Cumulative Risk for Periprosthetic Fracture and Operative Treatment Options After Revision Total Hip Arthroplasty with a Modular and Tapered Revision Device—A Consecutive Series of 117 Cases in a Mid-Term Duration
Abstract
1. Introduction
2. Patients and Methods
2.1. Inclusion Criteria and Methods
2.2. Surgical Technique at Index Operation and Aftercare
3. Results
3.1. Basic Data and Survivorship Analysis
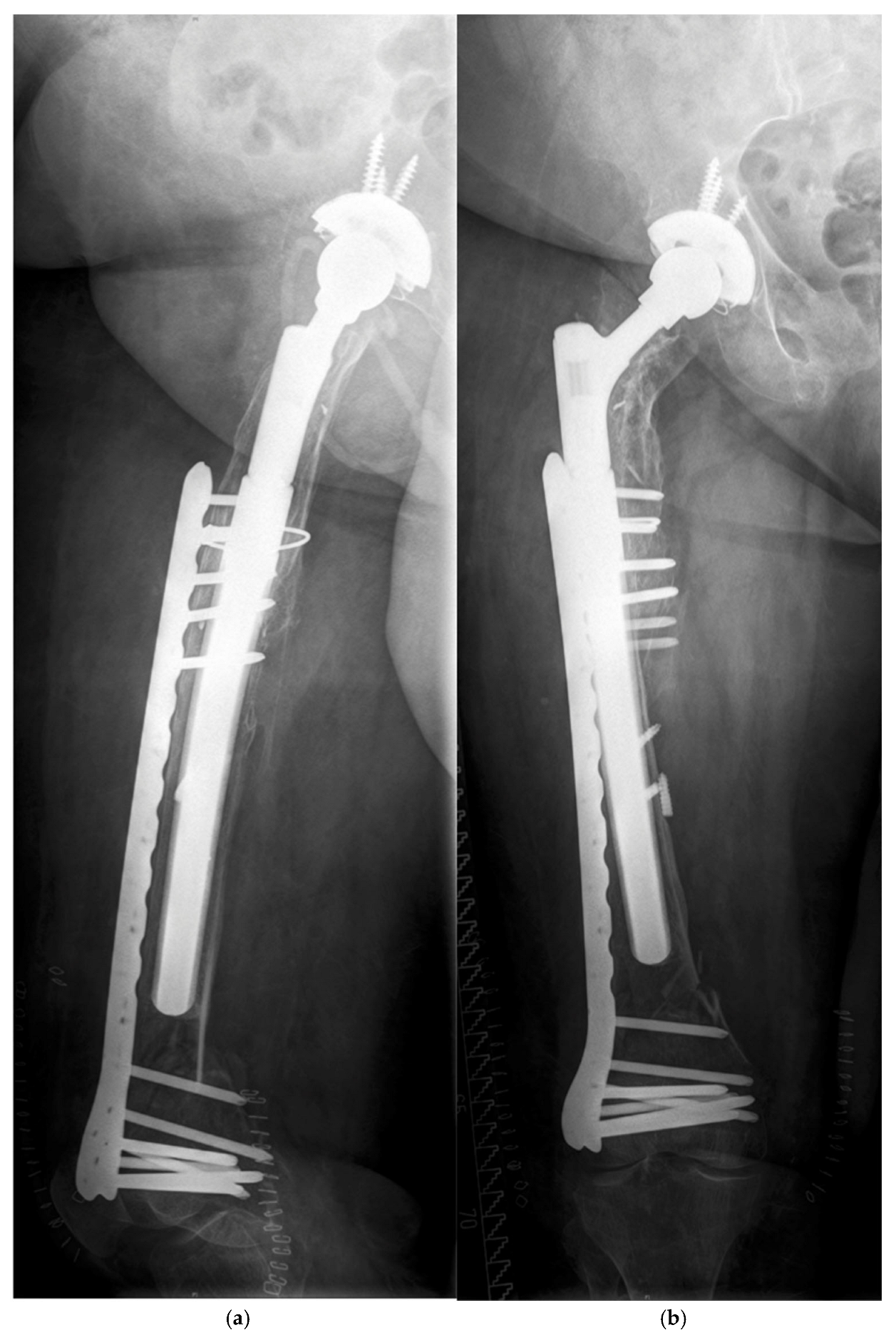
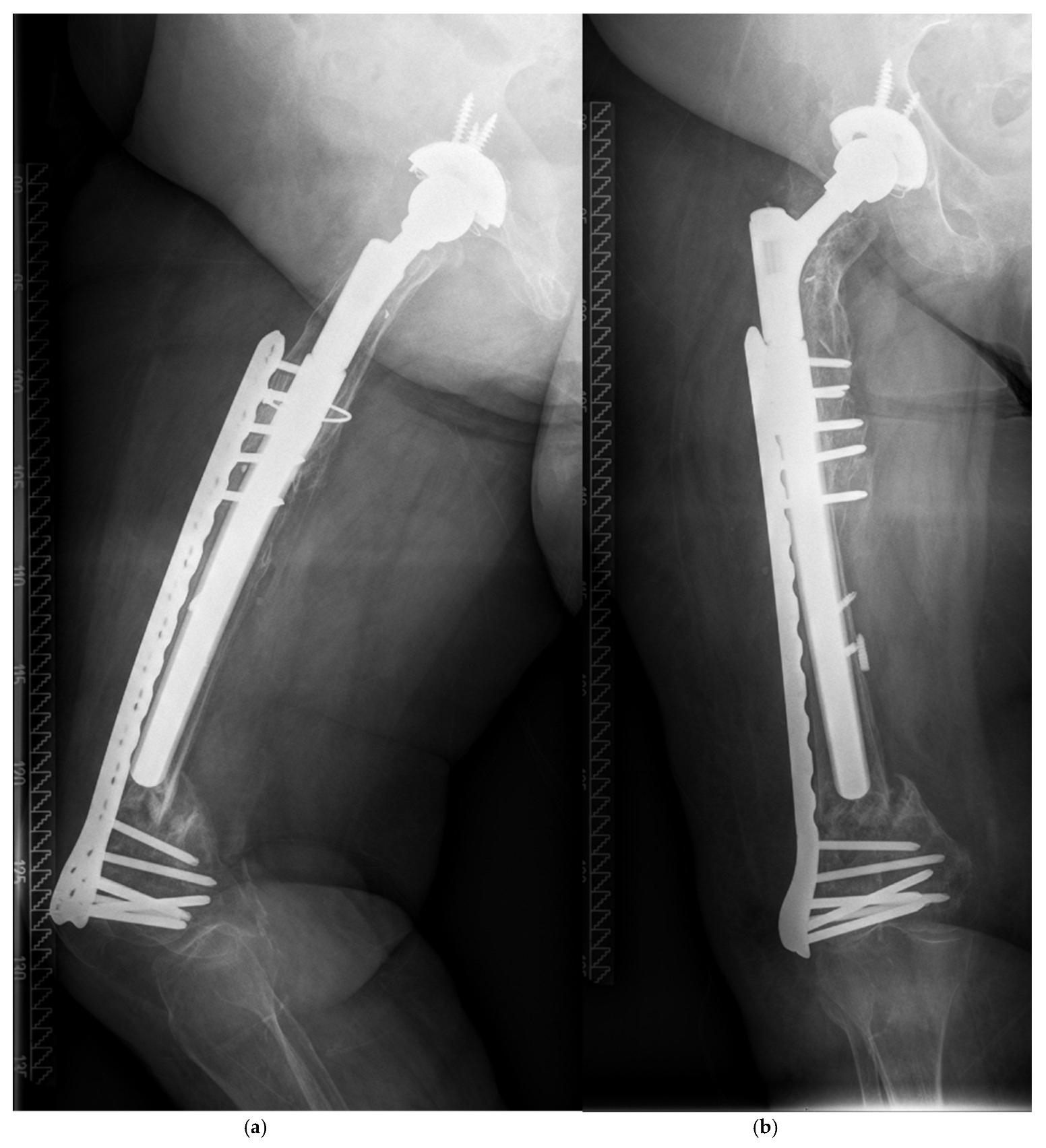
3.2. Periprosthetic Fractures
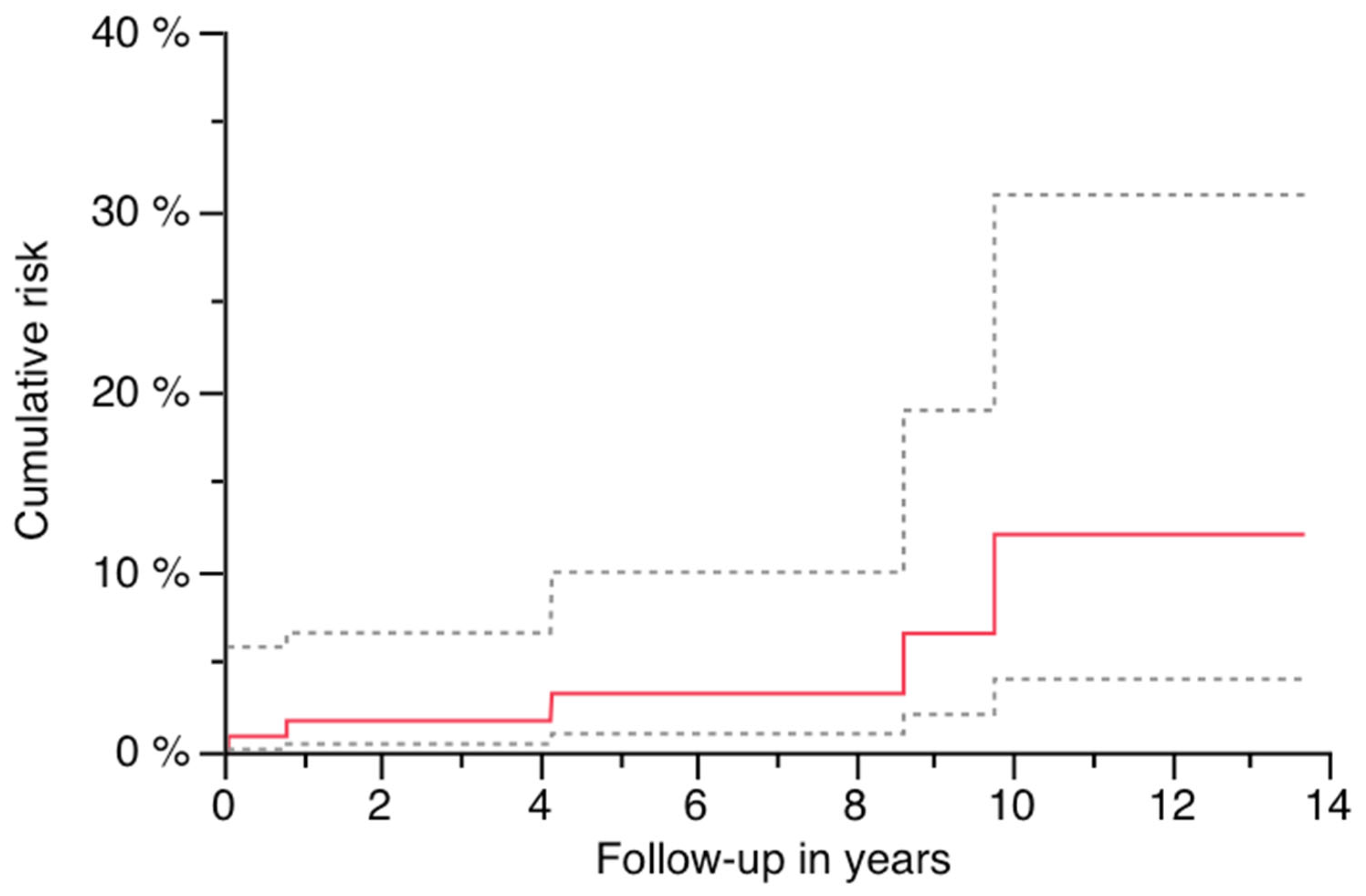
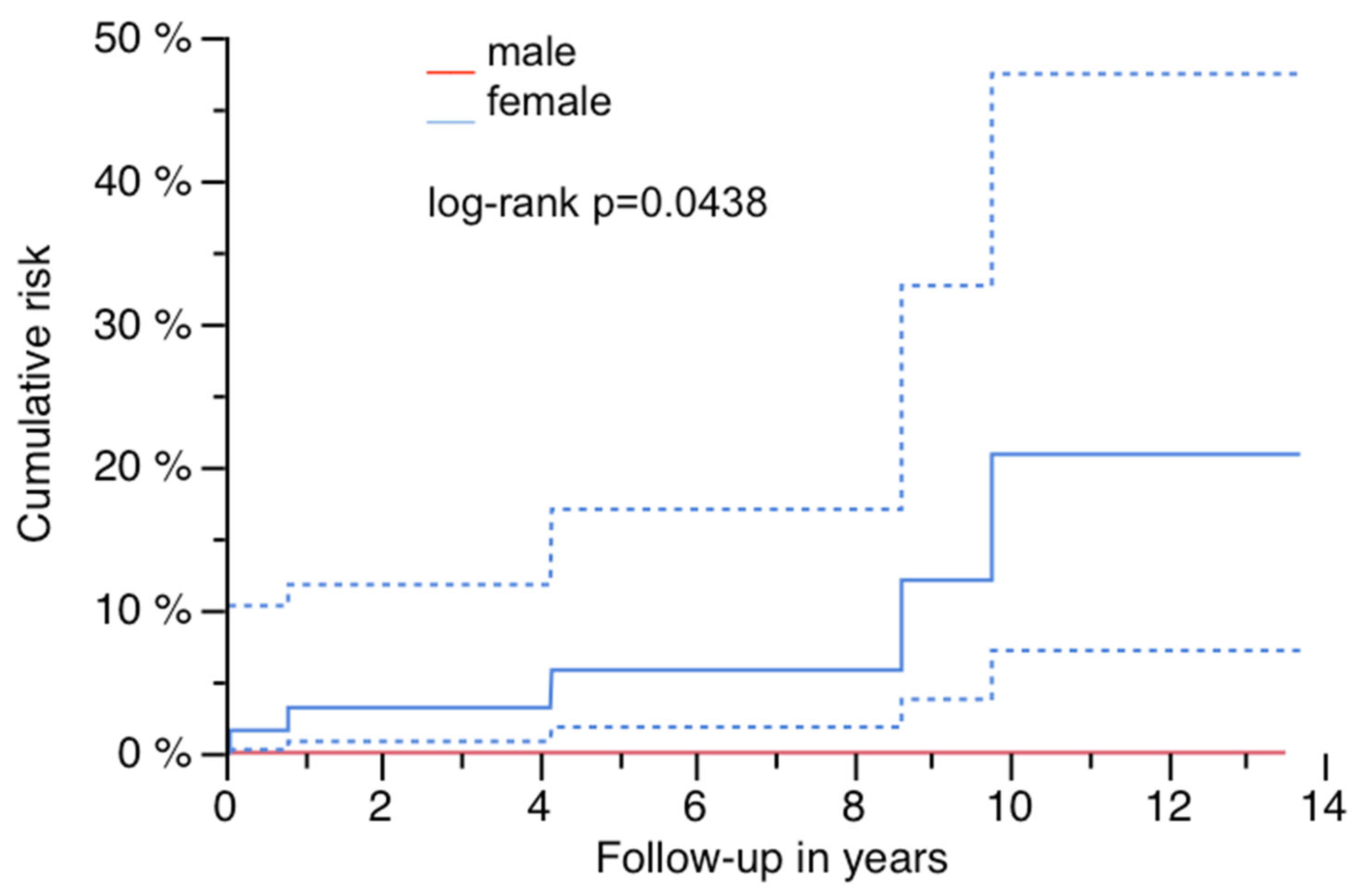
3.3. Survivorship Analysis and Predictive Risk Factors for PPF
