Early Rotator Cuff Repair Yields Lower Retear Rates and Superior Functional Outcomes: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
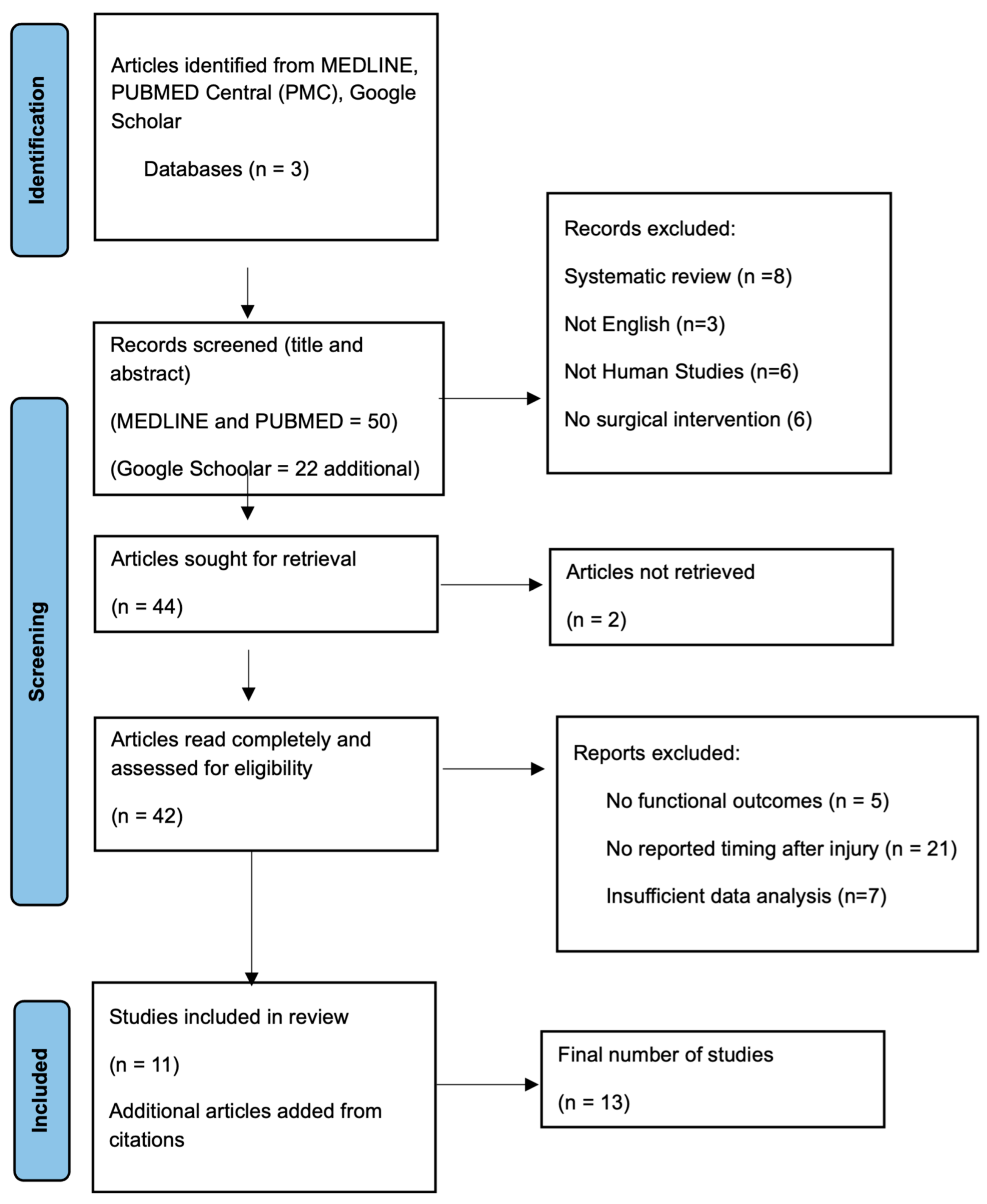
2. Methods
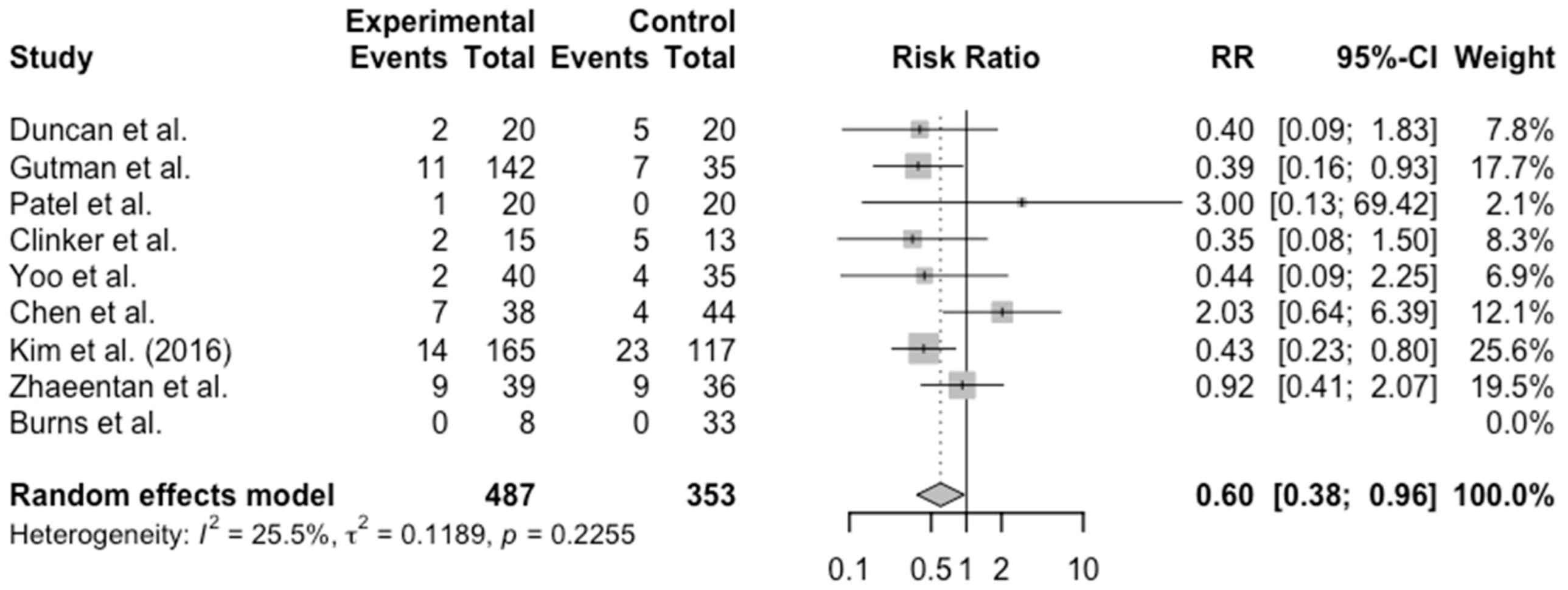
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Colvin, A.C.; Egorova, N.; Harrison, A.K.; Moskowitz, A.; Flatow, E.L. National Trends in Rotator Cuff Repair. J. Bone Jt. Surg. Am. Vol. 2012, 94, 227–233. [Google Scholar] [CrossRef]
- Karjalainen, T.V.; Jain, N.B.; Heikkinen, J.; Johnston, R.V.; Page, C.M.; Buchbinder, R. Surgery for Rotator Cuff Tears. Cochrane Database Syst. Rev. 2019, 12. [Google Scholar] [CrossRef] [PubMed]
- Cvetanovich, G.L.; Gowd, A.K.; Liu, J.N.; Nwachukwu, B.U.; Cabarcas, B.C.; Cole, B.J.; Forsythe, B.; Romeo, A.A.; Verma, N.N. Establishing Clinically Significant Outcome after Arthroscopic Rotator Cuff Repair. J. Shoulder Elbow Surg. 2019, 28, 939–948. [Google Scholar] [CrossRef] [PubMed]
- Harada, N.; Gotoh, M.; Ishitani, E.; Kakuma, T.; Yano, Y.; Tatara, D.; Kawakami, J.; Imai, T.; Karasuyama, M.; Kudoh, Y.; et al. Combination of Risk Factors Affecting Retear after Arthroscopic Rotator Cuff Repair: A Decision Tree Analysis. J. Shoulder Elbow Surg. 2021, 30, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Jeong, H.Y.; Kim, H.J.; Jeon, Y.S.; Rhee, Y.G. Factors Predictive of Healing in Large Rotator Cuff Tears: Is It Possible to Predict Retear Preoperatively? Am. J. Sports Med. 2018, 46, 1693–1700. [Google Scholar] [CrossRef] [PubMed]
- Mukovozov, I.; Byun, S.; Farrokhyar, F.; Wong, I. Time to Surgery in Acute Rotator Cuff Tear: A Systematic Review. Bone Jt. Res. 2013, 2, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Van Der List, J.P.; Kok, L.M.; Alta, T.D.W.; Van Der List, M.P.J.; Van Noort, A. Role of Delay Between Injury and Surgery on the Outcomes of Rotator Cuff Repair: A Systematic Review and Meta-Analysis. Am. J. Sports Med. 2023, 51, 1328–1339. [Google Scholar] [CrossRef] [PubMed]
