Effect of Orthodontic Movement on the Periapical Healing of Teeth Undergone Endodontic Root Canal Treatment: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Information Sources and Search Strategy
2.3. Study Eligibility Criteria
- Population: Living humans or animals with endodontically treated teeth.
- Intervention: Orthodontic tooth movement.
- Comparison: Controls (no orthodontic tooth movement or baseline status).
- Outcome: Periapical healing status (radiographic/histologic).
- Studies of living humans or animals examining the influence of orthodontic tooth movement on the periapical healing of teeth undergone root canal treatment/retreatment.
- Success of root canal treatment is based on clinical and/or radiographic criteria (strict = absence of apical radiolucency; loose = reduction in size of radiolucency).
- Overall success rate was assessed or could be calculated from the raw data.
- Studies investigating the influence of orthodontic tooth movement on root resorption or endodontically teeth with a trauma history.
- Other types of publications, include case reports/series, abstracts, reviews, editorials, letters to editors, and author opinion papers.
- Studies written in a language other than English.
2.4. Study Selection
2.5. Quality Assessment and Data Extraction
3. Results
3.1. Study Characteristics
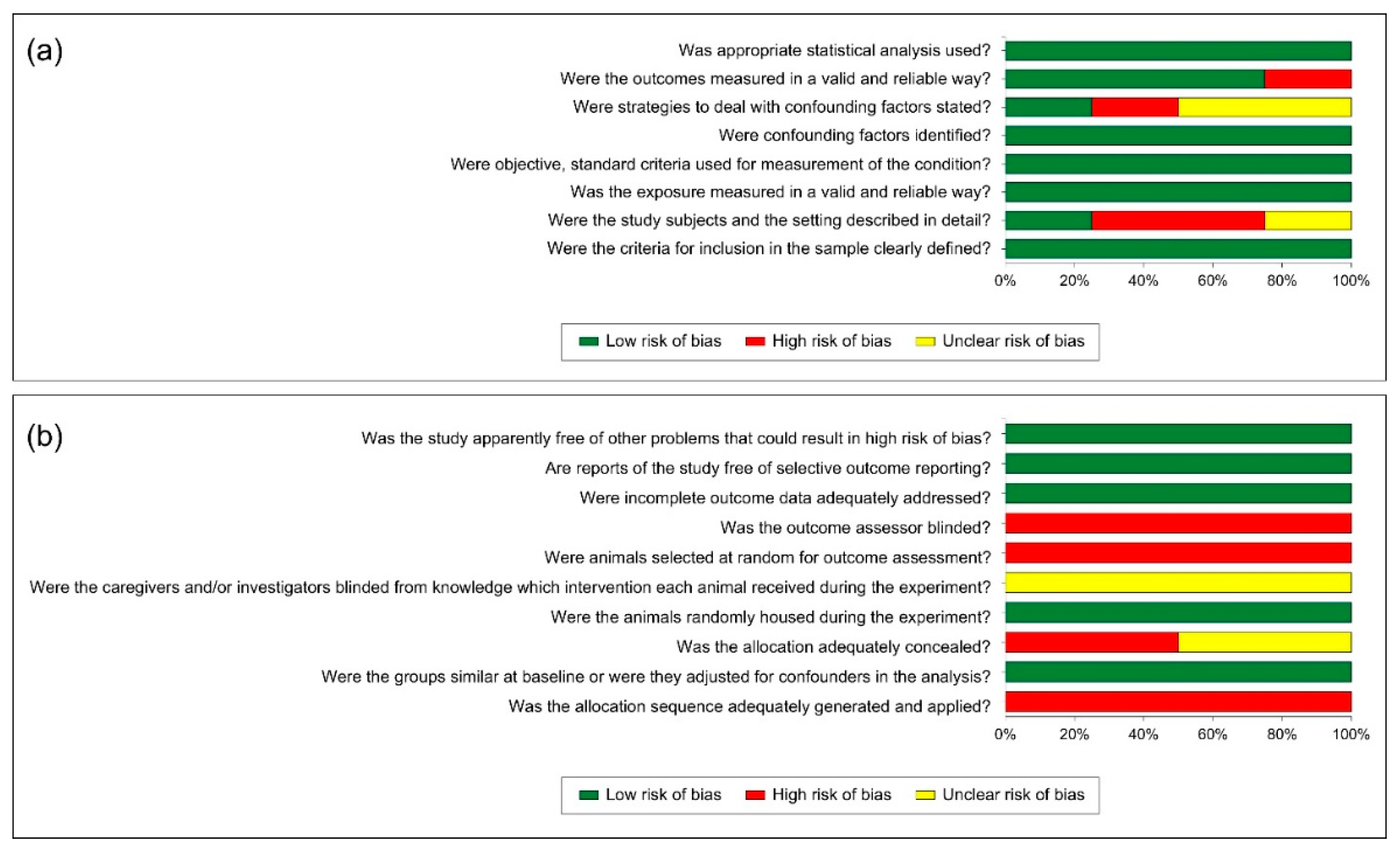
3.2. Study Quality Assessment
3.3. The Outcome of the Included Studies
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. The List of the Excluded Studies Based on the Full Text Assessment with the Reasons of Exclusion
| No. | Citation | Reason of Exclusion |
| 1 | Ozalp, S. O., Tuncer, B. B., Tulunoglu, O., & Akkaya, S. (2008). Endodontic and orthodontic treatment of fused maxillary central incisors: a case report. Dental Traumatology, 24(5). https://doi.org/10.1111/j.1600-9657.2008.00635.x | Endodontically treated teeth with a trauma history |
| 2 | Wickwire, N. A., Mc Neil, M. H., Norton, L. A., & Duell, R. C. (1974). The effects of tooth movement upon endodontically treated teeth. The Angle Orthodontist, 44(3), 235–242. https://doi.org/10.1043/0003-3219(1974)044<0235:TEOTMU>2.0.CO;2 | Endodontically treated teeth with a trauma history |
| 3 | Yoshpe, M., Kaufman, A. Y., & Einy, S. (2025). Effect of orthodontic treatment on traumatized teeth treated by regenerative endodontic procedure. Angle Orthodontist, 95(2), 173–178. https://research.ebsco.com/linkprocessor/plink?id=68e5503f-1cd7-37b0-92a2-2a316866ebe0 | Endodontically treated teeth with a trauma history |
| 4 | Singh, M., & Kaur, P. (1990). Temporary endodontics during active orthodontics. Journal of the Indian Dental Association, 61(12), 279, 281, 283. http://www.ncbi.nlm.nih.gov/pubmed/2130099 | Case report/series |
| 5 | Smidt, A., & Keinan, D. (2021). Accelerated healing of endodontically treated teeth with a periapical lesion as a result of orthodontic extrusion: evaluation and rationale. Quintessence International (Berlin, Germany : 1985), 53(1), 16–22. https://doi.org/10.3290/j.qi.b2091197 | Case report/series |