4. Discussion
4.1. Cumulative Risk of PPF and Predicting Factors
4.2. Technical Considerations
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sanghavi, S.A.; Paprosky, W.G.; Sheth, N.P. Evaluation and Management of Acetabular Bone Loss in Revision Total Hip Arthroplasty: A 10-year Update. J. Am. Acad. Orthop. Surg. 2024, 32, e466–e475. [Google Scholar] [CrossRef] [PubMed]
- Klimko, A.; Andronic, O.; Zhe Lu, V.Y.; Dimitriou, D.; Hoch, A.; Zingg, P.O. Survivorship and Patient-Reported Outcomes in Femoral Impaction Bone Grafting for Revision Hip Arthroplasty: A Systematic Review and Meta-Analysis of 4,102 Hips. J. Arthroplast. 2025, in press. [CrossRef]
- Richards, C.J.; Duncan, C.P.; Masri, B.A.; Garbuz, D.S. Femoral revision hip arthroplasty: A comparison of two stem designs. Clin. Orthop. Relat. Res. 2010, 468, 491–496. [Google Scholar] [CrossRef] [PubMed]
- Böhm, P.; Bischel, O. The use of tapered stems for femoral revision surgery. Clin. Orthop. Relat. Res. 2004, 420, 148–159. [Google Scholar] [CrossRef]
- Hoberg, M.; Konrads, C.; Engelien, J.; Oschmann, D.; Holder, M.; Walcher, M.; Rudert, M. Outcome of a modular tapered uncemented titanium femoral stem in revision hip arthroplasty. Int. Orthop. 2015, 39, 1709–1713. [Google Scholar] [CrossRef] [PubMed]
