Recent Trends in the Management of Varicocele
Abstract
1. Introduction
2. Materials and Methods
3. Potential Links Between Varicocele and Infertility
3.1. Genetic and Molecular Aspects
3.2. Seminal Fluid Analysis
3.3. Antisperm Antibodies
3.4. Sperm DNA Fragmentation (SDF)
4. Novel Trends in Diagnosis of Varicocele
4.1. Grey-Scale Colour Duplex Ultrasound
4.2. Shear-Wave Elastography
5. Novel Trends in the Management of Varicocele
5.1. Prognosis Assessment
5.1.1. Preoperative Hormonal Parameters
5.1.2. Results of Preoperative Ultrasound and Semen Analysis
5.1.3. Scoring Systems, Nomograms, and Inflammatory Markers in Outcome Prediction
5.2. New Indications of Varicocele Treatment
5.2.1. Non-Obstructive Azoospermia (NOA)
5.2.2. Medically Assisted Reproduction (MAR)
5.2.3. Hypogonadism
5.3. Novel Techniques and Methods in Varicocele Treatment
5.3.1. Stem Cell Therapy
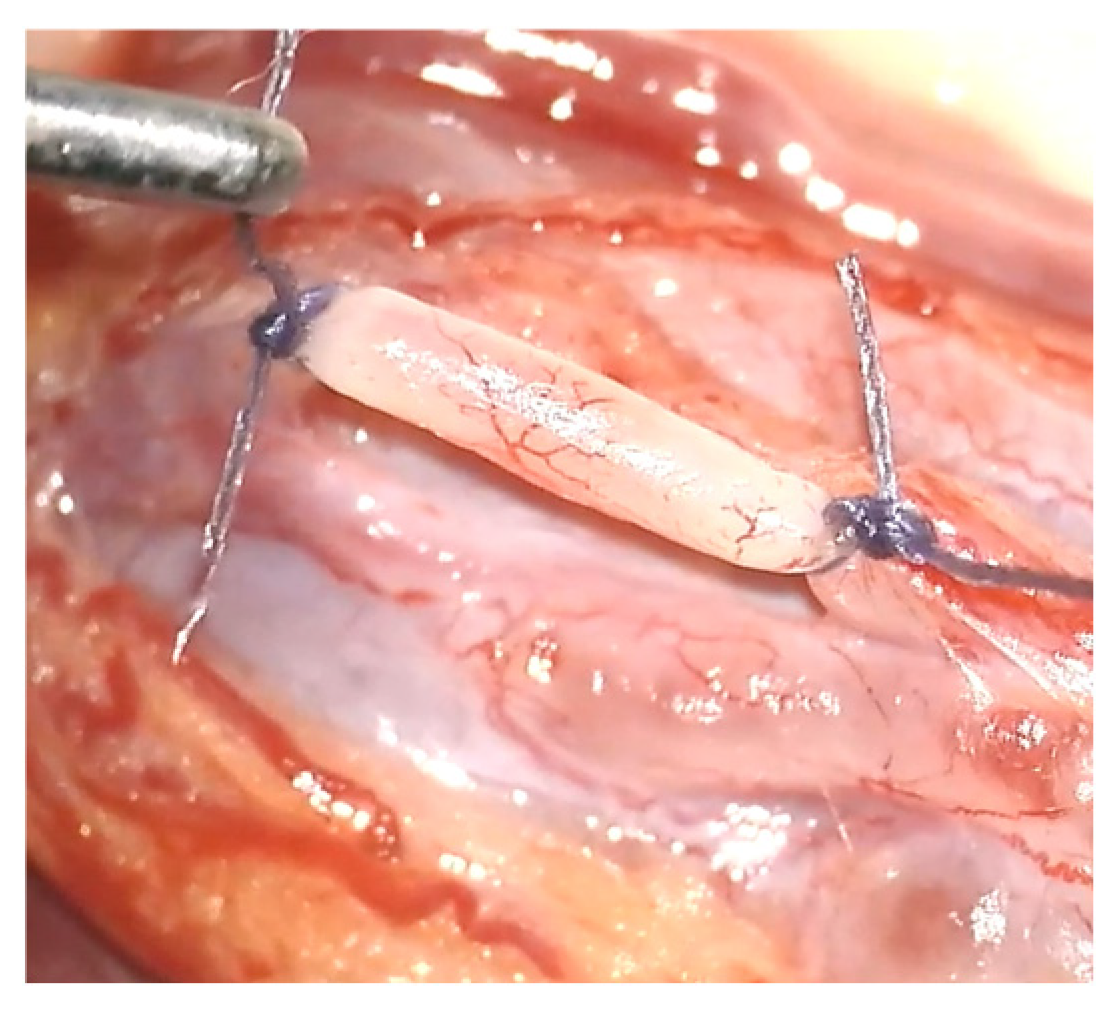
5.3.2. Surgical Techniques
5.3.3. Antioxidant Treatment
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| ASA | Antisperm Antibodies |
| AI | Artificial Intelligence |
| AUA | American Urological Association |
| AUC | Area Under the Curve |
| ARTs | Assisted Reproductive Technologies |
| ASRM | American Society for Reproductive Medicine |
| CFTR | Cystic Fibrosis Transmembrane Conductance Regulator |
| DNA | Deoxyribonucleic Acid |
| EAU | European Association of Urology |
| EAA | European Academy of Andrology |
| ESUR-SPIWG | European Society of Urogenital Radiology-Scrotal and Penile Imaging Working Group |
| FSH | Follicle-Stimulating Hormone |
| hAFMSCs | Human Amniotic Fluid Mesenchymal Stromal Cells |
| hAECs | Human Amniotic Epithelial Cells |
| ICG | Indocyanine Green |
| INSL-3 | Insulin-like 3 |
| IUI | Intrauterine Insemination |
| ICSI | Intracytoplasmic Sperm Injection |
| LH | Luteinizing Hormone |
| MAR | Medically Assisted Reproduction |
| MLR | Monocyte-to-Lymphocyte Ratio |
| miRNA | MicroRNA |
| NOA | Non-Obstructive Azoospermia |
| NLR | Neutrophil-to-Lymphocyte Ratio |
| ROC | Receiver Operating Characteristic |
| SDF | Sperm DNA Fragmentation |
| SII | Systemic Immune-Inflammation Index |
| SIRI | Systemic Inflammatory Response Index |
| SRR | Sperm Retrieval Rate |
| TMSC | Total Motile Sperm Count |
| TPMSC | Total Progressively Motile Sperm Count |
| VITOM | Video Telescopic Operating Microscope |
| WHO | World Health Organization |
References
- Alsaikhan, B.; Alrabeeah, K.; Delouya, G.; Zini, A. Epidemiology of varicocele. Asian J. Androl. 2016, 18, 179–181. [Google Scholar] [CrossRef] [PubMed]
- Minhas, S.; Boeri, L.; Capogrosso, P.; Cocci, A.; Corona, G.; Dinkelman-Smit, M.; Falcone, M.; Jensen, C.F.; Gül, M.; Kalkanli, A.; et al. European Association of Urology Guidelines on Male Sexual and Reproductive Health: 2025 Update on Male Infertility. Eur. Urol. 2025, 87, 601–616. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Gao, Y.; Wang, C.; Liang, M.; Liao, Y.; Hu, K. Role of Oxidative Stress in Varicocele. Front. Genet. 2022, 13, 850114. [Google Scholar] [CrossRef]
- Colpi, G.M.; Francavilla, S.; Haidl, G.; Link, K.; Behre, H.M.; Goulis, D.G.; Krausz, C.; Giwercman, A. European Academy of Andrology guideline Management of oligo-astheno-teratozoospermia. Andrology 2018, 6, 513–524. [Google Scholar] [CrossRef]
- Brannigan, R.E.; Hermanson, L.; Kaczmarek, J.; Kim, S.K.; Kirkby, E.; Tanrikut, C. Updates to Male Infertility: AUA/ASRM Guideline. J. Urol. 2024, 212, 789–799. [Google Scholar] [CrossRef] [PubMed]
- Raman, J.D.; Walmsley, K.; Goldstein, M. Inheritance of varicoceles. Urology 2005, 65, 1186–1189. [Google Scholar] [CrossRef]
- Gökçe, A.; Davarci, M.; Yalçinkaya, F.R.; Güven, E.O.; Kaya, Y.S.; Helvaci, M.R.; Balbay, M.D. Hereditary behavior of varicocele. J. Androl. 2010, 31, 288–290. [Google Scholar] [CrossRef]
- Griffiths, L.; Vasudevan, V.; Myers, A.; Morganstern, B.A.; Palmer, L.S. The role of inheritance in the development of adolescent varicoceles. Transl. Androl. Urol. 2018, 7, 920–925. [Google Scholar] [CrossRef]
- Akkan, S.S.; İzgüt-Uysal, V.N.; Çakır, T.; Özbey, Ö.; Üstünel, İ. The effect of experimental varicocele on the apelin and APJ expressions in rat testis tissue. Tissue Cell 2020, 63, 101318. [Google Scholar] [CrossRef]
