Comparing Close-Field and Open-Field Autorefractometry and Subjective Refraction
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample and Inclusion Criteria
2.2. Study Design
2.2.1. NVision-K 5001
2.2.2. Visionix VX120
2.2.3. Subjective Refraction
2.3. Statistical Analysis
3. Results
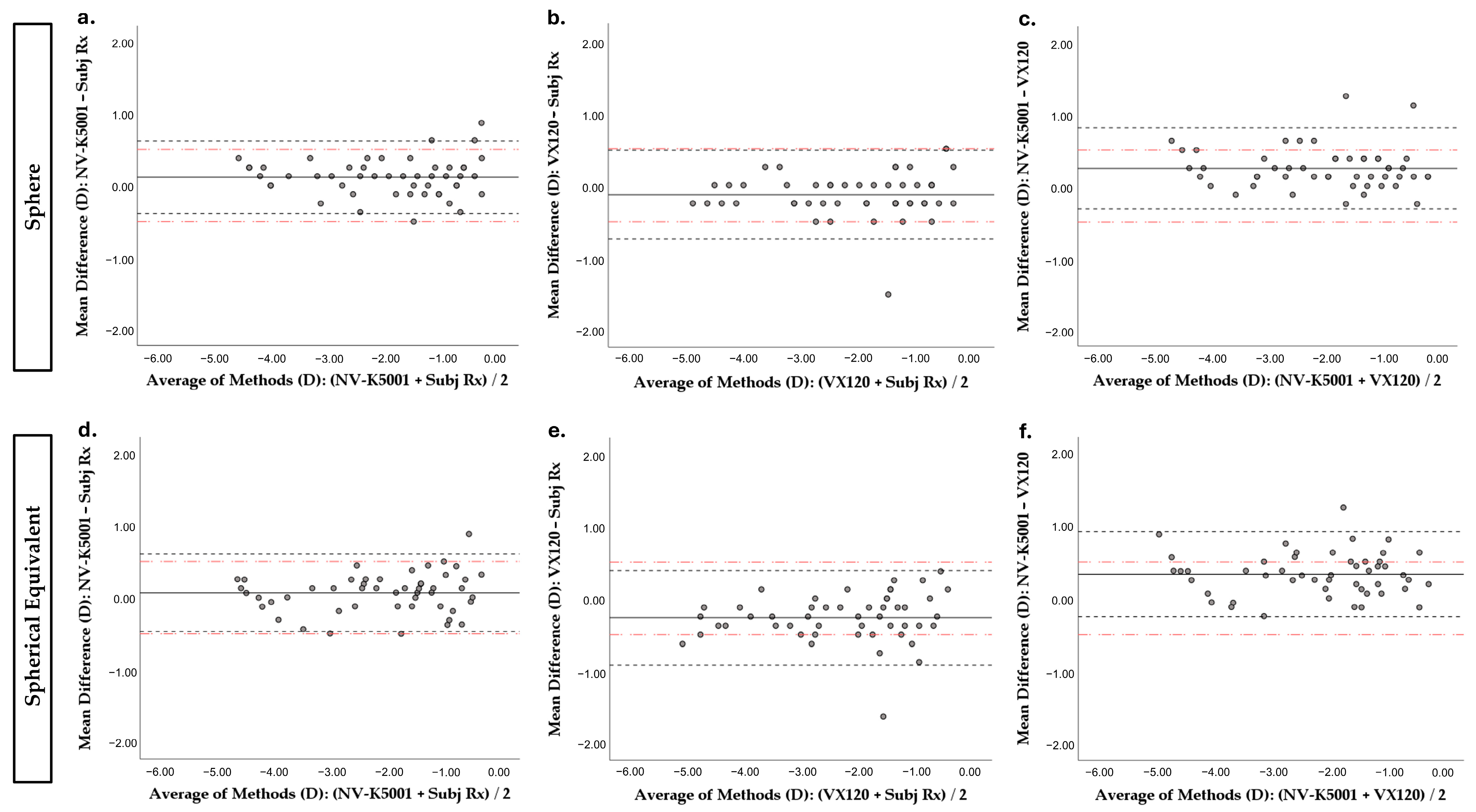
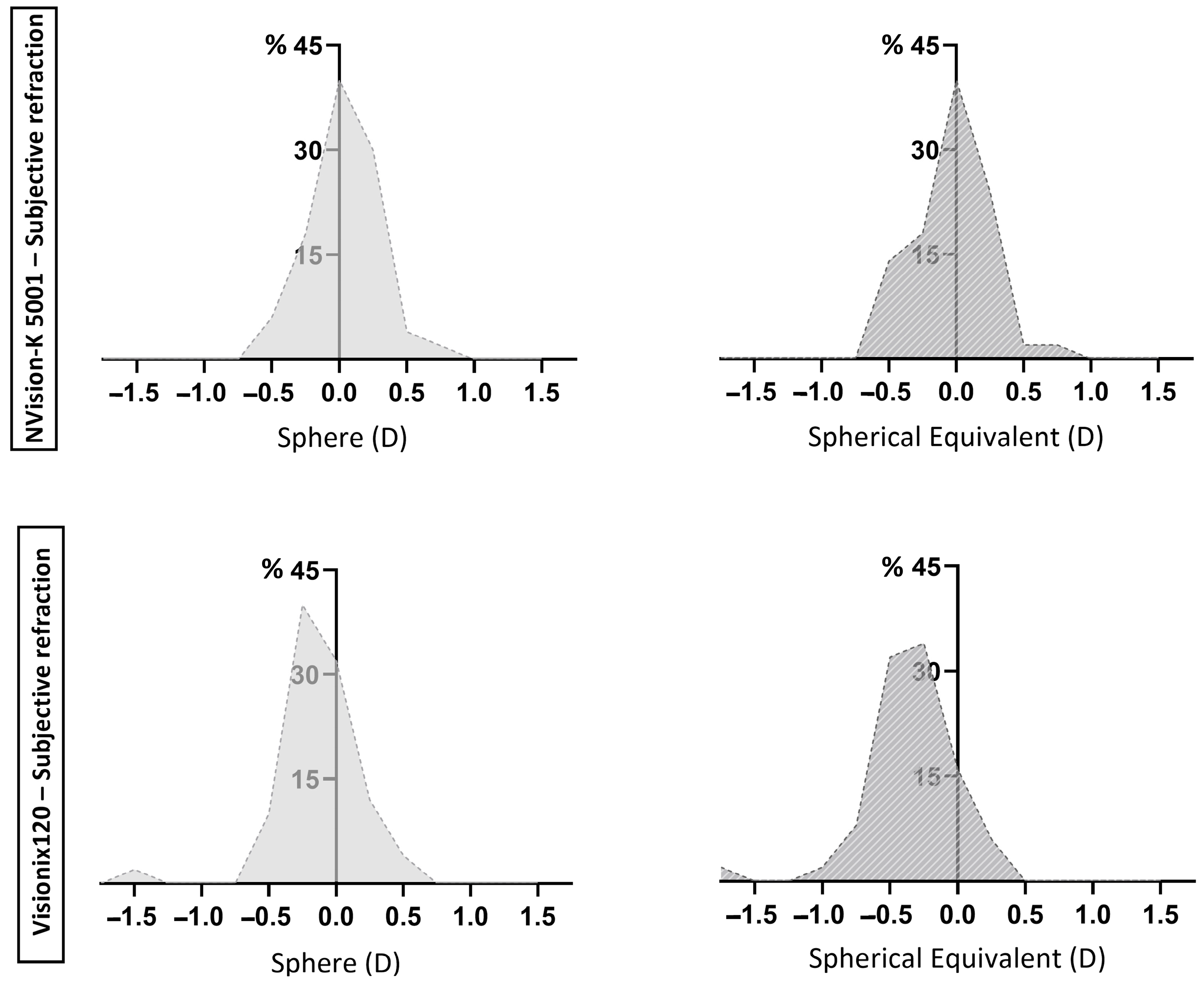
3.1. Differences Between Refractive Procedures for Sphere Value
3.2. Differences Between Refractive Procedures for SE Value
3.3. Differences Between Refractive Procedures for Jackson Cross-Cylinders at 0° and 45°
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BCVA | Best Corrected Visual Acuity |
| IQR | Interquartile Range |
| J0 vector | cylindrical vector at 0° |
| J45 vector | cylindrical vector at 45° |
| SE | spherical equivalent |
| 95% LoAs | 95% Limits of Agreement |
References
- Cleary, G.; Spalton, D.J.; Patel, P.M.; Lin, P.F.; Marshall, J. Diagnostic accuracy and variability of autorefraction by the Tracey Visual Function Analyzer and the Shin-Nippon NVision-K 5001 in relation to subjective refraction. Ophthalmic Physiol. Opt. 2009, 29, 173–181. [Google Scholar] [CrossRef]
- Calvo-Maroto, A.M.; Llorente-Gonzalez, S.; Bezunartea-Bezunartea, J.; Hurtado-Cena, F.J.; Berrozpe-Villabona, C.; Bilbao-Malave, V.; Pinero, D.P.; Barrio-Barrio, J.; Recalde-Maestre, S. Comparative Study of Refraction between Wave Front-Based Refraction and Autorefraction without and with Cycloplegia in Children and Adolescents. Children 2022, 9, 88. [Google Scholar] [CrossRef]
- Metsing, I.T.; Jacobs, W.; Hansraj, R. A review of vision screening methods for children. Afr. Vis. Eye Health 2018, 77, a446. [Google Scholar] [CrossRef]
- Vasudevan, B.; Esposito, C.; Peterson, C.; Coronado, C.; Ciuffreda, K.J. Under-correction of human myopia--is it myopigenic?: A retrospective analysis of clinical refraction data. J. Optom. 2014, 7, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Jonas, J.B.; Ang, M.; Cho, P.; Guggenheim, J.A.; He, M.G.; Jong, M.; Logan, N.S.; Liu, M.; Morgan, I.; Ohno-Matsui, K.; et al. IMI Prevention of Myopia and Its Progression. Investig. Ophthalmol. Vis. Sci. 2021, 62, 6. [Google Scholar] [CrossRef]
