1. Introduction
Robotic-assisted total knee arthroplasty (RA-TKA) surgery has gained popularity for improving surgical precision and reducing the percentage of unsatisfied patients [
1,
2,
3]. However, the lack of randomized controlled trials comparing RA with conventional total knee arthroplasty (TKA), or comparative studies including large samples of patients, to date is not reasonable to report the certainty that robotic-assisted surgery is the gold standard in knee arthroplasty. Proper alignment is a major factor in implant longevity and joint function [
4]. Radiographs are crucial for preoperative planning and postoperative assessments in TKA, and achieving planned resection angles is essential for considering a robotic system reliable and safe [
5,
6,
7,
8]. The ROSA (RObotic Surgical Assistant) Knee System (Zimmer Biomet, Warsaw, IN, USA) is a collaborative robotic and computer device to assist orthopedic surgeons during TKA [
9,
10,
11]. This robotic-assisted device promises to enhance precision by piloting bone resections [
12]. Several studies have demonstrated the ability of the ROSA Knee System to achieve specific limb alignment and angles in the coronal plane, such as the medial proximal tibial angle (MPTA), lateral distal femoral angle (LDFA), and hip–knee–ankle angle (HKA) [
13,
14,
15,
16]. However, low accuracy and a high percentage of outliers were reported in the sagittal plane, especially concerning distal femur flexion (DFF) and tibial slope (TS) angles [
17].
This investigation evaluates the accuracy of the ROSA Knee System in achieving planned MPTA, LDFA, HKA, DFF, and TS by comparing the planned angle values with those obtained from postoperative radiographs three months postoperatively. The authors hypothesized that the percentage of outliers would be less than 10% for each considered measurement.
2.1. Surgical Procedures
All surgical procedures were performed by the main author (S.P.) at the Joint Replacement Department, IRCCS Galeazzi-Sant’Ambrogio Hospital, Milan, Italy. All patients received Persona (Zimmer Biomet, Warsaw, IN, USA) ultracongruent cruciate-retaining TKA. All procedures were performed in a highly standardized fashion using a medial midvastus surgical approach. Two femoral pins (3.2 mm diameter) and two tibial pins (3.2 mm diameter) were positioned in the proximal part of the surgical access and in the distal third of the medial tibia. Restricted kinematical alignment and an adjusted mechanical alignment technique were used in the varus and valgus knees, respectively.
