Clinical Performance of Self-Adhesive vs. Conventional Flowable Resin Composite Restorations in Posterior Teeth: A Systematic Review and Meta-Analysis of Randomized Trials
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.3. Information Sources and Search Strategy
2.4. Selection Process
2.5. Data Collection Process
2.6. Study Risk of Bias Assessment
2.7. Effect Measures and Synthesis Methods
2.8. Certainty Assessment
3. Results
3.1. Study Selection
3.2. Study Characteristics
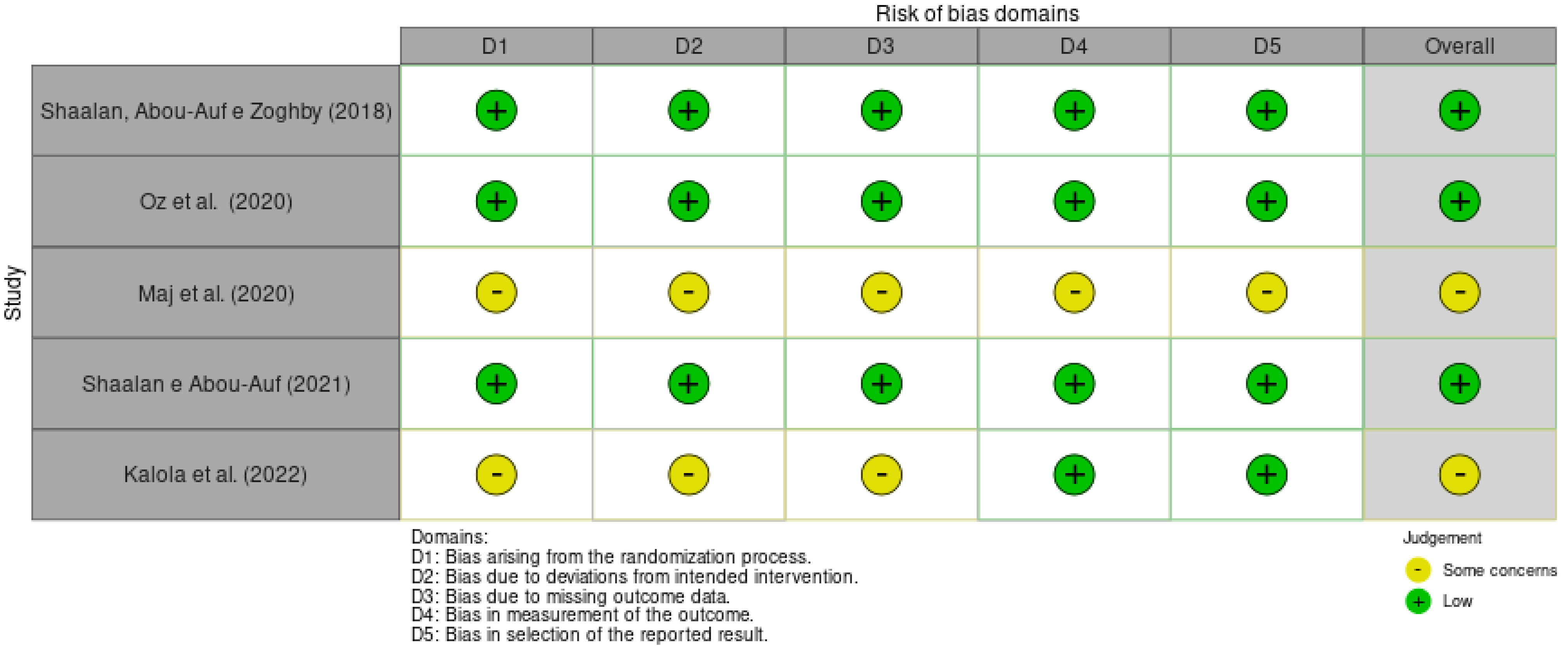
3.3. Risk of Bias in Studies
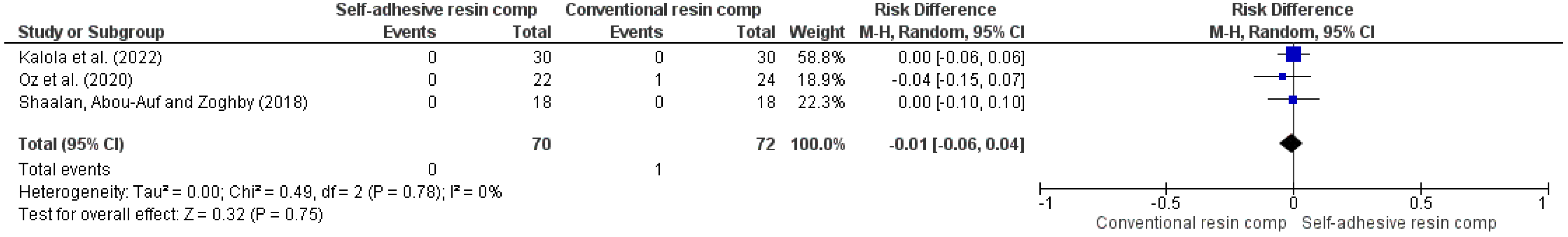
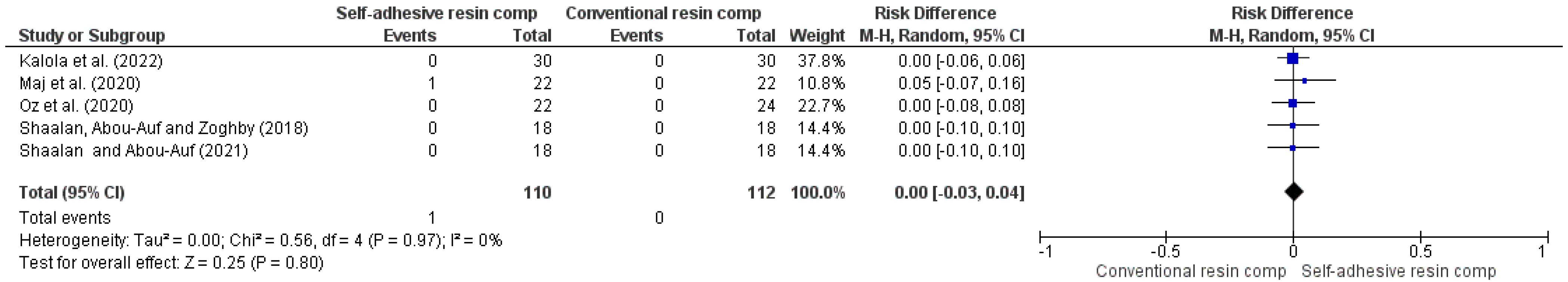
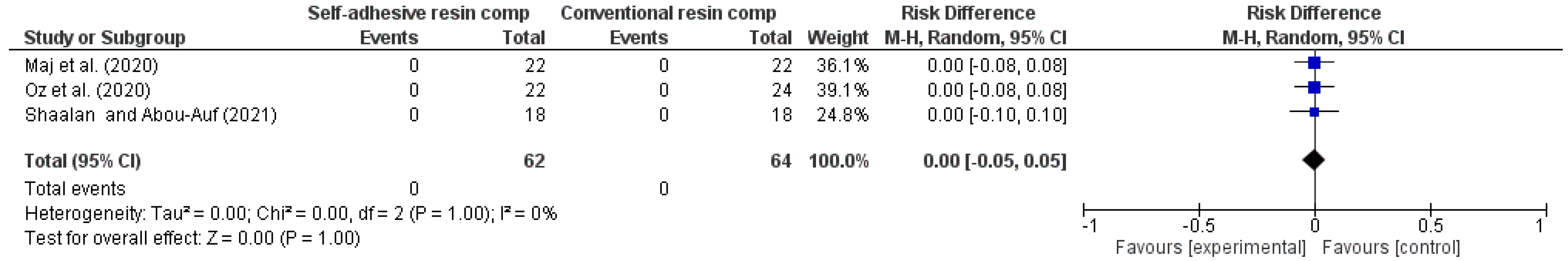
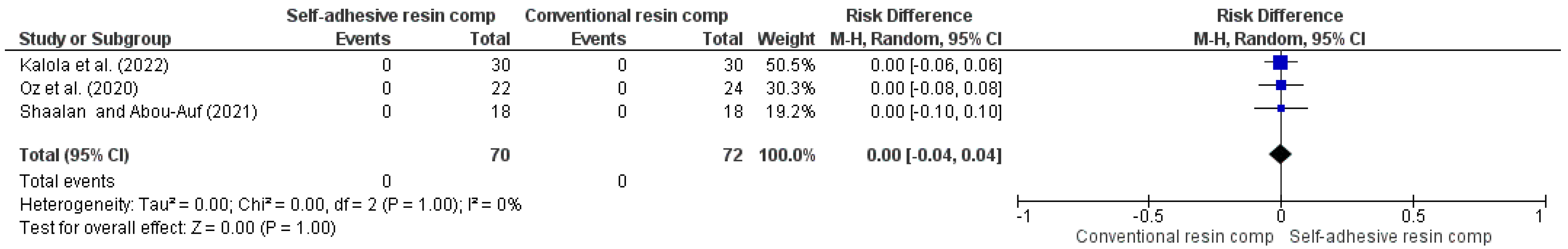
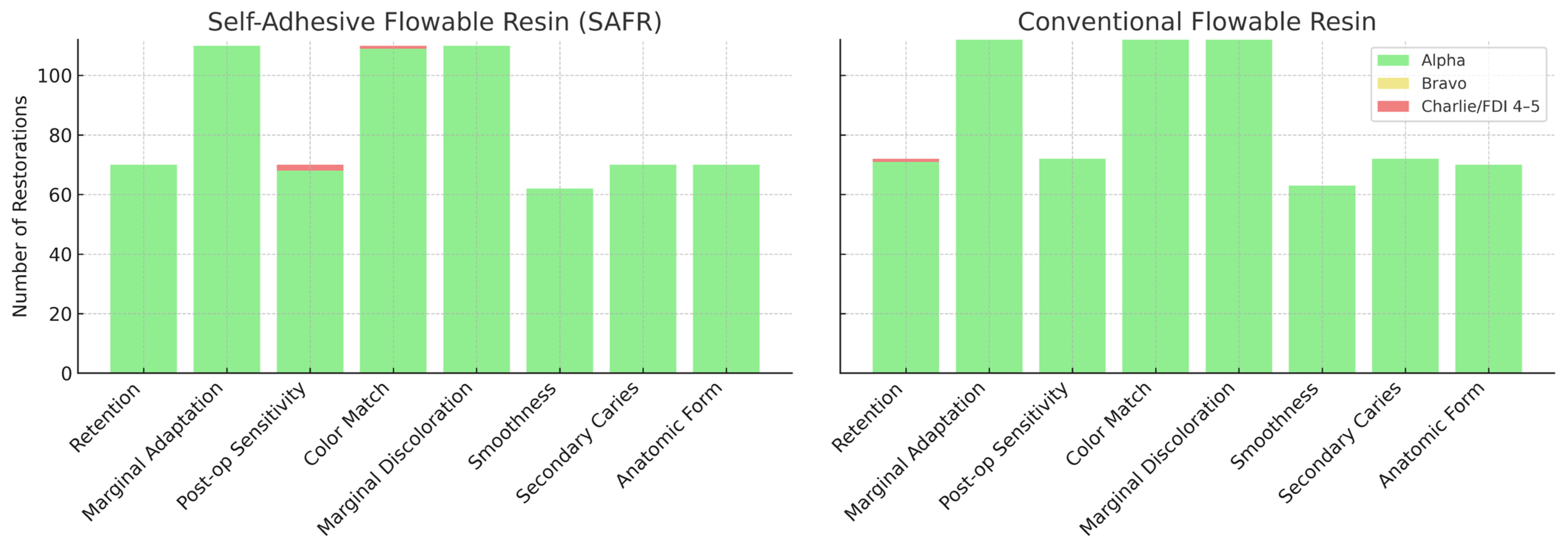
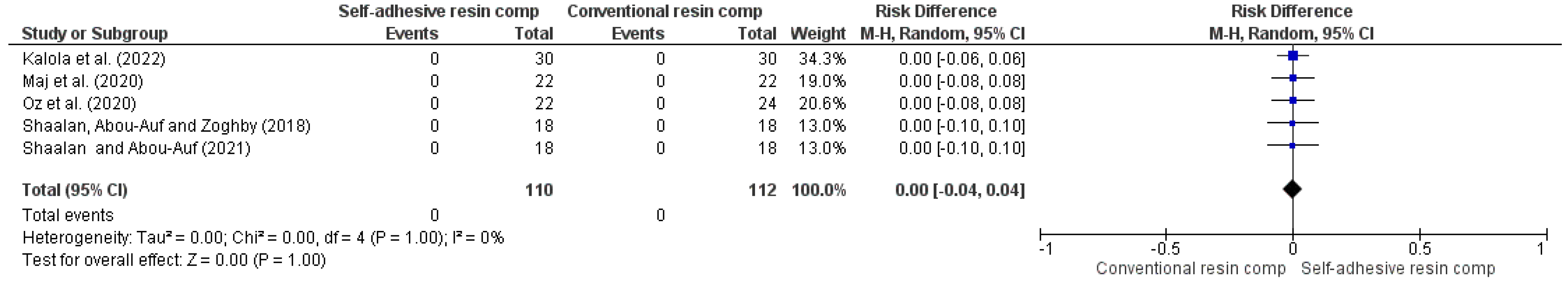
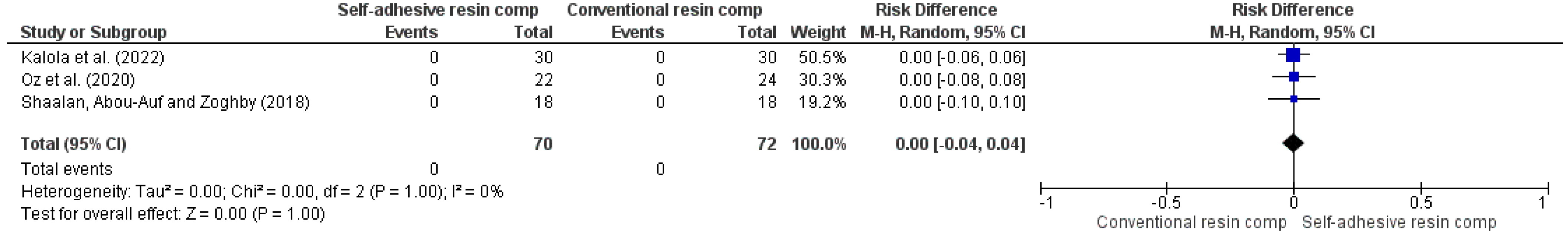
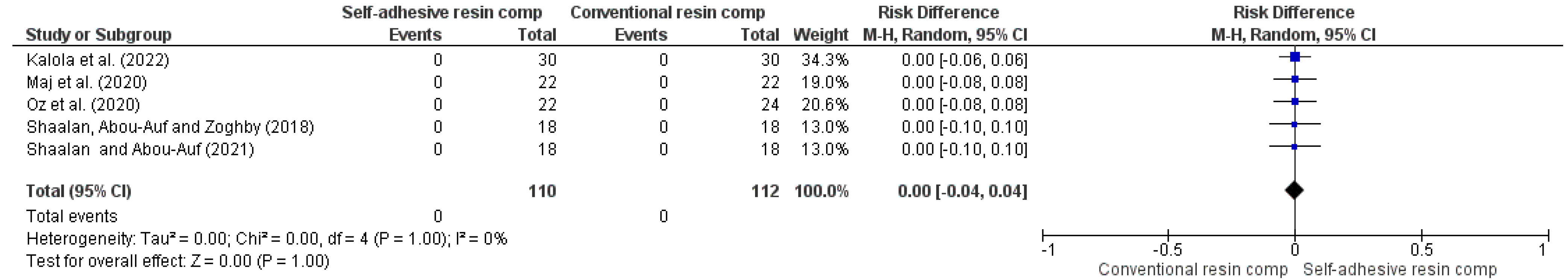
3.4. Results of Syntheses
3.5. Certainty of Evidence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Miletic, V. Development of Dental Composites. In Dental Composite Materials for Direct Restorations; Springer: Cham, Switzerland, 2018; Volume 1, pp. 1–15. [Google Scholar]
- Neto, J.M.A.S.; da Silva, L.E.E.; Souza, C.C.B.; de Castro Pereira, N.E.; de Mendonça, I.C.G. Utilização de resinas compostas em dentes anteriores. Rev. Eletrônica Acervo Saúde 2021, 13, 1–7. [Google Scholar] [CrossRef]
