Anterior Redisplacement After Intramedullary Nail Fixation for Trochanteric Femoral Fractures: Incidence and Risk Factors in 598 Older Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics
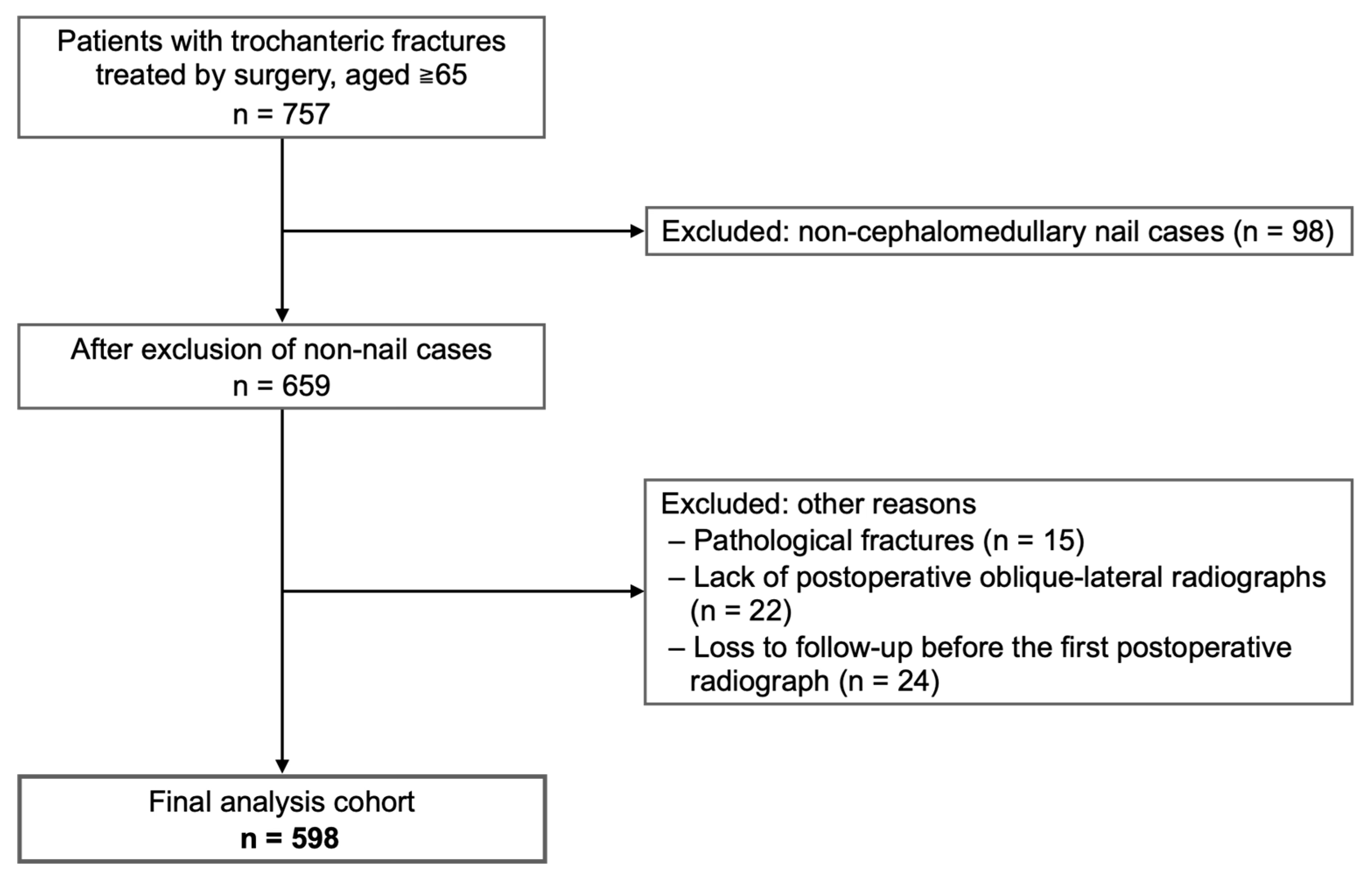
2.2. Study Design, Setting, and Participants
2.3. Surgical Technique
2.4. Radiographic Classification
2.5. Outcomes
2.6. Covariates
2.7. Statistical Analysis
3. Results
3.1. Patient Demographics
3.2. Incidence of Anterior Redisplacement
3.3. Multivariate Analysis
4. Discussion
4.1. Principal Findings
4.2. Pathophysiological Interpretation
4.3. Comparison with Previous Studies
4.4. Clinical Implications: Why a Deliberate Posterior Reduction Deserves Routine Consideration
4.5. Strengths and Limitations
- Single-institution, retrospective cohort—practice patterns may differ elsewhere; selection and information bias cannot be fully excluded;
- Follow-up heterogeneity—although 92% of patients had ≥3 months of imaging data, late attrition may underestimate very delayed redisplacement;
- Unmeasured confounders—bone density, surgeon experience, and rehabilitation protocols were not captured; each could influence stability.These caveats tamper the generalizability of our numeric risk estimates, but not the biomechanical principle that the anteromedial buttress matters;
- Clinical outcomes—functional or symptomatic endpoints—including walking capacity, pain, and quality-of-life scores—were not systematically captured in this retrospective cohort. Although lag-screw cut-out was predefined as a secondary endpoint, no such failures were observed, and postoperative lag-screw telescoping was not quantified. Prospective studies that collect patient-reported outcome measures and correlate them with the degree of anterior redisplacement are therefore warranted.
