Collision Course: A Decade of Traumatic Brain Injury Trends and the Impact of Urban Safety Initiatives in Eastern Massachusetts
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Collection
2.3. TBI Severity Determination
2.4. Discharge Disability Evaluation
2.5. Data Analysis
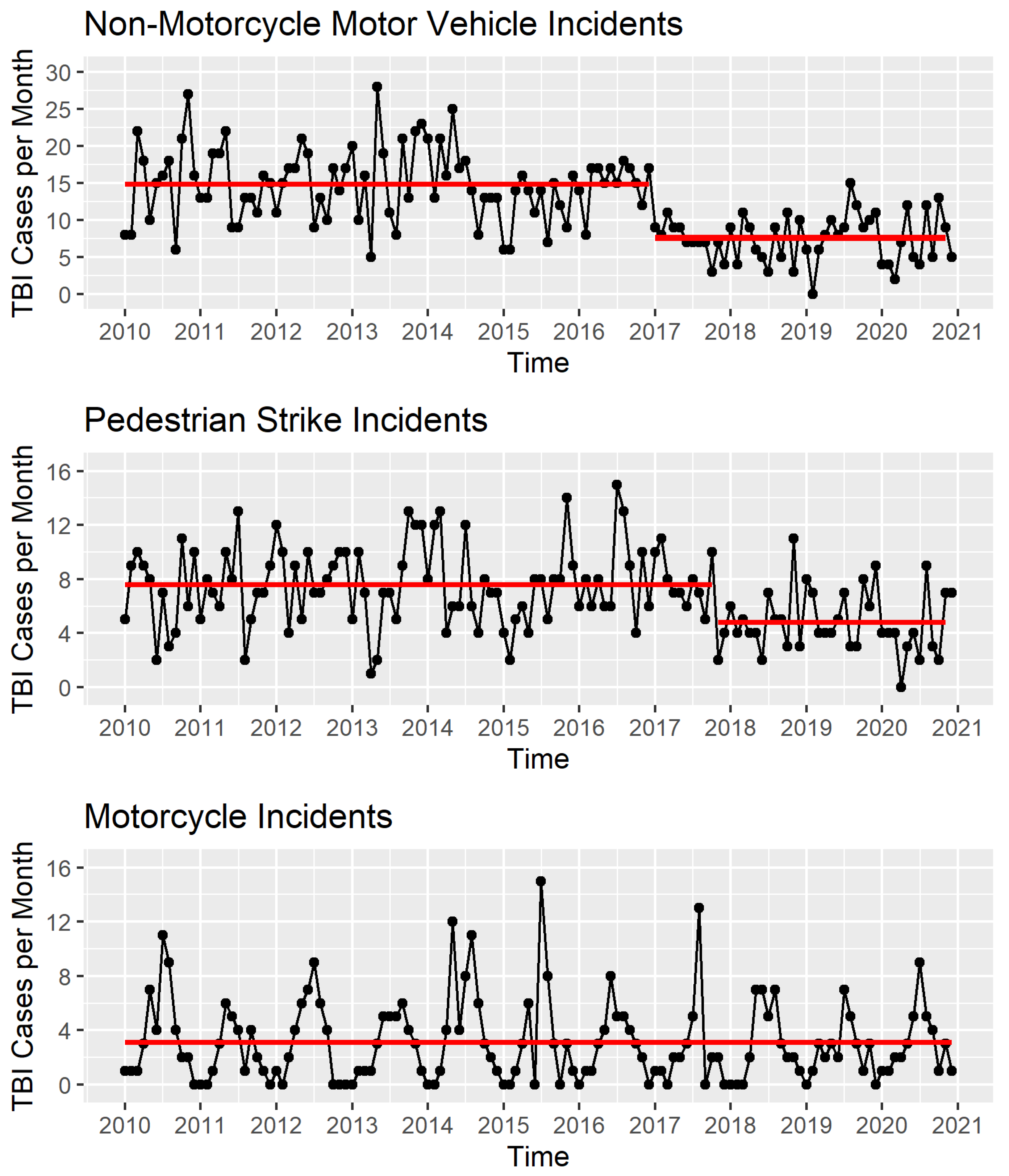
3. Results
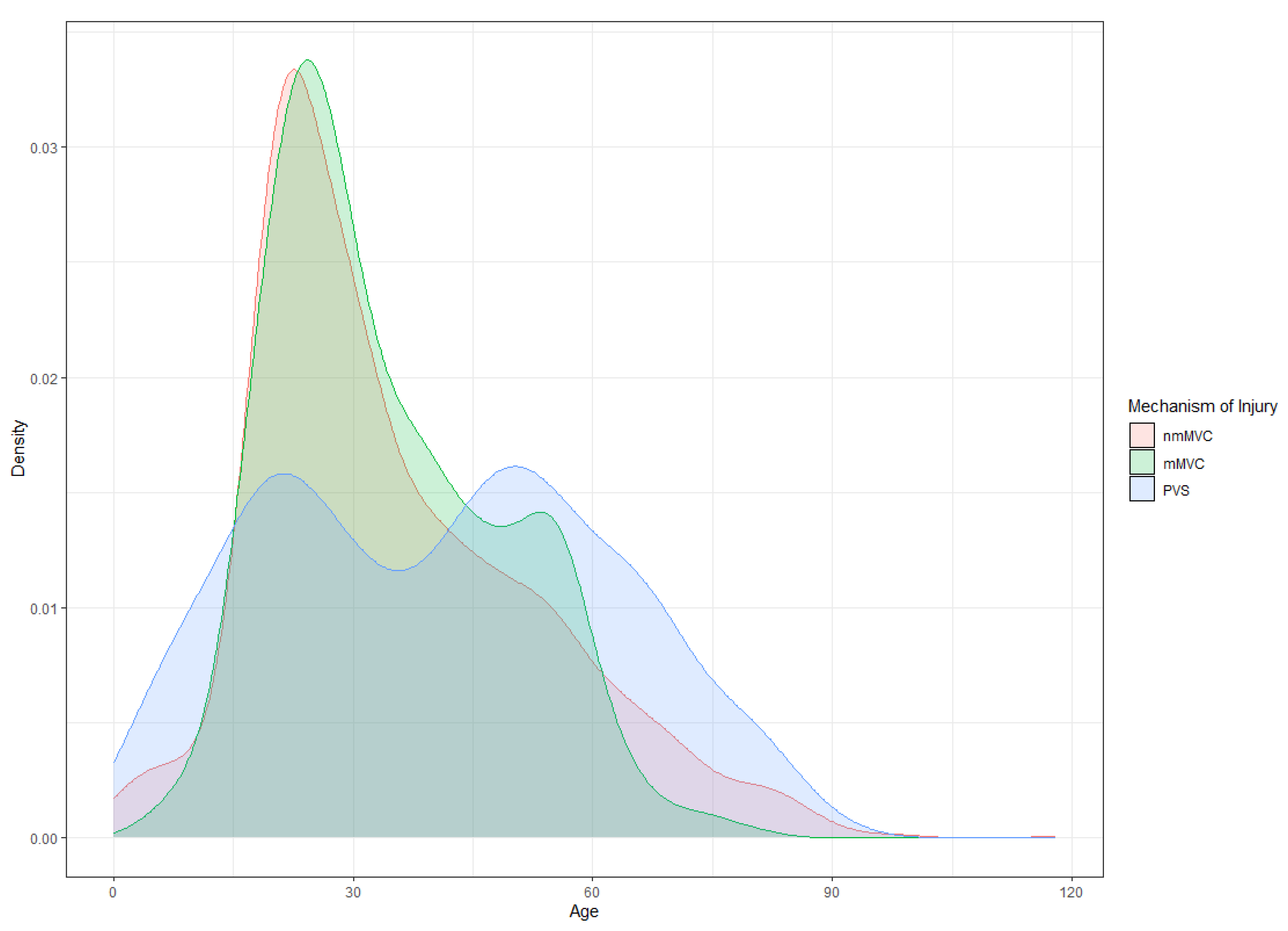
3.1. Age and Gender
3.2. Race/Ethnicity and Location
3.3. TBI Severity Incidence
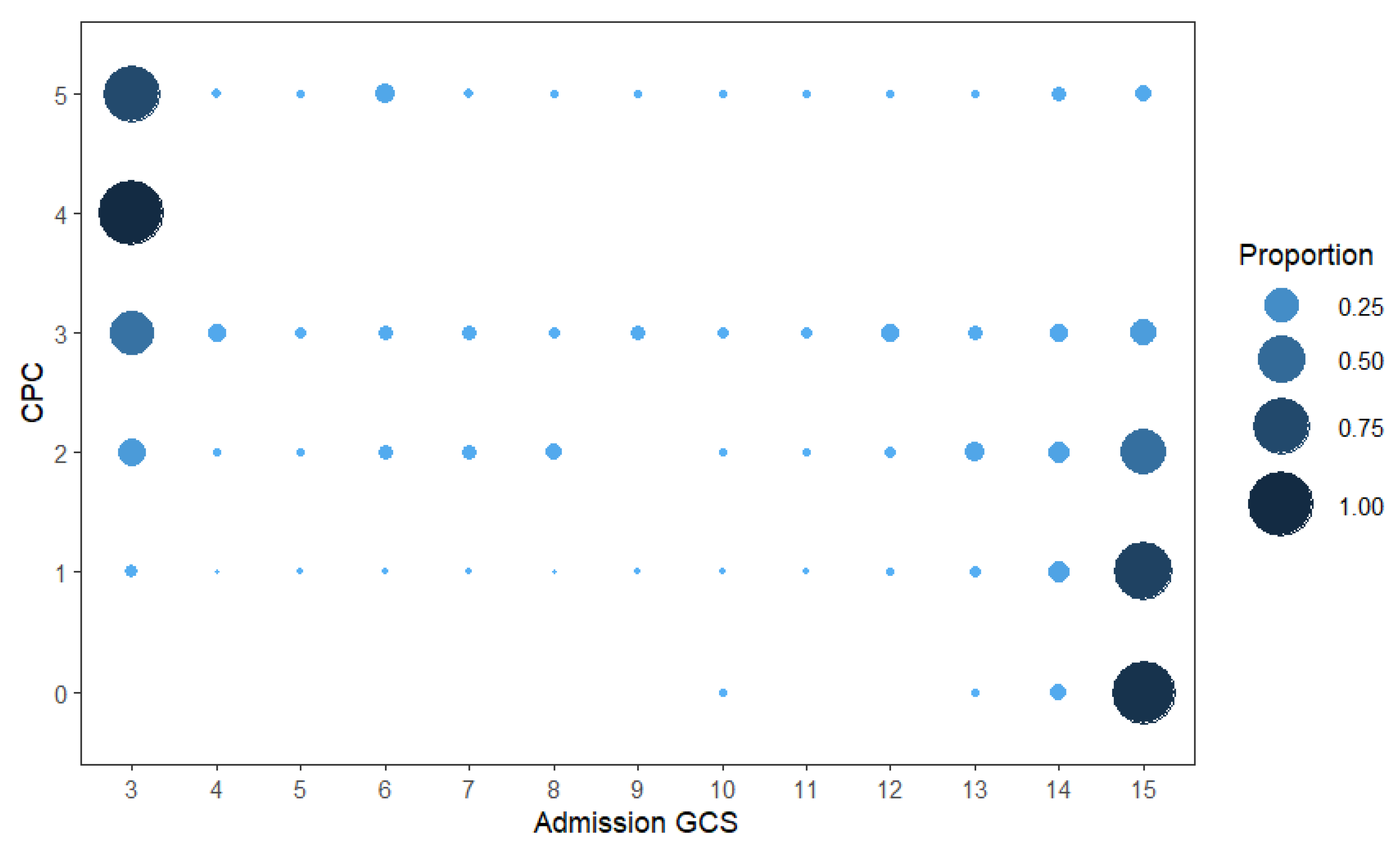
3.4. Discharge Disability Outcomes
4. Discussion
4.1. Demographic Findings
4.2. TBI Severity and Admission GCS Score
4.3. Discharge Outcomes
4.4. Implications for Prevention and Treatment
4.5. Limitations and Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- FastStats. Available online: https://www.cdc.gov/nchs/fastats/accidental-injury.htm (accessed on 20 January 2024).
