus in adults: A prospective multicenter study. J. Am. Acad. Dermatol. 2020, 82, 80–86. [Google Scholar] [CrossRef]
- Lee, K.C.; Bamford, A.; Gardiner, F.; Agovino, A.; Ter Horst, B.; Bishop, J.; Sitch, A.; Grover, L.; Logan, A.; Moiemen, N.S. Investigating the intra- and inter-rater reliability of a panel of subjective and objective burn scar measurement tools. Burns 2019, 45, 1311–1324. [Google Scholar] [CrossRef]
- Bernabe, R.M.; Madrigal, P.; Choe, D.; Pham, C.; Yenikomshian, H.A.; Gillenwater, J. Assessing Scar Outcomes Using Objective Scar Measurement Tools: An Adjunct to Validated Scar Evaluation Scales. Plast. Reconstr. Surg. 2024, 154, 885e–890e. [Google Scholar] [CrossRef]
- Vrijman, C.; van Drooge, A.M.; Limpens, J.; Bos, J.D.; van der Veen, J.P.W.; Spuls, P.I.; Wolkerstorfer, A. Laser and intense pulsed light therapy for the treatment of hypertrophic scars: A systematic review. Br. J. Dermatol. 2011, 165, 934–942. [Google Scholar] [CrossRef]
- Boutli-Kasapidou, F.; Tsakiri, A.; Anagnostou, E.; Mourellou, O. Hypertrophic and keloidal scars: An approach to polytherapy. Int. J. Dermatol. 2005, 44, 324–327. [Google Scholar] [CrossRef] [PubMed]
- Obaidi, N.; Keenan, C.; Chan, R.K. Burn Scar Management and Reconstructive Surgery. Surg. Clin. N. Am. 2023, 103, 515–527. [Google Scholar] [CrossRef]
- Scott, H.C.; Stockdale, C.; Robinson, A.; Robinson, L.S.; Brown, T. Is massage an effective intervention in the management of post-operative scarring? A scoping review. J. Hand Ther. 2022, 35, 186–199. [Google Scholar] [CrossRef] [PubMed]
| Population | All types of scars on humans with no age restrictions were included except for those that interfere with wound healing. |
| Concept | All types of conservative non-invasive interventions including education and self-management strategies (e.g., scar massage, soft tissue mobilization, splinting, etc.). |
| Context | Studies were included regardless of geographical location, social or cultural context, or level of care. |
| Population (P) | “Cicatrix” [Mesh], “Cicatrix, Hypertrophic” [Mesh], “Tissue Adhesions” [Mesh], “Keloid” [Mesh], “Scar *”, “Scarring”, “Hypertrophic Scar *”, “Burn Scar”, “Contracture Scar”. |
| Concept (C) | “Rehabilitation” [Mesh], “Exercise Therapy” [Mesh], “Physical Therapy Modalities” [Mesh], “Musculoskeletal Manipulations” [Mesh], “Therapy, Soft Tissue” [Mesh], “Exercise” [Mesh], “Self Care” [Mesh], “Patient education as topic [Mesh], “Muscle Stretching Exercises” [Mesh], “Conservative Treatment [Mesh], “Exercise”, “Habilitation”, “Rehabilitation”, “Physiotherapy”, “Physical Therapy”, “Manual Therapy”, “Patient Education”, “Mobilization”, “Resistance Training”, “Strength Training”, “Stretching”, “Conservative Treatment”, “Non-invasive Treatment”, “Soft Tissue Therapy”. |
| Context (C) | / |
| Database | Query Strings, Keywords and Boolean Operators | Results |
|---|---|---|