- Yang, B.; Yang, Y.; Liu, Y.; Li, H.; Ren, S.; Peng, Z.; Fang, K.; Yang, L.; Dong, Q. Molecular characteristics of varicocele: Integration of whole-exome and transcriptome sequencing. Fertil. Steril. 2021, 115, 363–372. [Google Scholar] [CrossRef]
- Zhang, C.; Li, X.; Chen, J.; Zhao, L.; Wei, X.; Dong, Y.; Sicheng, M.; Sun, Z. Transcriptome and genome sequencing investigating the molecular characteristics of patients with varicocele infertility. Andrologia 2022, 54, e14542. [Google Scholar] [CrossRef]
- Karthikeyan, V.; Vickram, A.S.; Manian, R. Estimation of varicocele associated human ARG2 and NOS1 proteins and computational analysis on the effect of its nsSNPs. Int. J. Biol. Macromol. 2020, 164, 735–747. [Google Scholar] [CrossRef] [PubMed]
- Mostafa, T.; Abdel-Hamid, I.; Taymour, M.; Ali, O. Genetic variants in varicocele-related male infertility: A systematic review and future directions. Hum. Fertil. 2023, 26, 632–648. [Google Scholar] [CrossRef]
- Naderi, N.; Tavalaee, M.; Nasr-Esfahani, M.H. The epigenetic approach of varicocele: A focus on sperm DNA and m6A-RNA methylation. Hum. Reprod. Update 2025, 31, 81–101. [Google Scholar] [CrossRef]
- Longini, M.; Moretti, E.; Signorini, C.; Noto, D.; Iacoponi, F.; Collodel, G. Relevance of seminal F(2)-dihomo-IsoPs, F(2)-IsoPs and F(4)-NeuroPs in idiopathic infertility and varicocele. Prostaglandins Other Lipid Mediat. 2020, 149, 106448. [Google Scholar] [CrossRef]
- El Taieb, M.A.; Hegazy, E.M.; Ibrahim, H.M.; Ibrahim, A.K. Seminal and serum leptin levels in male patients with varicocele and isolated asthenozoospermia before and after repair. Aging Male 2020, 23, 579–584. [Google Scholar] [CrossRef]
- Xu, Y.; Zhang, Y.; Yang, Y.; Liu, X.; Chen, Y. Seminal plasma miR-210-3p is a biomarker for screening dyszoospermia caused by varicocele. Andrologia 2019, 51, e13244. [Google Scholar] [CrossRef]
- Ma, Y.; Zhou, Y.; Xiao, Q.; Zou, S.S.; Zhu, Y.C.; Ping, P.; Chen, X.F. Seminal exosomal miR-210-3p as a potential marker of Sertoli cell damage in Varicocele. Andrology 2021, 9, 451–459. [Google Scholar] [CrossRef]
- Falcone, M.; Bocu, K.; Keskin, H.; Solorzano Vazquez, J.F.; Banthia, R.; Mahendran, T.; Deger, M.D.; Kv, V.; Mirko, P.; Harraz, A.M.; et al. Anti-sperm Antibody Positivity in Men with Varicocele: A Systematic Review and Meta-Analysis. World J. Men’s Health 2025, 43, 60–69. [Google Scholar] [CrossRef] [PubMed]
- Björndahl, L.; Kirkman Brown, J. The sixth edition of the WHO Laboratory Manual for the Examination and Processing of Human Semen: Ensuring quality and standardization in basic examination of human ejaculates. Fertil. Steril. 2022, 117, 246–251. [Google Scholar] [CrossRef] [PubMed]
- Szabó, A.; Váncsa, S.; Hegyi, P.; Váradi, A.; Forintos, A.; Filipov, T.; Ács, J.; Ács, N.; Szarvas, T.; Nyirády, P.; et al. Lifestyle-, environmental-, and additional health factors associated with an increased sperm DNA fragmentation: A systematic review and meta-analysis. Reprod. Biol. Endocrinol. 2023, 21, 5. [Google Scholar] [CrossRef]
- Szabó, A.; Váncsa, S.; Hegyi, P.; Kói, T.; Ács, J.; Hermánné, R.J.; Ács, N.; Szarvas, T.; Nyirády, P.; Kopa, Z. Assessing the efficacy of varicocelectomy, antioxidants, FSH treatment, and lifestyle modifications on sperm DNA fragmentation: A systematic review and meta-analysis. Sci. Rep. 2025, 15, 10118. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, W.; Wu, X.; Liu, G.; Dai, Y.; Jiang, H.; Zhang, X. Effect of varicocele on sperm DNA damage: A systematic review and meta-analysis. Andrologia 2022, 54, e14275. [Google Scholar] [CrossRef]
- Soetandar, A.; Noegroho, B.S.; Siregar, S.; Adriansjah, R.; Mustafa, A. Microsurgical varicocelectomy effects on sperm DNA fragmentation and sperm parameters in infertile male patients: A systematic review and meta-analysis of more recent evidence. Arch. Ital. Urol. Androl. 2022, 94, 360–365. [Google Scholar] [CrossRef]
- Lira Neto, F.T.; Roque, M.; Esteves, S.C. Effect of varicocelectomy on sperm deoxyribonucleic acid fragmentation rates in infertile men with clinical varicocele: A systematic review and meta-analysis. Fertil. Steril. 2021, 116, 696–712. [Google Scholar] [CrossRef]
- Qiu, D.; Shi, Q.; Pan, L. Efficacy of varicocelectomy for sperm DNA integrity improvement: A meta-analysis. Andrologia 2021, 53, e13885. [Google Scholar] [CrossRef]