- Duncan, N.S.; Booker, S.J.; Gooding, B.W.T.; Geoghegan, J.; Wallace, W.A.; Manning, P.A. Surgery within 6 Months of an Acute Rotator Cuff Tear Significantly Improves Outcome. J. Shoulder Elbow Surg. 2015, 24, 1876–1880. [Google Scholar] [CrossRef] [PubMed]
- Gutman, M.J.; Joyce, C.D.; Patel, M.S.; Kirsch, J.M.; Gutman, B.S.; Abboud, J.A.; Namdari, S.; Ramsey, M.L. Early Repair of Traumatic Rotator Cuff Tears Improves Functional Outcomes. J. Shoulder Elbow Surg. 2021, 30, 2475–2483. [Google Scholar] [CrossRef] [PubMed]
- Patel, V.; Thomas, C.; Fort, H.; Wood, R.; Modi, A.; Pandey, R.; Singh, H.; Armstrong, A. Early versus Delayed Repair of Traumatic Rotator Cuff Tears. Does Timing Matter on Outcomes? Eur. J. Orthop. Surg. Traumatol. 2022, 32, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Dimmen, S.; Owesen, C.; Lundgreen, K.; Jenssen, K.K. No Difference in Clinical Outcome after Rotator Cuff Repair Performed within or Later than 3 Months after Trauma: A Retrospective Cohort Study. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 672–680. [Google Scholar] [CrossRef] [PubMed]
- Clinker, C.; Smith, K.M.; Ishikawa, H.; Joyce, C.; Tashjian, R.Z.; Chalmers, P.N. Three-Month Delay in Rotator Cuff Repair: 2-Year Follow-Up. JAAOS Glob. Res. Rev. 2024, 8, e23. [Google Scholar] [CrossRef] [PubMed]
- De Sa, R.; Hassan, A.; Soliman, E.; Al-Yaseen, M.; Kane, P.; Selmi, H.; Makki, D. Traumatic Rotator Cuff Injury: Does Delayed Surgery Worsen Functional Outcomes? Int. Orthop. 2024, 48, 1271–1275. [Google Scholar] [CrossRef] [PubMed]
- Yoo, S.J.; Kang, H.; Kim, B.; Lee, C.H.; Song, J.; Choi, S. Which Is Better? Early versus Delayed Rehabilitation after Arthroscopic Rotator Cuff Repair. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 1049–1057. [Google Scholar] [CrossRef] [PubMed]
- Hantes, M.E.; Karidakis, G.K.; Vlychou, M.; Varitimidis, S.; Dailiana, Z.; Malizos, K.N. A Comparison of Early versus Delayed Repair of Traumatic Rotator Cuff Tears. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 1766–1770. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Chen, S.; Qiao, Y.; Ge, Y.; Li, H.; Chen, J.; Hua, Y.; Li, Y. A Long Preoperative Duration of Symptoms Is Associated with Worse Functional Outcomes After 1-Stage Arthroscopic Treatment of Rotator Cuff Tears with Shoulder Stiffness. Am. J. Sports Med. 2017, 45, 2336–2344. [Google Scholar] [CrossRef] [PubMed]