| 6 | Suda, N., Kawafuji, A., & Moriyama, K. (2009). Multidisciplinary management including endodontics, periodontics, orthodontics, anterior maxillary osteotomy and prosthetics in an adult case with a severe openbite. Orthodontic Waves, 68(1), 42–49. https://doi.org/10.1016/j.odw.2008.10.002 | Case report/series |
| 7 | Vieyra, J. P. (2018). Nonsurgical orthodontic-endodontic treatment of a maxillary central incisor diagnosed with infected dens invaginatus (Oehlers’ type III) and associated apical periodontitis. Endodontic Practice Today, 12(1), 43-43. | Case report/series |
| 8 | Alharbi, M. (2020). Long-term Follow-up for Immature Teeth Treated with Regenerative Endodontic Procedures and Underwent Orthodontic Treatment. European Endodontic Journal. https://doi.org/10.14744/eej.2020.29591 | Case report/series |
| 9 | Jawad, Z., Bates, C., Duggal, M., & Nazzal, H. (2018). Orthodontic management of a non-vital immature tooth treated with regenerative endodontics: a case report. Journal of Orthodontics, 45(4), 289–295. https://doi.org/10.1080/14653125.2018.1501935 | Case report/series |
| 10 | Yeap, C. W. (2023). Endodontic treatment of an immature maxillary lateral incisor with type II dens invaginatus in an orthodontic patient: A case report: The Bulletin of the Australian Society of Endodontology. Australian Endodontic Journal, 49(2), 373–379. https://doi.org/10.1111/aej.12653 | Case report/series |
| 11 | Liu, H., Hao, J., & Shen, Y. (2024). Partial regression of a healed periapical lesion in an endodontically treated premolar during orthodontic extrusion: A case report. Journal of Dental Sciences, 19(3), 1894–1896. https://research.ebsco.com/linkprocessor/plink?id=5a823c96-b48b-3117-9a79-7890668ea0c7 | Case report/series |
| 12 | Mendonca, M. R., Holland, R., & Almeida, M. H. C. (2000). Effects of orthodontic force on tooth endodontically treated. Journal of Dental Research, 79(5), 1141-1141. | Conference abstract |
| 13 | Consolaro, A., & Consolaro, R. B. (2013). Orthodontic movement of endodontically treated teeth. Dental Press Journal of Orthodontics, 18(4), 2–7. https://doi.org/10.1590/S2176-94512013000400002 | Literature review |
| 14 | Chaniotis, A. (2018). Orthodontic Movement after Regenerative Endodontic Procedure: Case Report and Long-term Observations. Journal of Endodontics, 44(3), 432–437. https://doi.org/10.1016/j.joen.2017.11.008 | Endodontically treated teeth with a trauma history |
| 15 | Natera, M., & Mukherjee, P. M. (2018). Regenerative Endodontic Treatment with Orthodontic Treatment in a Tooth with Dens Evaginatus: A Case Report with a 4-year Follow-up. Journal of Endodontics, 44(6), 952–955. https://doi.org/10.1016/j.joen.2018.01.011 | Case report/series |
| 16 | Chaniotis, A., & Chanioti, A. (2022). Long-term Complications of Previously Successful Regenerative Endodontic Procedures after Orthodontic Movement: A Report of 3 Different Complications after 4, 8, and 11 Years. Journal of Endodontics, 48(7), 951–960. https://doi.org/10.1016/j.joen.2022.04.002 | Case report/series |
| 17 | Keinan, D., Szwec, J., Matas, A., Moshonov, J., & Yitschaky, O. (2013). Applying extrusive orthodontic force without compromising the obturated canal space. The Journal of the American Dental Association, 144(8), 910–913. https://doi.org/10.14219/jada.archive.2013.0208 | Case report/series |