- Rotsos, T.; Grigoriou, D.; Kokkolaki, A.; Manios, N. A comparison of manifest refractions, cycloplegic refractions and retinoscopy on the RMA-3000 autorefractometer in children aged 3 to 15 years. Clin. Ophthalmol. 2009, 3, 429–431. [Google Scholar] [CrossRef] [PubMed]
- Mukash, S.N.; Kayembe, D.L.; Mwanza, J.C. Agreement Between Retinoscopy, Autorefractometry and Subjective Refraction for Determining Refractive Errors in Congolese Children. Clin. Optom. 2021, 13, 129–136. [Google Scholar] [CrossRef]
- Davies, L.N.; Mallen, E.A.; Wolffsohn, J.S.; Gilmartin, B. Clinical evaluation of the Shin-Nippon NVision-K 5001/Grand Seiko WR-5100K autorefractor. Optom. Vis. Sci. 2003, 80, 320–324. [Google Scholar] [CrossRef]
- Gammoh, Y.; Morjaria, P.; Block, S.; Massie, J.; Hendicott, P. 2023 Global Survey of Optometry: Defining Variations of Practice, Regulation and Human Resources Between Countries. Clin. Optom. 2024, 16, 211–220. [Google Scholar] [CrossRef]
- Gopalakrishnan, A.; Hussaindeen, J.R.; Chaudhary, R.; Ramakrishnan, B.; Arunachalam, S.; Balakrishnan, A.C.; Sri, J.S.D.; Sahoo, M.; Robin, S.; Varsaharinya, M.; et al. Results of the School Children Ocular Biometry and Refractive Error Study in South India. Turk. J. Ophthalmol. 2022, 52, 412–420. [Google Scholar] [CrossRef]
- Lee, L.; Burnett, A.M.; D’Esposito, F.; Fricke, T.; Nguyen, L.T.; Vuong, D.A.; Nguyen, H.T.T.; Yu, M.; Nguyen, N.V.M.; Huynh, L.P.; et al. Indicators for Assessing the Quality of Refractive Error Care. Optom. Vis. Sci. 2021, 98, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Wosik, J.; Patrzykont, M.; Pniewski, J. Comparison of refractive error measurements by three different models of autorefractors and subjective refraction in young adults. J. Opt. Soc. Am. A 2019, 36, B1–B6. [Google Scholar] [CrossRef]
