Short-Term Clinical and Biochemical Outcomes of Infants Born After 34 Weeks of Gestation with Mild-to-Moderate Cord Blood Acidosis—A Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Cord Blood Sampling
2.2. Neonatal Follow-Up
2.3. Data Extraction
2.4. Statistical Analysis
3. Results
3.1. Newborn Baseline Parameters and Cord Blood Characteristics
3.2. Clinical Outcomes
3.3. Biochemical Measures
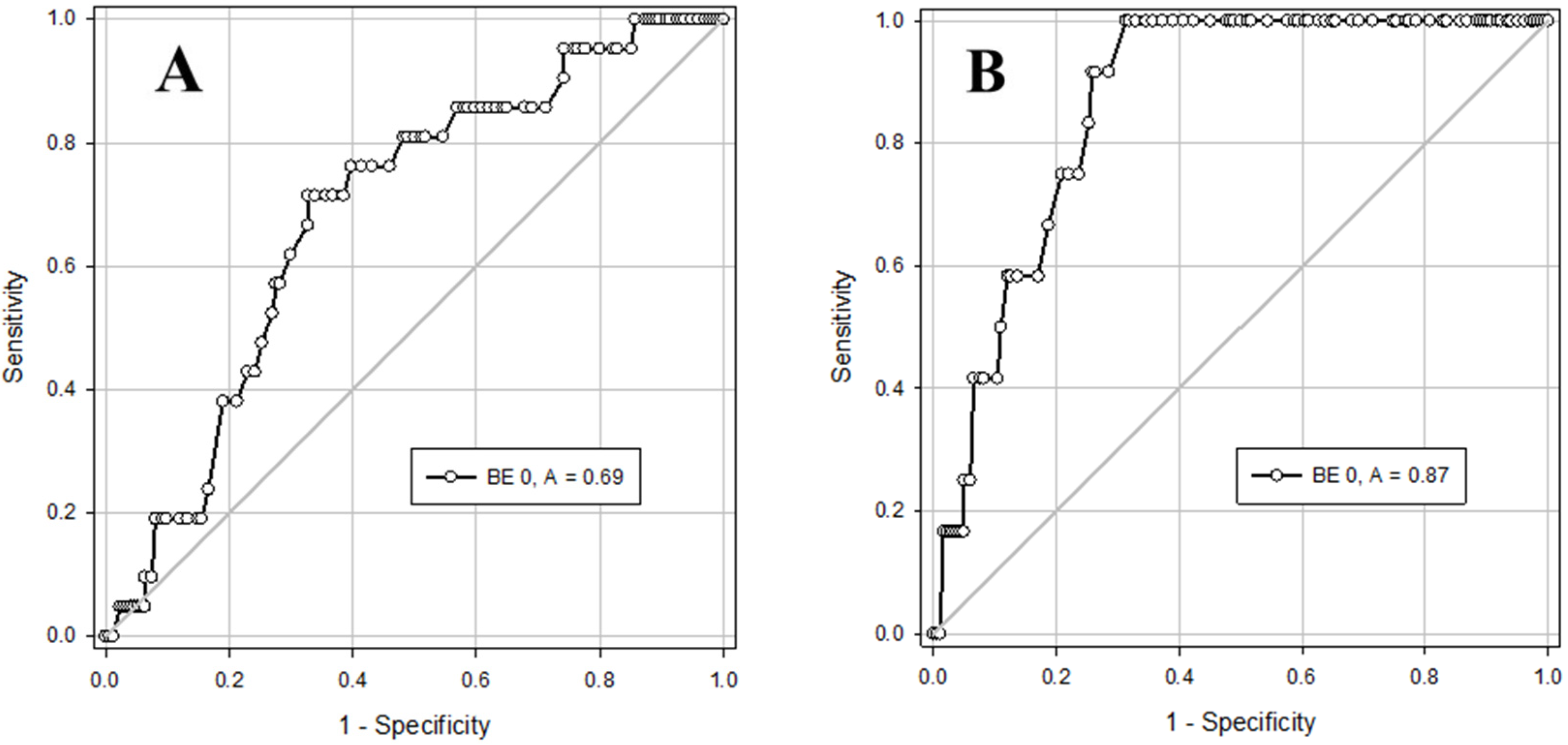
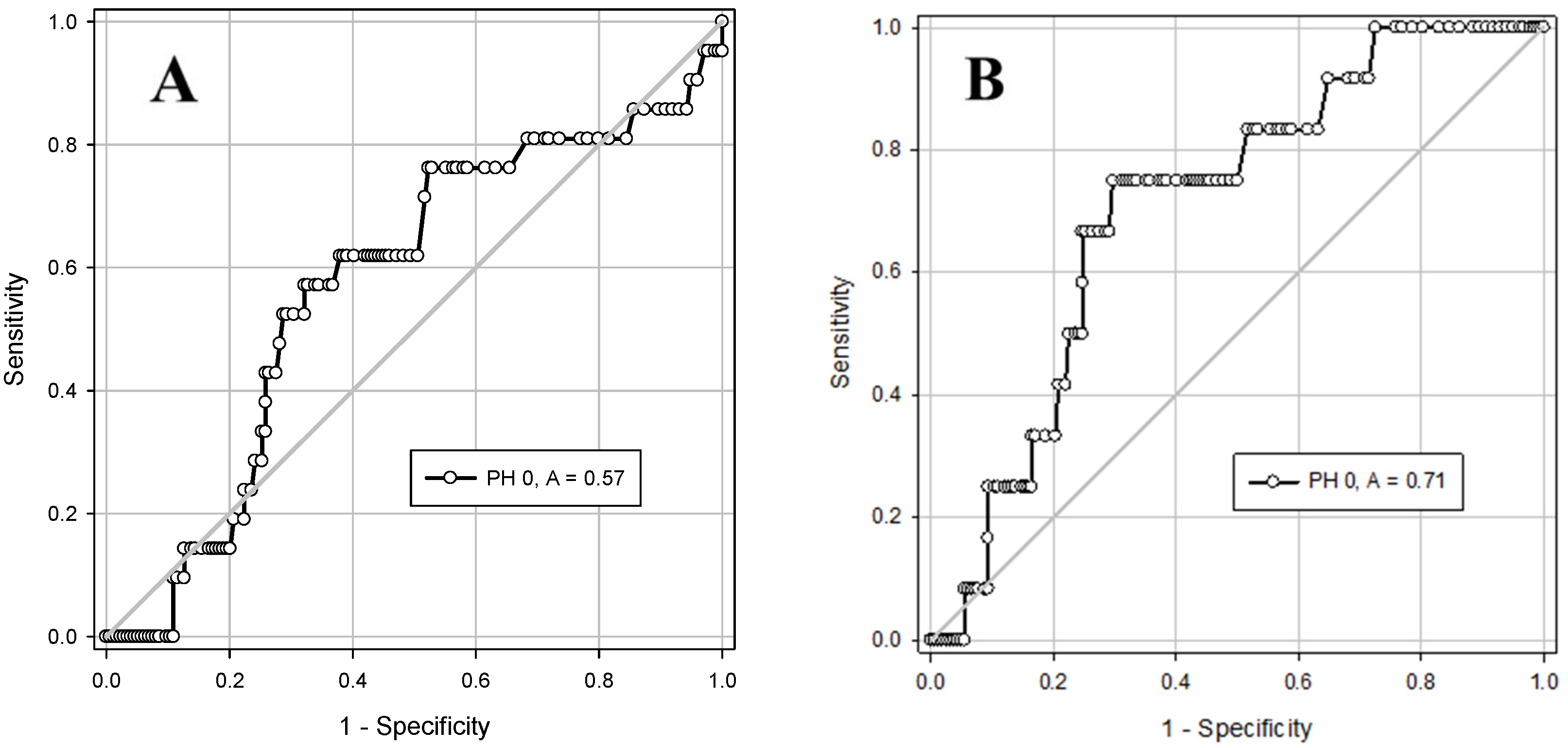
3.4. ROC Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| NICU | Neonatal intensive care unit |
| BE | Base excess |
| HIE | Hypoxic ischemic encephalopathy |
| ROC | Receiver operator curve |
References
- Olofsson, P. Umbilical cord pH, blood gases, and lactate at birth: Normal values, interpretation, and clinical utility. Am. J. Obstet. Gynecol. 2023, 228, S1222–S1240. [Google Scholar] [CrossRef]
- White, C.R.H.; Doherty, D.A.; Henderson, J.J.; Kohan, R.; Newnham, J.P.; Pennell, C.E. Benefits of introducing universal umbilical cord blood gas and lactate analysis into an obstetric unit. Aust. N. Z. J. Obstet. Gynaecol. 2010, 50, 318–328. [Google Scholar] [CrossRef]
- Malin, G.L.; Morris, R.K.; Khan, K.S. Strength of association between umbilical cord pH and perinatal and long-term outcomes: Systematic review and meta-analysis. BMJ 2010, 340, 1121. [Google Scholar] [CrossRef]
- National Collaborating Centre for Women’s and Children’s Health (UK). Intrapartum Care: Care of Healthy Women and Their Babies During Childbirth; NICE Clinical Guidelines, No. 55; RCOG Press: London, UK, 2007. [Google Scholar]
- American College of Obstetricians and Gynecologists’ Task Force on Neonatal Encephalopathy. Executive summary: Neonatal encephalopathy and neurologic outcome, second edition. Obstet. Gynecol. 2014, 123, 896–901. [Google Scholar] [CrossRef]
- Ahlberg, M.; Elvander, C.; Johansson, S.; Cnattingius, S.; Stephansson, O. A policy of routine umbilical cord blood gas analysis decreased missing samples from high-risk births. Acta Paediatr. 2017, 106, 43–48. [Google Scholar] [CrossRef]
- Riley, R.J.; Johnson, J.W.C. Collecting and analyzing cord blood gases. Clin. Obstet. Gynecol. 1993, 36, 13–23. [Google Scholar] [CrossRef]