- Fatal Injury Trends|Injury Center|CDC. Available online: https://www.cdc.gov/injury/wisqars/fatal/trends.html (accessed on 20 January 2024).
- Get the Facts About TBI|Concussion|Traumatic Brain Injury|CDC Injury Center. Available online: https://www.cdc.gov/traumaticbraininjury/get_the_facts.html (accessed on 20 January 2024).
- Devi, Y.; Khan, S.; Rana, P.; Dhandapani, M.; Ghai, S.; Gopichandran, L.; Dhandapani, S. Cognitive, Behavioral, and Functional Impairments among Traumatic Brain Injury Survivors: Impact on Caregiver Burden. J. Neurosci. Rural Pract. 2020, 11, 629–635. [Google Scholar] [CrossRef] [PubMed]
- Ritter, M. Evidence-Based Pearls: Traumatic Brain Injury. Crit. Care Nurs. Clin. N. Am. 2023, 35, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Faried, A.; Bachani, A.M.; Sendjaja, A.N.; Hung, Y.W.; Arifin, M.Z. Characteristics of Moderate and Severe Traumatic Brain Injury of Motorcycle Crashes in Bandung, Indonesia. World Neurosurg. 2017, 100, 195–200. [Google Scholar] [CrossRef]
- Sayyed Hoseinian, S.H.; Ebrahimzadeh, M.H.; Peivandi, M.T.; Bagheri, F.; Hasani, J.; Golshan, S.; Birjandinejad, A. Injury Patterns among Motorcyclist Trauma Patients: A Cross Sectional Study on 4200 Patients. Arch. Bone Jt. Surg. 2019, 7, 367–372. [Google Scholar] [PubMed]
- Edwards, M.; Leonard, D. Effects of Large Vehicles on Pedestrian and Pedalcyclist Injury Severity. J. Saf. Res. 2022, 82, 275–282. [Google Scholar] [CrossRef]
- Zohrevandi, B.; Rad, E.H.; Kouchakinejad-Eramsadati, L.; Imani, G.; Pourheravi, I.; Khodadadi-Hassankiadeh, N. Epidemiology of Head Injuries in Pedestrian-Motor Vehicle Accidents. Sci Rep. 2023, 13, 20249. [Google Scholar] [CrossRef]
- Bureau of Transportation Statistics. National Household Travel Survey Daily Travel Quick Facts. Available online: https://www.bts.gov/statistical-products/surveys/national-household-travel-survey-daily-travel-quick-facts (accessed on 20 January 2024).
- Halari, M.M.; Shkrum, M.J. Fatal Motor Vehicle-Pedestrian Collision Injury Patterns-A Systematic Literature Review. Acad. Forensic Pathol. 2020, 10, 144–157. [Google Scholar] [CrossRef]
- Gary, K.W.; Arango-Lasprilla, J.C.; Stevens, L.F. Do Racial/Ethnic Differences Exist in Post-Injury Outcomes after TBI? A Comprehensive Review of the Literature. Brain Inj. 2009, 23, 775–789. [Google Scholar] [CrossRef]
- Wu, M. Vision Zero Boston Action Plan 2023. Available online: https://www.boston.gov/sites/default/files/file/2024/05/2023%20Vision%20Zero%20Action%20Plan%2023-08-11.pdf (accessed on 20 January 2024).
- National Library of Medicine Institution. Brain Failure and Resuscitation. Available online: https://catalog.nlm.nih.gov/discovery/fulldisplay/alma995387133406676/01NLM_INST:01NLM_INST (accessed on 30 July 2025).
- R: The R Project for Statistical Computing. Available online: https://www.r-project.org/ (accessed on 19 September 2024).
