Statin Treatment for Reducing Mortality Risk in Individuals over 75 Years of Age: A Large-Scale Retrospective Analysis
Abstract
1. Background
2. Methods
2.1. Study Population
2.2. Data Source and Variables
2.3. Study Endpoints
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. CVA, MI and All-Cause Mortality
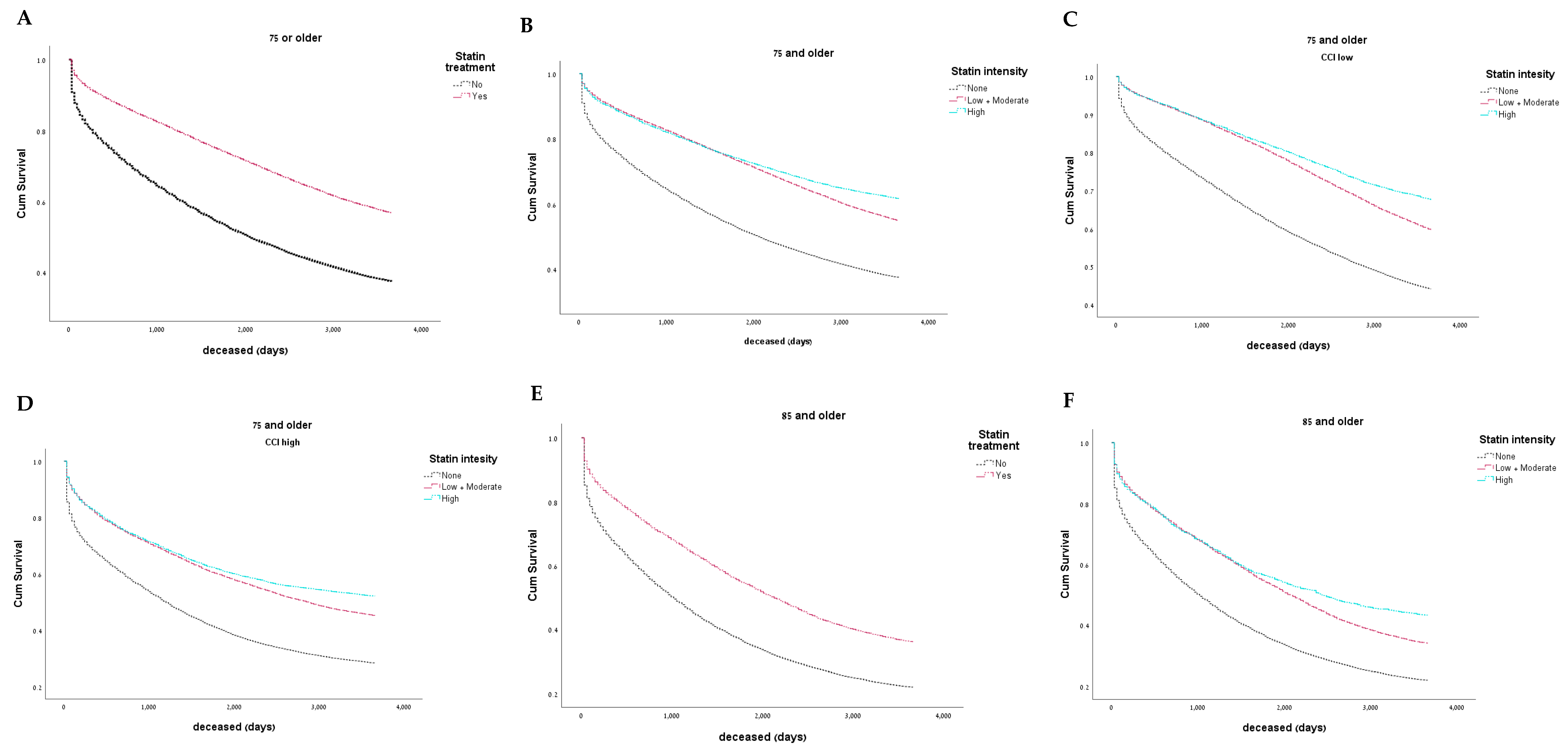
3.3. Impact of Statin Intensity on All-Cause Mortality
3.4. Impact of CCI on All-Cause Mortality
3.5. Impact of Statin Intensity on Cardiovascular Outcomes
3.6. Oldest Old Population
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CCI | Charlson comorbidity index |
| aOR | adjusted odds ratio |
| ASCVD | atherosclerotic cardiovascular disease |
| IRB | institutional review board |
| NNT | number needed to treat |
| TASMC | Tel Aviv Sourasky Medical Center |
| STROBE | Strengthening the Reporting of Observational Studies in Epidemiology |
| MI | myocardial infarction |
| CVA | cerebrovascular accident |
| LDL | low-density lipoprotein |
| HDL | high-density lipoprotein |
References
- Escourrou, E.; Laurent, S.; Leroux, J.; Oustric, S.; Gardette, V. The Shift from Old Age to Very Old Age: An Analysis of the Perception of Aging among Older People. BMC Prim. Care 2022, 23, 3. [Google Scholar] [CrossRef]
- Perna, G.P. Statins and Age: Is There a Limit beyond Which Primary Prevention Is Futile? Eur. Heart J. Suppl. 2021, 23, E109–E111. [Google Scholar] [CrossRef]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskina, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the Management of Dyslipidaemias: Lipid Modification to Reduce Cardiovascular Risk. Atherosclerosis 2019, 290, 140–205. [Google Scholar] [CrossRef] [PubMed]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 140, 11. [Google Scholar] [CrossRef] [PubMed]
- Thompson, W.; Pottegård, A.; Nielsen, J.B.; Haastrup, P.; Jarbøl, D.E. How Common Is Statin Use in the Oldest Old? Drugs Aging 2018, 35, 679–686. [Google Scholar] [CrossRef] [PubMed]
- Mortensen, M.B.; Nordestgaard, B.G. Elevated LDL Cholesterol and Increased Risk of Myocardial Infarction and Atherosclerotic Cardiovascular Disease in Individuals Aged 70–100 Years: A Contemporary Primary Prevention Cohort. Lancet 2020, 396, 1644–1652. [Google Scholar] [CrossRef]
- Gencer, B.; Marston, N.A.; Im, K.A.; Cannon, C.P.; Sever, P.; Keech, A.; Braunwald, E.; Giugliano, R.P.; Sabatine, M.S. Efficacy and Safety of Lowering LDL Cholesterol in Older Patients: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Lancet 2020, 396, 1637–1643. [Google Scholar] [CrossRef]