- Thorp, J.A.; Sampson, J.E.; Parisi, V.M.; Creasy, R.K. Routine umbilical cord blood gas determinations? Am. J. Obstet. Gynecol. 1989, 161, 600–605. [Google Scholar] [CrossRef] [PubMed]
- Roberts, S.W.; Leveno, K.J.; Sidawi, J.E.; Lucas, M.J.; Kelly, M.A. Fetal acidemia associated with regional anesthesia for elective cesarean delivery. Obstet. Gynecol. 1995, 85, 79–83. [Google Scholar] [CrossRef] [PubMed]
- Atalla, R.K.; Abrams, K.; Bell, S.C.; Taylor, D.J. Newborn acid-base status and umbilical cord morphology. Obstet. Gynecol. 1998, 92, 865–868. [Google Scholar] [CrossRef]
- Maher, J.T.; Conti, J.A. A comparison of umbilical cord blood gas values between newborns with and without true knots. Obstet. Gynecol. 1996, 88, 863–866. [Google Scholar] [CrossRef] [PubMed]
- Van den Berg, P.P.; Nelen, W.L.D.M.; Jongsma, H.W.; Nijland, R.; Kollée, L.A.; Nijhuis, J.G.; Eskes, T.K. Neonatal complications in newborns with an umbilical artery pH < 7.00. Am. J. Obstet. Gynecol. 1996, 175, 1152–1157. [Google Scholar]
- Murphy Goodwin, T.; Belai, I.; Hernandez, P.; Durand, M.; Paul, R.H. Asphyxial complications in the term newborn with severe umbilical acidemia. Am. J. Obstet. Gynecol. 1992, 167, 1506–1512. [Google Scholar] [CrossRef] [PubMed]
- Shah, P.S.; Barrett, J.; Claveau, M.; Cieslak, Z.; Makary, H.; Monterrosa, L.; Sherlock, R.; Yang, J.; McDonald, S.D. Association of umbilical cord blood gas values with mortality and severe neurologic injury in preterm neonates. Am. J. Obstet. Gynecol. 2022, 227, 85.e1–85.e10. [Google Scholar] [CrossRef] [PubMed]
- El-Dib, M.; Inder, T.E.; Chalak, L.F.; Massaro, A.N.; Thoresen, M.; Gunn, A.J. Should therapeutic hypothermia be offered to babies with mild neonatal encephalopathy in the first 6 h after birth? Pediatr. Res. 2019, 85, 442–448. [Google Scholar] [CrossRef]
- Yeh, P.; Emary, K.; Impey, L. The relationship between umbilical cord arterial pH and serious adverse neonatal outcome: Analysis of 51,519 consecutive validated samples. BJOG 2012, 119, 824–831. [Google Scholar] [CrossRef]
- Bailey, E.J.; Frolova, A.I.; López, J.D.; Raghuraman, N.; Macones, G.A.; Cahill, A.G. Mild Neonatal Acidemia Is Associated with Neonatal Morbidity at Term. Am. J. Perinatol. 2021, 38, E155–E161. [Google Scholar] [CrossRef] [PubMed]
