Association Between the Presence of Missed Canals, Detected Using CBCT, and Post-Treatment Apical Periodontitis in Root-Filled Teeth: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Review Question
2.2. Eligibility Criteria
2.2.1. Inclusion Criteria
2.2.2. Exclusion Criteria
2.3. The Literature Search Strategy and Study Selection
2.4. Data Collection and Extraction Process
2.5. Data Synthesis and Statistical Analysis
2.6. Quality Assessment and Risk of Bias of Individual Studies
- Domain “Sample selection” (maximum = 3 points).
- ○
- Representativeness of the sample: random sampling → two points; non-random sampling or selected group of patients → one point; no explanation of the sampling selection → no points.
- ○
- Sample size: the methods for sample size calculation are provided, or the entire population was enlisted (with a loss rate ≤ 20%) → one point; sample size calculation not provided → no points.
- Domain “Comparability” (maximum = 3 points).
- ○
- Control for quality of root canal treatment: Studies that assessed the quality of root canal fillings or coronal restorations and adjusted for it → one point; not controlling for RCT quality → no points.
- ○
- Control for other confounding factors (tooth type, age/sex): If the study controlled for a second confounding factor → one point; not controlling for other confounding factors: no points.
- ○
- Voxel size of the CBCT: If the analyzed CBCT had a voxel size equal to or smaller than 150 µm → one point; if the analyzed CBCT had a voxel size greater than 150 µm → no points.
- Domain “Outcome” (maximum = 4 points).
- ○
- Evaluation of the outcome: If diagnosis criteria for PAP was specified → one point; PAP was diagnosed without specifying criteria → no points.
- ○
- Number of observers: two or more → one point; only one → no points.
- ○
- CBCT observer experience: If the observer was calibrated and experienced in endodontics → two points; if the observer was not calibrated/or was not experienced in the field of endodontics → one point; if the article did not explain the observer’s calibration or experience → no points.
2.7. Grading Recommendations Assessment, Development, and Evaluation
3. Results
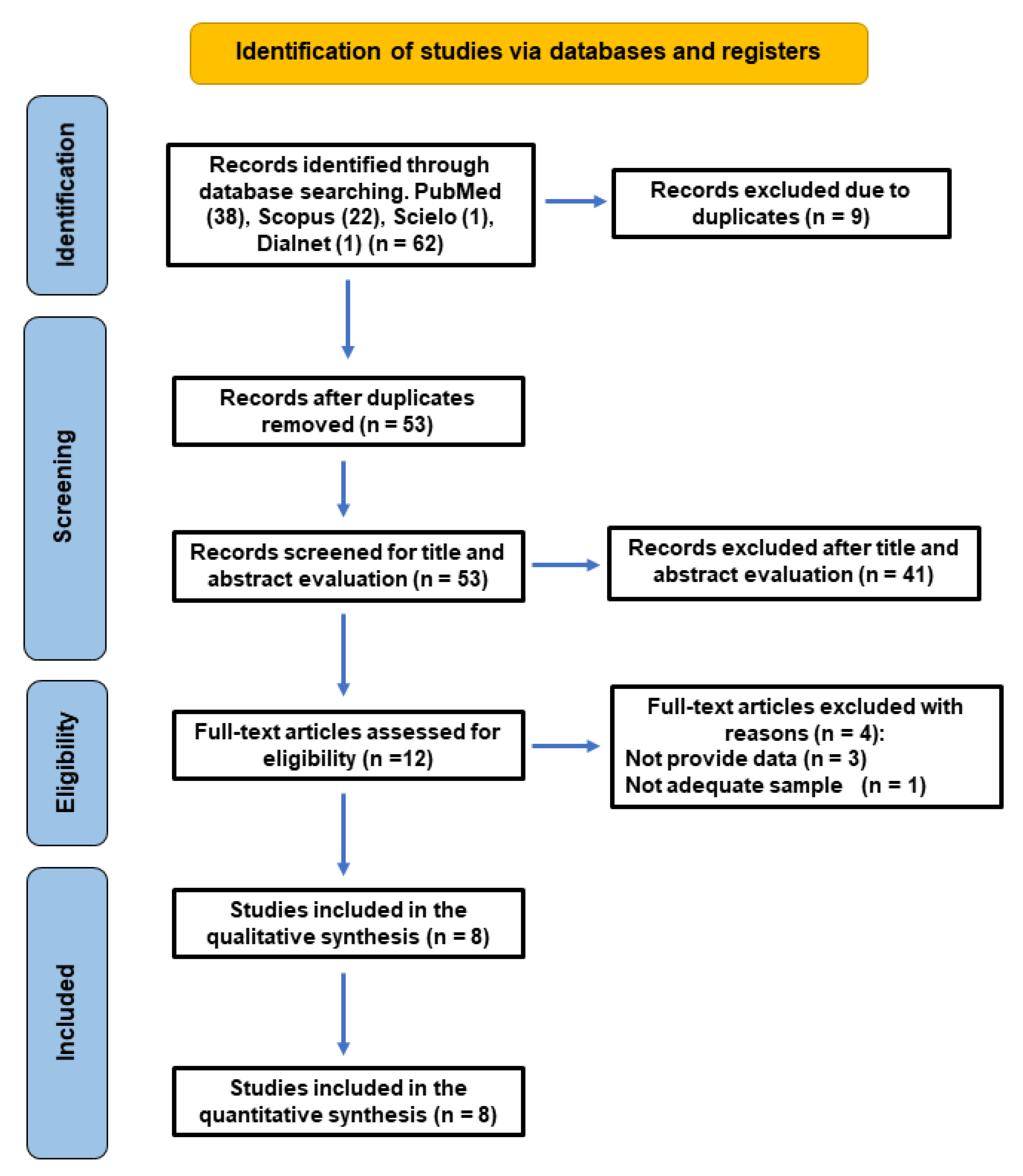
3.1. Study Selection
3.2. Characteristics of the Included Studies
3.3. Data Extracted from the Included Studies
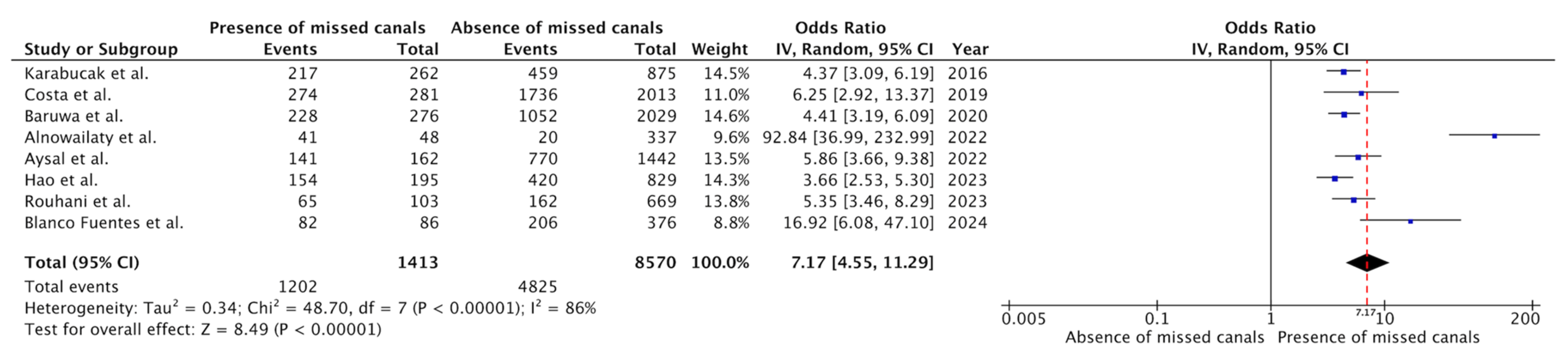
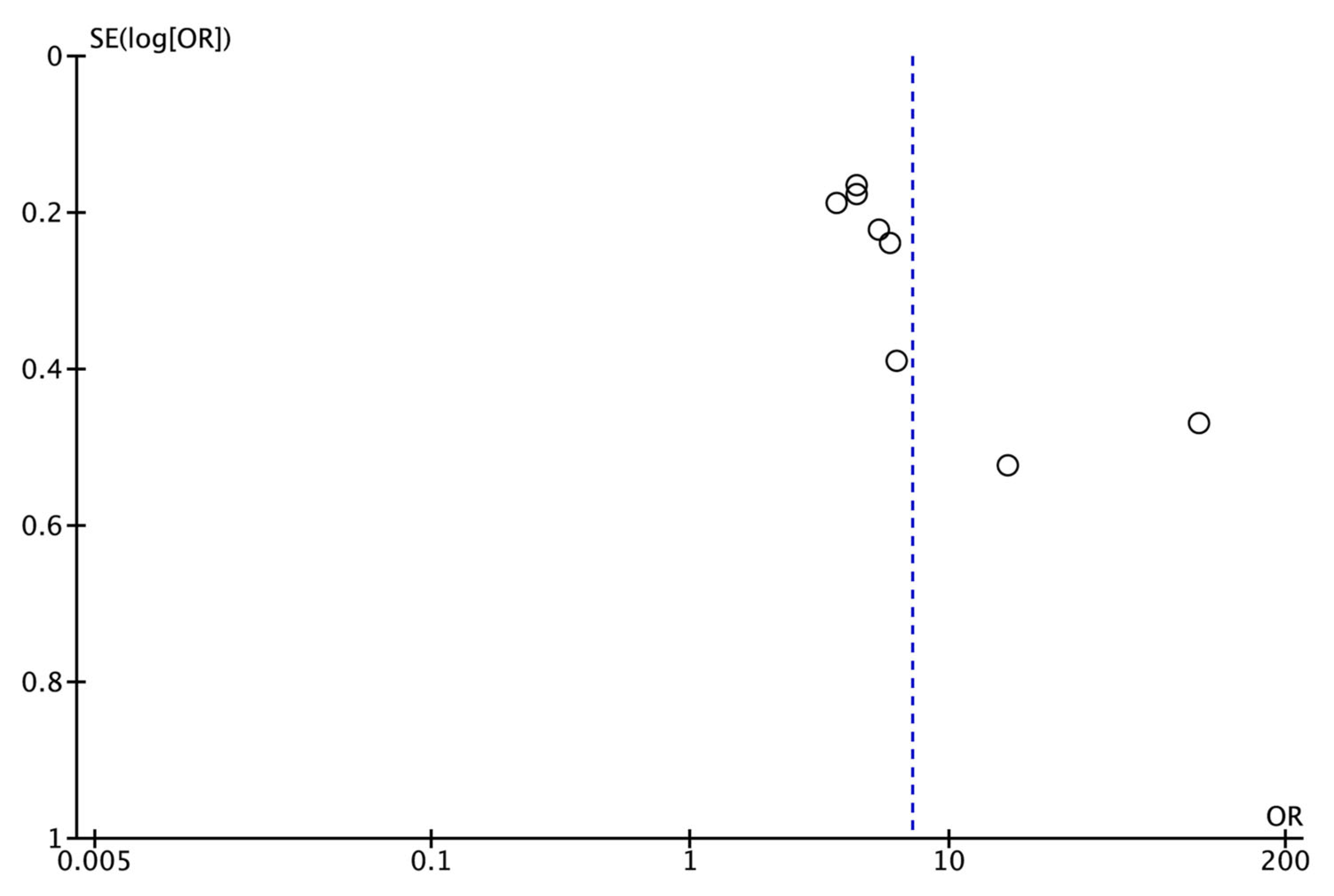
3.4. Meta-Analysis of the Prevalence of Post-Treatment Apical Periodontitis
3.5. Risk of Bias Assessment
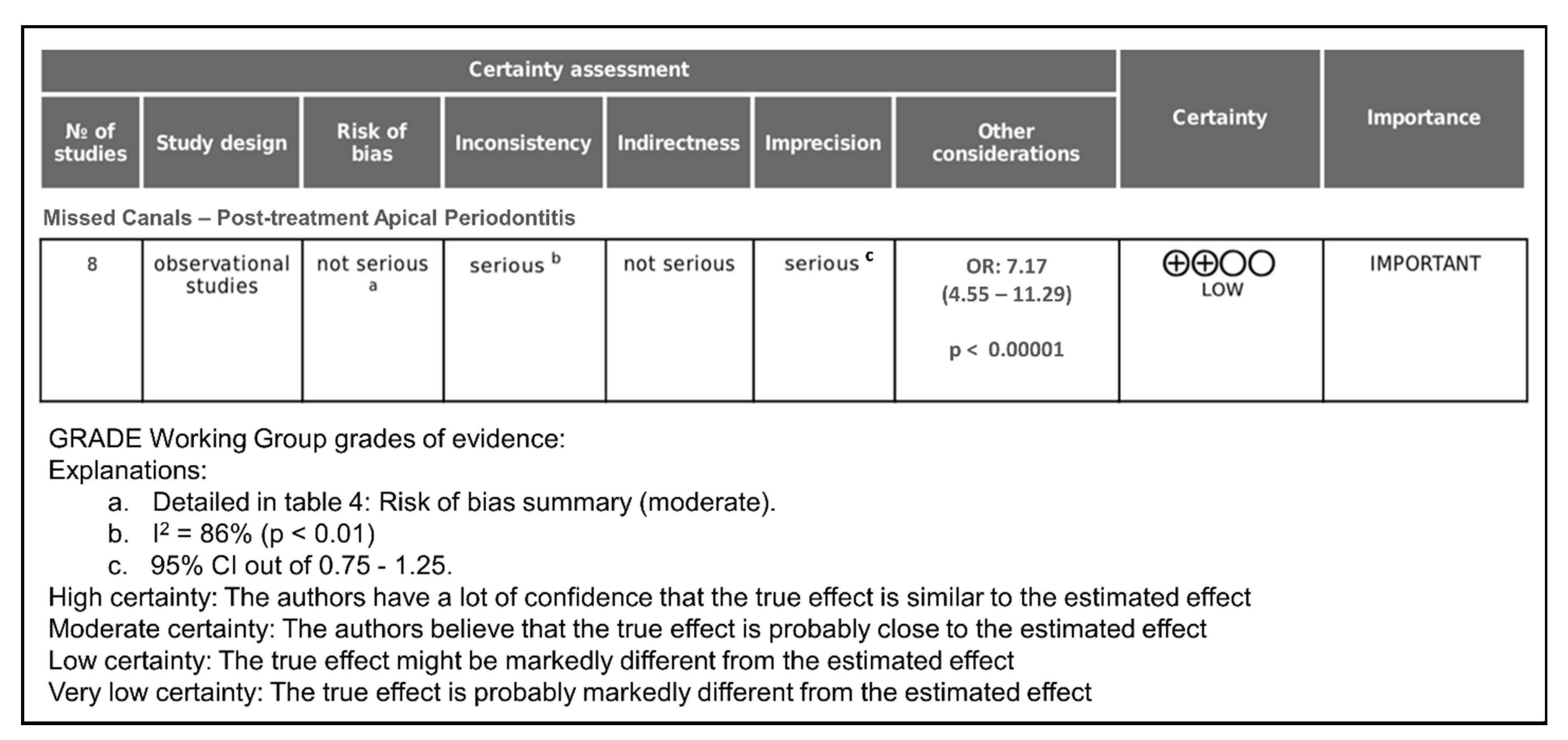
3.6. GRADE Evaluation of Certainty
4. Discussion
4.1. Interpretation of the Main Findings
4.2. Diagnostic Superiority of CBCT
4.3. Anatomical Considerations and Canal Omission
4.4. Quality of Endodontic Treatment
4.5. Methodological Strengths and Limitations
4.6. Comparison with Previous Literature
