Abstract
Background/Objectives: Endoscopic retrograde cholangiopancreatography (ERCP) with stone extraction is the standard treatment for common bile duct (CBD) stones. However, when complete removal is not feasible, the temporary placement of a plastic stent (PS) is commonly used. This study aimed to assess 12-month stent patency in elderly patients with CBD stones. Methods: This prospective study included patients aged 70 years or older who underwent ERCP with PS placement for CBD stones at Daegu Catholic University Medical Center from March to December 2023. Patients were followed every three months with laboratory tests and abdominal radiographs. Stent dysfunction was defined as either cholangitis or cholecystitis due to stent migration or occlusion. Results: Of 12 enrolled patients, 2 were lost to follow-up. The remaining 10 had a median age of 85 years. The median stone diameter and number were 16.5 mm and 3, respectively. Two patients (20%) experienced stent dysfunction at 1.4 and 2.7 months and underwent successful stent exchange. Of the remaining eight, one declined further ERCP, while seven underwent elective ERCP at 12 months. Among them, five achieved successful stone removal and two required stent exchange. Kaplan–Meier analysis showed 90% patency at 1.4 months and 80% at 2.7 months, maintained through 12 months. Conclusions: Plastic stents showed an acceptable 12-month patency in most elderly patients. Early complications suggest the need for close monitoring during the first three months, after which long-term stent maintenance may be feasible in selected cases. Larger studies are needed to validate these findings.
1. Introduction
Common bile duct (CBD) stones are typically managed with endoscopic retrograde cholangiopancreatography (ERCP) [1]. However, approximately 10% to 15% of cases are considered difficult due to stone characteristics or anatomical variations [2]. In such situations, temporary biliary drainage using plastic stent (PS) placement is often employed as an alternative strategy [1,2].
Temporary stenting has been shown to reduce stone size and facilitate delayed removal at follow-up ERCP, typically within a few months of initial drainage, with or without the addition of ursodeoxycholic acid (UDCA) [3,4]. However, when complete clearance remains unachievable despite repeated attempts, long-term biliary stenting with regular exchange may be required. According to the European Society of Gastrointestinal Endoscopy (ESGE) guideline, PSs placed for incomplete CBD stone clearance should be exchanged within 3–6 months to prevent infectious complications such as cholangitis [1].
ERCP is associated with inherent procedural risks, which are amplified with repeated procedures [5]. A meta-analysis showed octogenarians had higher rates of mortality compared with younger patients, whereas nonagenarians had increased rates of bleeding, cardiopulmonary events, and death [6]. Furthermore, when ERCP-related complications occur, they are often associated with worse clinical outcomes and longer hospital stays in elderly patients [7]. In this context, extending the stent exchange interval to 6 to 12 months may help reduce the cumulative procedural burden in selected elderly or high-risk patients. Several studies have reported acceptable long-term stent patency with on-demand exchange beyond 6 or even 12 months [8,9,10], whereas a randomized trial demonstrated that scheduled 3-month exchanges significantly reduced the incidence of cholangitis [11]. However, most of the available data are from retrospective or heterogeneous cohorts, and prospective studies evaluating long-term stent patency, particularly in elderly patients, remain scarce.
This study therefore aimed to evaluate the 12-month patency and clinical outcomes of PS in elderly patients with incompletely cleared CBD stones.
This article is a revised and expanded version of an abstract entitled ‘Long-term patency of plastic stents in elderly patients with common bile duct stones: A prospective pilot study’, which was presented at the International Pancreatobiliary Meeting (IPBM) 2025, Seoul, Korea, in April 2025 [12].
2. Materials and Methods
2.1. Study Design and Population
This prospective pilot study was conducted at Daegu Catholic University Medical Center. Although the first procedure among eligible patients was performed in March 2023 as part of routine clinical care, patients were considered enrolled in the study only after providing written informed consent during their first outpatient follow-up visit, in accordance with the IRB-approved protocol. Therefore, the actual enrollment period was from April 2023 to December 2023, and patients were followed for up to 12 months after enrollment, with the final follow-up completed in December 2024. Patients who underwent ERCP with PS placement for CBD stones were considered for inclusion. Eligible patients were adults aged 70 years or older, with CBD stones confirmed by imaging, and in whom stone extraction was not attempted during the index ERCP. Stone removal was not attempted in patients with large or multiple common bile duct stones in combination with either significant comorbidities or antiplatelet therapy.