4.6. Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dong, Y.; Zhang, Y.; Song, K.; Kang, H.; Ye, D.; Li, F. What was the Epidemiology and Global Burden of Disease of Hip Fractures from 1990 to 2019? Results from and Additional Analysis of the Global Burden of Disease Study 2019. Clin. Orthop. Relat. Res. 2023, 481, 1209–1220. [Google Scholar] [CrossRef]
- Shoji, A.; Gao, Z.; Arai, K.; Yoshimura, N. 30-year trends of hip and vertebral fracture incidence in Japan: A systematic review and meta-analysis. J. Bone Miner. Metab. 2022, 40, 327–336. [Google Scholar] [CrossRef] [PubMed]
- Nozaki, A.; Imai, N.; Shobugawa, Y.; Suzuki, H.; Horigome, Y.; Endo, N.; Kawashima, H. Increased incidence among the very elderly in the 2020 Niigata Prefecture Osteoporotic Hip Fracture Study. J. Bone Miner. Metab. 2023, 41, 533–541. [Google Scholar] [CrossRef] [PubMed]
- Hernlund, E.; Svedbom, A.; Ivergard, M.; Compston, J.; Cooper, C.; Stenmark, J.; McCloskey, E.V.; Jonsson, B.; Kanis, J.A. Osteoporosis in the European Union: Medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch. Osteoporos. 2013, 8, 136. [Google Scholar] [CrossRef] [PubMed]
- Kanis, J.A.; Norton, N.; Harvey, N.C.; Jacobson, T.; Johansson, H.; Lorentzon, M.; McCloskey, E.V.; Willers, C.; Borgstrom, F. SCOPE 2021: A new scorecard for osteoporosis in Europe. Arch. Osteoporos. 2021, 16, 82. [Google Scholar] [CrossRef]
- Li, S.; Chang, S.M.; Niu, W.X.; Ma, H. Comparison of tip apex distance and cut-out complications between helical blades and lag screws in intertrochanteric fractures among the elderly: A meta-analysis. J. Orthop. Sci. 2015, 20, 1062–1069. [Google Scholar]
- Inui, T.; Watanabe, Y.; Suzuki, T.; Matsui, K.; Kurata, Y.; Ishii, K.; Kurozumi, T.; Kawano, H. Anterior Malreduction is Associated with Lag Screw Cutout After Internal Fixation of Intertrochanteric Fractures. Clin. Orthop. Relat. Res. 2024, 482, 536–545. [Google Scholar] [CrossRef]
- Moldovan, F. Sterile Inflammatory Response and Surgery-Related Trauma in Elderly Patients with Subtrochanteric Fractures. Biomedicines 2024, 12, 354. [Google Scholar] [CrossRef]
- Chun, Y.S.; Oh, H.; Cho, Y.J.; Rhyu, K.H. Technique and early results of percutaneous reduction of sagittally unstable intertrochateric fractures. Clin. Orthop. Surg. 2011, 3, 217–224. [Google Scholar] [CrossRef]
- Kim, Y.; Dheep, K.; Lee, J.; Yoon, Y.C.; Shon, W.Y.; Oh, C.W.; Oh, J.K. Hook leverage technique for reduction of intertrochanteric fracture. Injury 2014, 45, 1006–1010. [Google Scholar] [CrossRef]
- Qiu, J.; Jiang, Z.; Han, L.; Li, X.; Zhang, R.; Wu, B.; Zhu, F.; Zhao, Y. Treatment of irreducible intertrochanteric femoral fracture with a minimally invasive clamp reduction technique via the anterior approach. J. Orthop. Surg. Res. 2023, 18, 167. [Google Scholar] [CrossRef]
- Takigawa, N.; Moriuchi, H.; Abe, M.; Yasui, K.; Eshiro, H.; Kinoshita, M. Complications and fixation techniques of trochanteric fractures with the TARGON((R)) PF. Injury 2014, 45 (Suppl. 1), S44–S48. [Google Scholar] [CrossRef]