4.7. Clinical Implications
4.8. Public Health and Educational Impact
4.9. Recommendations for Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ricucci, D.; Siqueira, J.F. Biofilms and apical periodontitis: Study of prevalence and association with clinical and histopathologic findings. J. Endod. 2010, 36, 1277–1288. [Google Scholar] [CrossRef]
- Duncan, H.F.; Kirkevang, L.L.; Peters, O.A.; El-Karim, I.; Krastl, G.; Del Fabbro, M.; Chong, B.S.; Galler, K.M.; Segura-Egea, J.J.; Kebschull, M.; et al. Treatment of pulpal and apical disease: The European Society of Endodontology (ESE) S3-level clinical practice guideline. Int. Endod. J. 2023, 56, 238–295. [Google Scholar] [CrossRef] [PubMed]
- Ricucci, D.; Lin, L.M.; Spångberg, L.S.W. Wound healing of apical tissues after root canal therapy: A long-term clinical, radiographic, and histopathologic observation study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2009, 108, 609–621. [Google Scholar] [CrossRef] [PubMed]
- Tibúrcio-Machado, C.S.; Michelon, C.; Zanatta, F.B.; Gomes, M.S.; Marin, J.A.; Bier, C.A. The global prevalence of apical periodontitis: A systematic review and meta-analysis. Int. Endod. J. 2021, 54, 712–735. [Google Scholar] [CrossRef] [PubMed]
- León-López, M.; Cabanillas-Balsera, D.; Martín-González, J.; Montero-Miralles, P.; Saúco-Márquez, J.J.; Segura-Egea, J.J. Prevalence of root canal treatment worldwide: A systematic review and meta-analysis. Int. Endod. J. 2022, 55, 1105–1127. [Google Scholar] [CrossRef]
- Ricucci, D.; Siqueira, J.F.; Bate, A.L.; Pitt Ford, T.R. Histologic Investigation of Root Canal–treated Teeth with Apical Periodontitis: A Retrospective Study from Twenty-four Patients. J. Endod. 2009, 35, 493–502. [Google Scholar] [CrossRef]
- Provenzano, J.C.; Antunes, H.S.; Alves, F.R.F.; Rôças, I.N.; Alves, W.S.; Silva, M.R.S.; Siqueira, J.F. Host-Bacterial Interactions in Post-treatment Apical Periodontitis: A Metaproteome Analysis. J. Endod. 2016, 42, 880–885. [Google Scholar] [CrossRef]
- Nair, P.N.R. On the causes of persistent apical periodontitis: A review. Int. Endod. J. 2006, 39, 249–281. [Google Scholar] [CrossRef]
- Jiménez-Pinzón, A.; Segura-Egea, J.J.; Poyato-Ferrera, M.; Velasco-Ortega, E.; Ríos-Santos, J.V. Prevalence of apical periodontitis and frequency of root-filled teeth in an adult Spanish population. Int. Endod. J. 2004, 37, 167–173. [Google Scholar] [CrossRef]
- Segura-Egea, J.J.; Martín-González, J.; Cabanillas-Balsera, D.; Fouad, A.F.; Velasco-Ortega, E.; López-López, J. Association between diabetes and the prevalence of radiolucent periapical lesions in root-filled teeth: Systematic review and meta-analysis. Clin. Oral Investig. 2016, 20, 1133–1141. [Google Scholar] [CrossRef]
- Sunay, H.; Tanalp, J.; Dikbas, I.; Bayirli, G. Cross-sectional evaluation of the periapical status and quality of root canal treatment in a selected population of urban Turkish adults. Int. Endod. J. 2007, 40, 139–145. [Google Scholar] [CrossRef]
