Maxillary Sinus Puncture: A Traditional Procedure in Decline—Insights from SHIP
Abstract
1. Introduction
- SHIP-START: The original cohort with baseline data collected between 1997 and 2001, followed by START-2 (2008–2012) and START-3 (2014–2016);
- SHIP-TREND: An independent cohort established in 2008 (TREND-0: 2008–2012) to refresh the population sample;
- SHIP-NEXT: Launched in 2021 but excluded from this analysis due to ongoing data collection.
Objective
2. Materials and Methods
2.1. Study Design and Population
- SHIP-START, the first cohort, with baseline data collected in 1997–2001 (START-0; n = 4308). We used follow-up data from START-2 (2008–2012; n = 2333) and START-3 (2014–2016; n = 1717);
- SHIP-TREND-0, the baseline data of an independent second cohort recruited in the same region (2008–2012; n = 4420).
2.2. Assessment of Sinonasal History and Interventions
- Have you ever had your nasal septum straightened? (0 = no, 1 = yes);
- If yes, when? (open-ended response);
- Have you ever undergone a maxillary sinus puncture?* (0 = no, 1 = yes);
- If yes, when? (open-ended response);
- Have you ever had surgery on the paranasal sinuses?* (0 = no, 1 = yes);
- If yes, when? (open-ended response).
2.3. Quality-of-Life Instruments
- SNOT-20-D: This 20-item questionnaire evaluates symptom burden and quality-of-life impact in individuals with sinonasal complaints. It includes items on nasal obstruction, facial pressure, and olfactory function. The German version (SNOT-20-D) is a standardized translation of the original SNOT-20 developed by Piccirillo et al. [8] and was the best-available tool at the time of SHIP-START for sinonasal health assessment in a German-speaking population. Higher scores indicate greater symptom severity; a mean score of ≥0.8 was defined as the minimal clinically important difference (MCID);