- Spranz, D.; Skrobek, D.; Randoll, J.; Kinkel, S.; Merle, C.; Walker, T.; Renkawitz, T.; Reiner, T. Femoral revision in total hip arthroplasty using a cementless modular stem: Clinical and radiological results with a 8-year follow-up. Arch. Orthop. Trauma Surg. 2024, 144, 1369–1377. [Google Scholar] [CrossRef] [PubMed]
- Fink, B. What can the surgeon do to reduce the risk of junction breakage in modular revision stems? Arthroplast. Today 2018, 4, 306–309. [Google Scholar] [CrossRef] [PubMed]
- Boettcher, J.M.; Sellenschloh, K.; Strube, A.; Huber, G.; Morlock, M.M. Strength of the taper junction of modular revision hip stems: The influence of contamination of the taper junction and the joining condition on the relative motion and pull-off force between the stem and neck part of the MRP prosthesis. Orthopadie 2024, 53, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Bischel, O.E.; Suda, A.J.; Bohm, P.M.; Bormann, T.; Jager, S.; Seeger, J.B. Breakage of Tapered Junctions of Modular Stems in Revision Total Hip Arthroplasty-High Incidence in a Consecutive Series of a Single Institution. Bioengineering 2023, 10, 341. [Google Scholar] [CrossRef] [PubMed]
- Swedish Arthroplasty Register. Annual Report 2022. Available online: https://registercentrum.blob.core.windows.net/sar/r/SAR-Annual-Report-2022_EN-HkgQE89Nus.pdf (accessed on 14 April 2025).
