Rehabilitative Good Practices in the Treatment of Patients with Muscle Injuries
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Information Sources and Search Strategy
2.3. Selection Process, Data Extraction, and Data Synthesis
2.4. Bias Assessment
3. Results
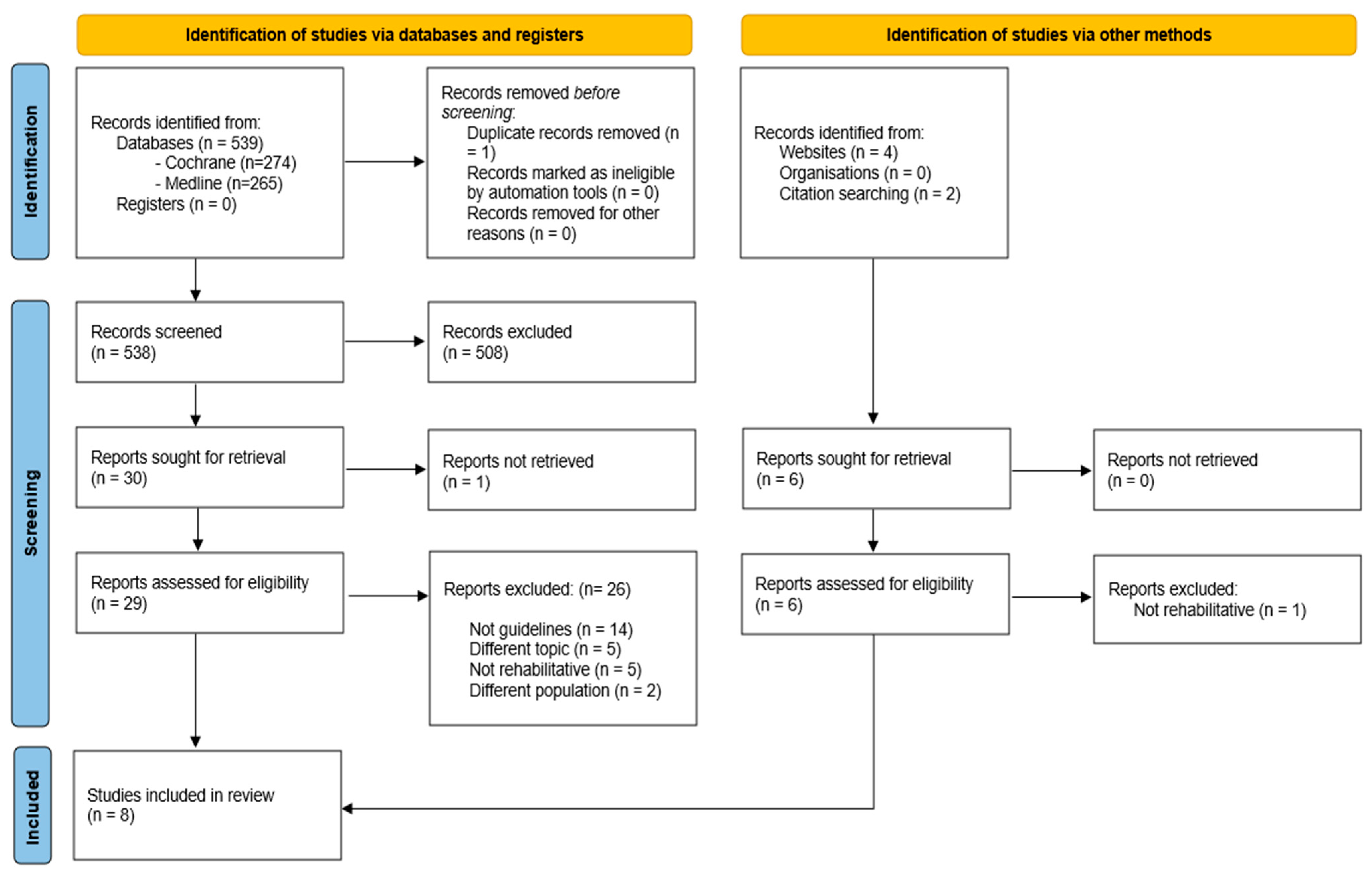
3.1. Study Selection
3.2. Study Characteristics
- -
- Paton B.M. et al. (2023) focused on the management of hamstring injuries. They gave directions for the selection of exercises, the progression of rehabilitation, and for the criteria to return to sport. In this document there is no mention of the level of the recommendations provided [1].