| 18 | Asnani, M. M., Jalaluddin, M., Goyal, V., Naqvi, Z. A., Gupta, B., & Sonigra, H. M. (2017). Assessment of the Effect of Orthodontic Treatment on the Periodontal Health of Endodontically Restored Tooth. The Journal of Contemporary Dental Practice, 18(7), 587–590. https://doi.org/10.5005/jp-journals-10024-2089 | Periodontal health not periapical health was assessed |
| 19 | Reddy, H., Singh, N., Vaghela, J., Sharma, S., Sachdeva, S. & Mishra, S. S. (2023). Effect Of Orthodontic Treatment On Endodontically Treated Tooth: A Clinical Study. Journal of Pharmaceutical Negative Results; 14 (2), 1338–1341. | Poor study quality outcome |
| 20 | Bud, E., Păcurar, M., Vlasa, A., Bica, C., Martha, K., Eșian, D., Bukhari, C., Lazăr, L., & Bud, A. (2021). Cone Beam Computed Tomography Study on the Incidence of Endodontic Filling Biomaterials Resorption in Patients With/Without Orthodontic Treatment. Journal of Interdisciplinary Medicine, 6(2), 103–107. https://doi.org/10.2478/jim-2021-0023 | Not related to research objectives |
| 21 | De Souza, R. S., De Souza, V., Holland, R., Gomes—Filho, J. E., Murata, S. S., & Sonoda, C. K. (2009). Effect of calcium hydroxide—based materials on periapical tissue healing and orthodontic root resorption of endodontically treated teeth in dogs. Dental Traumatology, 25(2), 213–218. https://doi.org/10.1111/j.1600-9657.2008.00758.x | Not related to research objectives |
| 22 | Asgary, S., & Talebzadeh, B. (2023). Impact of Orthodontic Treatment on Regenerative Endodontics in Immature Teeth: A Long-Term Case Study. CUREUS JOURNAL OF MEDICAL SCIENCE, 15(10). https://doi.org/10.7759/cureus.46953 | Not related to research objectives |
| 23 | Mah, R., Holland, G. R., & Pehowich, E. (1996). Periapical changes after orthodontic movement of root-filled ferret canines. Journal of endodontics, 22(6), 298–303. https://doi.org/10.1016/S0099-2399(96)80263-9 | The lesion size was compered only with or without orthodontic tooth movement in vital or non-vital teeth, however, no results were reported on the changes in periapical lesion size after ortho treatment. |
References
- Zhao, D.; Xue, K.; Meng, J.; Hu, M.; Bi, F.; Tan, X. Orthodontically induced external apical root resorption considerations of root-filled teeth vs vital pulp teeth: A systematic review and meta-analysis. BMC Oral Health 2023, 23, 241. [Google Scholar] [CrossRef]
- Duarte, P.H.M.; Weissheimer, T.; Michel, C.H.T.; Só, G.B.; da Rosa, R.A.; Só, M.V.R. Do orthodontic movements of traumatized teeth induce dental pulp necrosis? A systematic review. Clin. Oral Investig. 2023, 27, 4117–4129. [Google Scholar] [CrossRef]
- von Böhl, M.; Ren, Y.; Fudalej, P.S.; Kuijpers-Jagtman, A.M. Pulpal reactions to orthodontic force application in humans: A systematic review. J. Endod. 2012, 38, 1463–1469. [Google Scholar] [CrossRef] [PubMed]
- Huokuna, J.; Loimaranta, V.; Laine, M.A.; Svedström-Oristo, A.L. Adverse effects of orthodontic forces on dental pulp. Appearance and character. A systematic review. Acta Odontol. Scand. 2023, 81, 267–277. [Google Scholar] [CrossRef] [PubMed]