- Andersson, C.B.; Klingenberg, C.; Thellesen, L.; Johnsen, S.P.; Kesmodel, U.S.; Petersen, J.P. Umbilical Cord pH Levels and Neonatal Morbidity and Mortality. JAMA Netw. Open. 2024, 7, e2427604. [Google Scholar] [CrossRef]
- Lee, J.H.; Jung, J.; Park, H.; Kim, S.-Y.; Kwon, D.Y.; Choi, S.-J.; Oh, S.-Y.; Roh, C.-R. Umbilical cord arterial blood gas analysis in term singleton pregnancies: A retrospective analysis over 11 years. Obstet. Gynecol. Sci. 2020, 63, 293–304. [Google Scholar] [CrossRef]
- Sabol, B.A.; Caughey, A.B. Acidemia in Neonates with a 5-Minute Apgar Score of 7 or Greater—What Are the Outcomes? Am. J. Obstet. Gynecol. 2016, 215, 486.e1–486.e6. [Google Scholar] [CrossRef]
- Hensel, D.; Zahedi-Spung, L.; Carter, E.B.; Cahill, A.G.; Raghuraman, N.; Rosenbloom, J.I. The Risk of Neonatal Morbidity in Umbilical Artery Hypercarbia and Respiratory Acidosis. Am. J. Perinatol. 2024, 41, e1001–e1007. [Google Scholar] [CrossRef]
- Low, J.A.; Lindsay, B.G.; Derrick, E.J. Threshold of Metabolic Acidosis Associated with Newborn Complications. Am. J. Obstet. Gynecol. 1997, 177, 1391–1394. [Google Scholar] [CrossRef] [PubMed]
- Bitar, L.; Leon, R.L.; Liu, Y.L.; Kota, S.; Chalak, L.F. Multi-Organ Dysfunction across the Neonatal Encephalopathy Spectrum. Pediatr. Res. 2025. [Google Scholar] [CrossRef] [PubMed]
- Victory, R.; Penava, D.; Da Silva, O.; Natale, R.; Richardson, B. Umbilical cord pH and base excess values in relation to adverse outcome events for infants delivering at term. Am. J. Obstet. Gynecol. 2004, 191, 2021–2028. [Google Scholar] [CrossRef]
- Talisman, S.; Guedalia, J.; Farkash, R.; Avitan, T.; Srebnik, N.; Kasirer, Y.; Schimmel, M.S.; Ghanem, D.; Unger, R.; Granovsky, S.G. Neonatal intensive care admission for term neonates and subsequent childhood mortality: A retrospective linkage study. BMC Med. 2023, 21, 44. [Google Scholar] [CrossRef] [PubMed]
- Bligard, K.H.; Cameo, T.; McCallum, K.N.; Rubin, A.; Rimsza, R.R.; Cahill, A.G.; Palanisamy, A.; Odibo, A.O.; Raghuraman, N. The Association of Fetal Acidemia with Adverse Neonatal Outcomes at Time of Scheduled Cesarean Delivery. Am. J. Obstet. Gynecol. 2022, 227, 265.e1–265.e8. [Google Scholar] [CrossRef]
- Chakkarapani, E.; de Vries, L.S.; Ferriero, D.M.; Gunn, A.J. Neonatal Encephalopathy and Hypoxic-Ischemic Encephalopathy: The State of the Art. Pediatr. Res. 2025. [Google Scholar] [CrossRef]