- Gordon-Shaag, A.; Piñero, D.P.; Kahloun, C.; Markov, D.; Parnes, T.; Gantz, L.; Shneor, E. Validation of refraction and anterior segment parameters by a new multi-diagnostic platform (VX120). J. Optom. 2018, 11, 242–251. [Google Scholar] [CrossRef]
- Turull-Mallofre, A.; Garcia-Guerra, C.E.; Mestre, C.; Vilaseca, M.; Pujol, J.; Aldaba, M. Influence of power and the time of application of fogging lenses on accommodation. Biomed. Opt. Express 2023, 14, 5488–5498. [Google Scholar] [CrossRef]
- Ponce-Garcia, V.; Silva-Viguera, M.C.; Garcia-Romera, M.C.; Guerra-Sancho, Y.; Heredia-Rios, N.; Bautista-Llamas, M.J. Validation and evaluation of visual acuity and contrast sensitivity with a new digital device: OPTOTAB®+. Ophthalmic Physiol. Opt. 2025. Online ahead of print. [Google Scholar] [CrossRef]
- Armstrong, R.A. Statistical guidelines for the analysis of data obtained from one or both eyes. Ophthalmic Physiol. Opt. 2013, 33, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Thibos, L.N.; Wheeler, W.; Horner, D. Power vectors: An application of Fourier analysis to the description and statistical analysis of refractive error. Optom. Vis. Sci. 1997, 74, 367–375. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, R.A.; Davies, L.N.; Dunne, M.C.; Gilmartin, B. Statistical guidelines for clinical studies of human vision. Ophthalmic Physiol. Opt. 2011, 31, 123–136. [Google Scholar] [CrossRef]
- Armstrong, R.A. When to use the Bonferroni correction. Ophthalmic Physiol. Opt. 2014, 34, 502–508. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef]
- Hashemi, H.; Asharlous, A.; Jamali, A.; Mortazavi, A.; Hashemi, A.; Khabazkhoob, M. Auto-refraction versus subjective refraction in different phakic and pseudophakic conditions: The Tehran Geriatric Eye Study (TGES). Int. J. Ophthalmol. 2023, 16, 1309–1316. [Google Scholar] [CrossRef] [PubMed]
- Farook, M.; Venkatramani, J.; Gazzard, G.; Cheng, A.; Tan, D.; Saw, S.M. Comparisons of the handheld autorefractor, table-mounted autorefractor, and subjective refraction in Singapore adults. Optom. Vis. Sci. 2005, 82, 1066–1070. [Google Scholar] [CrossRef] [PubMed]