- Ricucci, D.; Russo, J.; Rutberg, M.; Burleson, J.A.; Spngberg, L.S.W. A prospective cohort study of endodontic treatments of 1,369 root canals: Results after 5 years. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2011, 112, 825–842. [Google Scholar] [CrossRef]
- Siqueira, J.F.; Rôças, I.N. Exploiting molecular methods to explore endodontic infections: Part 1—current molecular technologies for microbiological diagnosis. J. Endod. 2005, 31, 411–423. [Google Scholar] [CrossRef]
- Tavares, P.B.L.; Bonte, E.; Boukpessi, T.; Siqueira, J.F.; Lasfargues, J.J. Prevalence of Apical Periodontitis in Root Canal-Treated Teeth from an Urban French Population: Influence of the Quality of Root Canal Fillings and Coronal Restorations. J. Endod. 2009, 35, 810–813. [Google Scholar] [CrossRef] [PubMed]
- Segura-Egea, J.J.; Cabanillas-Balsera, D.; Martín-González, J.; Cintra, L.T.A. Impact of systemic health on treatment outcomes in endodontics. Int. Endod. J. 2023, 56 (Suppl. 2), 219–235. [Google Scholar] [CrossRef] [PubMed]
- Morsani, J.M.; Aminoshariae, A.; Han, Y.W.; Montagnese, T.A.; Mickel, A. Genetic predisposition to persistent apical periodontitis. J. Endod. 2011, 37, 455–459. [Google Scholar] [CrossRef] [PubMed]
- Eriksen, H.M.; Bjertness, E. Prevalence of apical periodontitis and results of endodontic treatment in middle-aged adults in Norway. Endod. Dent. Traumatol. 1991, 7, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Karabucak, B.; Bunes, A.; Chehoud, C.; Kohli, M.R.; Setzer, F. Prevalence of Apical Periodontitis in Endodontically Treated Premolars and Molars with Untreated Canal: A Cone-beam Computed Tomography Study. J. Endod. 2016, 42, 538–541. [Google Scholar] [CrossRef]
- Costa, F.F.N.P.; Pacheco-Yanes, J.; Siqueira, J.F.; Oliveira, A.C.S.; Gazzaneo, I.; Amorim, C.A.; Santos, P.H.B.; Alves, F.R.F. Association between missed canals and apical periodontitis. Int. Endod. J. 2019, 52, 400–406. [Google Scholar] [CrossRef]
- Huumonen, S.; Suominen, A.L.; Vehkalahti, M.M. Prevalence of apical periodontitis in root filled teeth: Findings from a nationwide survey in Finland. Int. Endod. J. 2017, 50, 229–236. [Google Scholar] [CrossRef]
- Nair, P.N.R. Pathogenesis of Apical Periodontitis and the Causes of Endodontic Failures. Crit. Rev. Oral Biol. Med. 2004, 15, 348–381. [Google Scholar] [CrossRef] [PubMed]
- Dugas, N.N.; Lawrence, H.P.; Teplitsky, P.E.; Pharoah, M.J.; Friedman, S. Periapical health and treatment quality assessment of root-filled teeth in two Canadian populations. Int. Endod. J. 2003, 36, 181–192. [Google Scholar] [CrossRef] [PubMed]