- Ioannidou-Marathiotou, I.; Zafeiriadis, A.A.; Papadopoulos, M.A. Root resorption of endodontically treated teeth following orthodontic treatment: A meta-analysis. Clin. Oral Investig. 2013, 17, 1733–1744. [Google Scholar] [CrossRef] [PubMed]
- Konno, Y.; Daimaruya, T.; Iikubo, M.; Kanzaki, R.; Takahashi, I.; Sugawara, J.; Sasano, T. Morphologic and hemodynamic analysis of dental pulp in dogs after molar intrusion with the skeletal anchorage system. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 199–207. [Google Scholar] [CrossRef]
- Baranowskyj, G.R. A histologic investigation of tissue response to an orthodontic intrusive force on a dog maxillary incisor with endodontic treatment and root resection. Am. J. Orthod. 1969, 56, 623–624. [Google Scholar] [CrossRef]
- de Souza, R.S.; Gandini, L.G., Jr.; de Souza, V.; Holland, R.; Dezan, E., Jr. Influence of orthodontic dental movement on the healing process of teeth with periapical lesions. J. Endod. 2006, 32, 115–119. [Google Scholar] [CrossRef]
- Alqerban, A.; Almanea, A.; Alkanhal, A.; Aljarbou, F.; Almassen, M.; Fieuws, S.; Willems, G. Impact of orthodontic treatment on the integrity of endodontically treated teeth. Eur. J. Orthod. 2019, 41, 238–243. [Google Scholar] [CrossRef]
- Mah, R.; Holland, G.R.; Pehowich, E. Periapical changes after orthodontic movement of root-filled ferret canines. J. Endod. 1996, 22, 298–303. [Google Scholar] [CrossRef]
- Kim, S.; Hwang, S.J.; Seo, M.S. Effect of orthodontic treatment on the periapical radiolucency of endodontically treated teeth: A CBCT analysis. BMC Oral Health 2023, 23, 289. [Google Scholar] [CrossRef]
- Estrela, C.; Bueno, M.R.; Leles, C.R.; Azevedo, B.; Azevedo, J.R. Accuracy of cone beam computed tomography and panoramic and periapical radiography for detection of apical periodontitis. J. Endod. 2008, 34, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Jakovljevic, A.; Nikolic, N.; Jacimovic, J.; Pavlovic, O.; Milicic, B.; Beljic-Ivanovic, K.; Miletic, M.; Andric, M.; Milasin, J. Prevalence of Apical Periodontitis and Conventional Nonsurgical Root Canal Treatment in General Adult Population: An Updated Systematic Review and Meta-analysis of Cross-sectional Studies Published between 2012 and 2020. J. Endod. 2020, 46, 1371–1386.e8. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Moola, S.; Munn, Z.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetcu, R.; Currie, M.; Lisy, K.; Qureshi, R.; Mattis, P.; et al. Systematic reviews of etiology and risk. In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; JBI: Adelaide, South Australia, 2020; Available online: https://synthesismanual.jbi.global (accessed on 20 March 2025).
- Hooijmans, C.R.; Rovers, M.M.; de Vries, R.B.; Leenaars, M.; Ritskes-Hoitinga, M.; Langendam, M.W. SYRCLE’s risk of bias tool for animal studies. BMC Med. Res. Methodol. 2014, 14, 43. [Google Scholar] [CrossRef]
- Ianos, I.; Bucur, S.M.; Todor, I.; Dinu, Ș.; Nuca, C.; Botond, F.; Păcurar, M. Effects of orthodontic treatment on periapical health in endodontically treated teeth. Rom. J. Oral Rehabil. 2024, 16, 35–40. [Google Scholar] [CrossRef]