- EQ-5D-3L: This is a standardized measure of general health across five domains: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Index scores were calculated using German-specific value sets [9,10], with higher values indicating better health. The EQ-5D is validated for use in CRS research and general populations [11];
- SF-12: This a concise, validated tool for assessing subjective physical and mental health. It produces two summary scores (physical and mental component summaries). Higher scores reflect better perceived health status [12].
2.4. Use of AI Tools
2.5. Statistical Analysis
- Years since MSP;
- Age at MSP;
- Interaction: years since × age at MSP;
- Interaction: age at MSP × sex.
3. Results
3.1. Cohort Characteristics and MSP Prevalence
3.2. Longitudinal Consistency and MSP Timing
3.3. Impact of MSP on Quality of Life
4. Discussion
4.1. Significance of the Study
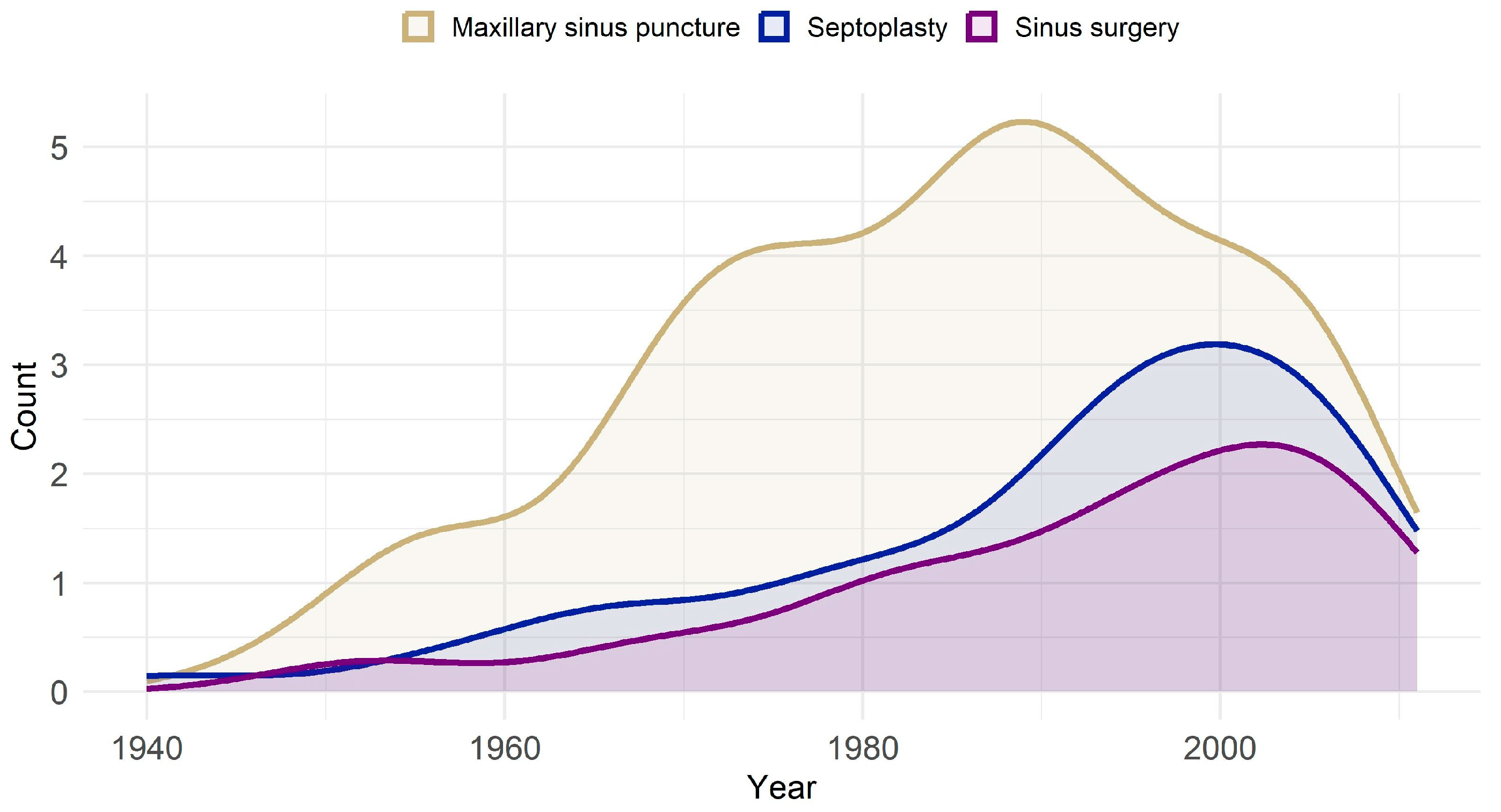
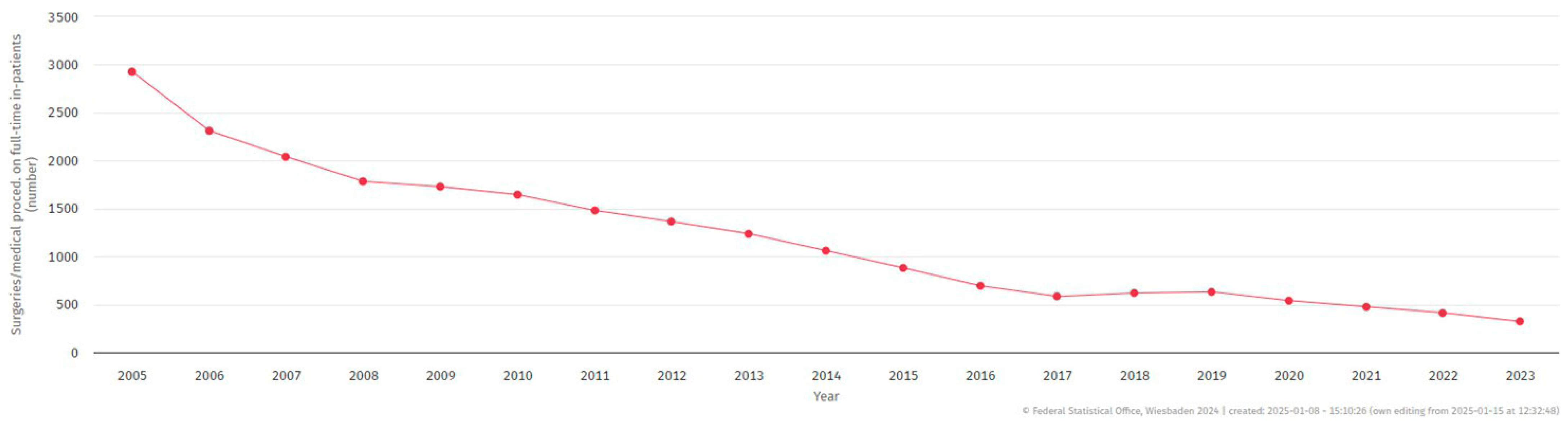
4.2. Historical Trends and Age Distribution
4.3. Reliability of Self-Reported MSP and Recall Bias
4.4. Impact on Quality of Life
4.5. Confounding Variables
4.6. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| MSP | Maxillary Sinus Puncture |
| ARS | Acute Rhinosinusitis |
| CRS | Chronic Rhinosinusitis |
| SNOT-20-D | Sinonasal Outcome Test (20-item, German version) |
| EQ-5D-3L | EuroQol 5-Dimension, 3-Level |
| SF-12 | 12-Item Short Form Health Survey |
| MCID | Minimal Clinically Important Difference |
| SHIP | Study of Health in Pomerania |
| ESS | Endoscopic Sinus Surgery |
| EDMM | Endoscopically Directed Middle Meatal Culture |
| QoL | Quality of Life |
| CI | Confidence Interval |
| OR | Odds Ratio |
| DFG | Deutsche Forschungsgemeinschaft |