- Diviney, M.; Pinnamaneni, R.; Murphy, J.F.; Lynch, B.; Rushe, H.; Madigan, C.; Geary, M.; Foran, A. Neurodevelopmental outcome at seven years in term, acidotic newborns. Ir. Med. J. 2015, 108, 106–109. [Google Scholar]
- Hafström, M.; Ehnberg, S.; Blad, S.; Norén, H.; Renman, C.; Rosén, K.G.; Kjellmer, I. Developmental outcome at 6.5 years after acidosis in term newborns: A population-based study. Pediatrics 2012, 129, e1501–e1507. [Google Scholar] [CrossRef]
- Shah, P.; Riphagen, S.; Beyene, J.; Perlman, M. Multiorgan Dysfunction in Infants with Post-Asphyxial Hypoxic-Ischaemic Encephalopathy. Arch. Dis. Child. Fetal Neonatal Ed. 2004, 89, F152–F155. [Google Scholar] [CrossRef]
- Alsina, M.; Martín-Ancel, A.; Alarcon-Allen, A.; Arca, G.; Gayá, F.; García-Alix, A. The Severity of Hypoxic-Ischemic Encephalopathy Correlates with Multiple Organ Dysfunction in the Hypothermia Era. Pediatr. Crit. Care Med. 2017, 18, 234–240. [Google Scholar] [CrossRef]
- Demirel, N.; Unal, S.; Durukan, M.; Celik, İ.H.; Bas, A.Y. Multi-Organ Dysfunction in Infants with Acidosis at Birth in the Absence of Moderate to Severe Hypoxic Ischemic Encephalopathy. Early Hum. Dev. 2023, 181, 105775. [Google Scholar] [CrossRef] [PubMed]
- Manalastas, M.; Shine, K.C.; Yuan, A.; Di Chiaro, B.A.; Weiss, M.G.; Amin, S.; Dina, P.; Muraskas, J.K. Neonatal Serial Creatinine Levels as an Adjunct Biomarker in Timing of Fetal Neurologic Injury. Eur. J. Obstet. Gynecol. Reprod. Biol. 2023, 18, 100191. [Google Scholar] [CrossRef]
- Michniewicz, B.; Szpecht, D.; Sowińska, A.; Sibiak, R.; Szymankiewicz, M.; Gadzinowski, J. Biomarkers in Newborns with Hypoxic-Ischemic Encephalopathy Treated with Therapeutic Hypothermia. Childs Nerv. Syst. 2020, 36, 2981–2988. [Google Scholar] [CrossRef]
- Elsadek, A.E.; Fathy Barseem, N.; Suliman, H.A.; Elshorbagy, H.H.; Kamal, N.M.; Talaat, I.M.; Al-Shokary, A.H.; Abdel Maksoud, Y.H.; Ibrahim, A.O.; Attia, A.M.; et al. Hepatic Injury in Neonates with Perinatal Asphyxia. Glob. Pediatr. Health 2021, 8, 2333794X20987781. [Google Scholar] [CrossRef]
- Brucknerová, I.; Ujházy, E.; Dubovický, M.; Mach, M. Early Assessment of the Severity of Asphyxia in Term Newborns Using Parameters of Blood Count. Interdiscip. Toxicol. 2008, 1, 211–213. [Google Scholar] [CrossRef]