Patients were excluded if they were unable to attend regular outpatient follow-up for at least six months, had biliary obstruction due to malignancy such as cholangiocarcinoma or pancreatic cancer, or had benign strictures related to conditions such as primary sclerosing cholangitis or chronic pancreatitis. Patients who underwent infundibulotomy during stent placement were also excluded.
All patients received a bile acid combination therapy consisting of UDCA and chenodeoxycholic acid (CDCA) (CnU, Daewoong Pharmaceutical Co., Ltd., Seoul, Korea), administered orally at a dose of one tablet three times daily throughout the follow-up period, as part of the study protocol.
The study protocol was reviewed and approved by the Institutional Review Board (IRB) of Daegu Catholic University Medical Center (IRB number: 2023-03-005). Written informed consent for study participation, including prospective follow-up and bile acid therapy, was obtained after the procedure but prior to study enrollment. Transportation costs were reimbursed using research funds in accordance with the approved study protocol.
2.2. Procedure
All procedures were performed using a side-viewing duodenoscope (JF-260V or TJF-260V, Olympus, Tokyo, Japan) under conscious sedation with intravenous midazolam and pethidine. In cases where patients had large or multiple CBD stones in combination with either significant comorbidities or were receiving antiplatelet therapy, the endoscopist determined that complete stone extraction posed a high procedural risk or was technically infeasible [1]. In such cases, endoscopic sphincterotomy was intentionally omitted, and a 7 Fr, 5 cm double pigtail plastic stent (Advanix™; Boston Scientific, Natick, MA, USA) was placed for biliary drainage. After the procedure, patients were monitored for immediate post-procedural complications and were observed for one to two days. They were discharged once clinically stable.
2.3. Outcome Measurement
Baseline data, including demographics, comorbidities, use of antithrombotic agents, laboratory findings, and imaging results, were collected at the time of enrollment. Patients were followed at 3-month intervals with blood tests, including complete blood count (CBC) and liver function tests, as well as abdominal radiographs to assess stent position and function. The primary outcome was stent patency at 12 months, which was defined as the continued presence of a functioning stent without clinical evidence of dysfunction. Stent dysfunction was defined as the occurrence of acute cholangitis or acute cholecystitis resulting from stent occlusion or migration. The diagnostic criteria for acute cholangitis and cholecystitis were based on the Tokyo Guidelines [13]. The secondary outcome was the occurrence of ERCP-related adverse events, including post-ERCP pancreatitis (PEP), bleeding, and perforation.
2.4. Statistical Analysis
The initial target sample size was 80 patients, based on an expected 6-month stent patency rate of 95%, as estimated from the previous literature and institutional experience. Using a 95% confidence level, a 5% margin of error, and an assumed 10% dropout rate, the required sample size was calculated accordingly. However, due to challenges in patient enrollment, particularly because patients with large or multiple CBD stones who were considered unsuitable for removal were less common than initially expected, only 12 patients were ultimately included during the study period. In light of this limitation, the study was redefined and reported as a prospective pilot study to explore the feasibility and describe the outcomes of long-term plastic stenting.
Descriptive statistics were used to summarize baseline characteristics and outcomes. Continuous variables were presented as medians with interquartile ranges (IQRs), and categorical variables as frequencies with percentages. Kaplan–Meier analysis was performed to estimate stent patency over time. Statistical analyses were conducted using IBM SPSS Statistics for Windows, version 26.0 (IBM Corp., Armonk, NY, USA).