- Mésidor, M.; Sirois, C.; Guertin, J.R.; Schnitzer, M.E.; Candas, B.; Blais, C.; Cossette, B.; Poirier, P.; Brophy, J.M.; Lix, L.; et al. Effect of Statin Use for the Primary Prevention of Cardiovascular Disease among Older Adults: A Cautionary Tale Concerning Target Trials Emulation. J. Clin. Epidemiol. 2024, 168, 111284. [Google Scholar] [CrossRef]
- Gharaibeh, A.; Koppikar, S.; Bonilla-Escobar., F.J. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) in the International Journal of Medical Students. Int. J. Med. Stud. 2014, 2, 36–37. [Google Scholar] [CrossRef]
- Foraker, R.E.; Yu, S.C.; Gupta, A.; Michelson, A.P.; Pineda Soto, J.A.; Colvin, R.; Loh, F.; Kollef, M.H.; Maddox, T.; Evanoff, B.; et al. Spot the Difference: Comparing Results of Analyses from Real Patient Data and Synthetic Derivatives. JAMIA Open 2020, 3, 557–566. [Google Scholar] [CrossRef]
- Huang, Y.Q.; Gou, R.; Diao, Y.S.; Yin, Q.H.; Fan, W.X.; Liang, Y.P.; Chen, Y.; Wu, M.; Zang, L.; Li, L.; et al. Charlson Comorbidity Index Helps Predict the Risk of Mortality for Patients with Type 2 Diabetic Nephropathy. J. Zhejiang Univ. Sci. B 2014, 15, 58–66. [Google Scholar] [CrossRef]
- Wilkinson, J.D.; Mamas, M.A.; Kontopantelis, E. Logistic regression frequently outperformed propensity score methods, especially for large datasets: A simulation study. J. Clin. Epidemiol. 2022, 152, 176–184. [Google Scholar] [CrossRef] [PubMed]
- Nowak, M.M.; Niemczyk, M.; Florczyk, M.; Kurzyna, M.; Pączek, L. Effect of Statins on All-Cause Mortality in Adults: A Systematic Review and Meta-Analysis of Propensity Score-Matched Studies. J. Clin. Med. 2022, 11, 5643. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- US Preventive Services Task Force. Statin Use for the Primary Prevention of Cardiovascular Disease in Adults: US Preventive Services Task Force Recommendation Statement. JAMA 2022, 328, 746–753. [Google Scholar] [CrossRef]
- Frieden, P.; Gagnon, R.; Bénard, É.; Cossette, B.; Bergeron, F.; Talbot, D.; Guertin, J.R. Strategies Aiming to Improve Statin Therapy Adherence in Older Adults: A Systematic Review. BMC Geriatr. 2024, 24, 444. [Google Scholar] [CrossRef] [PubMed]
- Kip, K.; Hollabaugh, K.; Marroquin, O.; David, O.; Williams, M.D. The Problem With Composite End Points in Cardiovascular Studies: The Story of Major Adverse Cardiac Events and Percutaneous Coronary Intervention. JACC 2008, 51, 701–707. [Google Scholar] [CrossRef] [PubMed]