- -
- FC Barcelona and the Aspetar Foundation [26] (a foundation located in Doha, Qatar, specializing in orthopedic and traumatological pathologies and sports medicine) collaborated in 2015 to develop a guideline which primarily focused on the diagnosis and treatment of the most common muscle injuries in professional footballers (both conservative and non-conservative). The research methodology used is not mentioned or explained, nor are any specific recommendations provided.
- -
- Maffulli et al. [27] (2015) developed the guidelines of the Italian Society of Muscles Ligaments and Tendons (ISMuLT). These guidelines focused both on the diagnosis (both clinical and instrumental), classification, and treatment (surgical or conservative), and the treatment of muscle injuries. This document represents an update to the 2013 guidelines of the Italian Society of Muscles, Ligaments, and Tendons (ISMuLT) [29].
- -
- The National Collegiate Athletic Association (NCAA) [28], in 2014, developed a document consisting of a set of guidelines for the management of muscle injury in sports in the collegiate athlete. They focused not only on the injury itself, but also on the psychological/motivational aspects of the athlete and on the equipment, from the perspective of 360-degree management. In this document there is no mention of the level of the recommendations provided.
- -
- Valle et al. [30], in 2011, focused on all aspects of the management of the patient with the muscle injury, including the prevention of re-injury. They did not provide clear recommendations but attributed to every source they included a score based on the methodological value used in the writing of the article. In this way, a level of recommendation is indirectly attributed.
- -
- The Association of Chartered Physiotherapists in Sports and Exercise Medicine (ACPSM) [31], in 2010, produced a guideline on the use of the PRICE protocol (Protection, Rest, Ice, Compression, and Elevation) in case of muscle injury. The document provides clear recommendations, as well as their level using GRADE.
- -
- Heiderscheit et al. [2], in 2010, wrote a detailed description of the diagnostic and therapeutic pathway for muscle injuries involving only the hamstrings. No recommendations are provided, nor the level of the recommendations or the sources used.
3.3. Risk of Bias Assessment
3.4. Synthesis of the Results
- (1)
- (2)
- (3)
- (4)
- (5)
- (6)
- (1)
- (2)
- (3)
- (4)
- (5)
- (6)
- (7)
- (1)
- (2)
- (3)
- (4)
- (5)
- (6)
- (7)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Paton, B.M.; Read, P.; van Dyk, N.; Wilson, M.G.; Pollock, N.; Court, N.; Giakoumis, M.; Head, P.; Kayani, B.; Kelly, S.; et al. London International Consensus and Delphi study on hamstring injuries part 3: Rehabilitation, running and return to sport. Br. J. Sports Med. 2023, 57, 278–291. [Google Scholar] [CrossRef] [PubMed]
- Heiderscheit, B.C.; Sherry, M.A.; Silder, A.; Chumanov, E.S.; Thelen, D.G. Hamstring strain injuries: Recommendations for diagnosis, rehabilitation, and injury prevention. J. Orthop. Sports Phys. Ther. 2010, 40, 67–81. [Google Scholar] [CrossRef] [PubMed]
- Marotta, N.; de Sire, A.; Gimigliano, A.; Demeco, A.; Moggio, L.; Vescio, A.; Iona, T.; Ammendolia, A. Impact of COVID-19 lockdown on the epidemiology of soccer muscle injuries in Italian Serie A professional football players. J. Sports Med. Phys. Fit. 2022, 62, 356–360. [Google Scholar] [CrossRef]