- Koreti, S.; Gupta, A. Simple and Feasible Blood Markers as Predictors of Perinatal Asphyxia. Int. J. Contemp. Pediatr. 2017, 4, 1041–1045. [Google Scholar] [CrossRef][Green Version]
- Ross, M.G.; Gala, R. Use of Umbilical Artery Base Excess: Algorithm for the Timing of Hypoxic Injury. Am. J. Obstet. Gynecol. 2002, 187, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Tuuli, M.G.; Stout, M.J.; Shanks, A.; Odibo, A.O.; Macones, G.A.; Cahill, A.G. Umbilical Cord Arterial Lactate Compared with pH for Predicting Neonatal Morbidity at Term. Obstet. Gynecol. 2014, 124, 756. [Google Scholar] [CrossRef] [PubMed]
- Ahmadpour-Kacho, M.; Zahedpasha, Y.; Hagshenas, M.; Akbarian Rad, Z.; Sadat Nasseri, B.; Bijani, A. Short Term Outcome of Neonates Born with Abnormal Umbilical Cord Arterial Blood Gases. Iran. J. Pediatr. 2015, 25, 174. [Google Scholar] [CrossRef]
| pH 7.00–7.12 n = 86 | pH 7.13–7.20 n = 251 | p-Value | |
|---|---|---|---|
| Gestational Age (weeks) * | 39.6 (38.6, 40.5) | 39.6 (38.6, 40.5) | 0.867 |
| Birth Weight (g) ** | 3260 ± 484 | 3276 ± 477 | 0.795 |
| Female n (%) | 39 (45) | 92 (37) | 0.194 |
| Delivery Mode n (%) | 0.478 | ||
| Vaginal | 22 (25) | 50 (20) | |
| Vacuum | 22 (25) | 76 (30) | |
| Emergency C/S | 36 (42) | 114 (45) | |
| Elective C/S | 6 (7) | 11 (4) | |
| APGAR 1 min * | 8 (6, 9) | 8 (7, 9) | 0.004 |
| APGAR 5 min * | 9 (9, 10) | 9 (9, 10) | 0.030 |
| Cord pH * | 7.09 (7.06, 7.11) | 7.17 (7.15, 7.18) | <0.001 |
| Cord Base excess ** | −12.7 ± 1.8 | −9.6 ± 1.9 | <0.001 |
| Cord Base excess ≤ −12 n (%) | 57 (66) | 33 (13) | <0.001 |
| Cord HCO3 * | 22.3 (20.6, 23.6) | 23.1 (21.6, 24.5) | 0.007 |
| Cord pCO2 * | 75.7 (70.2, 82.7) | 65.4 (60.1, 69.4) | <0.001 |
| Acidosis type n (%) | <0.001 | ||
| Respiratory | 1 (1) | 44 (17) | |
| Metabolic | 3 (3) | 59 (23) | |
| Mixed | 82 (95) | 148 (58) | |
| BE −12 to −16 n = 90 | BE > −12 n = 247 | p-Value | |
| Gestational Age (weeks) | 39.9 (39.1, 40.7) | 39.4 (38.5, 40.5) | 0.027 |
| Birth Weight (g) ** | 3281 ± 490 | 3268 ± 475 | 0.836 |
| Female n (%) | 35 (39) | 96 (39) | 0.902 |
| Delivery Mode n (%) | 0.019 | ||
| Vaginal | 25 (28) | 47 (19) | |
| Vacuum | 30 (33) | 68 (28) | |
| Emergency C/S | 28 (31) | 122 (49) | |