- Tsukada, S.; Okumura, G.; Matsueda, M. Postoperative stability on lateral radiographs in the surgical treatment of pertrochanteric hip fractures. Arch. Orthop. Trauma Surg. 2012, 132, 839–846. [Google Scholar] [CrossRef]
- Chang, S.M.; Zhang, Y.Q.; Du, S.C.; Ma, Z.; Hu, S.J.; Yao, X.Z.; Xiong, W.F. Anteromedial cortical support reduction in unstable pertrochanteric fractures: A comparison of intra-operative fluoroscopy and post-operative three dimensional computerised tomography reconstruction. Int. Orthop. 2018, 42, 183–189. [Google Scholar] [CrossRef]
- Kim, K.H.; Kang, M.S.; Lim, E.J.; Park, M.L.; Kim, J.J. Posterior Sagging After Cephalomedullary Nailing for Intertrochanteric Femur Fracture is Associated with a Separation of the Greater Trochanter. Geriatr. Orthop. Surg. Rehabil. 2020, 11, 2151459320946013. [Google Scholar] [CrossRef] [PubMed]
- Meinberg, E.G.; Agel, J.; Roberts, C.S.; Karam, M.D.; Kellam, J.F. Fracture and Dislocation Classification Compendium—2018. J. Orthop. Trauma 2018, 32 (Suppl. 1), S1–S170. [Google Scholar] [CrossRef] [PubMed]
- Jensen, J.S. Classification of trochanteric fractures. Acta Orthop. Scand. 1980, 51, 803–810. [Google Scholar] [CrossRef]
- Kozono, N.; Ikemura, S.; Yamashita, A.; Harada, T.; Watanabe, T.; Shirasawa, K. Direct reduction may need to be considered to avoid postoperative subtype P in patients with an unstable trochanteric fracture: A retrospective study using a multivariate analysis. Arch. Orthop. Trauma Surg. 2014, 134, 1649–1654. [Google Scholar] [CrossRef] [PubMed]
- Momii, K.; Fujiwara, T.; Mae, T.; Tokunaga, M.; Iwasaki, T.; Shiomoto, K.; Kubota, K.; Onizuka, T.; Miura, T.; Hamada, T.; et al. Risk factors for excessive postoperative sliding of femoral trochanteric fracture in elderly patients: A retrospective multicenter study. Injury 2021, 52, 3369–3376. [Google Scholar] [CrossRef]
- Chang, S.M.; Zhang, Y.Q.; Ma, Z.; Li, Q.; Dargel, J.; Eysel, P. Fracture reduction with positive medial cortical support: A key element in stability reconstruction for the unstable pertrochanteric hip fractures. Arch. Orthop. Trauma Surg. 2015, 135, 811–818. [Google Scholar] [CrossRef]
- Kawamura, T.; Minehara, H.; Tazawa, R.; Matsuura, T.; Sakai, R.; Takaso, M. Biomechanical Evaluation of Extramedullary Versus Intramedullary Reduction in Unstable Femoral Trochanteric Fractures. Geriatr. Orthop. Surg. Rehabil. 2021, 12, 2151459321998611. [Google Scholar] [CrossRef] [PubMed]
- Murena, L.; Moretti, A.; Meo, F.; Saggioro, E.; Barbati, G.; Ratti, C.; Canton, G. Predictors of cut-out after cephalomedullary nail fixation of pertrochanteric fractures: A retrospective study of 813 patients. Arch. Orthop. Trauma Surg. 2018, 138, 351–359. [Google Scholar] [CrossRef]
- Furui, A.; Terada, N.; Mito, K. Mechanical simulation study of postoperative displacement of trochanteric fractures using the finite element method. J. Orthop. Surg. Res. 2018, 13, 300. [Google Scholar] [CrossRef]