- Armitage, J.; Baigent, C.; Barnes, E.; Betteridge, D.J.; Blackwell, L.; Blazing, M.; Bowman, L.; Braunwald, E.; Byington, R.; Cannon, C.; et al. Efficacy and Safety of Statin Therapy in Older People: A Meta-Analysis of Individual Participant Data from 28 Randomised Controlled Trials. Lancet 2019, 393, 407–415. [Google Scholar] [CrossRef]
- Zoungas, S.; Curtis, A.; Spark, S.; Wolfe, R.; McNeil, J.J.; Beilin, L.; Chong, T.T.; Cloud, G.; Hopper, I.; Kost, A.; et al. Statins for extension of disability-free survival and primary prevention of cardiovascular events among older people: Protocol for a randomized controlled trial in primary care (STAREE trial). BMJ Open 2023, 13, e069915. [Google Scholar] [CrossRef]
- Zoungas, S.; Moran, C.; Curtis, A.J.; Spark, S.; Flanagan, Z.; Beilin, L.; Chong, T.T.; Cloud, G.C.; Hopper, I.; Kost, A.; et al. Baseline Characteristics of Participants in STAREE: A Randomized Trial for Primary Prevention of Cardiovascular Disease Events and Prolongation of Disability-Free Survival in Older People. J. Am. Heart Assoc. 2024, 13, e036357. [Google Scholar] [CrossRef]
- Charlson, M.E.; Carrozzino, D.; Guidi, J.; Patierno, C. Charlson Comorbidity Index: A Critical Review of Clinimetric Properties. Psychother. Psychosom. 2022, 91, 8–35. [Google Scholar] [CrossRef]
- Azami, P.; Mirhosseini, A.; Nobakhti, M.; Sayadi, M.; Keshavarz, M.; Parizi, M.D.; Saeedizade, R.; Borjzadeh, M.; Zibaeenezhad, M.J.; Attar, A. Association Between ECG Findings and Atherosclerotic Cardiovascular Disease (ASCVD) Risk Score: A Cross-Sectional Analysis of a Cohort Study. Health Sci. Rep. 2025, 8, e71026. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wu, G.; Wu, J.; Lu, Q.; Cheng, Y.; Mei, W. Association between cardiovascular risk factors and atrial fibrillation. Front. Cardiovasc. Med. 2023, 10, 1110424. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Attardo, S.; Musumeci, O.; Velardo, D.; Toscano, A. Statins Neuromuscular Adverse Effects. Int. J. Mol. Sci. 2022, 23, 8364. [Google Scholar] [CrossRef] [PubMed]
- Adam, L.; Baretella, O.; Feller, M.; Blum, M.R.; Papazoglou, D.D.; Boland, B.; Aujesky, D.; Baggio, S.; Rodondi, N. Statin therapy in multimorbid older patients with polypharmacy- a cross-sectional analysis of the Swiss OPERAM trial population. Front. Cardiovasc. Med. 2023, 10, 1236547. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Without Chronic Statin Treatment (N = 61331) | With Chronic Statin Treatment (N = 37171) | ||||