- Motorcycle Demographics: 59 User Facts & Numbers [2023]. Motor & Wheels. Available online: https://motorandwheels.com/motorcycle-demographics/ (accessed on 31 March 2024).
- Kelley, E.A.; Kandula, N.R.; Kanaya, A.M.; Yen, I.H. Neighborhood Walkability and Walking for Transport Among South Asians in the MASALA Study. J. Phys. Act. Health 2016, 13, 514–519. [Google Scholar] [CrossRef]
- Cerin, E.; Lee, K.; Barnett, A.; Sit, C.H.; Cheung, M.; Chan, W.; Johnston, J.M. Walking for Transportation in Hong Kong Chinese Urban Elders: A Cross-Sectional Study on What Destinations Matter and When. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 78. [Google Scholar] [CrossRef]
- Lewis, S.; Grande, E.; Robinson, R. Boston’s Walkable Neighborhood Systems: Delineation and Performance. GeoJournal 2023, 88, 4049–4079. [Google Scholar] [CrossRef]
- Harmon, K.J.; Marshall, S.W.; Proescholdbell, S.K.; Naumann, R.B.; Waller, A.E. Motorcycle Crash-Related Emergency Department Visits and Hospitalizations for Traumatic Brain Injury in North Carolina. J. Head Trauma Rehabil. 2015, 30, 175. [Google Scholar] [CrossRef] [PubMed]
- Yun, H.; Bae, S.J.; Lee, J.I.; Lee, D.H. Epidemiology, Injury Characteristics and Clinical Outcomes of Bicycle and Motorcycle Accidents in the under 20 Population: South Korea. BMC Emerg. Med. 2022, 22, 56. [Google Scholar] [CrossRef] [PubMed]
- Chudyk, A.M.; Winters, M.; Moniruzzaman, M.; Ashe, M.C.; Gould, J.S.; McKay, H. Destinations Matter: The Association between Where Older Adults Live and Their Travel Behavior. J. Transp. Health 2015, 2, 50–57. [Google Scholar] [CrossRef] [PubMed]
- Rasca, S.; Saeed, N. Exploring the Factors Influencing the Use of Public Transport by Commuters Living in Networks of Small Cities and Towns. Travel Behav. Soc. 2022, 28, 249–263. [Google Scholar] [CrossRef]
- Turrell, G.; Hewitt, B.; Haynes, M.; Nathan, A.; Giles-Corti, B. Change in Walking for Transport: A Longitudinal Study of the Influence of Neighbourhood Disadvantage and Individual-Level Socioeconomic Position in Mid-Aged Adults. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 151. [Google Scholar] [CrossRef]
- Jamal, S.; Newbold, K.B. Factors Associated with Travel Behavior of Millennials and Older Adults: A Scoping Review. Sustainability 2020, 12, 8236. [Google Scholar] [CrossRef]
- Zhao, G.; Cao, M.; De Vos, J. Exploring Walking Behaviour and Perceived Walkability of Older Adults in London. J. Transp. Health 2024, 37, 101832. [Google Scholar] [CrossRef]
- Doulabi, S.; Hassan, H.M.; Ferguson, M.R.; Razavi, S.; Paez, A. Exploring the Determinants of Older Adults’ Susceptibility to Pedestrians’ Incidents. Accid. Anal. Prev. 2021, 155, 106100. [Google Scholar] [CrossRef]
- Islam, M. The Effect of Motorcyclists’ Age on Injury Severities in Single-Motorcycle Crashes with Unobserved Heterogeneity. J. Saf. Res. 2021, 77, 125–138. [Google Scholar] [CrossRef]