- Kim, I.-B.; Kim, M.-W. Risk Factors for Retear After Arthroscopic Repair of Full-Thickness Rotator Cuff Tears Using the Suture Bridge Technique: Classification System. Arthrosc. J. Arthrosc. Relat. Surg. 2016, 32, 2191–2200. [Google Scholar] [CrossRef] [PubMed]
- Zhaeentan, S.; Von Heijne, A.; Stark, A.; Hagert, E.; Salomonsson, B. Similar Results Comparing Early and Late Surgery in Open Repair of Traumatic Rotator Cuff Tears. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 3899–3906. [Google Scholar] [CrossRef] [PubMed]
- Petersen, S.A.; Murphy, T.P. The Timing of Rotator Cuff Repair for the Restoration of Function. J. Shoulder Elbow Surg. 2011, 20, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Burns, J.P.; Snyder, S.J. Arthroscopic Rotator Cuff Repair in Patients Younger than Fifty Years of Age. J. Shoulder Elbow Surg. 2008, 17, 90–96. [Google Scholar] [CrossRef] [PubMed]
| Author | Confounding | Selection of Participants | Deviations from Intended Interventions | Missing Data | Measurement of Outcomes | Selection of the Reported Result | Overall Bias | Notes |
|---|---|---|---|---|---|---|---|---|
| Duncan et al. [8] | + | + | + | + | + | + | Low-Risk | |
| Gutman et al. [9] | − | + | + | + | + | + | Mod-risk | Lack of matching |
| Patel et al. [10] | + | + | + | + | + | + | Low-Risk | |
| Dimmen et al. [11] | − | + | + | + | + | + | Mod-risk | Lack of matching |
| Clinker et al. [12] | + | + | + | + | + | + | Low-risk | |
| Sa et al. [13] | − | − | − | + | + | + | High-risk | Lack of matching and variable treatment |
| Yoo et al. [14] | + | + | + | + | + | + | Low-risk | |
| Hantes et al. [15] | + | + | + | + | + | + | Low-Risk | |
| Chen et al. [16] | + | + | ? | + | + | + | Uncertain | Cohort study secondary to results of preliminary study |