- David, C.; Cardoso de Cardoso, G.; Isolan, C.P.; Piva, E.; Moraes, R.R.; Cuevas-Suarez, C.E. Bond strength of self-adhesive flowable composite resins to dental tissues: A systematic review and meta-analysis of in vitro studies. J. Prosthet. Dent. 2022, 128, 876–885. [Google Scholar] [CrossRef] [PubMed]
- Peterson, J.; Rizk, M.; Hoch, M.; Wiegand, A. Bonding performance of self-adhesive flowable composites to enamel, dentin and a nano-hybrid composite. Odontology 2018, 106, 171–180. [Google Scholar] [CrossRef] [PubMed]
- Jordehi, A.Y.; Shahabi, M.S.; Akbari, A. Comparison of self-adhering flowable composite microleakage with several types of bonding agent in class V cavity restoration. Dent. Res. J. 2019, 16, 257–263. [Google Scholar] [CrossRef]
- Sachdeva, P.; Goswami, M.; Singh, D. Comparative evaluation of shear bond strength and nanoleakage of conventional and self-adhering flowable composites to primary teeth dentin. Contemp. Clin. Dent. 2016, 7, 326–331. [Google Scholar] [CrossRef]
- Sismanoglu, S. Efficiency of self-adhering flowable resin composite and different surface treatments in composite repair using a universal adhesive. Niger. J. Clin. Pract. 2019, 22, 1675–1679. [Google Scholar] [CrossRef]