- Song, H.; Chang, S.M.; Hu, S.J.; Du, S.C. Low filling ratio of the distal nail segment to the medullary canal is a risk factor for loss of anteromedial cortical support: A case control study. J. Orthop. Surg. Res. 2022, 17, 27. [Google Scholar] [CrossRef]
- Yamamoto, N.; Tsujimoto, Y.; Yokoo, S.; Demiya, K.; Inoue, M.; Noda, T.; Ozaki, T.; Yorifuji, T. Association between Immediate Postoperative Radiographic Findings and Failed Internal Fixation for Trochanteric Fractures: Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 4879. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.Y.; Chang, S.M.; Tuladhar, R.; Wei, Z.; Xiong, W.F.; Hu, S.J.; Du, S.C. A new fluoroscopic view for evaluation of anteromedial cortex reduction quality during cephalomedullary nailing for intertrochanteric femur fractures: The 30 degrees oblique tangential projection. BMC Musculoskelet. Disord. 2020, 21, 719. [Google Scholar] [CrossRef] [PubMed]



| Variable | |
|---|---|
| Number of cases | 598 |
| Sex (female/male) | 444/154 |
| Age, years (mean ± SD) | 85.8 ± 7.5 |
| Comorbidities | |
| Cardiovascular disease | 197 |
| Renal disease | 96 |
| Pulmonary disease | 65 |
| Cerebrovascular disease | 123 |
| Dementia | 151 |
| AO/OTA classification | |
| A1 | 259 |
| A2 | 268 |
| A3 | 71 |
| Evans–Jensen classification | |
| Ⅰ | 23 |
| Ⅱ | 58 |
| Ⅲ | 217 |
| Ⅳ | 13 |
| Ⅴ | 287 |
| Nail length | |
| Short (<230 mm) | 435 |
| Middle (230 to <260 mm) | 98 |
| Long (>260 mm) | 65 |
| Preoperative subtype | |
| Posterior | 109 |
| Anatomical | 151 |
| Anterior | 338 |
| Filling ratio (mean ± SD) | |
| Anteroposterior view | 0.80 ± 0.10 |
| Oblique-lateral view | 0.70 ± 0.10 |
| Variable | All (n = 543) | Posterior (n = 204) | Anatomical (n = 339) | p-Value |
|---|---|---|---|---|
| Sex | 0.02 | |||
| Female | 411 | 166 | 245 | |
| Male | 132 | 38 | 94 | |
| Age, years (mean ± SD) | 85.8 ± 7.6 | 86.2 ± 7.6 | 85.5 ± 7.6 | 0.29 |
| Comorbidities | ||||
| Cardiovascular disease | 181 | 69 | 112 | 0.85 |
| Renal disease | 85 | 33 | 52 | 0.81 |
| Pulmonary disease | 62 | 25 | 37 | 0.68 |
| Cerebrovascular disease | 113 | 45 | 68 | 0.59 |
| Dementia | 141 | 49 | 92 | 0.48 |
| AO/OTA classification | 0.02 | |||
| A1 | 231 | 71 | 160 | |
| A2 | 249 | 105 | 144 | |
| A3 | 63 | 28 | 35 | |
| Evans–Jensen classification | 0.001 | |||
| Ⅰ | 23 | 2 | 21 | |
| Ⅱ | 54 | 14 | 40 | |
| Ⅲ | 185 | 65 | 120 | |
| Ⅳ | 12 | 5 | 7 | |
| Ⅴ | 269 | 118 | 151 | |
| Nail length | 0.001 | |||
| Short (<230 mm) | 390 | 130 | 260 | |
| Middle (230 to <260 mm) | 93 | 50 | 43 | |
| Long (>260 mm) | 60 | 24 | 36 | |
| Filling ratio (mean ± SD) | ||||
| Anteroposterior view | 0.80 ± 0.10 | 0.80 ± 0.10 | 0.81 ± 0.10 | 0.46 |
| Oblique-lateral view | 0.70 ± 0.10 | 0.71 ± 0.10 | 0.70 ± 0.10 | 0.09 |
| Variable | All (n = 543) | Anterior Redisplacement (n = 73) | No Redisplacement (n = 470) | p-Value |
|---|---|---|---|---|
| Sex | 0.77 | |||
| Female | 411 | 54 | 357 | |
| Male | 132 | 19 | 113 | |
| Age, years (mean ± SD) | 85.8 ± 7.6 | 85.4 ± 7.6 | 85.8 ± 7.6 | 0.68 |
| Comorbidities | ||||
| Cardiovascular disease | 181 | 19 | 162 | 0.18 |