| BMBF | Federal Ministry of Education and Research (Germany) |
References
- Benninger, M.S.; Payne, S.C.; Ferguson, B.J.; Hadley, J.A.; Ahmad, N. Endoscopically directed middle meatal cultures versus maxillary sinus taps in acute bacterial maxillary rhinosinusitis: A meta-analysis. Otolaryngol. Neck Surg. 2006, 134, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Mees, K. (Ed.) Die Unspezifische Rhino-Sinusitis: Aktuelle Aspekte zur Konservativen und Operativen Wiederherstellung der Mukoziliaren Clearance; Springer: Berlin/Heidelberg, Germany, 1996. [Google Scholar]
- Kryukov, A.; Tovmasyan, A.; Lapchenko, A.; Bolgar, A.; Kishinevskii, A.; Timofeeva, M.; Artemyeva-Karelova, A.; Ogorodnikov, D. Optimizatsiya metoda punktsionnogo lecheniya ostrogo bakterial’nogo verkhnechelyustnogo sinusita. Vestn. Otorinolaringol. 2024, 89, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Stuck, B.A.; Beule, A.; Jobst, D.; Klimek, L.; Laudien, M.; Lell, M.; Vogl, T.J.; Popert, U. Leitlinie “Rhinosinusitis”—Langfassung: S2k-Leitlinie der Deutschen Gesellschaft für Allgemeinmedizin und Familienmedizin und der Deutschen Gesellschaft für Hals-Nasen-Ohren-Heilkunde, Kopf- undHals-Chirurgie e. V. HNO 2018, 66, 38–74. [Google Scholar] [CrossRef] [PubMed]
- Fokkens, W.; Lund, V.; Hopkins, C.; Hellings, P.; Kern, R.; Reitsma, S.; Toppila-Salmi, S.; Bernal-Sprekelsen, M.; Mullol, J. Executive summary of EPOS 2020 including integrated care pathways. Rhinology 2020, 58, 82–111. [Google Scholar] [CrossRef]
- Völzke, H. Größte Gesundheitsstudie SHIP Startet mit Dritter Basisgruppe und Betritt Neuland in der Bevölkerungs-Forschung. 2021. Available online: https://www2.medizin.uni-greifswald.de/cm/fv/fileadmin/user_upload/ship/dokumente/PI-23-2021-Universitaetsmedizin-Greifswald.pdf (accessed on 10 January 2025).