- Kalola, A.V.; Sreejith, S.U.; Kanodia, S.; Parmar, A.; Iyer, J.V.; Parmar, G.J. Comparative clinical evaluation of a self-adhering flowable composite with conventional flowable composite in Class I cavity: An in vivo study. J. Conserv. Dent. 2022, 25, 156–160. [Google Scholar] [CrossRef]
- Wadhwa, S.; Nayak, U.; Kappadi, D.; Prajapati, D.; Sharma, R.; Pawar, A. Comparative Clinical Evaluation of Resin-based Pit and Fissure Sealant and Self-adhering Flowable Composite: An In Vivo Study. Int. J. Clin. Pediatr. Dent. 2018, 11, 430–434. [Google Scholar]
- Mine, A.; De Munck, J.; Van Ende, A.; Poitevin, A.; Matsumoto, M.; Yoshida, Y.; Kuboki, T.; Van Landuyt, K.L.; Yatani, H.; Van Meerbeek, B. Limited interaction of a self-adhesive flowable composite with dentin/enamel characterized by TEM. Dent. Mater. 2017, 33, 209–217. [Google Scholar] [CrossRef]
- Brueckner, C.; Schneider, H.; Haak, R. Shear Bond Strength and Tooth-Composite Interaction with Self-Adhering Flowable Composites. Oper. Dent. 2017, 42, 90–100. [Google Scholar] [CrossRef]
- Gayatri, C.; Rambabu, T.; Sajjan, G.; Battina, P.; Priyadarshini, M.S.; Sowjanya, B.L. Evaluation of Marginal Adaptation of a Self-Adhering Flowable Composite Resin Liner: A Scanning Electron Microscopic Stud. Contemp. Clin. Dent. 2018, 9 (Suppl. 2), S240–S245. [Google Scholar] [CrossRef] [PubMed]
- Vichi, A.; Margvelashvili, M.; Goracci, C.; Papacchini, F.; Ferrari, M. Bonding and sealing ability of a new self-adhering flowable composite resin in class I restorations. Clin. Oral Investig. 2013, 17, 1497–1506. [Google Scholar] [CrossRef]
- Maj, A.; Trzcionka, A.; Twardawa, H.; Tanasiewicz, M. A comparative clinical study of the self-adhering flowable composite resin vertise flow and the traditional flowable composite resin premise flowable. Coatings 2020, 10, 800. [Google Scholar] [CrossRef]
- Abusamra, E.M.M.; Elsharkawy, M.M.; Mahmoud, E.M.; El Mahy, W.E.M. Clinical evaluation of self-adhering flowable composite in non-carious cervical lesion. Egypt. Dent. J. 2016, 62, 757–764. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Paolone, G.; Mazzitelli, C.; Josic, U.; Scotti, N.; Gherlone, E.; Cantatore, G.; Breschi, L. Modeling Liquids and Resin-Based Dental Composite Materials—A Scoping Review. Materials 2022, 15, 3759. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Green, S.; Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Training. 2008. Available online: https://training.cochrane.org/handbook (accessed on 12 July 2025).