- Choong, Y.F.; Chen, A.H.; Goh, P.P. A comparison of autorefraction and subjective refraction with and without cycloplegia in primary school children. Am. J. Ophthalmol. 2006, 142, 68–74. [Google Scholar] [CrossRef]
- van der Zee, C.; Jamal, H.; Muijzer, M.; Frank, L.; Vink, G.; Wisse, R. Real world data on digital remote refraction in a healthy population of 14,680 eyes. npj Digit. Med. 2025, 8, 89. [Google Scholar] [CrossRef]
- Mathebula, S.D.; Rubin, A. Interexaminer reproducibility for subjective refractions for an ametropic participant. BMJ Open Ophthalmol. 2022, 7, e000954. [Google Scholar] [CrossRef]
- Wilson, S.; Ctori, I.; Shah, R.; Suttle, C.; Conway, M.L. Systematic review and meta-analysis on the agreement of non-cycloplegic and cycloplegic refraction in children. Ophthalmic Physiol. Opt. 2022, 42, 1276–1288. [Google Scholar] [CrossRef]
- Sheppard, A.L.; Davies, L.N. Clinical evaluation of the Grand Seiko Auto Ref/Keratometer WAM-5500. Ophthalmic Physiol. Opt. 2010, 30, 143–151. [Google Scholar] [CrossRef]
- Queirós, A.; González-Méijome, J.; Jorge, J. Influence of fogging lenses and cycloplegia on open-field automatic refraction. Ophthalmic Physiol. Opt. 2008, 28, 387–392. [Google Scholar] [CrossRef]
- Queirós, A.; Jorge, J.; González-Méijome, J.M. Influence of Fogging Lenses and Cycloplegia on Peripheral Refraction. J. Optom. 2009, 2, 83–89. [Google Scholar] [CrossRef][Green Version]
- Mallen, E.A.; Gilmartin, B.; Wolffsohn, J.S.; Tsujimura, S. Clinical evaluation of the Shin-Nippon SRW-5000 autorefractor in adults: An update. Ophthalmic Physiol. Opt. 2015, 35, 622–627. [Google Scholar] [CrossRef] [PubMed]
- Nagra, M.; Akhtar, A.; Huntjens, B.; Campbell, P. Open versus closed view autorefraction in young adults. J. Optom. 2021, 14, 86–91. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Median [IQR] | Range | p a |
|---|---|---|---|
| Sphere value (D) | <0.001 * | ||
| NV-K 5001 | −1.62 [1.91] | −4.37 to 0.12 | |
| VX120 | −2.00 [2.06] | −5.00 to −0.25 | |