- Chan, O.; Del Buono, A.; Best, T.M.; Maffulli, N. Acute muscle strain injuries: A proposed new classification system. Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 2356–2362. [Google Scholar] [CrossRef]
- Ishøi, L.; Krommes, K.; Husted, R.S.; Juhl, C.B.; Thorborg, K. Diagnosis, prevention and treatment of common lower extremity muscle injuries in sport—Grading the evidence: A statement paper commissioned by the Danish Society of Sports Physical Therapy (DSSF). Br. J. Sports Med. 2020, 54, 528–537. [Google Scholar] [CrossRef]
- Begum, F.A.; Kayani, B.; Chang, J.S.; Tansey, R.J.; Haddad, F.S. The management of proximal rectus femoris avulsion injuries. EFORT Open Rev. 2020, 5, 828–834. [Google Scholar] [CrossRef]
- de Sire, A.; Marotta, N.; Demeco, A.; Moggio, L.; Paola, P.; Marotta, M.; Iona, T.; Invernizzi, M.; Leigheb, M.; Ammendolia, A. Electromyographic Assessment of Anterior Cruciate Ligament Injury Risk in Male Tennis Players: Which Role for Visual Input? A Proof-of-Concept Study. Diagnostics 2021, 11, 997. [Google Scholar] [CrossRef]
- de Sire, A.; Demeco, A.; Marotta, N.; Moggio, L.; Palumbo, A.; Iona, T.; Ammendolia, A. Anterior Cruciate Ligament Injury Prevention Exercises: Could a Neuromuscular Warm-Up Improve Muscle Pre-Activation before a Soccer Game? A Proof-of-Principle Study on Professional Football Players. Appl. Sci. 2021, 11, 4958. [Google Scholar] [CrossRef]
- De Smet, A.A.; Best, T.M. MR imaging of the distribution and location of acute hamstring injuries in athletes. AJR Am. J. Roentgenol. 2000, 174, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.C.; Healy, J. Sonography of lower limb muscle injury. AJR Am. J. Roentgenol. 2004, 182, 341–351. [Google Scholar] [CrossRef]
- Koh, E.S.; McNally, E.G. Ultrasound of skeletal muscle injury. Semin. Musculoskelet. Radiol. 2007, 11, 162–173. [Google Scholar] [CrossRef]
- Goldman, E.F.; Jones, D.E. Interventions for preventing hamstring injuries. Cochrane Database Syst. Rev. 2010, 1, CD006782. [Google Scholar] [CrossRef] [PubMed]
- Mueller-Wohlfahrt, H.W.; Haensel, L.; Mithoefer, K.; Ekstrand, J.; English, B.; McNally, S.; Orchard, J.; van Dijk, C.N.; Kerkhoffs, G.M.; Schamasch, P.; et al. Terminology and classification of muscle injuries in sport: The Munich consensus statement. Br. J. Sports Med. 2013, 47, 342–350. [Google Scholar] [CrossRef] [PubMed]
- Pollock, N.; James, S.L.; Lee, J.C.; Chakraverty, R. British athletics muscle injury classification: A new grading system. Br. J. Sports Med. 2014, 48, 1347–1351. [Google Scholar] [CrossRef]
- Hickey, J.T.; Opar, D.A.; Weiss, L.J.; Heiderscheit, B.C. Hamstring Strain Injury Rehabilitation. J. Athl. Train. 2022, 57, 125–135. [Google Scholar] [CrossRef] [PubMed]
- Erickson, L.N.; Sherry, M.A. Rehabilitation and return to sport after hamstring strain injury. J. Sport Health Sci. 2017, 6, 262–270. [Google Scholar] [CrossRef]
- Raya-Gonzalez, J.; Castillo, D.; Clemente, F.M. Injury prevention of hamstring injuries through exercise interventions. J. Sports Med. Phys. Fit. 2021, 61, 1242–1251. [Google Scholar] [CrossRef]
- Futrell, M.; Rozzi, S.L. Principles of Rehabilitation. Prim. Care Clin. Off. Pract. 2020, 47, 87–103. [Google Scholar] [CrossRef]