- Chen, X.; Liu, S.Q.; Wang, X.X.; Liu, W.; Zhou, X.; Wang, X. Effect of Orthodontic Treatment on the Outcomes of Endodontically Treated Teeth: A Cone-Beam Computed Tomography Analysis. J. Endod. 2024, 50, 1091–1099. [Google Scholar] [CrossRef]
- Estrela, C.; Bueno, M.R.; Azevedo, B.C.; Azevedo, J.R.; Pécora, J.D. A new periapical index based on cone beam computed tomography. J. Endod. 2008, 34, 1325–1331. [Google Scholar] [CrossRef]
- Firth, F.A.; Farrar, R.; Farella, M. Investigating orthodontic tooth movement: Challenges and future directions. J. R. Soc. N. Z. 2020, 50, 67–79. [Google Scholar] [CrossRef]
- Krishnan, V.; Davidovitch, Z. Cellular, molecular, and tissue-level reactions to orthodontic force. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 469.e1–469.e32. [Google Scholar] [CrossRef]
- Consolaro, A.; Consolaro, R.B. Orthodontic movement of endodontically treated teeth. Dent. Press J. Orthod. 2013, 18, 2–7. [Google Scholar] [CrossRef]
- Forsberg, J.; Halse, A. Radiographic simulation of a periapical lesion comparing the paralleling and the bisecting-angle techniques. Int. Endod. J. 1994, 27, 133–138. [Google Scholar] [CrossRef] [PubMed]
- Michetti, J.; Maret, D.; Mallet, J.P.; Diemer, F. Validation of cone beam computed tomography as a tool to explore root canal anatomy. J. Endod. 2010, 36, 1187–1190. [Google Scholar] [CrossRef] [PubMed]
- Ríos-Santos, J.V.; Ridao-Sacie, C.; Bullón, P.; Fernández-Palacín, A.; Segura-Egea, J.J. Assessment of periapical status: A comparative study using film-based periapical radiographs and digital panoramic images. Med. Oral Patol. Oral Cir. Bucal 2010, 15, e952–e956. [Google Scholar] [CrossRef] [PubMed]
- Gliga, A.; Imre, M.; Grandini, S.; Marruganti, C.; Gaeta, C.; Bodnar, D.; Dimitriu, B.A.; Foschi, F. The Limitations of Periapical X-ray Assessment in Endodontic Diagnosis-A Systematic Review. J. Clin. Med. 2023, 12, 4647. [Google Scholar] [CrossRef]
- Yen, M.; Yeung, A.W.K. The Performance of Paralleling Technique and Bisecting Angle Technique for Taking Periapical Radiographs: A Systematic Review. Dent. J. 2023, 11, 155. [Google Scholar] [CrossRef]
- Special Committee to Revise the Joint AAE/AAOMR Position Statement on use of CBCT in Endodontics. AAE and AAOMR Joint Position Statement: Use of Cone Beam Computed Tomography in Endodontics 2015 Update. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2015, 120, 508–512. [Google Scholar] [CrossRef]
- Ng, Y.L.; Mann, V.; Gulabivala, K. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: Part 1: Periapical health. Int. Endod. J. 2011, 44, 583–609. [Google Scholar] [CrossRef]
- Ray, H.A.; Trope, M. Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration. Int. Endod. J. 1995, 28, 12–18. [Google Scholar] [CrossRef]
- Schaeffer, M.A.; White, R.R.; Walton, R.E. Determining the optimal obturation length: A meta-analysis of literature. J. Endod. 2005, 31, 271–274. [Google Scholar] [CrossRef]
- Ng, Y.L.; Mann, V.; Rahbaran, S.; Lewsey, J.; Gulabivala, K. Outcome of primary root canal treatment: Systematic review of the literature—Part 2. Influence of clinical factors. Int. Endod. J. 2008, 41, 6–31. [Google Scholar] [CrossRef] [PubMed]