| Elective C/S | 7 (8) | 10 (4) | |
| Apgar 1 * | 8 (6, 9) | 8 (7, 9) | 0.002 |
| Apgar 5 * | 9 (8, 10) | 9 (9, 10) | 0.011 |
| Cord pH * | 7.10 (7.06, 7.14) | 7.17 (7.14, 7.18) | <0.001 |
| Cord pH ≤ 7.12 n (%) | 57 (63) | 29 (12) | <0.001 |
| Cord Base excess * | −13.0 (−14.0, −12.5) | −9.4 (−10.6, −8.2) | <0.001 |
| Cord HCO3 ** | 20.1 ± 2 | 23.6 ± 1.9 | <0.001 |
| Cord pCO2 * | 66.3 (56.1, 75.9) | 67.1 (36.2, 72.5) | 0.220 |
| Acidosis type n (%) | <0.001 | ||
| Respiratory | 0 (0) | 45 (18) | |
| Metabolic | 31 (34) | 31 (13) | |
| Mixed | 59 (65) | 171 (69) |
| BE −12 to −16 n = 90 | BE > −12 n = 247 | p-Value | |
|---|---|---|---|
| Clinical outcomes | |||
| NICU admission n (%) | 22 (24) | 26 (11) | 0.002 |
| HIE any n (%) | 1 (0.4) | 0 (0) | 0.598 |
| Respiratory distress n (%) | 16 (18) | 12 (5) | <0.001 |
| Meconium aspiration syndrome n (%) | 1 (1) | 1 (0.4) | 0.956 |
| Mechanical ventilation n (%) | 1 (1) | 0 (0) | 0.598 |
| Non-invasive respiratory support n (%) | 12 (13) | 9 (4) | 0.003 |
| Length of hospital stay * | 4 (3, 5) | 3 (3, 4) | <0.001 |
| Laboratory measures | |||
| Base excess after 1 h * | −7.9 (−10.2, −6.8) n = 69 | −6.3 (−7.1, −4.9) n = 110 | <0.001 |
| Time to pH ≥ 7.25 h * | 2.25 (1, 6) n = 66 | 2 (1, 3) n = 108 | 0.007 |
| WBC * ×10 | 18 (14, 22) n = 74 | 17 (13, 21) n = 116 | 0.152 |
| Hct ** % | 52 ± 5.9 n = 72 | 57 ± 7.2 n = 118 | <0.001 |
| Plt * ×100 | 254 (213, 289) n = 73 | 242 (204, 287) n = 116 | 0.430 |
| Urea * mg/dL | 26 (21, 30) n = 72 | 25 (19, 29) n = 123 | 0.151 |
| Creatinine * mg/dL | 0.9 (0.7, 1.0) n = 72 | 0.8 (0.6, 0.9) n = 123 | 0.007 |
| AST * U/L | 64 (48, 80) n = 70 | 49 (38, 65) n = 124 | <0.001 |
| ALT * U/L | 22 (13, 28) n = 71 | 26 (22, 34) n = 122 | 0.001 |
| GGT * U/L | 91 (67, 111) n = 62 | 98 (84, 123) n = 110 | 0.013 |
| ALK-P * U/L | 178 (141, 221) n = 63 | 198 (189, 222) n = 115 | 0.005 |
| pH 7.00–7.12 n = 86 | pH 7.13–7.20 n = 251 | p-Value | |
|---|---|---|---|
| Clinical outcomes | |||
| NICU admission n (%) | 23 (27) | 25 (10) | <0.001 |
| HIE any n (%) | 1 (1) | 0 (0) | 0.574 |
| Respiratory distress n (%) | 15 (17) | 13 (5) | <0.001 |
| Meconium aspiration syndrome n (%) | 2 (2) | 0 (0) | 0.107 |
| Mechanical ventilation n (%) | 1 (1) | 0 (0) | 0.574 |