- Völzke, H.; Schössow, J.; Schmidt, C.O.; Jürgens, C.; Richter, A.; Werner, A.; Werner, N.; Radke, D.; Teumer, A.; Ittermann, T.; et al. Cohort Profile Update: The Study of Health in Pomerania (SHIP). Int. J. Epidemiol. 2022, 51, e372–e383. [Google Scholar] [CrossRef]
- Piccirillo, J.; Merritt, M.; Richards, M. Psychometric and clinimetric validity of the 20-Item Sino-Nasal Outcome Test (SNOT-20). Otolaryngol.–Head Neck Surg. 2002, 126, 41–47. [Google Scholar] [CrossRef]
- Greiner, W.; Claes, C.; Busschbach, J.; Graf von der Schulenburg, J.M. Validating the EQ-5D with time trade off for the German population. Eur. J. Health Econ. 2005, 6, 124–130. [Google Scholar] [CrossRef]
- Konerding, U.; Elkhuizen, S.G.; Faubel, R.; Forte, P.; Malmström, T.; Pavi, E.; Janssen, M.B. The validity of the EQ-5D-3L items: An investigation with type 2 diabetes patients from six European countries. Health Qual. Life Outcomes 2014, 12, 181. [Google Scholar] [CrossRef]
- Lange, B.; Holst, R.; Thilsing, T.; Baelum, J.; Kjeldsen, A. Quality of life and associated factors in persons with chronic rhinosinusitis in the general population: A prospective questionnaire and clinical cross-sectional study. Clin. Otolaryngol. 2013, 38, 474–480. [Google Scholar] [CrossRef]
- Bullinger, M.; Kirchberger, I.; Ware, J. Der deutsche SF-36 Health Survey. J. Public Health 1995, 3, 21–36. [Google Scholar] [CrossRef]
- Orlandi, R.R.; Kingdom, T.T.; Smith, T.L.; Bleier, B.; DeConde, A.; Luong, A.U.; Poetker, D.M.; Soler, Z.; Welch, K.C.; Wise, S.K.; et al. International consensus statement on allergy and rhinology: Rhinosinusitis 2021. Int. Forum Allergy Rhinol. 2021, 11, 213–739. [Google Scholar] [CrossRef]
- Joniau, S.; Vlaminck, S.; van Landuyt, H.; Kuhweide, R.; Dick, C. Microbiology of sinus puncture versus middle meatal aspiration in acute bacterial maxillary sinusitis. Am. J. Rhinol. 2005, 19, 135–140. [Google Scholar] [CrossRef]
- Kim, D.H.; Kim, S.W.; Basurrah, M.A.; Hwang, S.H. Diagnostic Value of Middle Meatal Cultures versus Maxillary Sinus Culture in Acute and Chronic Sinusitis: A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 6069. [Google Scholar] [CrossRef]
- Mendes Neto, J.; Guerreiro, V.; Hirai, E.; Kosugi, E.; Santos, R.; Gregório, L. The role of maxillary sinus puncture on the diagnosis and treatment of patients with hospital-acquired rhinosinusitis. Braz. J. Otorhinolaryngol. 2012, 78, 35–41. [Google Scholar] [CrossRef]
- Hsin, C.-H.; Tsao, C.-H.; Su, M.-C.; Chou, M.-C.; Liu, C.-M. Comparison of maxillary sinus puncture with endoscopic middle meatal culture in pediatric rhinosinusitis. Am. J. Rhinol. 2008, 22, 280–284. [Google Scholar] [CrossRef] [PubMed]