- Masri, B.A.; Meek, R.M.; Duncan, C.P. Periprosthetic fractures evaluation and treatment. Clin. Orthop. Relat. Res. 2004, 420, 80–95. [Google Scholar] [CrossRef] [PubMed]
- Paprosky, W.G.; Bradford, M.S.; Younger, T.I. Classification of bone defects in failed prostheses. Chir. Organi Mov. 1994, 79, 285–291. [Google Scholar] [PubMed]
- Abdel, M.P.; Watts, C.D.; Houdek, M.T.; Lewallen, D.G.; Berry, D.J. Epidemiology of periprosthetic fracture of the femur in 32 644 primary total hip arthroplasties: A 40-year experience. Bone Jt. J. 2016, 98-B, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Innmann, M.M.; Streit, M.R.; Bruckner, T.; Merle, C.; Gotterbarm, T. Comparable Cumulative Incidence of Late Periprosthetic Femoral Fracture and Aseptic Stem Loosening in Uncemented Total Hip Arthroplasty-A Concise Follow-Up Report at a Minimum of 20 Years. J. Arthroplast. 2018, 33, 1144–1148. [Google Scholar] [CrossRef] [PubMed]
- Deng, Y.; Kieser, D.; Wyatt, M.; Stringer, M.; Frampton, C.; Hooper, G. Risk factors for periprosthetic femoral fractures around total hip arthroplasty: A systematic review and meta-analysis. ANZ J. Surg. 2020, 90, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Thomsen, M.N.; Jakubowitz, E.; Seeger, J.B.; Lee, C.; Kretzer, J.P.; Clarius, M. Fracture load for periprosthetic femoral fractures in cemented versus uncemented hip stems: An experimental in vitro study. Orthopedics 2008, 31, 653. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Lamb, J.; Townsend, O.; Scott, C.E.H.; Kendrick, B.; Middleton, R.; Jones, S.A.; Board, T.; West, R.; Pandit, H. Risk factors influencing fracture characteristics in postoperative periprosthetic femoral fractures around cemented stems in total hip arthroplasty: A multicentre observational cohort study on 584 fractures. Bone Jt. Open 2021, 2, 466–475. [Google Scholar] [CrossRef] [PubMed]
- Konow, T.; Baetz, J.; Melsheimer, O.; Grimberg, A.; Morlock, M. Factors influencing periprosthetic femoral fracture risk. Bone Jt. J. 2021, 103-B, 650–658. [Google Scholar] [CrossRef] [PubMed]
- Layson, J.T.; Hameed, D.; Dubin, J.A.; Moore, M.C.; Mont, M.; Scuderi, G.R. Patients with Osteoporosis Are at Higher Risk for Periprosthetic Femoral Fractures and Aseptic Loosening Following Total Hip Arthroplasty. Orthop. Clin. N. Am. 2024, 55, 311–321. [Google Scholar] [CrossRef] [PubMed]
- Kraus, M.; Gueorguiev, B.; Pastor, T.; Zderic, I.; Lenz, M.; Knobe, M.; Beeres, F.J.P.; Richards, R.G.; Pape, H.C.; Pastor, T. Evolving fracture management: The role of helical plating in orthopaedic trauma surgery—A narrative review. Eur. J. Trauma Emerg. Surg. 2025, 51, 203. [Google Scholar] [CrossRef] [PubMed]
- Yeo, I.; Rhyu, K.H.; Kim, S.M.; Park, Y.S.; Lim, S.J. High union rates of locking compression plating with cortical strut allograft for type B1 periprosthetic femoral fractures. Int. Orthop. 2016, 40, 2365–2371. [Google Scholar] [CrossRef] [PubMed]