| Medline (via PubMed) | (((((((((“Scar”) OR (“Scarring”)) OR (“Hypertrophic Scars”)) OR (“Burn Scar”)) OR (“Contracture Scar”)) OR (“Cicatrix” [MeSH Terms])) OR (“Cicatrix, Hypertrophic” [MeSH Terms])) OR (“Keloid” [MeSH Terms])) OR (“Tissue Adhesions” [MeSH Terms])) AND (((((((((((((“Soft Tissue Therapy”) OR (“Rehabilitation”)) OR (“Habilitation”)) OR (“Physiotherapy”)) OR (“Physical Therapy”)) OR (“Exercise”)) OR (“Stretching”)) OR (“Resistance Training”)) OR (“Strength Training”)) OR (“Manual Therapy”)) OR (“Mobilization”)) OR (“Patient Education”)) OR (“Conservative Treatment”)) | 3223 |
| Variable | Number of Studies (%) |
|---|---|
| Year of Publication | |
| 1970–1979 | 1 (1.1%) |
| 1980–1989 | 7 (7.5%) |
| 1990–1999 | 5 (54%) |
| 2000–2009 | 19 (20.4%) |
| 2010–2019 | 31 (33.3%) |
| 2020–2024 | 29 (30.1%) |
| Study Design | |
| Book Chapter | 2 (2.1%) |
| Clinical Trials | 13 (13.9%) |
| Commentary | 1 (1%) |
| Consensus | 3 (3.2%) |
| Narrative Review | 41 (44%) |
| Observational Study | 3 (3.2%) |
| Prospective Study | 2 (2.1%) |
| RCT | 18 (19.3%) |
| Retrospective Study | 1 (1%) |
| Survey | 3 (3.2%) |
| Systematic Review | 5, 2 meta-analyses (5.3%) |
| Scar Type | |
| Burn Scars | 47 (50.5%) |
| Contracture | 7 (7.5%) |
| Hypertrophic Scars | 32 (34.4%) |
| Keloid | 20 (21.5%) |
| Not Reported | 7 (7.5%) |
| Population | |
| Adults | 27 (29%) |
| Children | 6 (6.5%) |
| Adults and Children | 25 (26.9%) |
| Not Reported | 34 (37.6%) |
| Scar Localization | |
| Face | 5 (5.3%) |
| Hand | 16 (17.2%) |
| Lower Limb | 20 (21.5%) |
| Neck | 8 (8.6%) |
| Trunk | 13 (13.9%) |
| Upper Limb | 27 (29%) |
| Various Body Areas | 53 (56.9%) |
| Interventions | |
| Pressure Therapy | 41 (44.1%) |
| Physical Therapy Modalities | 37 (39.8%) |
| Silicone-based Products | 29 (31.2%) |
| Massage | 20 (21.5%) |
| Splinting | 17 (18.3%) |
| Therapeutic Education | 11 (11.8%) |
| Range of Motion and Stretching Exercises | 10 (10.7%) |
| Adhesive Tapes | 7 (7.5%) |
| RAGT | 1 (1%) |
| Subjective Tools | Number of Studies | Objective Tools | Number of Studies |
|---|---|---|---|
| Vancouver Scar Scale | 23 (24.7%) | Ultrasonography | 13 (13.9%) |
| Visuo Analogic Scale | 11 (11.8%) | Doppler Laser or Ultrasound | 4 (4.3%) |
| Patient and Observer Scar Assessment Scale | 9 (9.7%) | Spectrocolorimeter® | 3 (3.2%) |
| Modified Vancouver Scar Scale | 5 (5.4%) | Colormeter® | 2 (2.1%) |
| Dermatology Life Quality Index | 2 (2.1%) | DermaLab Elasticity Probe | 2 (2.1%) |
| Smith Scale | 2 (2.1%) | Cutometer® | 2 (2.1%) |
| Hamilton Scale | 2 (2.1%) | Mexameter® | 2 (2.1%) |
| Manchester Scar Scale | 2 (2.1%) | Chromameter® | 2 (2.1%) |
| Seattle Scale | 1 (1%) | Tonometer® | 1 (1%) |
| Vancouver Burn Scale | 1 (1%) | Pressure Pain Treshold | 1 (1%) |
| Modified Itching Severity Scale | 1 (1%) | Tewameter® | 1 (1%) |
| Itch Man Scale | 1 (1%) | 3D Scanner | 1 (1%) |
| Numeric Rating Scale | 1 (1%) |
| Modalities | Parameters |
|---|---|
| PDL | 585–595 nm, 3 to 12 J/cm2, 0.45–10 ms, 7–10 mm spot for 2–6 sessions |
| NAFL (one study) | 1540 nm, 15 ms pulse duration, 70 mJ/cm2 |
| LLLT | 632.8 nm, 119 mW/cm2, energy density was 16 J/cm2 for 25 min in 24 sessions. |
| IPL | 515–1200 nm, 40 J/cm2 |