| Kim et al. [17] | − | + | + | + | + | + | Mod-risk | Lack of matching |
| Zhaeentan et al. [18] | + | + | + | + | + | + | Low-risk | |
| Petersen et al. [19] | − | − | + | − | + | + | High-risk | Lack of matching and robust statistical analyses |
| Burns et al. [20] | − | + | + | + | + | + | Mod-risk | Lack of matching |
| Study (Author) | Sample Size | Age | Retear Rates | Early/Young Outcomes | Delayed/ Older Outcomes | p-Value | Timing Concl |
|---|---|---|---|---|---|---|---|
| Duncan et al. [8] | 40 total <6 mo—20 >18 mo—20 | Mean age <6 mo—60 >18 mo—60 | 2/20 for <6 mo 5/20 for 18 mo | Change in Oxford score Early—20.3 | Change in Oxford score Delayed—10.4 | p = 0.0014 | Early beneficial |
| Gutman et al. [9] | 206 total 0–2 mo—66 2–4 mo—76 4–6 mo—29 6–12 mo—35 | Mean age 60 | 0–2 mo—6/66 2–4 mo—5/76 4–6 mo—3/29 6–12 mo—7/35 p-value 0.180 (fisher exact) | Change in ASES 0–2 mo—51 2–4 mo—42 | Change in ASES 6–12 mo—32 | p < 0.01 | Early beneficial |
| Patel et al. [10] | 40 total <4 mo—20 >4 mo to 2 yr—20 | <4 mo—65 >4 mo—65 | <4 mo—1/40 | Postop Oxford <4 mo—43 | Postop Oxford >4 mo—45 | p > 0.05 | Early beneficial |
| Dimmen et al. [11] | 358 total <3 mo—77 >3 mo—281 | <3 mo—58 >3 mo—58 | NR | Postop WORC <3 mo—43 | Postop WORC >3 mo—39 | p > 0.05 | No difference in outcomes based on timing |
| Clinker et al. [12] | 30 total <6 weeks—15 >6 weeks—13 | <6 weeks—55 >6 weeks—55 | <6 wks—15% >6 wks—42% Pts loss to follow-up | Difference in ASES <6 wks—51 | Difference in ASES >6 wks—42 | p = 0.07 | Delayed detrimental |
| Sa et al. [13] | 49 total <6 mo—15 >6 mo—34 | <6 mo—56 >6 mo—62 | Oxford improvement <6 mo—23 | Oxford improvement >6 mo—21 | p = 0.50 | No difference in outcomes based on timing | |
| Yoo et al. [14] | 75 total “early”—40 “delayed”—35 | “early”—61.5 “delayed”—63.5 | “early”—2/40 “delayed”—4/35 | Constant score “early”—83 | Constant scores “delayed”—88 | p > 0.05 | No difference in outcomes based on timing |
| Hantes et al. [15] | 35 total <3 wks—15 >3 wks—20 | <3 wks—54 >3 wks—56 | Constant score difference <3 wks—43 | Constant score difference >3 wks—30 | p < 0.05 | Early beneficial | |