- Dehoust, J.; Hinz, N.; Munch, M.; Behnk, F.; Kowald, B.; Schulz, A.P.; Frosch, K.H.; Hartel, M. Biomechanical comparison of different double plate constructs for distal supracondylar comminuted femur fractures (AO/OTA 33-A3). Injury 2025, 56, 112324. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Wei, Y.; Yin, W.; Shen, Y.; Cao, S. Biomechanical and clinical comparison of single lateral plate and double plating of comminuted supracondylar femoral fractures. Acta Orthop. Belg. 2018, 84, 141–148. [Google Scholar] [PubMed]
- Hoffmann, M.F.; Burgers, T.A.; Mason, J.J.; Williams, B.O.; Sietsema, D.L.; Jones, C.B. Biomechanical evaluation of fracture fixation constructs using a variable-angle locked periprosthetic femur plate system. Injury 2014, 45, 1035–1041. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Martin, D.; Hernandez-Castillejo, L.E.; Herrera-Perez, M.; Pais-Brito, J.L.; Gonzalez-Casamayor, S.; Garrido-Miguel, M. Osteosynthesis versus revision arthroplasty in Vancouver B2 periprosthetic hip fractures: A systematic review and meta-analysis. Eur. J. Trauma Emerg. Surg. 2023, 49, 87–106. [Google Scholar] [CrossRef] [PubMed]
- Di Martino, A.; Brunello, M.; Villari, E.; D’Agostino, C.; Cosentino, M.; Bordini, B.; Rivera, F.; Faldini, C. Stem revision vs. internal fixation in Vancouver B2/B3 periprosthetic hip fractures: Systematic review and metanalysis. Arch. Orthop. Trauma Surg. 2024, 144, 3787–3796. [Google Scholar] [CrossRef] [PubMed]
- Khan, T.; Grindlay, D.; Ollivere, B.J.; Scammell, B.E.; Manktelow, A.R.; Pearson, R.G. A systematic review of Vancouver B2 and B3 periprosthetic femoral fractures. Bone Jt. J. 2017, 99-B, 17–25. [Google Scholar] [CrossRef] [PubMed]


| MRP Brehm | |
|---|---|
| Original cohort: | 130 |
| Excluded patients due to the following: | |
| Infection | 7 |
| Subsidence within 6 weeks po./and instability | 4/2 |
| Aseptic loosening | 1 |
| Lost to follow-up | 1 |
| Included no. of patients | 117 |
| Implanted between (year) | 2003–2009 |
| Indication: | |
| Aseptic loosening | 51 (43.6%) |
| Septic two-stage revision | 50 (42.7%) |
| Periprosthetic fracture | 15 (12.8%) |
| Instability | 1 (0.9%) |
| Surgeons involved | 8 |
| Sex (w/m) | 64 (54.7%)/53 (45.3%) |
| Operated side (r/l) | 57 (48.7%)/60 (51.3%) |
| Mean age at surgery (range) in years | 67.87 (36.87–85.37) |
| Surgical approach: | |
| Transfemoral | 17 (14.5%) |
| Hardinge/transgluteal | 100 (85.5%) |
| Preoperative bone defect (Paprosky) | |
| Grade 1 | 18 (15.4) |
| Grade 2 | 73 (62.4%) |
| Grade 3A | 2 (1.7%) |
| Grade 3B | 18 (15.4%) |
| Grade 4 | 6 (5.1%) |
| Bone transplant at the femur: | |
| Total | 19 (16.2%) |
| Autogeneous | 3 (2.6%) |
| Allogeneous | 16 (13.7%) |
| Morsellized | 14 (12.0%) |
| Bulk/strut graft | 3 (2.6%) |
| Both morsellized and bulk graft | 2 (1.7%) |
| MRP Brehm | |
|---|---|
| Mean follow-up in years * | 5.7 (0.5–13.7) |
| Death during follow-up | n = 11 (9.4%) |
| Follow-up of deceased patients in years | 4.1 (0.5–13.7) |
| Mean reconstruction length (range)/median in mm | 249.5 (190–370)/250 |