- Chaudhuri, U.; Ratnapradipa, K.L.; Shen, S.; Rice, T.M.; Smith, G.A.; Zhu, M. Trends and Patterns in Fatal US Motorcycle Crashes, 2000–2016. Traffic Inj. Prev. 2019, 20, 641–647. [Google Scholar] [CrossRef]
- Reith, G.; Lefering, R.; Wafaisade, A.; Hensel, K.O.; Paffrath, T.; Bouillon, B.; Probst, C. Injury Pattern, Outcome and Characteristics of Severely Injured Pedestrian. Scand. J. Trauma Resusc. Emerg. Med. 2015, 23, 56. [Google Scholar] [CrossRef] [PubMed]
- Patil, R.; Baker, M.B.; Binda, D.D.; Hsieh, A.; Varghese, S.; He, X.A.; Dienes, E.; Nozari, A. Efficacy and Safety of Early Surgical Fixation of Fractures in Patients with Traumatic Brain Injury: A Scoping Review. J. Oral Maxillofac. Anesth. 2025, 4, 4–9. [Google Scholar] [CrossRef]
- Hillary, F.G.; Schatz, P.; Moelter, S.T.; Lowry, J.B.; Ricker, J.H.; Chute, D.L. Motor Vehicle Collision Factors Influence Severity and Type of TBI. Brain Inj. 2002, 16, 729–741. [Google Scholar] [CrossRef]
- Marmarou, A.; Lu, J.; Butcher, I.; McHugh, G.S.; Mushkudiani, N.A.; Murray, G.D.; Steyerberg, E.W.; Maas, A.I.R. Impact Database of Traumatic Brain Injury: Design and Description. J. Neurotrauma 2007, 24, 239–250. [Google Scholar] [CrossRef]
- Stocchetti, N.; Paternò, R.; Citerio, G.; Beretta, L.; Colombo, A. Traumatic Brain Injury in an Aging Population. J. Neurotrauma 2012, 29, 1119–1125. [Google Scholar] [CrossRef]
- McCrea, M.A.; Giacino, J.T.; Barber, J.; Temkin, N.R.; Nelson, L.D.; Levin, H.S.; Dikmen, S.; Stein, M.; Bodien, Y.G.; Boase, K.; et al. Functional Outcomes Over the First Year After Moderate to Severe Traumatic Brain Injury in the Prospective, Longitudinal TRACK-TBI Study. JAMA Neurol. 2021, 78, 982–992. [Google Scholar] [CrossRef] [PubMed]
- Daugherty, J. Traumatic Brain Injury–Related Deaths by Race/Ethnicity, Sex, Intent, and Mechanism of Injury—United States, 2000–2017. MMWR Morb. Mortal. Wkly. Rep. 2019, 68, 1050–1056. [Google Scholar] [CrossRef]
- Gao, S.; Kumar, R.G.; Wisniewski, S.R.; Fabio, A. Disparities in Health Care Utilization of Adults with Traumatic Brain Injuries Are Related to Insurance, Race, and Ethnicity: A Systematic Review. J. Head Trauma Rehabil. 2018, 33, E40–E50. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Baker, S.P.; Langlois, J.A.; Kelen, G.D. Are Female Drivers Safer? An Application of the Decomposition Method. Epidemiology 1998, 9, 379–384. [Google Scholar] [CrossRef]
- Hu, W.; Cicchino, J.B. Lowering the Speed Limit from 30 Mph to 25 Mph in Boston: Effects on Vehicle Speeds. Inj. Prev. 2020, 26, 99–102. [Google Scholar] [CrossRef]
- Maas, A.I.R.; Stocchetti, N.; Bullock, R. Moderate and Severe Traumatic Brain Injury in Adults. Lancet Neurol. 2008, 7, 728–741. [Google Scholar] [CrossRef] [PubMed]
- Maas, A.I.R.; Menon, D.K.; Manley, G.T.; Abrams, M.; Åkerlund, C.; Andelic, N.; Aries, M.; Bashford, T.; Bell, M.J.; Bodien, Y.G.; et al. Traumatic Brain Injury: Progress and Challenges in Prevention, Clinical Care, and Research. Lancet Neurol. 2022, 21, 1004–1060. [Google Scholar] [CrossRef] [PubMed]