- Lõpez-Lõpez, J.; Jané-Salas, E.; Estrugo-Devesa, A.; Castellanos-Cosano, L.; Martín-González, J.; Velasco-Ortega, E.; Segura-Egea, J.J. Frequency and distribution of root-filled teeth and apical periodontitis in an adult population of Barcelona, Spain. Int. Dent. J. 2012, 62, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Ríos-Santos, J.V.; Ridao-Sacie, C.; Bullón, P.; Fernández-Palacín, A.; Segura-Egea, J.J. Assessment of periapical status: A comparative study using film-based periapical radiographs and digital panoramic images. Med. Oral Patol. Oral Cir. Bucal 2010, 15, 952–956. [Google Scholar] [CrossRef]
- Lupi-Pegurier, L.; Bertrand, M.F.; Muller-Bolla, M.; Rocca, J.P.; Bolla, M. Periapical status, prevalence and quality of endodontic treatment in an adult French population. Int. Endod. J. 2002, 35, 690–697. [Google Scholar] [CrossRef]
- Huumonen, S.; Vehkalahti, M.M.; Nordblad, A. Radiographic assessments on prevalence and technical quality of endodontically-treated teeth in the Finnish population, aged 30 years and older. Acta Odontol. Scand. 2012, 70, 234–240. [Google Scholar] [CrossRef]
- Estrela, C.; Bueno, M.R.; Azevedo, B.C.; Azevedo, J.R.; Pécora, J.D. A new periapical index based on cone beam computed tomography. J. Endod. 2008, 34, 1325–1331. [Google Scholar] [CrossRef]
- Puleio, F.; Lizio, A.S.; Coppini, V.; Lo Giudice, R.; Lo Giudice, G. CBCT-Based assessment of vapor lock effects on endodontic disinfection. Appl. Sci. 2023, 13, 9542. [Google Scholar] [CrossRef]
- Pereira, B.; Martins, J.N.R.; Baruwa, A.O.; Meirinhos, J.; Gouveia, J.; Quaresma, S.A.; Monroe, A.; Ginjeira, A. Association between Endodontically Treated Maxillary and Mandibular Molars with Fused Roots and Periapical Lesions: A Cone-beam Computed Tomography Cross-sectional Study. J. Endod. 2020, 46, 771–777.e1. [Google Scholar] [CrossRef]
- Martins, J.N.R.; Alkhawas, M.B.A.M.; Altaki, Z.; Bellardini, G.; Berti, L.; Boveda, C.; Chaniotis, A.; Flynn, D.; Gonzalez, J.A.; Kottoor, J.; et al. Worldwide Analyses of Maxillary First Molar Second Mesiobuccal Prevalence: A Multicenter Cone-beam Computed Tomographic Study. J. Endod. 2018, 44, 1641–1649.e1. [Google Scholar] [CrossRef]
- Mashyakhy, M.; Hadi, F.A.; Alhazmi, H.A.; Alfaifi, R.A.; Alabsi, F.S.; Bajawi, H.; Alkahtany, M.; AbuMelha, A. Prevalence of Missed Canals and Their Association with Apical Periodontitis in Posterior Endodontically Treated Teeth: A CBCT Study. Int. J. Dent. 2021, 2021, 9962429. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; Estarli, M.; Barrera, E.S.A.; et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Rev. Esp. Nutr. Humana Y Diet. 2016, 20, 148–160. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Herzog, R.; Álvarez-Pasquin, M.J.; Díaz, C.; Del Barrio, J.L.; Estrada, J.M.; Gil, Á. Are healthcare workers intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health 2013, 13, 154–170. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.; Kunz, R.; Brozek, J.; Alonso-Coello, P.; Montori, V.; Akl, E.A.; Djulbegovic, B.; Falck-Ytter, Y.; et al. GRADE guidelines: 4. Rating the quality of evidence—study limitations (risk of bias). J. Clin. Epidemiol. 2011, 64, 407–415. [Google Scholar] [CrossRef]