- Tao, H.; Yu, F. The impact of psychological needs, social support, and sport motivation on college students’ sport commitment and sports participation. BMC Psychol. 2025, 13, 821. [Google Scholar] [CrossRef]
- Greising, S.M.; Corona, B.T.; Call, J.A. Musculoskeletal Regeneration, Rehabilitation, and Plasticity Following Traumatic Injury. Int. J. Sports Med. 2020, 41, 495–504. [Google Scholar] [CrossRef]
- de Sire, A.; Marotta, N.; Prestifilippo, E.; Parente, A.; Lopresti, E.; Drago Ferrante, V.; Sgro, M.; Lippi, L.; Invernizzi, M.; Ammendolia, A. Efficacy of platelet-rich plasma injection for pain relief in injured athletes: A systematic review of randomized controlled trials. J. Sports Med. Phys. Fit. 2025, 65, 665–672. [Google Scholar] [CrossRef]
- Al Attar, W.S.A.; Husain, M.A. Effectiveness of Injury Prevention Programs with Core Muscle Strengthening Exercises to Reduce the Incidence of Hamstring Injury Among Soccer Players: A Systematic Review and Meta-Analysis. Sports Health 2023, 15, 805–813. [Google Scholar] [CrossRef]
- Iolascon, G.; de Sire, A.; Curci, C.; Paoletta, M.; Liguori, S.; Calafiore, D.; Gimigliano, F.; Moretti, A. Osteoporosis guidelines from a rehabilitation perspective: Systematic analysis and quality appraisal using AGREE II. Eur. J. Phys. Rehabil. Med. 2021, 57, 273–279. [Google Scholar] [CrossRef]
- Institute of Medicine (US) Committee on Clinical Practice Guidelines. Guidelines for Clinical Practice: From Development to Use; Field, M.J., Lohr, K.N., Eds.; National Academies Press: Washington, DC, USA, 1992. [Google Scholar]
- Brouwers, M.C.; Kho, M.E.; Browman, G.P.; Burgers, J.S.; Cluzeau, F.; Feder, G.; Fervers, B.; Graham, I.D.; Grimshaw, J.; Hanna, S.E.; et al. AGREE Next Steps Consortium AGREE II: Advancing guideline development reporting evaluation in health care. Can. Med. Assoc. J. 2010, 182, E839–E842. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Valle, X.; Tol, H.; Hamilton, B.; Pruna, R. Muscle Injury Classification. In Muscle Injuries Clinical Guide 3.0; Barca Innovation Hub. 2015. Available online: https://static.capabiliaserver.com/frontend/clients/barca/wp/wp-content/uploads/2019/03/105e3b07-muscle-guide-general-principles-of-return-to-play-from-muscle-injury.pdf (accessed on 20 July 2025).
- Maffulli, N.; Del Buono, A.; Oliva, F.; Giai Via, A.; Frizziero, A.; Barazzuol, M.; Brancaccio, P.; Freschi, M.; Galletti, S.; Lisitano, G.; et al. Muscle Injuries: A Brief Guide to Classification and Management. Transl. Med. UniSa 2014, 12, 14–18. [Google Scholar] [PubMed]
- The National Collegiate Athletic Association. Sport Medicine Handbook, 24th ed.; The National Collegiate Athletic Association: Indianapolis, IN, USA, 2013. [Google Scholar]
- Maffulli, N.; Oliva, F.; Frizziero, A.; Nanni, G.; Barazzuol, M.; Via, A.G.; Ramponi, C.; Brancaccio, P.; Lisitano, G.; Rizzo, D.; et al. ISMuLT Guidelines for muscle injuries. Muscles Ligaments Tendons J. 2014, 3, 241–249. [Google Scholar] [CrossRef]
- Valle, X. Clinical practice guide for muscular injuries: Epidemiology, diagnosis, treatment and prevention. Br. J. Sports Med. 2011, 45, e2. [Google Scholar] [CrossRef]
- Bleakley, C.M.; Glasgow, P.D.; Philips, P.; Hanna, L.; Callaghan, M.J.; Davison, G.W. Acute Management of Soft Tissue Injuries, Guidelines. Available online: http://www.acpsm.org (accessed on 20 July 2025).