- Benninger, M.; Sedory Holzer, S.; Lau, J. Diagnosis and treatment of uncomplicated acute bacterial rhinosinusitis: Summary of the Agency for Health Care Policy and Research evidence-based report. Otolaryngol.–Head Neck Surg. 2000, 122, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Hosemann, W.; Loew, T.; Forster, M.; Kühnel, T.; Beule, A. Perioperative Schmerzen und Ängste bei endoskopischen Nasennebenhöhleneingriffen mit konventioneller Nasentamponade. Laryngo-Rhino-Otol. 2011, 90, 476–480. [Google Scholar] [CrossRef]
- Erskine, S.; Hopkins, C.; Kumar, N.; Wilson, J.; Clark, A.; Robertson, A.; Kara, N.; Sunkaraneni, V.; Anari, S.; Philpott, C. A cross sectional analysis of a case-control study about quality of life in CRS in the UK; a comparison between CRS subtypes. Rhinol. J. 2016, 54, 311–315. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Plath, M.; Sand, M.; Cavaliere, C.; Plinkert, P.; Baumann, I.; Zaoui, K. Normative data for interpreting the SNOT-22. Acta Otorhinolaryngol. Ital. 2023, 43, 390–399. [Google Scholar] [CrossRef]
- Stjärne, P.; Odebäck, P.; Ställberg, B.; Lundberg, J.; Olsson, P. High costs and burden of illness in acute rhinosinusitis: Real-life treatment patterns and outcomes in Swedish primary care. Prim. Care Respir. J. 2012, 21, 174–179. [Google Scholar] [CrossRef]
- Sathananthar, S.; Nagaonkar, S.; Paleri, V.; Le, T.; Robinson, S.; Wormald, P.J. Canine fossa puncture and clearance of the maxillary sinus for the severely diseased maxillary sinus. Laryngoscope 2005, 115, 1026–1029. [Google Scholar] [CrossRef]
- Garbutt, J.; Spitznagel, E.; Piccirillo, J. Use of the modified SNOT-16 in primary care patients with clinically diagnosed acute rhinosinusitis. Arch. Otolaryngol.–Head Neck Surg. 2011, 137, 792–797. [Google Scholar] [CrossRef]
- Quadri, N.; Lloyd, A.; Keating, K.; Nafees, B.; Piccirillo, J.; Wild, D. Psychometric evaluation of the Sinonasal Outcome Test-16 and activity impairment assessment in acute bacterial sinusitis. Otolaryngol.–Head Neck Surg. 2013, 149, 161–167. [Google Scholar] [CrossRef]
- Al-Asadi, Z.; Cui, R.; Lombardo, D.; Dewey, J.; Ramadan, H.; Makary, C. Impact of recurrent acute rhinosinusitis on quality of life. Int. Forum Allergy Rhinol. 2024, 14, 732–734. [Google Scholar] [CrossRef] [PubMed]
- Shin, Y.H.; Hwang, J.; Kwon, R.; Lee, S.W.; Kim, M.S.; GBD 2019 Allergic Disorders Collaborators; Shin, J.I.; Yon, D.K. Global, regional, and national burden of allergic disorders and their risk factors in 204 countries and territories, from 1990 to 2019: A systematic analysis for the Global Burden of Disease Study 2019. Allergy 2023, 78, 2232–2254. [Google Scholar] [CrossRef] [PubMed]
- Jha, P.; Ranson, M.; Nguyen, S.; Yach, D. Estimates of global and regional smoking prevalence in 1995, by age and sex. Am. J. Public Health 2002, 92, 1002–1006. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Tobacco Product Use Among Adults—United States. 2022. Available online: https://www.cdc.gov/tobacco/php/data-statistics/adult-data-cigarettes/index.html (accessed on 14 January 2025).


| START-2 | |||||||