- Benenati, F.W.; Khajotia, S.S. A radiographic recall evaluation of 894 endodontic cases treated in a dental school setting. J. Endod. 2002, 28, 391–395. [Google Scholar] [CrossRef]
- Park, D.M.; Seok, W.H.; Yoon, J.Y. Factors Influencing Non-Surgical Root Canal Treatment Outcomes in Mandibular Second Molars: A Retrospective Cone-Beam Computed Tomography Analysis. J. Clin. Med. 2024, 13, 2931. [Google Scholar] [CrossRef]
- Löst, C. Quality guidelines for endodontic treatment: Consensus report of the European Society of Endodontology. Int. Endod. J. 2006, 39, 921–930. [Google Scholar] [CrossRef]
- Currell, S.D.; Liaw, A.; Blackmore Grant, P.D.; Esterman, A.; Nimmo, A. Orthodontic mechanotherapies and their influence on external root resorption: A systematic review. Am. J. Orthod. Dentofac. Orthop. 2019, 155, 313–329. [Google Scholar] [CrossRef]
- Perry, J.; Popat, H.; Johnson, I.; Farnell, D.; Morgan, M.Z. Professional consensus on orthodontic risks: What orthodontists should tell their patients. Am. J. Orthod. Dentofac. Orthop. 2021, 159, 41–52. [Google Scholar] [CrossRef]
- Heboyan, A.; Avetisyan, A.; Karobari, M.I.; Marya, A.; Khurshid, Z.; Rokaya, D.; Zafar, M.S.; Fernandes, G.V.O. Tooth root resorption: A review. Sci. Prog. 2022, 105, 368504221109217. [Google Scholar] [CrossRef]

| PubMed |
| ((Orthodontics, Corrective * [MeSH Terms]) OR (Orthodontic * [Title/Abstract] OR Tooth movement [Title/Abstract])) AND ((Apical periodontitis [Title/Abstract] OR Periapical periodontitis [Title/Abstract] OR Apical lesion * [Title/Abstract] OR Periapical lesion * [Title/Abstract] OR Root-filled tooth [Title/Abstract] OR Root-filled teeth [Title/Abstract] OR Root canal treatment [Title/Abstract] OR Endodontic * [Title/Abstract] OR Periapical abscess [Title/Abstract] OR Apical abscess [Title/Abstract] OR Periapical cyst * [Title/Abstract] OR Apical cyst * [Title/Abstract]) OR (Periapical Periodontitis/physiopathology * OR Periapical Periodontitis * OR Root Canal Therapy OR Root Canal Obturation)) |
| Web of Science Core Collection |
| (TS = (Orthodontic * OR Tooth movement)) AND TS = (Apical periodontitis OR Periapical periodontitis OR Apical lesion * OR Periapical lesion * OR Root-filled tooth OR Root-filled teeth OR Root canal treatment OR Endodontic * OR Periapical abscess OR Apical abscess OR Periapical cyst * OR Apical cyst *) Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, ESCI Timespan = All years |
| EBSCO host (MEDLINE, Academic Search Ultimate, ERIC, Library, and Information Science & Technology Abstracts) |
| (TI (Apical periodontitis OR Periapical periodontitis OR Apical lesion * OR Periapical lesion * OR Root-filled tooth OR Root-filled teeth OR Root canal treatment OR Endodontic * OR Periapical abscess OR Apical abscess OR Periapical cyst * OR Apical cyst *) OR MH (Periapical Periodontitis/physiopathology * OR Periapical Periodontitis * OR Root Canal Therapy OR Root Canal Obturation)) AND (TI (Orthodontic * OR Tooth movement) OR MH (Orthodontics, Corrective *)) |
| ProQuest |