| Mean stem diameter (range)/median in mm | 17.0 (13–30)/17 |
| BMI in kg/m2 | 27.8 (16.3–47.7) |
| Overweight | 74 (63.2%) |
| Normal weight | 41 (35.0%) |
| Underweight | 2 (1.7%) |
| PPF during follow-up | 5 (4.3%) |
| Follow-up until PPF (ys.) | 4.7 (0.1–9.8) |
| Overall risk (95% CI) of PPF after years in % | 12.1 (0–24.6) after 13.7 ys. |
| Risk of PPF and sex: female vs. male after years in % | 20.8 (0.5–41.2) after 13.7 ys. |
| vs. | |
| 0 after 13.5 ys. | |
| Log-rank p = 0.0438 | |
| Risk of PPF and stem length: shorter devices vs. ≥ median length after years in % | 0 after 11.2 ys. |
| vs. | |
| 16.7 (0–33.7) after 13.7 ys. | |
| Log-rank p = 0.1597 |
| Patient, Age at Surgery (ys.), Gender | Indication # | Bone Defect Paprosky et al. | Approach § | BMI (kg/m2) | Diabetes (y/n) | PPF Postop. (ys.) | Vancouver Classifi-cation | Conservative (C) vs. Operative Therapy (O) | Stem/Recon-Struction Length/Diameter (mm) * |
|---|---|---|---|---|---|---|---|---|---|
| 77, f. | TSR | 4 | TG | 20.8 | y | 4.2 | C | O (ORIF by Plate) | 290/14 |
| 68, f. | AL | 2B | TG | 22.5 | n | 0.8 | C | O (ORIF by Plate, Liss ©) | 250/18 |
| 73 +, f. | AL | 3B | TG | 34.4 | n | 8.6 | C | O (MIS by Plate, VA ©) | 290/21 |
| 75, f. | AL | 2B | TG | 25.9 | n | 9.8 | C | O (ORIF by Plate, VA ©) | 250/19 |
| 76, f. | AL | 2A | TG | 31.8 | n | 0.1 | B1 | O (ORIF by Plate, Liss ©) | 240/22 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bischel, O.E.; Jung, M.K.; Pilgrim, M.; Höppchen, A.J.; Böhm, P.M.; Seeger, J.B. Cumulative Risk for Periprosthetic Fracture and Operative Treatment Options After Revision Total Hip Arthroplasty with a Modular and Tapered Revision Device—A Consecutive Series of 117 Cases in a Mid-Term Duration. J. Clin. Med. 2025, 14, 5321. https://doi.org/10.3390/jcm14155321
Bischel OE, Jung MK, Pilgrim M, Höppchen AJ, Böhm PM, Seeger JB. Cumulative Risk for Periprosthetic Fracture and Operative Treatment Options After Revision Total Hip Arthroplasty with a Modular and Tapered Revision Device—A Consecutive Series of 117 Cases in a Mid-Term Duration. Journal of Clinical Medicine. 2025; 14(15):5321. https://doi.org/10.3390/jcm14155321
Chicago/Turabian StyleBischel, Oliver E., Matthias K. Jung, Max Pilgrim, Arnold J. Höppchen, Paul M. Böhm, and Jörn B. Seeger. 2025. "Cumulative Risk for Periprosthetic Fracture and Operative Treatment Options After Revision Total Hip Arthroplasty with a Modular and Tapered Revision Device—A Consecutive Series of 117 Cases in a Mid-Term Duration" Journal of Clinical Medicine 14, no. 15: 5321. https://doi.org/10.3390/jcm14155321
APA StyleBischel, O. E., Jung, M. K., Pilgrim, M., Höppchen, A. J., Böhm, P. M., & Seeger, J. B. (2025). Cumulative Risk for Periprosthetic Fracture and Operative Treatment Options After Revision Total Hip Arthroplasty with a Modular and Tapered Revision Device—A Consecutive Series of 117 Cases in a Mid-Term Duration. Journal of Clinical Medicine, 14(15), 5321. https://doi.org/10.3390/jcm14155321