- Liguori, G.; Trombetta, C.; Garaffa, G.; Bucci, S.; Gattuccio, I.; Salamè, L.; Belgrano, E. Color Doppler ultrasound investigation of varicocele. World J. Urol. 2004, 22, 378–381. [Google Scholar] [CrossRef] [PubMed]
- Hirsh, A.V.; Cameron, K.M.; Tyler, J.P.; Simpson, J.; Pryor, J.P. The Doppler assessment of varicoceles and internal spermatic vein reflux in infertile men. Br. J. Urol. 1980, 52, 50–56. [Google Scholar] [CrossRef]
- Lotti, F.; Frizza, F.; Balercia, G.; Barbonetti, A.; Behre, H.M.; Calogero, A.E.; Cremers, J.F.; Francavilla, F.; Isidori, A.M.; Kliesch, S.; et al. The European Academy of Andrology (EAA) ultrasound study on healthy, fertile men: An overview on male genital tract ultrasound reference ranges. Andrology 2022, 10 (Suppl. S2), 118–132. [Google Scholar] [CrossRef] [PubMed]
- Freeman, S.; Bertolotto, M.; Richenberg, J.; Belfield, J.; Dogra, V.; Huang, D.Y.; Lotti, F.; Markiet, K.; Nikolic, O.; Ramanathan, S.; et al. Ultrasound evaluation of varicoceles: Guidelines and recommendations of the European Society of Urogenital Radiology Scrotal and Penile Imaging Working Group (ESUR-SPIWG) for detection, classification, and grading. Eur. Radiol. 2020, 30, 11–25. [Google Scholar] [CrossRef] [PubMed]
- Lotti, F.; Studniarek, M.; Balasa, C.; Belfield, J.; De Visschere, P.; Freeman, S.; Kozak, O.; Markiet, K.; Ramanathan, S.; Richenberg, J.; et al. The role of the radiologist in the evaluation of male infertility: Recommendations of the European Society of Urogenital Radiology-Scrotal and Penile Imaging Working Group (ESUR-SPIWG) for scrotal imaging. Eur. Radiol. 2025, 35, 752–766. [Google Scholar] [CrossRef]
- Cocuzza, M.S.; Tiseo, B.C.; Srougi, V.; Wood, G.J.A.; Cardoso, J.; Esteves, S.C.; Srougi, M. Diagnostic accuracy of physical examination compared with color Doppler ultrasound in the determination of varicocele diagnosis and grading: Impact of urologists’ experience. Andrology 2020, 8, 1160–1166. [Google Scholar] [CrossRef]
- Lotti, F.; Maggi, M. Ultrasound of the male genital tract in relation to male reproductive health. Hum. Reprod. Update 2015, 21, 56–83. [Google Scholar] [CrossRef] [PubMed]
- Bertolotto, M.; Cantisani, V.; Drudi, F.M.; Lotti, F. Varicocoele. Classification and pitfalls. Andrology 2021, 9, 1322–1330. [Google Scholar] [CrossRef]
- Jain, B.; Gaddi, M.; Nallathambi, N.; Palande, A.; Holebasu, B.; Prasad, R.; Mittal, G. Advanced Sonographic Techniques in the Comprehensive Evaluation and Diagnosis of Male Infertility. Cureus 2024, 16, e62848. [Google Scholar] [CrossRef]
- Kayra, M.V.; Şahin, A.; Toksöz, S.; Serindere, M.; Altıntaş, E.; Özer, H.; Gül, M. Machine learning-based classification of varicocoele grading: A promising approach for diagnosis and treatment optimization. Andrology 2024. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.S.; Chen, L.K. Predictive factors of successful varicocelectomy in infertile patients. Urol. Int. 2011, 86, 320–324. [Google Scholar] [CrossRef]
- Camargo, M.; Intasqui, P.; Belardin, L.B.; Antoniassi, M.P.; Cardozo, K.H.M.; Carvalho, V.M.; Fraietta, R.; Bertolla, R.P. Molecular pathways of varicocele and its repair—A paired labelled shotgun proteomics approach. J. Proteom. 2019, 196, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Fu, W.; Cui, J.; Tang, S. The role of testicular stiffness derived from shear wave elastography in the assessment of spermatogenesis in men with varicocele. Quant. Imaging Med. Surg. 2024, 14, 4987–4997. [Google Scholar] [CrossRef]
- Li, K.; Liu, X.; Huang, Y.; Liu, X.; Song, Q.; Wang, R. Evaluation of testicular spermatogenic function by ultrasound elastography in patients with varicocele-associated infertility. Am. J. Transl. Res. 2021, 13, 9136–9142. [Google Scholar]
- Fuschi, A.; Capone, L.; Abuorouq, S.; Al Salhi, Y.; Velotti, G.; Aversa, S.; Carbone, F.; Maceroni, P.; Petrozza, V.; Carbone, A.; et al. Shear wave elastography in varicocele patients: Prospective study to investigate correlation with semen parameters and histological findings. Int. J. Clin. Pract. 2021, 75, e13699. [Google Scholar] [CrossRef] [PubMed]
- Bello, J.O.; Bhatti, K.H.; Gherabi, N.; Philipraj, J.; Narayan, Y.; Tsampoukas, G.; Shaikh, N.; Papatsoris, A.; Moussa, M.; Buchholz, N. The usefulness of elastography in the evaluation and management of adult men with varicocele: A systematic review. Arab. J. Urol. 2021, 19, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Kroese, A.C.; de Lange, N.M.; Collins, J.; Evers, J.L. Surgery or embolization for varicoceles in subfertile men. Cochrane Database Syst. Rev. 2012, 10, Cd000479. [Google Scholar] [CrossRef] [PubMed]