- Hultcrantz, M.; Rind, D.; Akl, E.A.; Treweek, S.; Mustafa, R.A.; Iorio, A.; Alper, B.S.; Meerpohl, J.J.; Murad, M.H.; Ansari, M.T.; et al. The GRADE Working Group clarifies the construct of certainty of evidence. J. Clin. Epidemiol. 2017, 87, 4–13. [Google Scholar] [CrossRef]
- Meirinhos, J.; Martins, J.N.R.; Pereira, B.; Baruwa, A.O.; Ginjeira, A. Prevalence of Lateral Radiolucency, Apical Root Resorption and Periapical Lesions in Portuguese Patients: A CBCT Cross-Sectional Study with a Worldwide Overview. Eur. Endod. J. 2021, 6, 56–71. [Google Scholar] [CrossRef]
- do Carmo, W.D.; Verner, F.S.; Aguiar, L.M.; Visconti, M.A.; Ferreira, M.D.; Lacerda, M.F.L.S.; Junqueira, R.B. Missed canals in endodontically treated maxillary molars of a Brazilian subpopulation: Prevalence and association with periapical lesion using cone-beam computed tomography. Clin. Oral Investig. 2021, 25, 2317–2323. [Google Scholar] [CrossRef]
- Alotaibi, B.B.; Khan, K.I.; Javed, M.Q.; Dutta, S.D.; Shaikh, S.S.; Almutairi, N.M. Relationship between apical periodontitis and missed canals in mesio-buccal roots of maxillary molars: CBCT study. J. Taibah Univ. Med. Sci. 2023, 19, 18–27. [Google Scholar] [CrossRef]
- Alnowailaty, Y.; Alghamdi, F. Prevalence of Endodontically Treated Premolars and Molars with Untreated Canals and Their Association with Apical Periodontitis Using Cone-Beam Computed Tomography. Cureus 2022, 14, 4–14. [Google Scholar] [CrossRef] [PubMed]
- Baruwa, A.O.; Martins, J.N.R.; Meirinhos, J.; Pereira, B.; Gouveia, J.; Quaresma, S.A.; Monroe, A.; Ginjeira, A. The Influence of Missed Canals on the Prevalence of Periapical Lesions in Endodontically Treated Teeth: A Cross-sectional Study. J. Endod. 2020, 46, 34–39.e1. [Google Scholar] [CrossRef]
- Aysal, Z.; Kocasarac, H.D.; Orhan, K.; Helvacioglu-Yigi, D. Radiological Assessment of Prevalance and Quality of Periapical Status of Endodontic Treatments. Med. Sci. Monit. 2022, 28, e9365691–e93656911. [Google Scholar] [CrossRef] [PubMed]
- Rouhani, A.; Aboutorabzadeh, S.M.R.; Reyhani, M.; Kheirabadi, N.; Mortazavi, S.; Navabi, S. Prevalence of missed canals in endodontically treated teeth: A cone-beam computed tomography study. J. Clin. Exp. Dent. 2023, 15, 605–611. [Google Scholar] [CrossRef] [PubMed]
- Hao, J.; Liu, H.; Shen, Y. Periapical Lesions and Missed Canals in Endodontically Treated Teeth: A Cone-Beam Computed Tomographic Study of a Chinese Subpopulation. Med. Sci. Monit. 2023, 29, e9405331–e9405339. [Google Scholar] [CrossRef]
- Blanco Fuentes, B.Y.; Moreno Monsalve, J.O.; Mesa Herrera, U.; Amoroso-Silva, P.A.; Rodrigues Ferreira Alves, F.; Marceliano-Alves, M.F. Apical periodontitis in endodontically-treated teeth: Association between missed canals and quality of endodontic treatment in a Colombian subpopulation. A cross-sectional study. Acta Odontol. Latinoam. 2024, 37, 59–67. [Google Scholar] [CrossRef]