- Iaccarino, C.; Carretta, A.; Nicolosi, F.; Morselli, C. Epidemiology of Severe Traumatic Brain Injury. J. Neurosurg. Sci. 2018, 62, 535–541. [Google Scholar] [CrossRef] [PubMed]
- Peterson, A.B.; Zhou, H.; Thomas, K.E. Disparities in Traumatic Brain Injury-Related Deaths—United States, 2020. J. Saf. Res. 2022, 83, 419–426. [Google Scholar] [CrossRef]
- Jenkins, K.; Binda, D.D.; Baker, M.B.; Hsieh, A.; Aronow, B.; Merriel, M.; Nozari, A. Anesthetic Considerations for Oral Maxillofacial Surgery in Neurologically Injured Patients: A Comprehensive Narrative Review. J. Oral Maxillofac. Anesth. 2023, 2, 31. [Google Scholar] [CrossRef]
| Mechanism of Injury | Term | Estimate | Standard Error | Statistic | p-Value | 95% Lower Bound | 95% Upper Bound |
|---|---|---|---|---|---|---|---|
| mMVC | (Intercept) | 0.257 | 0.607 | −2.229 | 0.026 | 0.079 | 0.849 |
| mMVC | Age | 0.998 | 0.003 | −0.675 | 0.500 | 0.992 | 1.004 |
| mMVC | Asian | 0.257 | 0.602 | −2.258 | 0.024 | 0.079 | 0.836 |
| mMVC | Black/ African American | 1.102 | 0.607 | 0.157 | 0.875 | 0.335 | 3.618 |
| mMVC | Other | 1.236 | 0.688 | 0.305 | 0.760 | 0.320 | 4.752 |
| mMVC | Unknown | 1.314 | 0.601 | 0.452 | 0.651 | 0.404 | 4.268 |
| PVS | (Intercept) | 0.221 | 0.209 | −7.213 | 0.000 | 0.147 | 0.333 |
| PVS | Age | 1.017 | 0.002 | 7.480 | 0.000 | 1.013 | 1.022 |
| PVS | Asian | 3.415 | 0.199 | 6.172 | 0.000 | 2.312 | 5.043 |
| PVS | Black/ African American | 1.506 | 0.211 | 1.941 | 0.052 | 0.996 | 2.277 |
| PVS | Other | 1.398 | 0.395 | 0.847 | 0.397 | 0.644 | 3.031 |
| PVS | Unknown | 0.728 | 0.199 | −1.595 | 0.111 | 0.493 | 1.075 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baker, M.B.; Sood, H.; Binda, D.D.; Dienes, E.; Nozari, A.; Brahmbhatt, T.S.; Suchdev, K.; Daneshmand, A. Collision Course: A Decade of Traumatic Brain Injury Trends and the Impact of Urban Safety Initiatives in Eastern Massachusetts. J. Clin. Med. 2025, 14, 5825. https://doi.org/10.3390/jcm14165825
Baker MB, Sood H, Binda DD, Dienes E, Nozari A, Brahmbhatt TS, Suchdev K, Daneshmand A. Collision Course: A Decade of Traumatic Brain Injury Trends and the Impact of Urban Safety Initiatives in Eastern Massachusetts. Journal of Clinical Medicine. 2025; 14(16):5825. https://doi.org/10.3390/jcm14165825
Chicago/Turabian StyleBaker, Maxwell B., Himani Sood, Dhanesh D. Binda, Erin Dienes, Ala Nozari, Tejal S. Brahmbhatt, Kushak Suchdev, and Ali Daneshmand. 2025. "Collision Course: A Decade of Traumatic Brain Injury Trends and the Impact of Urban Safety Initiatives in Eastern Massachusetts" Journal of Clinical Medicine 14, no. 16: 5825. https://doi.org/10.3390/jcm14165825
APA StyleBaker, M. B., Sood, H., Binda, D. D., Dienes, E., Nozari, A., Brahmbhatt, T. S., Suchdev, K., & Daneshmand, A. (2025). Collision Course: A Decade of Traumatic Brain Injury Trends and the Impact of Urban Safety Initiatives in Eastern Massachusetts. Journal of Clinical Medicine, 14(16), 5825. https://doi.org/10.3390/jcm14165825