| Subj Rx | −1.62 [1.87] | −4.75 to −0.25 | |
| SE value (D) | <0.001 * | ||
| NV-K 5001 | −1.71 [1.95] | −4.50 to −0.12 | |
| VX120 | −2.12 [1.91] | −5.38 to −0.38 | |
| Subj Rx | −1.75 [1.72] | −4.75 to −0.50 | |
| J0 vector | 0.434 | ||
| NV-K 5001 | 0.00 [0.30] | −0.68 to 0.62 | |
| VX120 | 0.02 [0.23] | −0.44 to 0.46 | |
| Subj Rx | 0.00 [0.04] | −0.37 to 0.32 | |
| J45 vector | 0.166 | ||
| NV-K 5001 | 0.00 [0.11] | −0.32 to 0.61 | |
| VX120 | −0.02 [0.34] | −0.48 to 0.36 | |
| Subj Rx | 0.00 [0.10] | −0.25 to 0.25 |
| Variable | p | Adjusted p a |
|---|---|---|
| Sphere value | ||
| VX120—Subj Rx | 0.011 | 0.032 * |
| VX120—NV-K5001 | <0.001 | 0.001 * |
| Subj Rx—NV-K5001 | 0.007 | 0.021 * |
| SE value | ||
| VX120—Subj Rx | <0.001 | 0.001 * |
| VX120—NV-K5001 | <0.001 | 0.001 * |
| Subj Rx—NV-K5001 | 0.064 | 0.193 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Noya-Padin, V.; Nores-Palmas, N.; Sabucedo-Villamarin, B.; Giraldez, M.J.; Yebra-Pimentel, E.; Pena-Verdeal, H. Comparing Close-Field and Open-Field Autorefractometry and Subjective Refraction. J. Clin. Med. 2025, 14, 5680. https://doi.org/10.3390/jcm14165680
Noya-Padin V, Nores-Palmas N, Sabucedo-Villamarin B, Giraldez MJ, Yebra-Pimentel E, Pena-Verdeal H. Comparing Close-Field and Open-Field Autorefractometry and Subjective Refraction. Journal of Clinical Medicine. 2025; 14(16):5680. https://doi.org/10.3390/jcm14165680
Chicago/Turabian StyleNoya-Padin, Veronica, Noelia Nores-Palmas, Belen Sabucedo-Villamarin, Maria J. Giraldez, Eva Yebra-Pimentel, and Hugo Pena-Verdeal. 2025. "Comparing Close-Field and Open-Field Autorefractometry and Subjective Refraction" Journal of Clinical Medicine 14, no. 16: 5680. https://doi.org/10.3390/jcm14165680
APA StyleNoya-Padin, V., Nores-Palmas, N., Sabucedo-Villamarin, B., Giraldez, M. J., Yebra-Pimentel, E., & Pena-Verdeal, H. (2025). Comparing Close-Field and Open-Field Autorefractometry and Subjective Refraction. Journal of Clinical Medicine, 14(16), 5680. https://doi.org/10.3390/jcm14165680