|---|---|---|---|---|---|---|---|
| Variable | N | Overall | Men | Women | <40 Years | 40–60 Years | >60 Years |
| Sex [women] | 2332 | 1235 (53.0) | – | – | 148 (57.4) | 581 (54.4) | 506 (50.3) |
| Age [years] | 2332 | 57.4 (13.7) | 58.3 (13.8) | 56.5 (13.5) | 35.8 (2.5) | 50.2 (6.1) | 70.5 (6.8) |
| Allergies [yes] | 2309 | 217 (9.4) | 73 (6.7) | 144 (11.8) | 24 (9.3) | 105 (9.9) | 88 (8.9) |
| Current smoking [yes] | 2323 | 484 (20.8) | 232 (21.2) | 252 (20.5) | 81 (31.4) | 309 (29.0) | 94 (9.4) |
| EQ-5D-3L index | 2301 | 0.9 (0.2) | 0.9 (0.1) | 0.9 (0.2) | 0.9 (0.1) | 0.9 (0.1) | 0.9 (0.2) |
| SF12 general health | 2318 | 3.0 (0.7) | 3.0 (0.7) | 3.0 (0.7) | 3.4 (0.7) | 3.1 (0.7) | 2.9 (0.6) |
| SF12 physical health | 2262 | 47.0 (9.1) | 46.9 (9.3) | 47.1 (8.9) | 50.7 (7.0) | 48.5 (8.3) | 44.4 (9.7) |
| SF12 mental health | 2262 | 52.5 (8.7) | 54.0 (7.7) | 51.2 (9.3) | 51.7 (8.6) | 51.9 (8.7) | 53.4 (8.6) |
| SNOT-20-D summary score | 1247 | 13.1 (12.2) | 11.0 (10.5) | 15.1 (13.4) | 15.1 (12.8) | 14.0 (12.8) | 11.2 (10.8) |
| SNOT-20-D mean score | 1247 | 0.7 (0.6) | 0.6 (0.5) | 0.8 (0.7) | 0.8 (0.6) | 0.7 (0.6) | 0.6 (0.5) |
| SNOT-20-D MCID [yes] | 1247 | 407 (32.6) | 161 (26.3) | 246 (38.7) | 66 (43.7) | 226 (34.9) | 115 (25.7) |
| Maxillary sinus puncture [yes] | 2306 | 258 (11.2) | 116 (10.7) | 142 (11.6) | 9 (3.5) | 111 (10.5) | 138 (14.0) |
| Age at puncture [years] | 218 | 35.7 (15.8) | 37.7 (17.9) | 34.2 (13.6) | 26.8 (5.4) | 30.7 (12.1) | 40.2 (17.3) |
| Time since puncture [years] | 218 | 25.1 (15.2) | 25.7 (16.7) | 24.6 (14.0) | 9.1 (5.2) | 20.7 (12.5) | 29.7 (15.9) |
| TREND-0 | |||||||
| Variable | N | Overall | Men | Women | < 40 years | 40–60 years | > 60 years |
| Sex [women] | 4420 | 2275 (51.5) | – | – | 582 (53.8) | 990 (52.1) | 703 (48.9) |
| Age [years] | 4420 | 52.0 (15.5) | 52.6 (15.7) | 51.3 (15.2) | 31.4 (5.1) | 50.3 (6.1) | 69.6 (5.7) |
| Allergies [yes] | 4248 | 1245 (29.3) | 443 (21.4) | 802 (36.8) | 372 (34.8) | 557 (29.8) | 316 (24.1) |
| Current smoking [yes] | 4398 | 1183 (26.9) | 624 (29.3) | 559 (24.7) | 458 (42.5) | 593 (31.2) | 132 (9.3) |
| EQ-5D-3L index | 4369 | 0.9 (0.1) | 0.9 (0.1) | 0.9 (0.2) | 0.9 (0.1) | 0.9 (0.1) | 0.9 (0.2) |
| SF12 general health | 4404 | 3.1 (0.7) | 3.1 (0.7) | 3.0 (0.7) | 3.4 (0.7) | 3.1 (0.7) | 2.8 (0.6) |
| SF12 physical health | 4310 | 47.3 (8.8) | 47.6 (8.7) | 47.0 (9.0) | 51.4 (6.1) | 47.6 (8.6) | 43.7 (9.4) |
| SF12 mental health | 4310 | 52.4 (8.6) | 53.8 (7.9) | 51.2 (9.1) | 51.5 (7.8) | 52.0 (9.0) | 53.8 (8.6) |
| SNOT-20-D summary score | 2422 | 13.8 (12.0) | 12.3 (11.3) | 15.4 (12.4) | 14.2 (12.0) | 14.3 (12.5) | 12.8 (10.9) |
| SNOT-20-D mean score | 2422 | 0.7 (0.6) | 0.6 (0.6) | 0.8 (0.6) | 0.7 (0.6) | 0.7 (0.6) | 0.6 (0.5) |
| SNOT-20-D MCID [yes] | 2422 | 853 (35.2) | 359 (29.5) | 494 (41.0) | 220 (36.7) | 422 (36.0) | 211 (32.5) |