- Evers, J.H.; Collins, J.; Clarke, J. Surgery or embolisation for varicoceles in subfertile men. Cochrane Database Syst. Rev. 2008, 3, Cd000479. [Google Scholar] [CrossRef]
- Halpern, J.; Mittal, S.; Pereira, K.; Bhatia, S.; Ramasamy, R. Percutaneous embolization of varicocele: Technique, indications, relative contraindications, and complications. Asian J. Androl. 2016, 18, 234–238. [Google Scholar] [CrossRef]
- Liu, Q.; Zhang, X.; Zhou, F.; Xi, X.; Lian, S.; Lian, Q. Comparing Endovascular and Surgical Treatments for Varicocele: A Systematic Review and Meta-Analysis. J. Vasc. Interv. Radiol. 2022, 33, 834–840.e832. [Google Scholar] [CrossRef]
- Agarwal, A.; Cannarella, R.; Saleh, R.; Boitrelle, F.; Gül, M.; Toprak, T.; Salvio, G.; Arafa, M.; Russo, G.I.; Harraz, A.M.; et al. Impact of Varicocele Repair on Semen Parameters in Infertile Men: A Systematic Review and Meta-Analysis. World J. Men’s Health 2023, 41, 289–310. [Google Scholar] [CrossRef]
- Fallara, G.; Capogrosso, P.; Pozzi, E.; Belladelli, F.; Corsini, C.; Boeri, L.; Candela, L.; Schifano, N.; Dehò, F.; Castiglione, F.; et al. The Effect of Varicocele Treatment on Fertility in Adults: A Systematic Review and Meta-analysis of Published Prospective Trials. Eur. Urol. Focus. 2023, 9, 154–161. [Google Scholar] [CrossRef]
- Persad, E.; O’Loughlin, C.A.; Kaur, S.; Wagner, G.; Matyas, N.; Hassler-Di Fratta, M.R.; Nussbaumer-Streit, B. Surgical or radiological treatment for varicoceles in subfertile men. Cochrane Database Syst. Rev. 2021, 4, Cd000479. [Google Scholar] [CrossRef]
- Cayan, S.; Shavakhabov, S.; Kadioğlu, A. Treatment of palpable varicocele in infertile men: A meta-analysis to define the best technique. J. Androl. 2009, 30, 33–40. [Google Scholar] [CrossRef]
- Shah, R.; Agarwal, A.; Kavoussi, P.; Rambhatla, A.; Saleh, R.; Cannarella, R.; Harraz, A.M.; Boitrelle, F.; Kuroda, S.; Hamoda, T.A.A.; et al. Consensus and Diversity in the Management of Varicocele for Male Infertility: Results of a Global Practice Survey and Comparison with Guidelines and Recommendations. World J. Men’s Health 2023, 41, 164–197. [Google Scholar] [CrossRef] [PubMed]
- Okuyama, A.; Fujisue, H.; Matsui, T.; Doi, Y.; Koh, E.; Kondoh, N.; Takeyama, M.; Nakamura, M.; Namiki, M.; Fujioka, H.; et al. Preoperative parameters related to the improvement of semen characteristics after surgical repair of varicocele in subfertile men. Eur. Urol. 1988, 14, 442–446. [Google Scholar] [CrossRef] [PubMed]
- Kondo, Y.; Ishikawa, T.; Yamaguchi, K.; Fujisawa, M. Predictors of improved seminal characteristics by varicocele repair. Andrologia 2009, 41, 20–23. [Google Scholar] [CrossRef] [PubMed]
- Madhusoodanan, V.; Blachman-Braun, R.; Patel, P.; Ji, L.; Masterson, T.A.; Owyong, M.; Greer, A.; Ramasamy, R. Preoperative follicle-stimulating hormone: A factor associated with semen parameter improvement after microscopic subinguinal varicocelectomy. Can. Urol. Assoc. J. 2020, 14, E27–E31. [Google Scholar] [CrossRef]
- Liu, L.; Huang, W.; Luo, K.; Zeng, Y.; Shao, Y.; Long, Z. Relationship between semen parameters, serum InhB, and INSL-3 levels, and the degree of varicocele. Clinics 2024, 79, 100339. [Google Scholar] [CrossRef]
- Samplaski, M.K.; Yu, C.; Kattan, M.W.; Lo, K.C.; Grober, E.D.; Zini, A.; Lau, S.; Jarvi, K.A. Nomograms for predicting changes in semen parameters in infertile men after varicocele repair. Fertil. Steril. 2014, 102, 68–74. [Google Scholar] [CrossRef]
- Takahara, M.; Ichikawa, T.; Shiseki, Y.; Nakamura, T.; Shimazaki, J. Relationship between grade of varicocele and the response to varicocelectomy. Int. J. Urol. 1996, 3, 282–285. [Google Scholar] [CrossRef]
- You, K.; Chen, B.B.; Wang, P.; Bu, R.G.; Xu, X.W. Intense venous reflux, quantified by a new software to analyze presurgical ultrasound, is associated with unfavorable outcomes of microsurgical varicocelectomy. Asian J. Androl. 2023, 25, 119–125. [Google Scholar] [CrossRef]
- Ou, N.; Zhu, J.; Zhang, W.; Liang, Z.; Hu, R.; Song, Y.; Yang, Y.; Liu, X. Bilateral is superior to unilateral varicocelectomy in infertile men with bilateral varicocele: Systematic review and meta-analysis. Andrologia 2019, 51, e13462. [Google Scholar] [CrossRef]