3. Results
3.1. Study Flow and Baseline Characteristics
A total of 12 patients underwent biliary plastic stenting with double pigtail PS (7 Fr, 5 cm). Two patients were lost to follow-up, resulting in a final analysis cohort of 10 patients (dropout rate: 16.7%) (Figure 1). Baseline characteristics are summarized in Table 1. The median age was 85 years (IQR 79–86), with five male patients (50%). The median body mass index (BMI) was 24.4 kg/m2 (IQR 20.8–26.2). Hypertension was the most common comorbidity (60%), followed by diabetes mellitus (40%), ischemic heart disease (40%), and cerebrovascular accident (30%). Most patients (80%) were taking aspirin, and one patient (10%) was on clopidogrel. The median diameter of the largest common bile duct stone was 16.5 mm (IQR 11.9–21.4), and the median number of stones was three (IQR 2–4). Laboratory values at baseline showed a median white blood cell count of 14,000/μL, aspartate aminotransferase 81 U/L, alanine aminotransferase 81 U/L, total bilirubin 2.5 mg/dL, alkaline phosphatase 170 U/L, and gamma-glutamyl transferase 270 U/L.
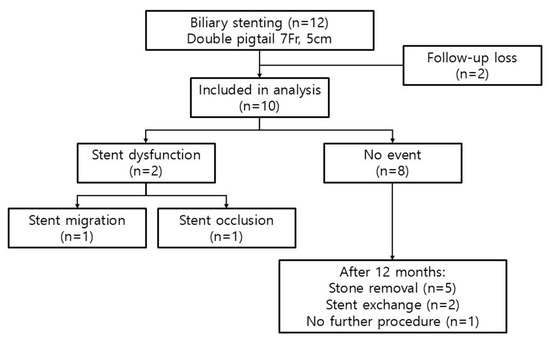
Figure 1.
Patient flow and clinic al outcomes. Of 12 patients who received biliary stenting, 10 were included in the final analysis. Two experienced early stent dysfunctions, and eight had no events. At 12 months, five underwent stone removal, two had elective stent exchange, and one was managed with observation.

Table 1.
Baseline characteristics of patients who underwent ERCP.
3.2. Stent-Related Events and Patency
Over a median follow-up of 9.4 months, two patients experienced stent-related complications. One patient developed cholangitis due to stent migration at 1.4 months after the initial ERCP, while another developed cholangitis due to stent occlusion at 2.7 months. Both underwent successful stent exchange without further adverse events. Kaplan–Meier analysis of stent patency showed a patency rate of 90.0% at 1.4 months and 80.0% at 2.7 months, which remained unchanged through 12 months (Figure 2). It showed that all adverse events occurred within the first 3 months, and the patency remained stable thereafter, with no dysfunctions observed between 3 and 12 months.
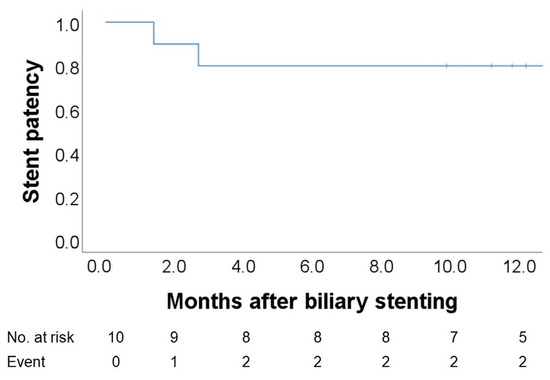
Figure 2.
Kaplan–Meier curve of 12-month stent patency. Stent patency was 90% at 1.4 months and 80% at 2.7 months after stent placement, with no additional events observed during the remainder of the 12-month follow-up.
3.3. Clinical Course and Adverse Events
The clinical course during the follow-up period is shown in Figure 1. Of the ten patients included in the final analysis, two experienced stent dysfunctions, while the remaining eight showed no evidence of stent dysfunction. At 12 months, one of the eight patients declined to undergo further ERCP and was instead followed conservatively through outpatient monitoring, with plans for intervention only if symptoms developed. The remaining seven patients underwent elective ERCP for stent exchange. Among them, five showed significant stone fragmentation or size reduction, allowing for successful stone removal. No ERCP-related adverse events such as PEP, cholangitis, bleeding, or perforation were observed during the follow-up period. Detailed individual data, including baseline characteristics, stent-related events, and 12-months outcomes, are presented in Table 2. Of the seven patients who underwent follow-up ERCP, five achieved complete stone removal, while two underwent stent exchange due to incomplete clearance.

Table 2.
Individual patient outcomes following plastic biliary stenting.