- Mason, D.L.; Dickens, V.A.; Vail, A. Rehabilitation for hamstring injuries. Cochrane Database Syst. Rev. 2012, 12, CD004575. [Google Scholar] [CrossRef] [PubMed]
- Palermi, S.; Vittadini, F.; Vecchiato, M.; Corsini, A.; Demeco, A.; Massa, B.; Pedret, C.; Dorigo, A.; Gallo, M.; Pasta, G.; et al. Managing Lower Limb Muscle Reinjuries in Athletes: From Risk Factors to Return-to-Play Strategies. J. Funct. Morphol. Kinesiol. 2023, 8, 155. [Google Scholar] [CrossRef]
- Witvrouw, E.; Mahieu, N.; Danneels, L.; McNair, P. Stretching and injury prevention: An obscure relationship. Sports Med. 2004, 34, 443–449. [Google Scholar] [CrossRef]
- Kim, G.; Kim, H.; Kim, W.K.; Kim, J. Effect of stretching-based rehabilitation on pain, flexibility and muscle strength in dancers with hamstring injury: A single-blind, prospective, randomized clinical trial. J. Sports Med. Phys. Fit. 2018, 58, 1287–1295. [Google Scholar] [CrossRef]
- Mahieu, N.N.; McNair, P.; De Muynck, M.; Stevens, V.; Blanckaert, I.; Smits, N.; Witvrouw, E. Effect of static and ballistic stretching on the muscle-tendon tissue properties. Med. Sci. Sports Exerc. 2007, 39, 494–501. [Google Scholar] [CrossRef]
- Davies, G.; Riemann, B.L.; Manske, R. Current concepts of plyometric exercise. Int. J. Sports Phys. Ther. 2015, 10, 760–786. [Google Scholar] [PubMed]
- Akuthota, V.; Ferreiro, A.; Moore, T.; Fredericson, M. Core stability exercise principles. Curr. Sports Med. Rep. 2008, 7, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Holcomb, W.R.; Rubley, M.D.; Lee, H.J.; Guadagnoli, M.A. Effect of hamstring-emphasized resistance training on hamstring: Quadriceps strength ratios. J. Strength Cond. Res. 2007, 21, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Fowler, C. Do nonsteroidal anti-inflammatory drugs impair tissue healing? J. Am. Acad. Physician Assist. 2018, 31, 1–5. [Google Scholar] [CrossRef]
- Leeder, J.; Gissane, C.; van Someren, K.; Gregson, W.; Howatson, G. Cold water immersion and recovery from strenuous exercise: A meta-analysis. Br. J. Sports Med. 2012, 46, 233–240. [Google Scholar] [CrossRef]
- Hotfiel, T.; Seil, R.; Bily, W.; Bloch, W.; Gokeler, A.; Krifter, R.M.; Mayer, F.; Ueblacker, P.; Weisskopf, L.; Engelhardt, M. Nonoperative treatment of muscle injuries—Recommendations from the GOTS expert meeting. J. Exp. Orthop. 2018, 5, 24. [Google Scholar] [CrossRef]
- Nakano, J.; Yamabayashi, C.; Scott, A.; Reid, W.D. The effect of heat applied with stretch to increase range of motion: A systematic review. Phys. Ther. Sport 2012, 13, 180–188. [Google Scholar] [CrossRef]
- Ainsworth, L.; Budelier, K.; Clinesmith, M.; Fiedler, A.; Landstrom, R.; Leeper, B.J.; Moeller, L.; Mutch, S.; O’Dell, K.; Ross, J.; et al. Transcutaneous electrical nerve stimulation (TENS) reduces chronic hyperalgesia induced by muscle inflammation. Pain 2006, 120, 182–187. [Google Scholar] [CrossRef]
- Dubois, B.; Esculier, J. Soft-tissue injuries simply need PEACE and LOVE. Br. J. Sports Med. 2020, 54, 72–73. [Google Scholar] [CrossRef]
- Bleakley, C.M.; Glasgow, P.; MacAuley, D.C. PRICE needs updating, should we call the POLICE? Br. J. Sports Med. 2012, 46, 220–221. [Google Scholar] [CrossRef] [PubMed]
- Alves, A.N.; Fernandes, K.P.; Deana, A.M.; Bussadori, S.K.; Mesquita-Ferrari, R.A. Effects of low-level laser therapy on skeletal muscle repair: A systematic review. Am. J. Phys. Med. Rehabil. 2014, 93, 1073–1085. [Google Scholar] [CrossRef] [PubMed]