|---|---|---|---|---|---|
| Male | 26,388 (43%) | 17,772 (47.8%) | |||
| Mean Age | 82.69 | ±5.77 | 80.67 | ±4.73 | p < 0.001 |
| 75 to 85 years | 42,078 | 68.61% | 30,367 | 81.7% | p < 0.001 |
| 85+ | 19,253 | 31.39% | 6804 | 18.3% | p < 0.001 |
| CCI | 4 | [3, 5] | 4 | [3, 5] | p < 0.001 |
| HTN | 27,000 | 27.41% | 28,958 | 29.39% | p < 0.001 |
| Cr | 1.03 | ±0.79 | 1.22 | ±0.75 | p < 0.001 |
| HDL | 46.9 | ±16.93 | 45.4 | ±15.58 | p < 0.001 |
| LDL | 94 | ±34.68 | 83.5 | ±15.58 | p < 0.001 |
| Aspirin | 4886 | 4.96% | 13,871 | 14.08% | p < 0.001 |
| Statin * | ---- | High intensity statins ** | 10,186 (27.4%) | ||
| Medium/Low intensity ** statins | 26,985 (72.6%) | ||||
| Combination therapy *** | 632 (1.7%) | ||||
| Without Chronic Statin Treatment (N = 61,331) | With Chronic Statin Treatment (N = 37,171) | ||||
|---|---|---|---|---|---|
| CVA | 3426 | 5.58% | 6277 | 16.88% | p < 0.001 |
| MI | 3450 | 5.62% | 6613 | 17.79% | p < 0.001 |
| 365-day mortality | 14,131 | 23.04% | 3805 | 10.24% | p < 0.001 |
| Total mortality | 42,805 | 69.79% | 19,274 | 51.85% | p < 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nachmias, N.; Matsri, S.; Sharary, M.; Yaniv, N.; Netser, T.; Buch, A.; Greenman, Y.; Izkhakov, E.; Feigin, E. Statin Treatment for Reducing Mortality Risk in Individuals over 75 Years of Age: A Large-Scale Retrospective Analysis. J. Clin. Med. 2025, 14, 5739. https://doi.org/10.3390/jcm14165739
Nachmias N, Matsri S, Sharary M, Yaniv N, Netser T, Buch A, Greenman Y, Izkhakov E, Feigin E. Statin Treatment for Reducing Mortality Risk in Individuals over 75 Years of Age: A Large-Scale Retrospective Analysis. Journal of Clinical Medicine. 2025; 14(16):5739. https://doi.org/10.3390/jcm14165739
Chicago/Turabian StyleNachmias, Noy, Sher Matsri, Maisaa Sharary, Noam Yaniv, Tal Netser, Assaf Buch, Yona Greenman, Elena Izkhakov, and Eugene Feigin. 2025. "Statin Treatment for Reducing Mortality Risk in Individuals over 75 Years of Age: A Large-Scale Retrospective Analysis" Journal of Clinical Medicine 14, no. 16: 5739. https://doi.org/10.3390/jcm14165739
APA StyleNachmias, N., Matsri, S., Sharary, M., Yaniv, N., Netser, T., Buch, A., Greenman, Y., Izkhakov, E., & Feigin, E. (2025). Statin Treatment for Reducing Mortality Risk in Individuals over 75 Years of Age: A Large-Scale Retrospective Analysis. Journal of Clinical Medicine, 14(16), 5739. https://doi.org/10.3390/jcm14165739