- Hill, A.B. The environment and disease: Association or causation? Proc. R. Soc. Med. 1965, 58, 295–300. [Google Scholar] [CrossRef]
- Wolcott, J.; Ishley, D.; Kennedy, W.; Johnson, S.; Minnich, S.; Meyers, J. A 5 yr clinical investigation of second mesiobuccal canals in endodontically treated and retreated maxillary molars. J. Endod. 2005, 31, 262–264. [Google Scholar] [CrossRef]
- Peña-Bengoa, F.; Cáceres, C.; Niklander, S.E.; Meléndez, P. Association between second mesiobuccal missed canals and apical periodontitis in maxillary molars of a Chilean subpopulation. J. Clin. Exp. Dent. 2023, 15, e173–e176. [Google Scholar] [CrossRef]
- Studebaker, B.; Hollender, L.; Mancl, L.; Johnson, J.D.; Paranjpe, A. The Incidence of Second Mesiobuccal Canals Located in Maxillary Molars with the Aid of Cone-beam Computed Tomography. J. Endod. 2018, 44, 565–570. [Google Scholar] [CrossRef]
- Ng, Y.-L.L.; Mann, V.; Gulabivala, K. A prospective study of the factors affecting outcomes of non-surgical root canal treatment: Part 2: Tooth survival. Int. Endod. J. 2011, 44, 610–625. [Google Scholar] [CrossRef] [PubMed]
- Burns, L.E.; Kim, J.; Wu, Y.; Alzwaideh, R.; McGowan, R.; Sigurdsson, A. Outcomes of primary root canal therapy: An updated systematic review of longitudinal clinical studies published between 2003 and 2020. Int. Endod. J. 2022, 55, 714–731. [Google Scholar] [CrossRef] [PubMed]
- Siqueira, J.F.; Rôças, I.N.; Ricucci, D.; Hülsmann, M. Causes and management of post-treatment apical periodontitis. Br. Dent. J. 2014, 216, 305–312. [Google Scholar] [CrossRef]
- Witherspoon, D.; Small, J.C.; Regan, J.D. Missed Canal Systems Are the Most Likely Basis for Endodontic Retreatment of Molars—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/23930451/ (accessed on 11 June 2025).
- Siqueira, J.F.; Rôças, I.N.; Alves, F.R.F.; Campos, L.C. Periradicular status related to the quality of coronal restorations and root canal fillings in a Brazilian population. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2005, 100, 369–374. [Google Scholar] [CrossRef] [PubMed]
- Chugal, N.M.; Clive, J.M.; Spångberg, L.S.W. Endodontic infection: Some biologic and treatment factors associated with outcome. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2003, 96, 81–90. [Google Scholar] [CrossRef]
- Jakovljevic, A.; Nikolic, N.; Jacimovic, J.; Pavlovic, O.; Milicic, B.; Beljic-Ivanovic, K.; Miletic, M.; Andric, M.; Milasin, J. Prevalence of Apical Periodontitis and Conventional Nonsurgical Root Canal Treatment in General Adult Population: An Updated Systematic Review and Meta-analysis of Cross-sectional Studies Published between 2012 and 2020. J. Endod. 2020, 46, 1371–1386.e8. [Google Scholar] [CrossRef]