| Chen et al. [16] | 82 total <6 mo—38 >6 mo—44 | <6 mo—57 >6 mo—58 | <6 mo—7/38 >6 mo—4/44 p value = 0.22 | ASES <6 mo—91 | ASES >6 mo—82 | p < 0.001 | Delayed detrimental |
| Kim et al. [17] | 282 total | <65 y/o—230 >65 y/o—52 | >12 mo—19.7% <12 mo—8.5% p-value < 0.01 | Delayed detrimental | |||
| Zhaeentan et al. [18] | 75 total <3 mo—39 >3 mo—36 | <3 mo—59 >3 mo—59 | 18/75 | Constant scores <3 mo—68 | Constant scores >3 mo—69 | p > 0.05 | No difference in outcomes based on timing |
| Petersen et al. [19] | 36 total 0–8 wks—15 9–16 wks—15 >16 wks—6 | Avg age 57 | NR | ASES 0–8 wks—82 9–16 wks—79 UCLA 0–8 wks—30 9–16 wks—30 | ASES >16 wks—65 UCLA >16 wks—25 | No stats reported | Early beneficial |
| Burns et al. [20] | Total 41 (avg time to surgery 13 mo) <3 mo—8 >3 mo—33 | Avg age—43.7 | 0/41 | UCLA Postop 32.6 Surgery < 3 mo—32.5 | UCLA Postop Surgery > 3 mo—32.9 | p > 0.05 | Early beneficial |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baur, A.; Lemons, W.; Protzuk, O.; Goodloe, J.B. Early Rotator Cuff Repair Yields Lower Retear Rates and Superior Functional Outcomes: A Systematic Review and Meta-Analysis. J. Clin. Med. 2025, 14, 5552. https://doi.org/10.3390/jcm14155552
Baur A, Lemons W, Protzuk O, Goodloe JB. Early Rotator Cuff Repair Yields Lower Retear Rates and Superior Functional Outcomes: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2025; 14(15):5552. https://doi.org/10.3390/jcm14155552
Chicago/Turabian StyleBaur, Alexander, Wesley Lemons, Omar Protzuk, and Jonathan Brett Goodloe. 2025. "Early Rotator Cuff Repair Yields Lower Retear Rates and Superior Functional Outcomes: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 14, no. 15: 5552. https://doi.org/10.3390/jcm14155552
APA StyleBaur, A., Lemons, W., Protzuk, O., & Goodloe, J. B. (2025). Early Rotator Cuff Repair Yields Lower Retear Rates and Superior Functional Outcomes: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 14(15), 5552. https://doi.org/10.3390/jcm14155552