- Kim, H.J.; Seo, J.T.; Kim, K.J.; Ahn, H.; Jeong, J.Y.; Kim, J.H.; Song, S.H.; Jung, J.H. Clinical significance of subclinical varicocelectomy in male infertility: Systematic review and meta-analysis. Andrologia 2016, 48, 654–661. [Google Scholar] [CrossRef] [PubMed]
- Kohn, T.P.; Ohlander, S.J.; Jacob, J.S.; Griffin, T.M.; Lipshultz, L.I.; Pastuszak, A.W. The Effect of Subclinical Varicocele on Pregnancy Rates and Semen Parameters: A Systematic Review and Meta-Analysis. Curr. Urol. Rep. 2018, 19, 53. [Google Scholar] [CrossRef]
- Rodriguez Peña, M.; Alescio, L.; Russell, A.; Lourenco da Cunha, J.; Alzu, G.; Bardoneschi, E. Predictors of improved seminal parameters and fertility after varicocele repair in young adults. Andrologia 2009, 41, 277–281. [Google Scholar] [CrossRef] [PubMed]
- Krausz, C.; Riera-Escamilla, A. Genetics of male infertility. Nat. Rev. Urol. 2018, 15, 369–384. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Liu, D.; Pan, C.; Su, H. Nomogram for Predicting Semen Parameters Improvement after Microscopic Varicocelectomy in Infertile Men with Abnormal Semen Parameters. J. Pers. Med. 2022, 13, 11. [Google Scholar] [CrossRef]
- Shabana, W.; Teleb, M.; Dawod, T.; Elsayed, E.; Desoky, E.; Shahin, A.; Eladl, M.; Sorour, W. Predictors of improvement in semen parameters after varicocelectomy for male subfertility: A prospective study. Can. Urol. Assoc. J. 2015, 9, E579–E582. [Google Scholar] [CrossRef]
- Ren, W.; Qu, J.; Xue, B.; Hu, J.; Zu, X. Infertility duration and pre-operative sperm progressive motility are significant factors of spontaneous pregnancy after varicocele repair. Am. J. Reprod. Immunol. 2020, 84, e13318. [Google Scholar] [CrossRef]
- Enatsu, N.; Yamaguchi, K.; Chiba, K.; Miyake, H.; Fujisawa, M. Clinical outcome of microsurgical varicocelectomy in infertile men with severe oligozoospermia. Urology 2014, 83, 1071–1074. [Google Scholar] [CrossRef]
- Niu, Y.; Wang, D.; Chen, Y.; Pokhrel, G.; Xu, H.; Wang, T.; Wang, S.; Liu, J. Comparison of clinical outcome of bilateral and unilateral varicocelectomy in infertile males with left clinical and right subclinical varicocele: A meta-analysis of randomised controlled trials. Andrologia 2018, 50, e13078. [Google Scholar] [CrossRef] [PubMed]
- D’Andrea, S.; Barbonetti, A.; Castellini, C.; Nolletti, L.; Martorella, A.; Minaldi, E.; Giordano, A.V.; Carducci, S.; Necozione, S.; Francavilla, F.; et al. Left spermatic vein reflux after varicocele repair predicts pregnancies and live births in subfertile couples. J. Endocrinol. Investig. 2019, 42, 1215–1221. [Google Scholar] [CrossRef]
- Crafa, A.; Cannarella, R.; Condorelli, R.A.; Mongioì, L.M.; Vignera, S.; Calogero, A.E. Predictive parameters of the efficacy of varicocele repair: A review. Asian J. Androl. 2024, 26, 441–450. [Google Scholar] [CrossRef]
- Ory, J.; Tradewell, M.B.; Blankstein, U.; Lima, T.F.; Nackeeran, S.; Gonzalez, D.C.; Nwefo, E.; Moryousef, J.; Madhusoodanan, V.; Lau, S.; et al. Artificial Intelligence Based Machine Learning Models Predict Sperm Parameter Upgrading after Varicocele Repair: A Multi-Institutional Analysis. World J. Men’s Health 2022, 40, 618–626. [Google Scholar] [CrossRef] [PubMed]
- Maimaitiming, A.; Muhemaiti, A.; Mulati, Y.; Li, X. Nomograms for Predicting Postoperative Sperm Improvements in Varicocele Patients. Eur. Urol. Open Sci. 2024, 59, 40–48. [Google Scholar] [CrossRef]
- Duran, M.B.; Kizilkan, Y.; Senel, S.; Yikilmaz, T.N.; Toksoz, S. Can preoperative inflammatory markers predict the success of varicocelectomy? Andrologia 2022, 54, e14514. [Google Scholar] [CrossRef]
- Ates, E.; Ucar, M.; Keskin, M.Z.; Gokce, A. Preoperative neutrophil-to-lymphocyte ratio as a new prognostic predictor after microsurgical subinguinal varicocelectomy. Andrologia 2019, 51, e13188. [Google Scholar] [CrossRef]
- Erdogan, O.; Ok, F. The effect of systemic inflammatory index and systemic inflammatory response index on success of varicoselectomy. Urologia 2024, 91, 170–175. [Google Scholar] [CrossRef]
- Liu, L.; Li, J.; Liu, G.; Pan, C.; Bai, S.; Zhan, Y.; Shan, L. Nomogram for predicting spontaneous pregnancy after microscopic varicocelectomy in infertile men with normal hormone. BMC Pregnancy Childbirth 2022, 22, 791. [Google Scholar] [CrossRef]