| HILT: | 1064 nm, 3 kW, 510–1780 mJ/cm2, 10–40 Hz, 120–150μs, duty cycle of about 0.1% for 18 sessions over 3 weeks |
| Ultrasound (one study) | 1 MHz, 1 w/cm2, 10 min. Every day for 2 weeks |
| ESWT | 100 to 3000 pulses, 0.015 to 0.3 mJ/mm2, 1 to 6 Hz, 1 to 12 sessions |
| Ionthoforesis (one study) | 2.5–4 mA, 40–50 mA/min., 3 to 12 sessions |
| Cryotherapy (one study) | 10 min, −14 degrees, 2 sessions per week, for 10 weeks |
| Light therapy (one study) | 480–3.400 nm, degree of polarization >95% (590–1550 nm), 40 mW/cm2, light energy per minute 2.4 J/cm2. 30 min, three times a week for 4 weeks |
| ES + NP | 5 Hz square wave with adjustable output up to 0.36 mA at 500 Ohm. Negative pressure up to 35 atm. |
| Techniques |
|---|
| Cutaneous mobilizations |
| Pulpar massage |
| Push-pull |
| J Stroke |
| Modified version of the “Indian Burn” |
| Skin Rehabilitation Massage Therapy |
| Deep friction massage |
| GAF techniques |
| Massage dermo-épidermique |
| Pressing movements |
| Circular, transverse, and vertical strokes |
| Pinching and lifting |
| Interventions | Suggested Parameters |
|---|---|
| Pressure Therapy | Early application at 24 mmHg for 23 h a day up to 12 months or scar maturation. |
| ESWT for burn scars | 1–2 sessions per week for 4–8 weeks, at least 100 ESWs per cm2 or between 2000 and 3000 ESWs in total per session, highest EFD the patient can tolerate. |
| Silicone-based Products | SGS: Early application, Worn between 12 and 24 h a day and maintained at least for 2 months Silicone Gel: early application, two times per day at least for 2 months |
| Massage | 10–15 min per session repeated for 1–3 times during the day. |
| Splinting | Application should vary considering localization, depth, elasticity of the scar and patient’s tolerance and ability to move the affected area |
| Education | Inform about injuries, course of treatment and self-management. |
| Stretching and Mobilizations | Stretching based on skin blanching and patient’s tolerance. Active, passive, resisted ROM exercise and Proprioceptive Neuromuscular Facilitations. |
| Adhesive Tapes | 25–100% tension, worn for 7 days. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Serio, S.; Congiu, M.; Minnucci, S.; Scalise, V.; Mourad, F. Current Physical Therapy for Skin Scar Management: A Scoping Review. J. Clin. Med. 2025, 14, 5920. https://doi.org/10.3390/jcm14175920
Di Serio S, Congiu M, Minnucci S, Scalise V, Mourad F. Current Physical Therapy for Skin Scar Management: A Scoping Review. Journal of Clinical Medicine. 2025; 14(17):5920. https://doi.org/10.3390/jcm14175920
Chicago/Turabian StyleDi Serio, Sara, Matteo Congiu, Silvia Minnucci, Valentina Scalise, and Firas Mourad. 2025. "Current Physical Therapy for Skin Scar Management: A Scoping Review" Journal of Clinical Medicine 14, no. 17: 5920. https://doi.org/10.3390/jcm14175920
APA StyleDi Serio, S., Congiu, M., Minnucci, S., Scalise, V., & Mourad, F. (2025). Current Physical Therapy for Skin Scar Management: A Scoping Review. Journal of Clinical Medicine, 14(17), 5920. https://doi.org/10.3390/jcm14175920