4. Discussion
Current ESGE guidelines recommend that PS be exchanged within 3–6 months to minimize the risk of infectious complications [1]. However, strict adherence to this schedule may not always be feasible in frail or elderly patients, as the risks associated with repeated ERCP procedures, including bleeding, cardiopulmonary complications, and mortality, are significantly higher in individuals aged 80 years and older [6].
In this study, we evaluated the safety and feasibility of maintaining PSs in elderly patients with difficult CBD stones, particularly when stone removal was deemed high-risk due to comorbidities or general condition. Although patient selection was based on clinical judgment regarding overall status, a formal frailty assessment was not performed, which may have limited the objectivity of risk stratification in this elderly cohort.
This pilot study demonstrated a stent patency rate of 80.0% at 2.7 months, which was maintained throughout 12 months. These findings are consistent with previous studies reporting 6-month patency rates between 88.0% and 94.0%, and 12-month rates ranging from 75.4% to 79.0% [8,10,14]. Notably, all stent-related complications in this study occurred within the first three months after plastic stent placement, suggesting that this may represent a high-risk period for dysfunction.
The mechanism of PS occlusion involves early bacterial colonization and biofilm formation, leading to luminal narrowing and irregular stent surfaces that promote biliary sludge accumulation [15]. This process begins within 4 to 8 weeks after placement and forms the theoretical basis for recommending stent exchange every three months [16]. In this study, only one patient experienced early occlusion, and no additional events occurred thereafter. Although the small sample size limits generalizability, our findings suggest that stent occlusion tends to occur during an early high-risk period, and that once this window passes, the progression of biofilm and sludge accumulation may slow, resulting in a plateau phase with stable long-term patency.
Double pigtail stents are generally considered less prone to migration than straight stents due to their anchoring loops, whereas straight stents align with the bile duct axis and are more susceptible to distal migration [17,18]. Duodenal perforation, although rare, has been more frequently reported with straight stents and is thought to result from such migration [17]. For these reasons, a double pigtail stent was used in all patients in this study. Only one case of early migration was observed, while all other stents remained in place throughout the follow-up period. This pattern is hypothesized to reflect similar dynamics to occlusion, in which early intraductal pressure elevation due to biofilm or sludge may predispose to migration but a more stable state is subsequently achieved.
Among the eight patients with stents in place at 12 months, seven consented to ERCP. Five of these showed significant stone size reduction with fragmentation, allowing for successful stone clearance. Several studies have demonstrated that delayed stone removal after plastic stenting can be effective [4,19]. One study reported that patients receiving UDCA in addition to stenting had higher stone clearance rates at 3 months compared to stenting alone (93.8% vs. 84.4%) [4]. In our cohort, all patients received a combination of UDCA and CDCA, and five of seven patients achieved successful stone removal. These findings support the viability of prolonged stenting followed by interval stone extraction in selected cases.
Based on these observations, we propose a risk-adapted follow-up strategy. Rather than performing routine 3-month exchanges in all patients, clinicians could consider intensive monitoring during the first 1 to 2 months, such as monthly laboratory tests and imaging. If no signs of stent dysfunction are observed during this period, the stent duration may be safely extended to 6 to 12 months before elective exchange or stone removal. This approach may help reduce procedural burden while maintaining safety in appropriately selected patients.
5. Limitations
This study has several limitations. First, although originally designed with a target sample size of 80 patients, only 12 were ultimately enrolled due to recruitment challenges. As such, the study was conducted and interpreted as a pilot. Second, the small sample size limits the ability to draw definitive conclusions. Due to the limited sample size, multivariate analysis to adjust for potential confounding variables could not be performed. Third, as a single-center study, the findings may not be generalizable to other settings. Lastly, several study protocol-related factors may have limited the comprehensiveness of data collection and interpretation. For example, follow-up imaging relied solely on plain radiographs, which may have underestimated subtle stent dysfunction. Hepatotoxicity monitoring and evaluation of potential drug interactions between bile acid therapy and antiplatelet use were not conducted. Additionally, microbiological analysis of occluded stents was not performed, limiting insight into infection-related mechanisms.
Importantly, the absence of a control group, such as patients undergoing routine stent exchange, precludes direct comparison and weakens the ability to draw firm conclusions regarding the safety and feasibility of long-term stent retention. However, it is worth noting that the follow-up strategy used in this study reflects real-world clinical practice, which may enhance the applicability of our findings to similar patient populations.