- Sajadi, H.; Hosseini, J.; Farrahi, F.; Dadkhah, F.; Sepidarkish, M.; Sabbaghian, M.; Eftekhari-Yazdi, P.; Sadighi Gilani, M.A. Varicocelectomy May Improve Results for Sperm Retrieval and Pregnancy Rate in Non-Obstructive Azoospermic Men. Int. J. Fertil. Steril. 2019, 12, 303–305. [Google Scholar] [CrossRef]
- Esteves, S.C.; Miyaoka, R.; Roque, M.; Agarwal, A. Outcome of varicocele repair in men with nonobstructive azoospermia: Systematic review and meta-analysis. Asian J. Androl. 2016, 18, 246–253. [Google Scholar] [CrossRef]
- Abdel-Meguid, T.A. Predictors of sperm recovery and azoospermia relapse in men with nonobstructive azoospermia after varicocele repair. J. Urol. 2012, 187, 222–226. [Google Scholar] [CrossRef] [PubMed]
- Elzanaty, S. Varicocele repair in non-obstructive azoospermic men: Diagnostic value of testicular biopsy—A meta-analysis. Scand. J. Urol. 2014, 48, 494–498. [Google Scholar] [CrossRef] [PubMed]
- Jensen, S.; Ko, E.Y. Varicocele treatment in non-obstructive azoospermia: A systematic review. Arab. J. Urol. 2021, 19, 221–226. [Google Scholar] [CrossRef] [PubMed]
- Ramon, R.; Warli, S.M.; Siregar, G.P.; Prapiska, F.F.; Kadar, D.D.; Tala, M.R.Z. Varicocele repair in improving spermatozoa, follicle-stimulating hormone, and luteinizing hormone parameters in infertile males with azoospermia: A systematic review and meta-analysis. Asian J. Androl. 2024, 26, 628–634. [Google Scholar] [CrossRef] [PubMed]
- Palani, A.; Cannarella, R.; Saleh, R.; Salvio, G.; Harraz, A.M.; Crafa, A.; Bahar, F.; Bocu, K.; Kumar, N.; Kothari, P.; et al. Impact of Varicocele Repair on Assisted Reproductive Technique Outcomes in Infertile Men: A Systematic Review and Meta-Analysis. World J. Men’s Health 2025, 43, 344–358. [Google Scholar] [CrossRef]
- Kirby, E.W.; Wiener, L.E.; Rajanahally, S.; Crowell, K.; Coward, R.M. Undergoing varicocele repair before assisted reproduction improves pregnancy rate and live birth rate in azoospermic and oligospermic men with a varicocele: A systematic review and meta-analysis. Fertil. Steril. 2016, 106, 1338–1343. [Google Scholar] [CrossRef]
- Esteves, S.C.; Roque, M.; Agarwal, A. Outcome of assisted reproductive technology in men with treated and untreated varicocele: Systematic review and meta-analysis. Asian J. Androl. 2016, 18, 254–258. [Google Scholar] [CrossRef]
- Jayadevan, R.; Amighi, A.; Mills, S.; Almuzeni, A.; Nork, J.; Pollard, M.; Kwan, L.; Eleswarapu, S.; Mills, J. Decisional Conflict and Knowledge Among Patients With Varicocele Seeking Treatment for Infertility. Urology 2020, 142, 112–118. [Google Scholar] [CrossRef]
- Gonzalez-Daza, S.J.; Díaz-Hung, A.M.; García-Perdomo, H.A. Association between varicocele and hypogonadism, or erectile dysfunction: A systematic review and meta-analysis. Actas Urol. Esp. Engl. Ed. 2024, 48, 751–759. [Google Scholar] [CrossRef]
- Çayan, S.; Akbay, E.; Saylam, B.; Kadıoğlu, A. Effect of Varicocele and Its Treatment on Testosterone in Hypogonadal Men with Varicocele: Review of the Literature. Balkan Med. J. 2020, 37, 121–124. [Google Scholar] [CrossRef]
- Chen, X.; Yang, D.; Lin, G.; Bao, J.; Wang, J.; Tan, W. Efficacy of varicocelectomy in the treatment of hypogonadism in subfertile males with clinical varicocele: A meta-analysis. Andrologia 2017, 49, e12778. [Google Scholar] [CrossRef]
- Cannarella, R.; Shah, R.; Ko, E.; Kavoussi, P.; Rambhatla, A.; Hamoda, T.A.A.; Saleh, R.; Harraz, A.M.; Calogero, A.E.; Durairajanayagam, D.; et al. Effects of Varicocele Repair on Testicular Endocrine Function: A Systematic Review and Meta-Analysis. World J. Men’s Health 2024, 42, e92. [Google Scholar] [CrossRef] [PubMed]
- Tian, D.; Yang, C.; Xie, B.; Li, H.; Li, J.; Yang, D.; Zhu, Z. Effects of Varicocele Surgical Repair on Serum Hormone and Inhibin B Levels for Patients with Varicocele: A Systematic Review and Meta-Analysis. Am. J. Men’s Health 2023, 17, 15579883231199400. [Google Scholar] [CrossRef]
- Saha, S.; Roy, P.; Corbitt, C.; Kakar, S.S. Application of Stem Cell Therapy for Infertility. Cells 2021, 10, 1613. [Google Scholar] [CrossRef] [PubMed]
- Serefoglu, E.C.; Kolbasi, B.; Bulbul, M.V.; Karabulut, S.; Cakici, C.; Gundogdu Ozdemir, R.Z.; Keskin, I. Therapeutic Effects of Mesenchymal Stem Cell Conditioned Medium in Rat Varicocele Model. World J. Men’s Health 2025, 43, 437–447. [Google Scholar] [CrossRef] [PubMed]