- de Oliveira, N.G.; Lima, A.S.L.C.; da Silveira, M.T.; de Souza Araújo, P.R.; Monteiro, G.Q.d.M.; de Vasconcelos, M.C. Evaluation of postoperative sensitivity in restorations with self-adhesive resin: A randomized split-mouth design-controlled study. Clin. Oral. Investig. 2020, 24, 1829–1835. [Google Scholar] [CrossRef]
- Pinna, R.; Bortone, A.; Sotgiu, G.; Dore, S.; Usai, P.; Milia, E. Clinical evaluation of the efficacy of one self-adhesive composite in dental hypersensitivity. Clin. Oral Investig. 2015, 19, 1663–1672. [Google Scholar] [CrossRef] [PubMed]
- Çelik, E.U.; Aka, B.; Yilmaz, F. Six-month Clinical Evaluation of a Self-adhesive Flowable Composite in Noncarious Cervical Lesions. J. Adhes. Dent. 2015, 17, 361–368. [Google Scholar] [PubMed]
- Sabbagh, J.; Dagher, S.; El Osta, N.; Souhaid, P. Randomized Clinical Trial of a Self-Adhering Flowable Composite for Class I Restorations: 2-Year Results. Int. J. Dent. 2017, 2017, 5041529. [Google Scholar] [CrossRef]
- AlHumaid, J.; Al Harbi, F.A.; ElEmbaby, A.E. Performance of Self-adhering Flowable Composite in Class V Restorations: 18 Months Clinical Study. J. Contemp. Dent. Pract. 2018, 19, 785–791. [Google Scholar]
- Shaalan, O.O.; Abou-Auf, E.; El Zoghby, A.F. Clinical evaluation of self-adhering flowable composite versus conventional flowable composite in conservative Class I cavities: Randomized controlled trial. J. Conserv. Dent. 2018, 21, 485–490. [Google Scholar] [CrossRef] [PubMed]
- Serin, B.A.; Yazicioglu, I.; Deveci, C.; Dogan, M.C. Clinical evaluation of a self-adhering flowable composite as occlusal restorative material in primary molars: One-year results. Eur. Oral Res. 2019, 53, 119–124. [Google Scholar] [PubMed]
- Oz, F.D.; Ergin, E.; Cakir, F.Y.; Gurgan, S. Clinical Evaluation of a Self-Adhering Flowable Resin Composite in Minimally Invasive Class I Cavities: 5-year Results of a Double Blind Randomized, Controlled Clinical Trial. Acta Stomatol. Croat. 2020, 54, 10–21. [Google Scholar] [CrossRef]
- Shaalan, O.O.; Abou-Auf, E. A 24-Month Evaluation of Self-Adhering Flowable Composite Compared to Conventional Flowable Composite in Conservative Simple Occlusal Restorations: A Randomized Clinical Trial. Contemp. Clin. Dent. 2021, 12, 368–375. [Google Scholar] [CrossRef]
- Vertise Flow Instructions for Use Kerr. Available online: https://www.ultimatedental.com/uploads/KaVoKerr-VertiseFlowIFU.pdf (accessed on 6 December 2024).
- Fusion Liquid Dentin Instructions for Use Pentrol Clinical Technologies. Available online: https://docplayer.net/167674922-Liquid-dentin-a-fusion-of-composite-adhesive-technology.html (accessed on 6 December 2024).
- Hickel, R.; Roulet, J.F.; Bayne, S.; Heintze, S.D.; Mjör, I.A.; Peters, M.; Rousson, V.; Randall, R.; Schmalz, G.; Tyas, M.; et al. Recommendations for conducting controlled clinical studies of dental restorative materials. Clin. Oral Investig. 2007, 11, 5–33. [Google Scholar] [CrossRef]
- Valizadeh, S.; Asiaie, Z.; Kiomarsi, N.; Kharazifard, M.J. Color stability of self-adhering composite resins in different solutions. Dent. Med. Probl. 2020, 57, 31–38. [Google Scholar] [CrossRef]
- Marquillier, T.; Doméjean, S.; Le Clerc, J.; Chemla, F.; Gritsch, K.; Maurin, J.C.; Millet, P.; Pérard, M.; Grosgogeat, B.; Dursun, E. The use of FDI criteria in clinical trials on direct dental restorations: A scoping review. J. Dent. 2018, 68, 1–9. [Google Scholar] [CrossRef]
- Elshinawy, F.M.; Abu, A.E.; Khallaf, Y.S. Evaluation of Clinical Performance of Self-Adhering Flowable Composite vs. Conventional Flowable Composite in Cervical Carious Lesions: A Randomized Clinical Trial. Adv. Dent. J. 2023, 5, 186–194. [Google Scholar] [CrossRef]
- Arbildo-Vega, H.I.; Lapinska, B.; Panda, S. Clinical Effectiveness of Bulk-Fill and Conventional Resin Composite Restorations: Systematic Review and Meta-Analysis. Polymers 2020, 12, 1786. [Google Scholar] [CrossRef]
- Azizi, F.; Ezoji, F.; Khafri, S.; Esmaeili, B. Surface Micro-Hardness and Wear Resistance of a Self-Adhesive Flowable Composite in Comparison to Conventional Flowable Composites. Front. Dent. 2023, 20, 10. [Google Scholar] [CrossRef]
- Veloso, S.R.M.; Lemos, C.A.A.; de Moraes, S.L.D.; Vasconcelos, B.C.d.E.; Pellizzer, E.P.; Monteiro, G.Q.d.M. Clinical performance of bulk-fill and conventional resin composite restorations in posterior teeth: A systematic review and meta-analysis. Clin. Oral Investig. 2019, 23, 221–233. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]

| The USPHS Criteria |
|---|
| Retention Alpha (A): Restoration is present. Delta (D): Restoration is partially or totally missing. Color match Alpha (A): The restoration matches the adjacent tooth tissue in color, shade, or translucency. Bravo (B): There is a slight mismatch in color, shade, or translucency, but within the normal range of the adjacent tooth structure. Charlie (C): There is a slight mismatch in color, shade, or translucency, but outside of the normal range of the adjacent tooth structure. |