6. Conclusions
In conclusion, this pilot study suggests that long-term stent patency may be achievable in selected patients, particularly when early stent-related complications are absent. A follow-up strategy emphasizing early intensive monitoring followed by individualized stent management may represent a safe and cost-effective alternative to routine short-interval exchanges. Larger, multicenter prospective studies are warranted to confirm these findings and further refine risk-based follow-up protocols.
Author Contributions
Conceptualization, J.H. and H.T.J.; methodology, J.H.; formal analysis, H.T.J.; investigation, H.T.J. and G.H.Y.; resources, J.H.; data curation, H.T.J. and G.H.Y.; writing—original draft preparation, H.T.J.; writing—review and editing, H.T.J., G.H.Y., and J.H.; visualization, H.T.J. and G.H.Y.; supervision, J.H.; project administration, J.H.; funding acquisition, H.T.J. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Research Institute of Medical Science, Daegu Catholic University, grant number RD-23-0023.
Institutional Review Board Statement
The study protocol was reviewed and approved by the Institutional Review Board (IRB) of Daegu Catholic University Medical Center (IRB number 2023-03-005 and date of approval 12 April 2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author due to privacy restrictions.
Acknowledgments
This work was supported by a grant from the Research Institute of Medical Science, Daegu Catholic University (2023) [20].
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| ERCP | Endoscopic retrograde cholangiopancreatography |
| ESGE | European Society of Gastrointestinal Endoscopy |
| CBD | Common bile duct |
| PS | Plastic stent |
| UDCA | Ursodeoxycholic acid |
| CDCA | Chenodeoxycholic acid |
| CBD | Complete blood count |
| PEP | Post-ERCP pancreatitis |
| SSR | Successful stone removal |
| SE | Stent exchange |
References
- Manes, G.; Paspatis, G.; Aabakken, L.; Anderloni, A.; Arvanitakis, M.; Ah-Soune, P.; Barthet, M.; Domagk, D.; Dumonceau, J.M.; Gigot, J.F.; et al. Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy 2019, 51, 472–491. [Google Scholar] [CrossRef] [PubMed]
- Tringali, A.; Costa, D.; Fugazza, A.; Colombo, M.; Khalaf, K.; Repici, A.; Anderloni, A. Endoscopic management of difficult common bile duct stones: Where are we now? A comprehensive review. World J. Gastroenterol. 2021, 27, 7597–7611. [Google Scholar] [CrossRef] [PubMed]
- Horiuchi, A.N.Y.; Kajiyama, M.; Kato, N.; Kamijima, T.; Graham, D.Y.; Tanaka, N. Biliary stenting in the management of large or multiple common bile duct stones. Gastrointest. Endosc. 2010, 71, 1200–1203. [Google Scholar] [CrossRef] [PubMed]
- Hormati, A.; Ghadir, M.R.; Sarkeshikian, S.S.; Alemi, F.; Moghaddam, M.; Ahmadpour, S.; Mohammadbeigi, A.; Sivandzadeh, G.R. Adding ursodeoxycholic acid to the endoscopic treatment and common bile duct stenting for large and multiple biliary stones: Will it improve the outcomes? BMC Gastroenterol. 2020, 20, 374. [Google Scholar] [CrossRef] [PubMed]
- Dumonceau, J.M.; Kapral, C.; Aabakken, L.; Papanikolaou, I.S.; Tringali, A.; Vanbiervliet, G.; Beyna, T.; Dinis-Ribeiro, M.; Hritz, I.; Mariani, A.; et al. ERCP-related adverse events: European Society of Gastrointestinal Endoscopy (ESGE). Guidel. Endosc. 2020, 52, 127–149. [Google Scholar] [CrossRef] [PubMed]
- Day, L.W.; Lin, L.; Somsouk, M. Adverse events in older patients undergoing ERCP: A systematic review and meta-analysis. Endosc. Int. Open 2014, 2, E28–E36. [Google Scholar] [CrossRef] [PubMed]