| Renal disease | 85 | 13 | 72 | 0.60 |
| Pulmonary disease | 62 | 8 | 54 | 1.0 |
| Cerebrovascular disease | 113 | 16 | 97 | 0.76 |
| Dementia | 141 | 17 | 124 | 0.67 |
| AO/OTA classification | 1.00 | |||
| A1 | 231 | 31 | 200 | |
| A2 | 249 | 34 | 215 | |
| A3 | 63 | 8 | 55 | |
| Evans–Jensen classification | 0.26 | |||
| Ⅰ | 23 | 1 | 22 | |
| Ⅱ | 54 | 5 | 49 | |
| Ⅲ | 185 | 22 | 163 | |
| Ⅳ | 12 | 3 | 9 | |
| Ⅴ | 269 | 42 | 227 | |
| Evans–Jensen classification | 0.12 | |||
| Ⅰ + Ⅱ | 77 | 6 | 71 | |
| Ⅲ − Ⅴ | 469 | 67 | 399 | |
| Nail length | 0.74 | |||
| Short (<230 mm) | 390 | 55 | 335 | |
| Middle (230 to < 260 mm) | 93 | 10 | 83 | |
| Long (>260 mm) | 60 | 8 | 52 | |
| Filling ratio (mean ± SD) | ||||
| Anteroposterior view | 0.80 ± 0.10 | 0.80 ± 0.10 | 0.81 ± 0.09 | 0.67 |
| Oblique-lateral view | 0.70 ± 0.10 | 0.70 ± 0.10 | 0.69 ± 0.09 | 0.39 |
| Preoperative Subtype | Anterior Translation (+) | Anterior Translation (−) | Total | Incidence (%) | p-Value |
|---|---|---|---|---|---|
| Posterior | 6 | 91 | 97 | 6.2% | - |
| Anatomical | 12 | 129 | 141 | 8.5% | - |
| Anterior | 55 | 250 | 305 | 18.0% | 0.0016 |
| Total | 73 | 470 | 543 | 13.4% |
| Preoperative Subtype | Anterior Translation (+) | Anterior Translation (−) | Total | Incidence (%) | p-Value |
|---|---|---|---|---|---|
| Posterior | 7 | 197 | 204 | 3.4% | <0.0001 |
| Anatomical | 66 | 273 | 339 | 19.5% | - |
| Total | 73 | 470 | 543 | 13.4% |
| Variable | OR (95% CI) | p-Value |
|---|---|---|
| Preoperative anterior position (vs. non-anterior) | 1.87 (1.24–2.81) | 0.003 |
| Postoperative anatomical reduction (vs. posterior) | 6.49 (2.92–14.44) | <0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuroda, H.; Yokoo, S.; Okada, Y.; Kondo, J.; Sakagami, K.; Ichikawa, T.; Yamana, K.; Terada, C. Anterior Redisplacement After Intramedullary Nail Fixation for Trochanteric Femoral Fractures: Incidence and Risk Factors in 598 Older Patients. J. Clin. Med. 2025, 14, 5557. https://doi.org/10.3390/jcm14155557
Kuroda H, Yokoo S, Okada Y, Kondo J, Sakagami K, Ichikawa T, Yamana K, Terada C. Anterior Redisplacement After Intramedullary Nail Fixation for Trochanteric Femoral Fractures: Incidence and Risk Factors in 598 Older Patients. Journal of Clinical Medicine. 2025; 14(15):5557. https://doi.org/10.3390/jcm14155557
Chicago/Turabian StyleKuroda, Hironori, Suguru Yokoo, Yukimasa Okada, Junya Kondo, Koji Sakagami, Takahiko Ichikawa, Keiya Yamana, and Chuji Terada. 2025. "Anterior Redisplacement After Intramedullary Nail Fixation for Trochanteric Femoral Fractures: Incidence and Risk Factors in 598 Older Patients" Journal of Clinical Medicine 14, no. 15: 5557. https://doi.org/10.3390/jcm14155557
APA StyleKuroda, H., Yokoo, S., Okada, Y., Kondo, J., Sakagami, K., Ichikawa, T., Yamana, K., & Terada, C. (2025). Anterior Redisplacement After Intramedullary Nail Fixation for Trochanteric Femoral Fractures: Incidence and Risk Factors in 598 Older Patients. Journal of Clinical Medicine, 14(15), 5557. https://doi.org/10.3390/jcm14155557