| Marginal discoloration Alpha (A): There is discoloration anywhere along the margin between the restoration and the adjacent tooth structure. Bravo (B): Discoloration is present, but has not penetrated along the margin in a pulpal direction. Charlie (C): Discoloration has penetrated along the margin in a pulpal direction. |
| Recurrent caries Alpha (A): No caries are present at the margin of the restoration, as evidenced by softness, opacity, or etching at the margin. Bravo (B): There is evidence of caries at the margin of the restoration. |
| Surface roughness Alpha (A): The restoration surface is as smooth as the surrounding enamel. Bravo (B): The restoration surface is rougher than the surrounding enamel. Charlie (C): Surface pitting is sufficiently coarse to inhibit the continuous movement of an explorer across the surface. |
| Marginal integrity Alpha (A): There is no visible evidence of a crevice along the margin into which the explorer penetrates. Bravo (B): There is visible evidence of a crevice along the margin into which the explorer penetrates or catches. Charlie (C): The explorer penetrates the crevice, and dentin or the base is exposed. Delta (D): The restoration is mobile, or missing, either in part or total. |
| Post-operative sensitivity Alpha (A): Normal reaction to cold spray compared with that of no restored teeth. Bravo (B): Increased cold sensitivity. Charlie (C): Spontaneous pain. Delta (D): Nonvital. |
| The FDI Criteria |
|---|
|
Aesthetic properties
Surface gloss Score 1: Gloss similar to enamel. Score 2: Slightly opaque; Some isolated pores. Score 3: Opaque surface, but acceptable if covered by saliva; Multiple pores in more than half of the surface. Score 4: Rough surface, where polishing is not sufficient. Score 5: Very rough surface, unacceptable. Staining Score 1: No superficial or marginal staining. Score 2: Minimal staining, easily removable. Score 3: Moderate staining, also present in other teeth, and aesthetically acceptable. Score 4: Unacceptable staining in the restoration, intervention necessary. Score 5: Severe generalized or localized staining, without access for intervention. Color stability or translucency Score 1: Good coloration and translucency compared to neighboring teeth. Score 2: Minimal color and translucency deviation. Score 3: Clear deviation, but without affecting aesthetics. Score 4: Localized clinical deviation that can be corrected by repair. Score 5: Unacceptable, replacement necessary. Anatomic shape Score 1: Ideal shape. Score 2: Shape slightly deviates from normal. Score 3: Shape differs from normal but does not compromise aesthetics. Score 4: Shape is affected and aesthetically unacceptable. Intervention/correction is necessary. Score 5: Unacceptable or lost. Requires replacement. |
|
Functional properties
Fractures and retention Score 1: No fractures or cracks. Score 2: Small crack. Score 3: Cracks that do not affect marginal adaptation. Score 4: Chips that damage marginal adaptation or contact point. Score 5: Partial or total loss of the restoration. Marginal adaptation Score 1: Harmonious line without gaps or discoloration. Score 2: Small marginal fracture, removable with polishing. Score 3: Gap less than 150µm, not removable; Several small fractures in enamel and dentin. Score 4: Gap larger than 250 µm or exposed dentin; Chips damage margin; Noticeable fracture in enamel or dentin. Score 5: Large gaps or widespread irregularities. Anatomic shape Score 1: Normal contact point (dental floss or 25 µm metal foil can pass through; Normal contour. Score 2: Slightly too strong contact but without disadvantage (dental floss or 25 µm metal foil can only pass with pressure); Slightly deficient contour. Score 3: Somewhat weak contact, no indication of damage to the tooth, gum, or periodontal structures; 50 µm metal foil can pass; Visibly deficient contour. Score 4: Too weak and possible damage due to food impaction; 100 µm metal foil can pass; Inadequate contour; Repair possible. Score 5: Too weak and/or clear damage due to food impaction and/or pain/gingivitis; Insufficient contour, requires replacement. |
|
Biological properties
Post-operative sensitivity Score 1: No hypersensitivity; normal vitality. Score 2: Low hypersensitivity for a short period of time; normal vitality. Score 3: Moderate hypersensitivity; Weak sensitivity that does not require treatment. Score 4: Intense hypersensitivity; Negative sensitivity; intervention necessary, but no replacement. Score 5: Very intense, pulpitis or nonvital. Endodontics is necessary for restoration or replacement. Caries recurrence Score 1: No secondary or primary caries. Score 2: Small and localized; Demineralization. Score 3: Larger areas of lesion without dentin exposure. Score 4: Caries with cavitation. Score 5: Deep secondary caries or exposed dentin, not accessible for repair or restoration |