| (mainsubject(Periapical Periodontitis/physiopathology * OR Periapical Periodontitis * OR Root Canal Therapy OR Root Canal Obturation) OR abstract(Apical periodontitis OR Periapical periodontitis OR Apical lesion * OR Periapical lesion * OR Root-filled tooth OR Root-filled teeth OR Root canal treatment OR Endodontic * OR Periapical abscess OR Apical abscess OR Periapical cyst * OR Apical cyst *) OR title(Apical periodontitis OR Periapical periodontitis OR Apical lesion * OR Periapical lesion * OR Root-filled tooth OR Root-filled teeth OR Root canal treatment OR Endodontic * OR Periapical abscess OR Apical abscess OR Periapical cyst * OR Apical cyst *)) AND (mainsubject(Orthodontics, Corrective *) OR abstract(Orthodontic * OR Tooth movement) OR title(Orthodontic * OR Tooth movement)) |
| Citation | Study Type; Country; Date Publication | Sample Size (Age); Gender Distribution | Investigated Teeth | Malocclusion Type | Endodontic Treatment Type | Timing of Endodontic Treatment | Orthodontic Treatment Type; Duration | Orthodontic Forces | Periapical Assessment Method | Outcome of Interest | Main Results | Study Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (Alqerban et al., 2019) [9] | Cross-sectional retrospective clinical study; Saudi Arabia; 2019 | 72 patients (23.4 ± 6.9 yr); 49 F: 23 M | 128 teeth (incisors, premolars, and molars) | Not mentioned. | Primary RCT but no further details | Before orthodontic tx. | FA but no further details; tx duration 1.8 ± 1.1 yr | Not mentioned. | OPG assessment of RCT quality, length, density, and homogeneity, and coronal restoration. The probability index and the periapical index were used to evaluate periapical bone destruction and healing, respectively before and after orthodontic treatment. | RCT treatment integrity and quality, and periapical bone destruction and lesions. | Teeth with adequate RCT showed no changes in the periapical bone destruction or healing after orthodontic tx, while teeth with inadequate RCT had greater risk of periapical bone destruction and lesions after orthodontic tx. | Moderate |
| (Kim et al., 2023) [11] | Cross-sectional retrospective clinical study; South Korea; 2023 | 61 patients (14–54 yr); Not clear | 115 teeth (37 anterior teeth, 22 premolars and 56 molars) | Not mentioned. | RCT but no further details | Not mentioned. | Not reported; tx duration was variable with 24 mo and more than 48 mo | Not mentioned. | CBCT was used to evaluate the size of the periapical radiolucency of endodontically treated teeth before and after orthodontic tx. | The size of periapical radiolucency | Orthodontic treatment did not affect the size of periapical radiolucency. However, females and maxillary teeth showed statistical reduction compared to males and mandibular teeth, respectively. | High |
| (De Souza et al., 2006) [8] | Cross-sectional animal study; United States; 2006 | 2 dogs (1 yr); not mentioned | Incisors and premolars | Not applicable | Root canals were kept opened for 6 mo to induce periapical lesion followed by RCT | Immediately before orthodontic movement. | FA with power chain; tx duration 5 mo and 15 d | 200 g | Animals were scarified and 10 specimens for 16 histological criteria were taken from RCT-free teeth that moved orthodontically, RCT-teeth with no orthodontic movement, and RCT-teeth that moved orthodontically. | Healing of periapical lesions. | The results showed that orthodontic forces delayed but did not hinder the periapical healing process. | Moderate |