- Wilkin, L.D.; Merrick, M.A.; Kirby, T.E.; Devor, S.T. Influence of therapeutic ultrasound on skeletal muscle regeneration following blunt contusion. Int. J. Sports Med. 2004, 25, 73–77. [Google Scholar] [CrossRef]
- Bizzini, M. Ice and modern sports physiotherapy: Still cool? Br. J. Sports Med. 2012, 46, 219. [Google Scholar] [CrossRef]
- Chellini, F.; Tani, A.; Zecchi-Orlandini, S.; Sassoli, C. Influence of Platelet-Rich and Platelet-Poor Plasma on Endogenous Mechanisms of Skeletal Muscle Repair/Regeneration. Int. J. Mol. Sci. 2019, 20, 683. [Google Scholar] [CrossRef]
- Trofa, D.P.; Obana, K.K.; Herndon, C.L.; Noticewala, M.S.; Parisien, R.L.; Popkin, C.A.; Ahmad, C.S. The Evidence for Common Nonsurgical Modalities in Sports Medicine, Part 1: Kinesio Tape, Sports Massage Therapy, and Acupuncture. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2020, 4, e1900104. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Cai, Z.; Li, X.; Zhu, A. Efficacy of cupping therapy on pain outcomes: An evidence-mapping study. Front. Neurol. 2023, 14, 1266712. [Google Scholar] [CrossRef]
- Cognetti, D.J.; Sheean, A.J.; Owens, J.G. Blood Flow Restriction Therapy and Its Use for Rehabilitation and Return to Sport: Physiology, Application, and Guidelines for Implementation. Arthrosc. Sports Med. Rehabil. 2022, 4, e71–e76. [Google Scholar] [CrossRef]
- Giombini, A.; Giovannini, V.; Di Cesare, A.; Pacetti, P.; Ichinoseki-Sekine, N.; Shiraishi, M.; Naito, H.; Maffulli, N. Hyperthermia induced by microwave diathermy in the management of muscle and tendon injuries. Br. Med. Bull. 2007, 83, 379–396. [Google Scholar] [CrossRef]
- Jordi, S.R.; Joaquim, S.F.; Iris, P.F. Profound diathermy uhf in sport traumatological pathology. Br. J. Sports Med. 2011, 45, e1. [Google Scholar] [CrossRef]
- Menon, V.P.; Sudheer, A.R. Antioxidant and anti-inflammatory properties of curcumin. Adv. Exp. Med. Biol. 2007, 595, 105–125. [Google Scholar] [CrossRef]
- Salter, D.; Yalamanchi, H.; Yalamanchi, A.; Yalamanchi, A. Ten days of supplementation with a standardized Boswellia serrata extract attenuates soreness and accelerates recovery after repeated bouts of downhill running in recreationally active men. Front. Sports Act. Living 2025, 7, 1488821. [Google Scholar] [CrossRef] [PubMed]
- Kimmatkar, N.; Thawani, V.; Hingorani, L.; Khiyani, R. Efficacy and tolerability of Boswellia serrata extract in treatment of osteoarthritis of knee—A randomized double blind placebo controlled trial. Phytomedicine 2003, 10, 3–7. [Google Scholar] [CrossRef]
- Nozaki, M.; Ota, S.; Terada, S.; Li, Y.; Uehara, K.; Gharaibeh, B.; Fu, F.H.; Huard, J. Timing of the administration of suramin treatment after muscle injury. Muscle Nerve 2012, 46, 70–79. [Google Scholar] [CrossRef] [PubMed]
- Taniguti, A.P.; Pertille, A.; Matsumura, C.Y.; Santo Neto, H.; Marques, M.J. Prevention of muscle fibrosis and myonecrosis in mdx mice by suramin, a TGF-β1 blocker. Muscle Nerve 2010, 43, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Brock, J.; Golding, D.; Smith, P.M.; Nokes, L.; Kwan, A.; Lee, P.Y.F. Update on the Role of Actovegin in Musculoskeletal Medicine: A Review of the Past 10 Years. Clin. J. Sport Med. 2020, 30, 83–90. [Google Scholar] [CrossRef]
- Gimigliano, F.; Moretti, A.; de Sire, A.; Calafiore, D.; Iolascon, G. The combination of vitamin D deficiency and overweight affects muscle mass and function in older post-menopausal women. Aging Clin. Exp. Res. 2018, 30, 625–631. [Google Scholar] [CrossRef]