- Cagir, Y.; Durak, M.B.; Simsek, C.; Yuksel, I. Comparison of ERCP Outcomes and Complication Risk between Elderly and Younger Patients: A Large Single-Center Study. J. Clin. Med. 2024, 13, 6112. [Google Scholar] [CrossRef] [PubMed]
- Akazawa, Y.; Ohtani, M.; Nosaka, T.; Saito, Y.; Takahashi, K.; Naito, T.; Ofuji, K.; Matsuda, H.; Hiramatsu, K.; Nemoto, T.; et al. Long-term prognosis after biliary stenting for common bile duct stones in high-risk elderly patients. J. Dig. Dis. 2018, 19, 626–634. [Google Scholar] [CrossRef] [PubMed]
- Sbeit, W.; Khoury, T.; Kadah, A.; MLivovsky, D.; Nubani, A.; Mari, A.; Goldin, E.; Mahamid, M. Long-Term Safety of Endoscopic Biliary Stents for Cholangitis Complicating Choledocholithiasis: A Multi-Center Study. J. Clin. Med. 2020, 9, 2953. [Google Scholar] [CrossRef] [PubMed]
- Li, K.W.; Zhang, X.W.; Ding, J.; Chen, T.; Wang, J.; Shi, W.J. A prospective study of the efficacy of endoscopic biliary stenting on common bile duct stones. J. Dig. Dis. 2009, 10, 328–331. [Google Scholar] [CrossRef] [PubMed]
- Di Giorgio, P.M.G.; Grimaldi, E.; Schettino, M.; D’Alessandro, A.; Di Giorgio, A.; Giannattasio, F. Endoscopic plastic stenting for bile duct stones: Stent changing on demand or every 3 months. A prospective comparison study. Endoscopy 2013, 45, 1014–1017. [Google Scholar] [CrossRef] [PubMed]
- Jeong, H.T.; Yim, G.H.; Han, J.M. Long-term patency of plastic stents in elderly patients with common bile duct stones: A prospective pilot study. In Proceedings of the International Pancreatobiliary Meeting (IPBM) 2025, Seoul, Republic of Korea, 4–5 April 2025; p. 377. [Google Scholar]
- Kiriyama, S.; Kozaka, K.; Takada, T.; Strasberg, S.M.; Pitt, H.A.; Gabata, T.; Hata, J.; Liau, K.H.; Miura, F.; Horiguchi, A.; et al. Tokyo Guidelines 2018: Diagnostic criteria and severity grading of acute cholangitis (with videos). J. Hepatobiliary Pancreat. Sci. 2018, 25, 17–30. [Google Scholar] [CrossRef] [PubMed]
- Slattery, E.; Kale, V.; Anwar, W.; Courtney, G.; Aftab, A.R. Role of long-term biliary stenting in choledocholithiasis. Dig. Endosc. 2013, 25, 440–443. [Google Scholar] [CrossRef] [PubMed]
- Kwon, C.I.; Lehman, G.A. Mechanisms of Biliary Plastic Stent Occlusion and Efforts at Prevention. Clin. Endosc. 2016, 49, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Donelli, G.; Guaglianone, E.; Di Rosa, R.; Fiocca, F.; Basoli, A. Plastic biliary stent occlusion: Factors involved and possible preventive approaches. Clin. Med. Res. 2007, 5, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Qu, J.; Li, K. Duodenal perforations secondary to a migrated biliary plastic stent successfully treated by endoscope: Case-report and review of the literature. BMC Gastroenterol. 2020, 20, 149. [Google Scholar] [CrossRef] [PubMed]
- Emara, M.H.; Ahmed, M.H.; Mohammed, A.S.; Radwan, M.I.; Mahros, A.M. Biliary stent migration: Why, how, and what? Eur. J. Gastroenterol. Hepatol. 2021, 33, 967–973. [Google Scholar] [CrossRef] [PubMed]
- Ye, X.; Huai, J.; Sun, X. Effectiveness and safety of biliary stenting in the management of difficult common bile duct stones in elderly patients. Turk. J. Gastroenterol. 2016, 27, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Korean Pancreatobiliary Association. In In Proceedings of the Presented at the International Pancreatobiliary Meeting (IPBM 2025), Seoul, Republic of Korea, 4–5 April 2025.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).