| (Baranowskyj, 1969) [7] | Cross-sectional animal study; United States; 1969 | 2 dogs (not mentioned); females | Maxillary second incisors | Not applicable | RCT and apicectomy 6 w apart | 2 w before orthodontic treatment. | Orthodontic intrusive forces for 4 w. | Not mentioned. | Animals were scarified and histological investigation was conducted of periapical healing of both control and experimental dogs. | Healing of periapical tissues. | Early application of orthodontic forces on teeth undergone RCT can delay the healing process of periapical soft and hard tissues. | Low |
| (Chen et al., 2024) [18] | Retrospective cohort clinical study; China; 2024 | 169 teeth of 100 (52 F + 48 M) age (33–23) median age 27. | Mandibular teeth (63) Maxillary teeth (44) Anterior teeth (27) Premolars (37) Molars (43). | Not mentioned. | Primary RCT. | Not mentioned. | Fixed orthodontic movement ortho treatment was 2.6 years. | Not mentioned. | Pre-orthodontic and post-orthodontic CBCTs Absence of AP was assigned 0, while the presence of AP > 0.5 was assigned a score from 1 to 5 based on severity. | Healing of periapical tissue. | Orthodontic movement had no effect on the outcomes of RCT teeth. | High |
| (Ianos et al., 2024) [17] | Cross-sectional retrospective clinical study; Romania; 2024 | 32 teeth from 25 patients. | Not mentioned. | Not mentioned. | Primary RCT. | During orthodontic tx. | Fixed orthodontic movement. | Not mentioned. | CBCT Periapical bone destruction probability index (PRI) was evaluated as follows (absent, uncertain or present). | The size of apical radiolucency. | Endodontically teeth with inadequate RCT show a significantly higher risk of periapical bone destruction. | Moderate |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alharbi, H.; Almutairi, M.S.; Alrajhi, S.; Almotairy, N. Effect of Orthodontic Movement on the Periapical Healing of Teeth Undergone Endodontic Root Canal Treatment: A Systematic Review. J. Clin. Med. 2025, 14, 7292. https://doi.org/10.3390/jcm14207292
Alharbi H, Almutairi MS, Alrajhi S, Almotairy N. Effect of Orthodontic Movement on the Periapical Healing of Teeth Undergone Endodontic Root Canal Treatment: A Systematic Review. Journal of Clinical Medicine. 2025; 14(20):7292. https://doi.org/10.3390/jcm14207292
Chicago/Turabian StyleAlharbi, Hanan, Mishal S. Almutairi, Suliman Alrajhi, and Nabeel Almotairy. 2025. "Effect of Orthodontic Movement on the Periapical Healing of Teeth Undergone Endodontic Root Canal Treatment: A Systematic Review" Journal of Clinical Medicine 14, no. 20: 7292. https://doi.org/10.3390/jcm14207292
APA StyleAlharbi, H., Almutairi, M. S., Alrajhi, S., & Almotairy, N. (2025). Effect of Orthodontic Movement on the Periapical Healing of Teeth Undergone Endodontic Root Canal Treatment: A Systematic Review. Journal of Clinical Medicine, 14(20), 7292. https://doi.org/10.3390/jcm14207292