- Jang, Y.E.; Kim, Y.; Kim, S.Y.; Kim, B.S. Predicting early endodontic treatment failure following primary root canal treatment. BMC Oral Health 2024, 24, 327–336. [Google Scholar] [CrossRef]
| Authors and Year | Country | Study Type | Sample (%) | Types of Included RFT | Prevalence of PAP in RFT (%) | Presence of Missed Canals (%) | CBCT Voxel Size |
|---|---|---|---|---|---|---|---|
| Karabucak et al., 2016 [18] | USA | Cross-sectional | 655 patients 1137 RFT | Molar and premolar | 59.5 * | Maxillary molars (40.1) Maxillary premolars (9.5) | 76 µm |
| Costa et al., 2019 [19] | Brazil | Cross-sectional | 764 patients 2294 RFT Men (37) Women (63) | All | 87.6 * | Maxillary molars (57) Mandibular molars (26) Maxillary premolars (10) Mandibular premolars (6) | 200 µm |
| Baruwa et al., 2020 [42] | Portugal | Cross-sectional | 1160 patients 2305 RFT Men (43) Women (57) | All | 55.5 * | Maxillary 1st molars (59.5) Maxillary 2nd molars (40) Mandibular 1st molars (11.2) Mandibular 2nd molars (9.5) | ≤200 µm |
| Alnowailaty & Alghamdi et al., 2022 [41] | Saudi Arabia | Cross-sectional | 300 patients 385 RFT Men (50) Women (50) | Molar and premolar | 15.8 * | Maxillary teeth (26) Mandibular teeth (22) Maxillary 2nd molars (38.1) | 125 µm |
| Aysal et al., 2022 [43] | Turkey | Cross-sectional | 1069 patients 1604 RFT Men (51) Women (49) | All | 56.8 * | Teeth without apical lesions (3) Teeth with apical lesions (15.5) | ≤200 µm |
| Hao et al., 2023 [45] | China | Cross-sectional | 561 patients 1024 RFT Men (35) Women (65) | Molar and premolar | 56.1 * | Maxillary 1st molars (65.7) Mandibular 1st molars (16.4) Mandibular 2nd molars (11.7) Maxillary 2nd molars (10.3) | 200 µm |
| Rouhani et al., 2023 [44] | Iran | Cross-sectional | 298 patients 772 RFT Men (46) Women (54) | Molar | 29.4 * | Maxillary 1st molars (56) Maxillary 2nd molars (14) Mandibular 1st molars (10) | 160 µm |
| Blanco Fuentes et al., 2024 [46] | Colombia | Cross-sectional | 318 patients 462 RFT Men (40) Women (60) | All | 62.3 ** | Maxillary 1st molars (61.9) Maxillary 2nd molars (41.1) Mandibular 1st molars (18.8) | 125 or 200 µm |
| Authors and Year | RFT (No.) | Presence of Missed Canals | Absence of Missed Canals | Odds Ratio (95% CI) | p | ||
|---|---|---|---|---|---|---|---|
| RFT | Prevalence of PAP (%) | RFT | Prevalence of PAP (%) | ||||
| Karabucak et al., 2016 [18] | 1137 | 262 | 217 (82.8) | 875 | 459 (52.5) | 4.37 (3.1–6.2) | <0.01 |
| Costa et al., 2019 [19] | 2294 | 281 | 274 (97.5) | 2013 | 1736 (86.2) | 6.25 (2.9–13.4) | <0.01 |
| Baruwa et al., 2020 [42] | 2305 | 276 | 228 (82.6) | 2029 | 1052 (51.8) | 4.41 (3.2–6.1) | <0.01 |
| Alnowailaty & Alghamdi et al., 2022 [41] | 385 | 48 | 41 (85.4) | 337 | 20 (5.9) | 92.84 (37.0–233.0) | <0.01 |
| Aysal et al., 2022 [43] | 1604 | 162 | 141 (87.0) | 1442 | 770 (53.4) | 5.86 (3.7–9.4) | <0.01 |