| Maxillary sinus puncture [yes] | 4235 | 401 (9.5) | 182 (8.8) | 219 (10.1) | 35 (3.3) | 186 (10.0) | 180 (13.8) |
| Outcome | Cohort | N (No MSP) | N (MSP) | Estimate [95% CI] | p-Value |
|---|---|---|---|---|---|
| EQ-5D-3L index (β) | START-2 | 1919 | 238 | −0.02 [−0.04; −0.001] | 0.042 |
| TREND-0 | 3692 | 397 | 0.01 [−0.01; 0.02] | 0.324 | |
| SF-12 general health (β) | START-2 | 1932 | 241 | −0.06 [−0.14; 0.03] | 0.193 |
| TREND-0 | 3721 | 400 | −0.05 [−0.11; 0.02] | 0.178 | |
| SF-12 physical health (β) | START-2 | 1883 | 237 | −0.94 [−2.10; 0.22] | 0.112 |
| TREND-0 | 3650 | 392 | −0.81 [−1.66; 0.04] | 0.060 | |
| SF-12 mental health (β) | START-2 | 1883 | 237 | −1.24 [−2.41; −0.07] | 0.039 |
| TREND-0 | 3650 | 392 | −0.36 [−1.25; 0.52] | 0.423 | |
| SNOT-20-D mean score (β) | START-2 | 1051 | 119 | 0.28 [0.17; 0.39] | 8.9 × 10−7 |
| TREND-0 | 2117 | 231 | 0.17 [0.09; 0.25] | 5.6 × 10−5 | |
| SNOT-20-D MCID (OR) | START-2 | 1051 | 119 | 2.41 [1.62; 3.57] | 1.3 × 10−5 |
| TREND-0 | 2117 | 231 | 1.56 [1.18; 2.07] | 5.4 × 10−6 |
| Outcome | Statistic | Time Since Intervention | Age at Intervention | Time × Age Interaction | Age × Sex Interaction |
|---|---|---|---|---|---|
| N | 216 | 216 | 216 | 216 | |
| EQ-5D-3L index | F-value | 2.81 | 2.60 | 0.20 | 1.61 |
| p-value | 0.041 | 0.053 | 0.994 | 0.188 | |
| N | 218 | 218 | 218 | 218 | |
| SF-12 general health | F-value | 0.80 | 2.10 | 0.64 | 0.90 |
| p-value | 0.497 | 0.101 | 0.766 | 0.444 | |
| N | 213 | 213 | 213 | 213 | |
| SF-12 physical health | F-value | 1.24 | 1.51 | 1.18 | 3.05 |
| p-value | 0.296 | 0.214 | 0.309 | 0.030 | |
| N | 213 | 213 | 213 | 213 | |
| SF-12 mental health | F-value | 0.92 | 1.52 | 1.05 | 0.24 |
| p-value | 0.432 | 0.209 | 0.403 | 0.869 | |
| N | 106 | 106 | 106 | 106 | |
| SNOT-20-D summary score | F-value | 0.64 | 1.43 | 0.66 | 0.63 |
| p-value | 0.593 | 0.239 | 0.740 | 0.594 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paperlein, F.; Klinger-König, J.; Busch, C.-J.; Scharf, C.; Beule, A.G. Maxillary Sinus Puncture: A Traditional Procedure in Decline—Insights from SHIP. J. Clin. Med. 2025, 14, 5578. https://doi.org/10.3390/jcm14155578
Paperlein F, Klinger-König J, Busch C-J, Scharf C, Beule AG. Maxillary Sinus Puncture: A Traditional Procedure in Decline—Insights from SHIP. Journal of Clinical Medicine. 2025; 14(15):5578. https://doi.org/10.3390/jcm14155578
Chicago/Turabian StylePaperlein, Fabian, Johanna Klinger-König, Chia-Jung Busch, Christian Scharf, and Achim Georg Beule. 2025. "Maxillary Sinus Puncture: A Traditional Procedure in Decline—Insights from SHIP" Journal of Clinical Medicine 14, no. 15: 5578. https://doi.org/10.3390/jcm14155578
APA StylePaperlein, F., Klinger-König, J., Busch, C.-J., Scharf, C., & Beule, A. G. (2025). Maxillary Sinus Puncture: A Traditional Procedure in Decline—Insights from SHIP. Journal of Clinical Medicine, 14(15), 5578. https://doi.org/10.3390/jcm14155578