| Author (s) | Country | Study Design | Patients (n) | Mean Age (Years) | Teeth Restored | Groups | Tooth Type | Cavity Type | Follow-Up (Months) | Criteria | Conclusion |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Çelik, Aka and Yilmaz (2015) [22] | Turkey | RCT | 19 | 35–79 | 80 | G1: FLD G2: G-aenial | Anterior and posterior | Class V (NCCLs) | 6 | FDI | SAFR exhibited unacceptable performance |
| Sabbagh et al. (2017) [23] | Lebanon | RCT | 34 | 6–12 | 68 | G1: VF G2: PF | Molar | Class I | 24 | USPHS | SAFR performed similarly to CC |
| AlHumaid, Harbi, and ElEmbaby (2018) [24] | Saudi Arabia | RCT | 20 | * | 40 | G1: FLD G2: TNF | Anterior | Class V (CCLs) | 18 | USPHS | SAFR exhibited comparable performance to CC |
| Shaalan, Abou-Auf and Zoghby (2018) [25] | Egypt | RCT | 18 | 19–40 | 18 | G1: VF G2: z350 | Molar | Class I | 6 | USPHS | SAFR exhibited similar performance to CC |
| Serin et al. (2019) [26] | Egypt | RCT | 31 | 4–9 | 62 | G1: VF G2: z250 | Molar deciduous | Class I | 12 | USPHS | SAFRs predominantly showed alpha scores |
| Oz et al. (2020) [27] | Egypt | RCT | 15 | 20 | 65 | G1: VF G2: LF | Molar | Class I | 60 | FDI | SAFR demonstrated performance similar to CC |
| Maj et al. (2020) [14] | Poland | RCT | 37 | 34–54 | 64 | G1: VF G2: PF + OAO G3: PF + AE + OSP | Molar and incisor | Class I | 24 | USHPS | SAFR exhibited weaker results in terms of marginal adaptation and polishing. |
| Shaalan and Abou-Auf (2021) [28] | Egypt | RCT | 18 | 19–40 | 36 | G1: VF G2: z350 Xt | Molar | Class I | 24 | USHPS | SAFR showed performance comparable to CC |
| Kalola et al. (2022) [8] | India | RCT | 30 | 18–54 | 60 | G1: FLD G2: TNF | Molar | Class I | 12 | USPHS | SAFR exhibited satisfactory clinical performance. |
| Author, Year | Cavity | Conventional Resin Composite | Self-Adhering Resin Flowable | ||
|---|---|---|---|---|---|
| Criteria | Failure/Total | Criteria | Failure/ Total | ||
| Çelik, Aka and Yilmaz (2015) [22] | Class V | Marginal adaptation | 0/40 | Marginal adaptation | 0/13 |
| Retention | 0/40 | Retention | 27/40 | ||
| Post-operative sensibility | 0/40 | Post-operative sensibility | 0/13 | ||
| Marginal staining | 0/40 | Marginal staining | 0/13 | ||
| Color Match | 0/40 | Color Match | 0/13 | ||
| Secondary caries | 0/40 | Secondary caries | 0/13 | ||
| Anatomical Form | 0/40 | Anatomical Form | 0/13 | ||
| Sabbagh et al. (2017) [23] | Class I | * | * | ||
| AlHumaid, Harbi, and ElEmbaby (2018) [24] | Class V | Marginal adaptation | 3/20 | Marginal adaptation | 0/20 |
| Marginal staining | 1/20 | Marginal staining | 0/20 | ||
| Color match | 2/20 | Color match | 0/20 | ||
| Surface roughness | 1/20 | Surface roughness | 0/20 | ||
| Shaalan, Abou-Auf and Zoghby (2018) [25] | Class I | Marginal adaptation | 0/18 | Marginal adaptation | 0/18 |
| Retention | 0/18 | Retention | 0/18 | ||
| Post-operative sensibility | 0/18 | Post-operative sensibility | 0/18 | ||
| Marginal Staining | 0/18 | Marginal Staining | 0/18 | ||
| Color Match | 0/18 | Color Match | 0/18 | ||
| Serin et al. (2019) [26] | Class I | Retention | 0/29 | Retention | 0/29 |
| Post-operative sensibility | 0/29 | Post-operative sensibility | 0/29 | ||
| Marginal Staining | 0/29 | Marginal Staining | 0/29 | ||
| Anatomical form | 0/29 | Anatomical form | 0/29 | ||
| Maj et al. (2020) [14] | Class I | Retention | 0/22 | Retention | 1/22 |
| Marginal Staining | 0/22 | Marginal Staining | 0/22 | ||
| Color Match | 0/22 | Color Match | 1/22 | ||
| Proper Smoothness | 0/22 | Proper Smoothness | 0/22 | ||
| Anatomical form | 0/22 | Anatomical form | 0/22 | ||
| Oz et al. (2020) [27] | Class I | Marginal adaptation | 0/24 | Marginal adaptation | 0/22 |
| Retention | 1/24 | Retention | 0/22 | ||
| Post-operative sensibility | 0/24 | Post-operative sensibility | 0/22 | ||
| Marginal staining | 0/24 | Marginal staining | 0/22 | ||
| Color Match | 0/24 | Color Match | 0/22 | ||
| Proper Smoothness | 0/24 | Proper Smoothness | 0/22 | ||
| Secondary caries | 0/24 | Secondary caries | 0/22 | ||
| Shaalan e Abou-Auf (2021) [28] | Class I | Marginal adaptation | 0/18 | Marginal adaptation | 0/18 |
| Marginal staining | 0/18 | Marginal staining | 0/18 | ||
| Color Match | 0/18 | Color Match | 0/18 | ||
| Proper Smoothness | 0/18 | Proper Smoothness | 0/18 | ||
| Secondary caries | 0/18 | Secondary caries | 0/18 | ||
| Anatomical Form | 0/18 | Anatomical Form | 0/18 | ||