- Peserico, A.; Barboni, B.; Russo, V.; Nardinocchi, D.; Turriani, M.; Cimini, C.; Bernabò, N.; Parolini, O.; Silini, A.R.; Antonucci, I.; et al. AEC and AFMSC Transplantation Preserves Fertility of Experimentally Induced Rat Varicocele by Expressing Differential Regenerative Mechanisms. Int. J. Mol. Sci. 2023, 24, 8737. [Google Scholar] [CrossRef]
- Monje Fuente, S.; Fernández Bautista, B.; Blanco Verdú, M.D.; Bada Bosch, I.; Ortiz Rodríguez, R.; Burgos Lucena, L.; De Agustín, J.C.; Angulo Madero, J.M. Usefulness of indocyanine green in the laparoscopic Palomo technique: A comparative study. Cir. Pediatr. 2024, 37, 127–132. [Google Scholar] [CrossRef]
- Esposito, C.; Borgogni, R.; Chiodi, A.; Cerulo, M.; Autorino, G.; Esposito, G.; Coppola, V.; Del Conte, F.; Di Mento, C.; Escolino, M. Indocyanine green (ICG)-GUIDED lymphatic sparing laparoscopic varicocelectomy in children and adolescents. Is intratesticular injection of the dye safe? A mid-term follow-up study. J. Pediatr. Urol. 2024, 20, 282.e1–282.e6. [Google Scholar] [CrossRef]
- Mohd Hashim, M.H.; Fam, X.I.; Azizi, M.H.; Khoo, H.C.; Shukor, S. Microscopic subinguinal varicocelectomy with video telescopic operating microscope (VITOM) telescope: Outcome analysis. Transl. Androl. Urol. 2024, 13, 560–567. [Google Scholar] [CrossRef] [PubMed]
- Duarsa, G.W.K.; Kloping, Y.P.; Duarsa, G.W.D.; Daryanto, B.; Satyagraha, P. Video-Assisted Telescope Operating Monitor 3D System in Microsurgical Varicocelectomy: A Preliminary Report. Surg. Innov. 2024, 31, 240–244. [Google Scholar] [CrossRef]
- Kaya, C.; Eryilmaz, S.; Kapisiz, A.; Atan, A.; Karabulut, R.; Türkyilmaz, Z.; Sönmez, K. Use of intraoperative microvascular Doppler during subinguinal microsurgical varicocelectomy in children reduces complications. Turk. J. Med. Sci. 2024, 54, 778–783. [Google Scholar] [CrossRef]
- Lv, K.L.; Zhang, Y.D.; Zhuang, J.T.; Gao, Y.; Zhao, L.; Wan, Z.; Zhou, M.K.; Yu, J.W.; Sun, X.Z.; Zhang, Y.Y.; et al. Subinguinal microsurgical varicocelectomy with intraoperative microvascular Doppler ultrasound leads to the pain-free outcome after surgery. J. Xray Sci. Technol. 2017, 25, 839–846. [Google Scholar] [CrossRef]
- Ramasamy, R.; Schlegel, P.N. Microsurgical inguinal varicocelectomy with and without testicular delivery. Urology 2006, 68, 1323–1326. [Google Scholar] [CrossRef]
- Wald, G.; Punjani, N.; Gaffney, C.; Goldstein, M.; Kashanian, J.A. Impact of testicular delivery and vasal vein ligation on clinical outcomes in men undergoing microsurgical varicocelectomy. Int. Urol. Nephrol. 2021, 53, 2453–2458. [Google Scholar] [CrossRef] [PubMed]
- Jin, L.; Yao, Q.; Wu, S.; Dai, G.; Xiang, H.; Liu, X.; Xue, B. Evaluation of clinical effects of microsurgical subinguinal varicocelectomy with and without testicular delivery. Andrologia 2020, 52, e13605. [Google Scholar] [CrossRef]
- Hou, Y.; Zhang, Y.; Zhang, Y.; Huo, W.; Li, H. Comparison between Microsurgical Subinguinal Varicocelectomy with and without Testicular Delivery for Infertile Men: Is Testicular Delivery an Unnecessary Procedure. Urol. J. 2015, 12, 2261–2266. [Google Scholar]
- Choi, C.I.; Park, K.C.; Lee, T.H.; Hong, Y.K. Recurrence rates in pediatric patients undergoing microsurgical subinguinal varicocelectomy with and without testicular delivery. J. Pediatr. Surg. 2017, 52, 1507–1510. [Google Scholar] [CrossRef]
- Song, Y.; Lu, Y.; Xu, Y.; Yang, Y.; Liu, X. Comparison between microsurgical varicocelectomy with and without testicular delivery for treatment of varicocele: A systematic review and meta-analysis. Andrologia 2019, 51, e13363. [Google Scholar] [CrossRef]
- Napolitano, L.; Pandolfo, S.D.; Aveta, A.; Cirigliano, L.; Martino, R.; Mattiello, G.; Celentano, G.; Barone, B.; Rosati, C.; La Rocca, R.; et al. The Management of Clinical Varicocele: Robotic Surgery Approach. Front. Reprod. Health 2022, 4, 791330. [Google Scholar] [CrossRef]
- Shu, T.; Taghechian, S.; Wang, R. Initial experience with robot-assisted varicocelectomy. Asian J. Androl. 2008, 10, 146–148. [Google Scholar] [CrossRef]