- Iolascon, G.; Moretti, A.; de Sire, A.; Calafiore, D.; Gimigliano, F. Effectiveness of Calcifediol in Improving Muscle Function in Post-Menopausal Women: A Prospective Cohort Study. Adv. Ther. 2017, 34, 744–752. [Google Scholar] [CrossRef]
- Oh, D.Y.; Talukdar, S.; Bae, E.J.; Imamura, T.; Morinaga, H.; Fan, W.; Li, P.; Lu, W.J.; Watkins, S.M.; Olefsky, J.M. GPR120 is an omega-3 fatty acid receptor mediating potent anti-inflammatory and insulin-sensitizing effects. Cell 2010, 142, 687–698. [Google Scholar] [CrossRef]
- Nagy, S.R.; Mititelu, M.; Marin, R.C.; Popovici, V.; Pallag, A.; Jurca, T. The Impact of Protein and Amino Acid Supplementation on Muscular Strength and Endurance in Recreational Gym-Goers During 8-Week Resistance Training. Sports 2025, 13, 182. [Google Scholar] [CrossRef] [PubMed]
- Farup, J.; Rahbek, S.K.; Vendelbo, M.H.; Matzon, A.; Hindhede, J.; Bejder, A.; Ringgard, S.; Vissing, K. Whey protein hydrolysate augments tendon and muscle hypertrophy independent of resistance exercise contraction mode. Scand. J. Med. Sci. Sports 2014, 24, 788–798. [Google Scholar] [CrossRef] [PubMed]
- de Sire, A.; Andrenelli, E.; Negrini, F.; Lazzarini, S.G.; Patrini, M.; Ceravolo, M.G.; International Multiprofessional Steering Committee of Cochrane Rehabilitation REH-COVER action. Rehabilitation and COVID-19: The Cochrane Rehabilitation 2020 rapid living systematic review. Update as of 31 August 2020. Eur. J. Phys. Rehabil. Med. 2020, 56, 839–845. [Google Scholar] [CrossRef] [PubMed]
- Paolucci, T.; de Sire, A.; Ferrillo, M.; di Fabio, D.; Molluso, A.; Patruno, A.; Pesce, M.; Lai, C.; Ciacchella, C.; Saggino, A.; et al. Telerehabilitation proposal of mind-body technique for physical and psychological outcomes in patients with fibromyalgia. Front. Physiol. 2022, 13, 917956. [Google Scholar] [CrossRef]
- Zirek, E.; Analay Akbaba, Y.; Guven, M.F. Is synchronous telerehabilitation effective in the treatment of rotator cuff tears?—A randomized controlled trial. Physiother. Theory Pract. 2025, 2, 1–12. [Google Scholar] [CrossRef]
- Süzer, A.; Büker, N.; Güngör, H.R.; Ök, N.; Şavkin, R. Effects of telerehabilitation-implemented core stability exercises on patient-reported and performance-based outcomes in total knee arthroplasty patients: Randomised controlled trial. Physiother. Theory Pract. 2025, 41, 1213–1227. [Google Scholar] [CrossRef]
| Guideline | Authors/Society/Year | Multidisciplinarity | Hamstring |
|---|---|---|---|
| London International Consensus and Delphi study on hamstring injuries part 3: rehabilitation, running and return to sport [1] | Paton B.M. et al., 2023 | Yes | Yes |
| Muscle injuries clinical guide 3.0 [26] | FC Barcelona, Aspetar, 2015. | Yes | No |
| Muscle injuries: a brief guide to classification and management [27] | Maffulli N. et al., 2015. | Yes | No |
| Sport medicine handbook: Guidelines [28] | National Collegiate Athletic Association, 2014. | Yes | No |
| ISMuLT guidelines for muscle injuries [29] | Maffulli N. et al., 2013. | Yes | No |
| Clinical practice guide for muscular injuries: epidemiology, diagnosis, treatment and prevention [30] | Valle X., 2011. | Yes | No |
| Acute management of soft tissue injuries: Guidelines [31] | Bleakley C.M. et al., 2010. | No | No |
| Hamstring strain injuries: recommendations for diagnosis, rehabilitation, and injury prevention [2] | Heiderscheit B.C. et al., 2010. | Yes | Yes |
| CPG | Domain 1 | Domain 2 | Domain 3 | Domain 4 | Domain 5 | Domain 6 | Overall 1 | Overall 2 | |
|---|---|---|---|---|---|---|---|---|---|
| R1 | R2 | ||||||||
| Paton, 2023 [1] | 91.6% | 44.4% | 52.0% | 91.6% | 35.4% | 75.0% | 83.3% | 1 | 2 |