| Hao et al., 2023 [45] | 1024 | 195 | 154 (79.0) | 829 | 420 (50.7) | 3.66 (2.5–5.3) | <0.01 |
| Rouhani et al., 2023 [44] | 772 | 103 | 65 (63.1) | 669 | 162 (24.2) | 5.35 (3.5–8.3) | <0.01 |
| Blanco Fuentes et al., 2024 [46] | 462 | 86 | 82 (95.3) | 376 | 206 (54.8) | 16.92 (6.1–47.1) | <0.01 |
| Overall | 9983 | 1413 | 1202 (85.1) | 8570 | 4825 (56.3) | ||
| Author and Year | Sample Selection | Comparability | Outcome | Risk of Bias | |||||
|---|---|---|---|---|---|---|---|---|---|
| Sample Representativeness | Sample Size | Control for RCT Quality | Control for Other Confounding Factors | Voxel Size | Criteria for PAP Diagnosis | No. Observers | CBCT Observer Experience | ||
| Karabucak et al., 2016 [18] | * | - | - | - | * | * | * | * | 5 Moderate |
| Costa et al., 2019 [19] | * | - | - | - | - | * | * | ** | 5 Moderate |
| Baruwa et al., 2020 [42] | * | - | * | * | - | * | * | ** | 7 Moderate |
| Alnowailaty & Alghamdi et al., 2022 [41] | * | - | - | - | * | * | * | ** | 6 Moderate |
| Aysal et al., 2022 [43] | * | - | - | - | - | * | * | * | 4 Moderate |
| Hao et al., 2023 [45] | * | - | - | - | - | * | * | * | 4 Moderate |
| Rouhani et al., 2023 [44] | * | - | - | - | - | * | * | * | 4 Moderate |
| Blanco Fuentes et al., 2024 [46] | * | - | * | * | * | * | * | ** | 8 Low |
| OVERALL | 8 | 0 | 2 | 2 | 3 | 8 | 8 | 12 | 43/80 Moderate |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
León-López, M.; Montero-Miralles, P.; Cabanillas-Balsera, D.; Saúco-Márquez, J.J.; Martín-González, J.; Segura-Egea, J.J. Association Between the Presence of Missed Canals, Detected Using CBCT, and Post-Treatment Apical Periodontitis in Root-Filled Teeth: A Systematic Review and Meta-Analysis. J. Clin. Med. 2025, 14, 5781. https://doi.org/10.3390/jcm14165781
León-López M, Montero-Miralles P, Cabanillas-Balsera D, Saúco-Márquez JJ, Martín-González J, Segura-Egea JJ. Association Between the Presence of Missed Canals, Detected Using CBCT, and Post-Treatment Apical Periodontitis in Root-Filled Teeth: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2025; 14(16):5781. https://doi.org/10.3390/jcm14165781
Chicago/Turabian StyleLeón-López, María, Paloma Montero-Miralles, Daniel Cabanillas-Balsera, Juan J. Saúco-Márquez, Jenifer Martín-González, and Juan J. Segura-Egea. 2025. "Association Between the Presence of Missed Canals, Detected Using CBCT, and Post-Treatment Apical Periodontitis in Root-Filled Teeth: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 14, no. 16: 5781. https://doi.org/10.3390/jcm14165781
APA StyleLeón-López, M., Montero-Miralles, P., Cabanillas-Balsera, D., Saúco-Márquez, J. J., Martín-González, J., & Segura-Egea, J. J. (2025). Association Between the Presence of Missed Canals, Detected Using CBCT, and Post-Treatment Apical Periodontitis in Root-Filled Teeth: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 14(16), 5781. https://doi.org/10.3390/jcm14165781