- McCullough, A.; Elebyjian, L.; Ellen, J.; Mechlin, C. A retrospective review of single-institution outcomes with robotic-assisted microsurgical varicocelectomy. Asian J. Androl. 2018, 20, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Parekattil, S.J.; Gudeloglu, A. Robotic assisted andrological surgery. Asian J. Androl. 2013, 15, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Pyrgidis, N.; Sokolakis, I.; Palapelas, V.; Tishukov, M.; Mykoniatis, I.; Symeonidis, E.N.; Zachariou, A.; Kaltsas, A.; Sofikitis, N.; Hatzichristodoulou, G.; et al. The Effect of Antioxidant Supplementation on Operated or Non-Operated Varicocele-Associated Infertility: A Systematic Review and Meta-Analysis. Antioxidants 2021, 10, 1067. [Google Scholar] [CrossRef] [PubMed]
- Ioannidou, P.G.; Papanikolaou, D.A.; Bosdou, J.K.; Goulis, D.G.; Lambropoulos, A.F.; Grimbizis, G.F.; Κolibianakis, E.M. Improvement in sperm quality by oral antioxidant supplementation in infertile men with varicocele who have not undergone surgical repair: Systematic review and meta-analysis. Andrologia 2022, 54, e14533. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, A.; Leisegang, K.; Majzoub, A.; Henkel, R.; Finelli, R.; Panner Selvam, M.K.; Tadros, N.; Parekh, N.; Ko, E.Y.; Cho, C.L.; et al. Utility of Antioxidants in the Treatment of Male Infertility: Clinical Guidelines Based on a Systematic Review and Analysis of Evidence. World J. Men’s Health 2021, 39, 233–290. [Google Scholar] [CrossRef]
- Wang, J.; Wang, T.; Ding, W.; Wu, J.; Wu, G.; Wang, Y.; Zhou, Z.; Xu, L.; Cui, Y. Efficacy of antioxidant therapy on sperm quality measurements after varicocelectomy: A systematic review and meta-analysis. Andrologia 2019, 51, e13396. [Google Scholar] [CrossRef]
- Chen, Y.W.; Niu, Y.H.; Wang, D.Q.; Li, H.; Pokhrel, G.; Xu, H.; Wang, T.; Wang, S.G.; Liu, J.H. Effect of adjuvant drug therapy after varicocelectomy on fertility outcome in males with varicocele-associated infertility: Systematic review and meta-analysis. Andrologia 2018, 50, e13070. [Google Scholar] [CrossRef] [PubMed]
| Classification | Basis of Grading | Grade I | Grade II | Grade III | Grade IV | Grade V |
|---|---|---|---|---|---|---|
| Hirsch (1980) [28] | Reflux pattern | No spontaneous reflux, elicitable with Valsalva maneuver. | Intermittent spontaneous reflux. | Continuous spontaneous reflux. | - | - |
| Sarteschi (1993) [27] | Vein diameter, reflux pattern | No dilated veins, only inguinal reflux during Valsalva maneuver. | Supra-testicular varicosities, reflux during Valsalva maneuver. | Peritesticular varicosities only in standing position, reflux during Valsalva maneuver. | Dilated veins in supine position, increasing in standing position and Valsalva, reflux at rest, increasing with during Valsalva maneuver, possible testicular hypotrophy. | Dilated veins in standing and supine position, reflux at rest, not increasing during Valsalva maneuver. |
| EAA (Lotti, 2022) [29] | Vein diameter, reflux pattern | Dilated veins (>3 mm) at rest at the funicular region with retrograde venous flow absent/intermittent at rest and enhanced during Valsalva maneuver. | Dilated veins (>3 mm) at rest at the upper pole of the testis with retrograde venous flow absent/intermittent at rest and enhanced during Valsalva maneuver. | Dilated veins (>3 mm) at rest at the lower pole of the testis with retrograde venous flow absent/intermittent at rest and enhanced during Valsalva maneuver. | Dilated veins (>3 mm) at rest (irrespective of location but usually extending to the peritesticular region) with retrograde venous flow continuous at rest and enhanced during Valsalva maneuver. Possible testicular hypotrophy. | Dilated veins (>3 mm) at rest (irrespective of location, but usually extending to the peritesticular region) with retrograde venous flow continuous at rest and not increasing during Valsalva maneuver. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Takács, T.; Szabó, A.; Kopa, Z. Recent Trends in the Management of Varicocele. J. Clin. Med. 2025, 14, 5445. https://doi.org/10.3390/jcm14155445
Takács T, Szabó A, Kopa Z. Recent Trends in the Management of Varicocele. Journal of Clinical Medicine. 2025; 14(15):5445. https://doi.org/10.3390/jcm14155445
Chicago/Turabian StyleTakács, Tamás, Anett Szabó, and Zsolt Kopa. 2025. "Recent Trends in the Management of Varicocele" Journal of Clinical Medicine 14, no. 15: 5445. https://doi.org/10.3390/jcm14155445
APA StyleTakács, T., Szabó, A., & Kopa, Z. (2025). Recent Trends in the Management of Varicocele. Journal of Clinical Medicine, 14(15), 5445. https://doi.org/10.3390/jcm14155445