| Valle, 2015 [26] | 80.55% | 44.4% | 13.5% | 88.8% | 41.7% | 37.5% | 58.3% | 2 | 2 |
| Maffulli, 2015 [27] | 80.5% | 30.5% | 17.7% | 80.5% | 18.7% | 41.6% | 58.3% | 2 | 2 |
| NCAA, 2014 [28] | 83.3% | 72.2% | 26.0% | 91.7% | 27.1% | 16.7% | 66.7% | 2 | 2 |
| Maffulli, 2013 [29] | 80.5% | 52.7% | 21.9% | 88.9% | 20.8% | 20.8% | 66.7% | 2 | 2 |
| Valle, 2011 [30] | 88.8% | 55.5% | 14.6% | 91.6% | 33.3% | 33.3% | 58.3% | 2 | 2 |
| Bleakley, 2010 [31] | 97.2% | 58.3% | 73.9% | 80.5% | 35.4% | 83.3% | 91.7% | 1 | 2 |
| Heiderscheit, 2010 [2] | 80.5% | 47.2% | 22.9% | 94.4% | 37.5% | 37.5% | 58.3% | 2 | 2 |
| Isometric Exercise | Eccentric Exercise | Concentric Exercise | Isokinetic Exercise | Plyometric Exercise | Stretching | |
|---|---|---|---|---|---|---|
| Paton B.M., 2023 [1] | R | R | R | R | R | I |
| Valle, 2015 [26] | R | R | R | |||
| Maffulli, 2015 [27] | R | R | R | R | R | R |
| NCAA, 2014 [28] | R | R | ||||
| Maffulli, 2013 [29] | R | R | R | R | R | R |
| Valle X., 2011 [30] | R | R | R | |||
| Bleakley, 2010 [31] | ||||||
| Heiderscheit, 2010 [2] | R | R | R | R |
| PRICE | POLICE | NSAID’s | Laser Therapy | US Therapy | PRP Injections | Neuromuscular Taping | Analgesic Electrotherapy | Endogenous Thermotherapy | |
|---|---|---|---|---|---|---|---|---|---|
| Paton B.M., 2023 [1] | |||||||||
| Valle, 2015 [26] | R | ||||||||
| Maffulli, 2015 [27] | R | R | R | R | I | R | R | R | |
| NCAA, 2014 [28] | |||||||||
| Maffulli, 2013 [29] | R | R | NR | R | R | I | R | R | |
| Valle X., 2011 [30] | R | R | I | R | |||||
| Bleakley, 2010 [31] | R | ||||||||
| Heiderscheit, 2010 [2] | R | I | R | R |
| Manual Therapy | Core Stability | Coordination Balance | Neurodynamics | Multitask Exercise | Cardiovascular Maintenance | Hydrokinesis | |
|---|---|---|---|---|---|---|---|
| Paton B.M., 2023 [1] | R | R | R | ||||
| Valle, 2015 [26] | R | R | R | ||||
| Maffulli, 2015 [27] | R | R | R | R | R | I | |
| NCAA, 2014 [28] | R | ||||||
| Maffulli, 2013 [29] | R | R | R | R | R | ||
| Valle X., 2011 [30] | R | R | R | ||||
| Bleakley, 2010 [31] | |||||||
| Heiderscheit, 2010 [2] | R | R | R | R |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Agostini, F.; de Sire, A.; Finamore, N.; Savina, A.; Sveva, V.; Fisicaro, A.; Fricano, A.; Longo, U.G.; Ammendolia, A.; Bernetti, A.; et al. Rehabilitative Good Practices in the Treatment of Patients with Muscle Injuries. J. Clin. Med. 2025, 14, 5355. https://doi.org/10.3390/jcm14155355
Agostini F, de Sire A, Finamore N, Savina A, Sveva V, Fisicaro A, Fricano A, Longo UG, Ammendolia A, Bernetti A, et al. Rehabilitative Good Practices in the Treatment of Patients with Muscle Injuries. Journal of Clinical Medicine. 2025; 14(15):5355. https://doi.org/10.3390/jcm14155355
Chicago/Turabian StyleAgostini, Francesco, Alessandro de Sire, Nikolaos Finamore, Alessio Savina, Valerio Sveva, Andrea Fisicaro, Alessio Fricano, Umile Giuseppe Longo, Antonio Ammendolia, Andrea Bernetti, and et al. 2025. "Rehabilitative Good Practices in the Treatment of Patients with Muscle Injuries" Journal of Clinical Medicine 14, no. 15: 5355. https://doi.org/10.3390/jcm14155355
APA StyleAgostini, F., de Sire, A., Finamore, N., Savina, A., Sveva, V., Fisicaro, A., Fricano, A., Longo, U. G., Ammendolia, A., Bernetti, A., Mangone, M., & Paoloni, M. (2025). Rehabilitative Good Practices in the Treatment of Patients with Muscle Injuries. Journal of Clinical Medicine, 14(15), 5355. https://doi.org/10.3390/jcm14155355