| Non-invasive respiratory support n (%) | 12 (14) | 9 (4) | 0.002 |
| Length of hospital stay * | 4 (4, 5) | 3 (3, 4) | <0.001 |
| Laboratory measures | |||
| pH after 1 h * | 7.24 (7.13, 7.29) n = 48 | 7.33 (7.28, 7.36) n = 131 | <0.001 |
| Time to pH ≥ 7.25 h * | 3.5 (1, 6.5) n = 48 | 2 (1, 3) n = 126 | 0.001 |
| WBC * ×10 | 18.6 (13.6, 20.8) n = 59 | 17.0 (13.3, 22.1) n = 131 | 0.430 |
| Hct ** % | 54.1 ± 6.4 n = 60 | 56.3 ± 7.3 n = 132 | 0.040 |
| Plt * ×100 | 252 (205, 282) n = 59 | 247 (211, 290) n = 130 | 0.866 |
| Urea * mg/dL | 26 (20, 32) n = 53 | 25 (20, 29) n = 142 | 0.280 |
| Creatinine * mg/dL | 0.8 (0.8, 1.0) n = 53 | 0.8 (0.7, 0.9) n = 142 | 0.039 |
| AST * U/L | 65 (45, 80) n = 52 | 53 (38, 66) n = 142 | 0.002 |
| ALT * U/L | 20 (13, 29) n = 51 | 26 (21, 33) n = 142 | 0.005 |
| GGT * U/L | 89 (66, 111) n = 40 | 98 (77, 122) n = 132 | 0.022 |
| ALK-P * U/L | 187 (141, 222) n = 44 | 198 (184, 221) n = 134 | 0.110 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gover, A.; Riskin, A.; Sharkansky, L.; Hijazi, R.; Ghannam, R.; Zaitoon, H. Short-Term Clinical and Biochemical Outcomes of Infants Born After 34 Weeks of Gestation with Mild-to-Moderate Cord Blood Acidosis—A Retrospective Study. J. Clin. Med. 2025, 14, 5720. https://doi.org/10.3390/jcm14165720
Gover A, Riskin A, Sharkansky L, Hijazi R, Ghannam R, Zaitoon H. Short-Term Clinical and Biochemical Outcomes of Infants Born After 34 Weeks of Gestation with Mild-to-Moderate Cord Blood Acidosis—A Retrospective Study. Journal of Clinical Medicine. 2025; 14(16):5720. https://doi.org/10.3390/jcm14165720
Chicago/Turabian StyleGover, Ayala, Arieh Riskin, Livnat Sharkansky, Rawan Hijazi, Ranin Ghannam, and Hussein Zaitoon. 2025. "Short-Term Clinical and Biochemical Outcomes of Infants Born After 34 Weeks of Gestation with Mild-to-Moderate Cord Blood Acidosis—A Retrospective Study" Journal of Clinical Medicine 14, no. 16: 5720. https://doi.org/10.3390/jcm14165720
APA StyleGover, A., Riskin, A., Sharkansky, L., Hijazi, R., Ghannam, R., & Zaitoon, H. (2025). Short-Term Clinical and Biochemical Outcomes of Infants Born After 34 Weeks of Gestation with Mild-to-Moderate Cord Blood Acidosis—A Retrospective Study. Journal of Clinical Medicine, 14(16), 5720. https://doi.org/10.3390/jcm14165720