| Kalola et al. (2022) [8] | Class I | Retention | 0/30 | Retention | 0/30 |
| Post-operative sensibility | 0/30 | Post-operative sensibility | 2/30 | ||
| Marginal staining | 0/30 | Marginal staining | 0/30 | ||
| Color Match | 0/30 | Color Match | 0/30 | ||
| Surface roughness | 0/30 | Surface roughness | 0/30 | ||
| Secondary caries | 0/30 | Secondary caries | 0/30 | ||
| Anatomical Form | 0/30 | Anatomical Form | 0/30 | ||
| Certainty Assessment | No. of Patients | Effect | Certainty | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No of Studies | Study Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Other Considerations | SAFRs | CFR | Relative (95% CI) | Absolute (95% CI) | |
| Marginal Adaptation (follow-up: range 6 months to 5 years) | |||||||||||
| 5 | RCT | NS a | NS b | NS c | NS d | VSA e | 0/110 (0.0%) | 0/112 (0.0%) | RR 0.00 (−0.04 to 0.04) | -- per 1.000 (from 0 fewer to 0 fewer) | ⊕⊕⊕⊕ High |
| Retention (follow-up: range 6 months to 5 years) | |||||||||||
| 3 | RCT | NS e | NS b | NS c | NS d | VSA e | 0/70 (0.0%) | 1/72 (1.4%) | RR −0.01 (−0.06 to 0.04) | 14 fewer per 1.000 (from 15 fewer to 13 fewer) | ⊕⊕⊕⊕ High |
| Post-operative sensibility (follow-up: range 6 months to 5 years) | |||||||||||
| 3 | RCT | NS e | NS b | NS c | NS d | VSA e | 0/70 (0.0%) | 0/72 (0.0%) | RR 0.00 (−0.04 to 0.04) | -- per 1.000 (from 0 fewer to 0 fewer) | ⊕⊕⊕⊕ High |
| Color match (follow-up: range 1 year to 5 years) | |||||||||||
| 5 | RCT | NS a | NS b | NS c | NS d | VSA e | 1/110 (0.9%) | 0/112 (0.0%) | RR 0.00 (−0.03 to 0.04) | -- per 1.000 (from 0 fewer to 0 fewer) | ⊕⊕⊕⊕ High |
| Marginal discoloration (follow-up: range 6 months to 5 years) | |||||||||||
| 5 | RCT | NS | NS | NS | NS | VSA e | 0/110 (0.0%) | 0/112 (0.0%) | RR 0.00 (−0.04 to 0.04) | -- per 1.000 (from 0 fewer to 0 fewer) | ⊕⊕⊕⊕ High |
| Anatomic Form (follow-up: range 1 year to 2 years) | |||||||||||
| 3 | RCT | NS | NS | NS | NS | VSA e | 0/70 (0.0%) | 0/70 (0.0%) | RR 0.00 (−0.05 to 0.05) | -- per 1.000 (from 0 fewer to 0 fewer) | ⊕⊕⊕⊕ High |
| Secondary caries (follow-up: range 1 year to 2 years) | |||||||||||
| 3 | RCT | NS | NS | NS | NS | VSA e | 0/70 (0.0%) | 0/72 (0.0%) | RR 0.00 (−0.04 to 0.04) | -- per 1.000 (from 0 fewer to 0 fewer) | ⊕⊕⊕⊕ High |
| Smoothness (follow-up: range 1 year to 2 years) | |||||||||||
| 3 | RCT | NS | NS | NS | NS | VSA e | 0/62 (0.0%) | 0/63 (0.0%) | RR 0.00 (−0.05 to 0.05) | -- per 1.000 (from 0 fewer to 0 fewer) | ⊕⊕⊕⊕ High |
| Outcome | RR | 95% CI | n (SAFR/CFR) | p-Value | GRADE Certainty |
|---|---|---|---|---|---|
| Marginal Adaptation | 0.00 | −0.04 to 0.04 | 110/112 | 0.53 | High |
| Retention | −0.01 | −0.06 to 0.04 | 70/72 | 0.81 | High |
| Post-operative Sensitivity | 0.00 | −0.04 to 0.04 | 70/72 | 0.62 | High |
| Color Match | 0.00 | −0.03 to 0.04 | 110/112 | >0.05 | High |
| Marginal Discoloration | 0.00 | −0.04 to 0.04 | 110/112 | >0.05 | High |
| Anatomic Form | 0.00 | −0.05 to 0.05 | 70/70 | >0.05 | High |
| Secondary Caries | 0.00 | −0.04 to 0.04 | 70/72 | >0.05 | High |
| Smoothness | 0.00 | −0.05 to 0.05 | 62/63 | >0.05 | High |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miranda, S.B.; Leal, C.d.F.C.; Mendonça, G.L.d.; Lima, R.B.W.e.; Andrade, A.K.M.d.; Lins, R.B.E.; Montes, M.A.J.R. Clinical Performance of Self-Adhesive vs. Conventional Flowable Resin Composite Restorations in Posterior Teeth: A Systematic Review and Meta-Analysis of Randomized Trials. J. Clin. Med. 2025, 14, 5862. https://doi.org/10.3390/jcm14165862
Miranda SB, Leal CdFC, Mendonça GLd, Lima RBWe, Andrade AKMd, Lins RBE, Montes MAJR. Clinical Performance of Self-Adhesive vs. Conventional Flowable Resin Composite Restorations in Posterior Teeth: A Systematic Review and Meta-Analysis of Randomized Trials. Journal of Clinical Medicine. 2025; 14(16):5862. https://doi.org/10.3390/jcm14165862
Chicago/Turabian StyleMiranda, Samille Biasi, Caroline de Farias Charamba Leal, Giovana Lordsleem de Mendonça, Renally Bezerra Wanderley e Lima, Ana Karina Maciel de Andrade, Rodrigo Barros Esteves Lins, and Marcos Antonio Japiassú Resende Montes. 2025. "Clinical Performance of Self-Adhesive vs. Conventional Flowable Resin Composite Restorations in Posterior Teeth: A Systematic Review and Meta-Analysis of Randomized Trials" Journal of Clinical Medicine 14, no. 16: 5862. https://doi.org/10.3390/jcm14165862
APA StyleMiranda, S. B., Leal, C. d. F. C., Mendonça, G. L. d., Lima, R. B. W. e., Andrade, A. K. M. d., Lins, R. B. E., & Montes, M. A. J. R. (2025). Clinical Performance of Self-Adhesive vs. Conventional Flowable Resin Composite Restorations in Posterior Teeth: A Systematic Review and Meta-Analysis of Randomized Trials. Journal of Clinical Medicine, 14(16), 5862. https://doi.org/10.3390/jcm14165862