2.2. Outcomes of Interest
According to limitations previously highlighted [
19], the planned intraoperative MPTA, LDFA, HKA, DFF, and TS angles of bone resections were extracted from the surgical report generated by the ROSA Knee System. Postoperative evaluation of radiographic outcomes was conducted three months postoperatively, and angle measurements were performed, as shown in
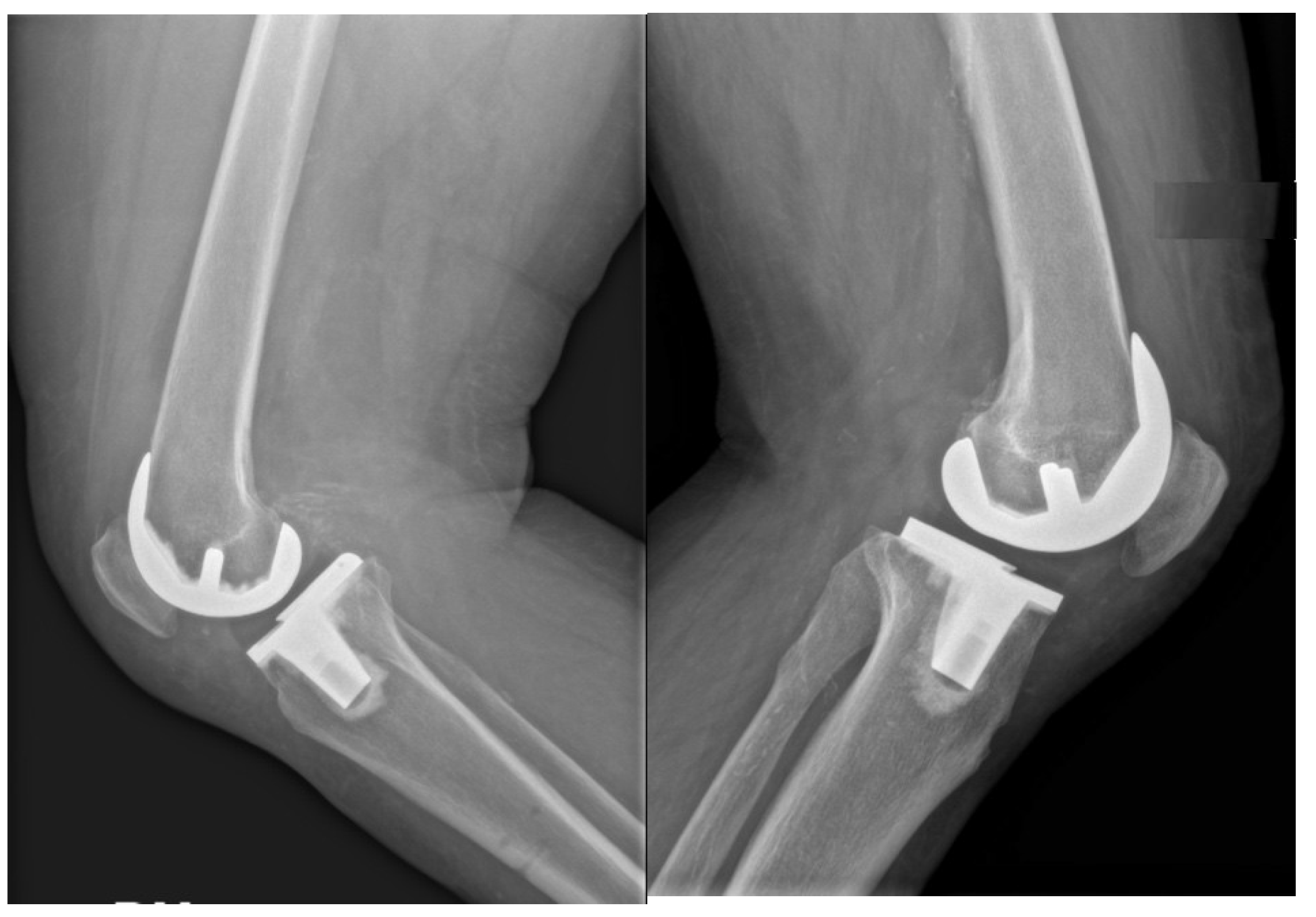
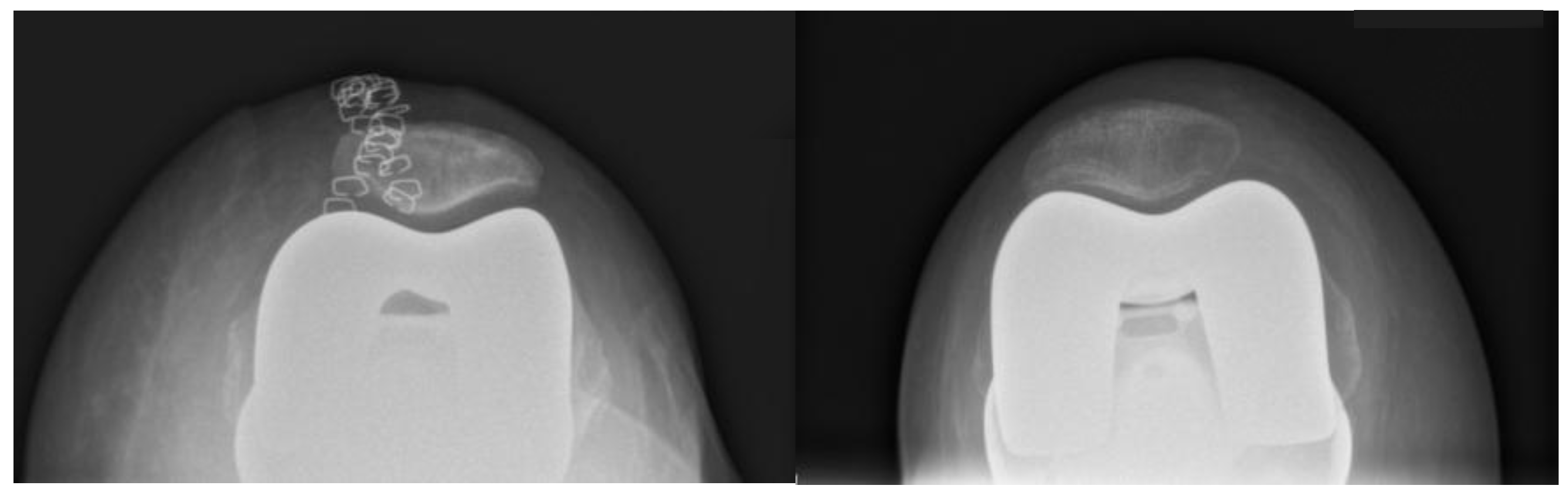
Table 1. Standardized full-length weight-bearing anteroposterior lower limb radiographs and lateral 90° flexion knee and axial radiographs of the patella were obtained (
Figure 1,
Figure 2 and
Figure 3). Incomplete radiographs because of a lack of weight bearing or incomplete extension warranted the exclusion from the present study. The arithmetic mean was calculated for each measurement performed by the two observers, and the obtained values were used for statistical purposes. Outliers from target angles were considered as follows: MPTA 90° ± 3°, LFDA 90° ± 3°, HKA 180° ± 3°, DFF 3° ± 3°, and TS 7° ± 3.
4. Discussion
According to the main finding of the present investigation, the ROSA Knee System was associated with a percentage of outliers lower than 10% during robotic-assisted TKA. Moreover, outliers greater than 3° were found in only 5.7% of patients for MPTA. The accuracy in the coronal plane is crucial to guarantee the longevity of a TKA [
20]. ROSA software can plan femoral and tibial coronal angles with good precision, with a difference between planned and achieved LDFA and MPTA of 0.53 ± 1.00 and 0.31 ± 1.29, respectively. This result agrees with those observed in previously published preclinical and biomechanics studies [
17,
21,
22]. Furthermore, a significant accuracy for the HKA with only 3.6% of outliers was found, confirming results reported by Rossi et al. and Schrednitzki et al. [
14,
15,
23]. Similar results were recently reported by Hax et al., who have demonstrated that most angles in the coronal plane were generally within the target range set for both groups and more frequently for femur than tibia components [
24].
Moreover, regarding the evaluation of HKA, the preoperative lower limb axis did not influence the accuracy of the robot in the varus and valgus limbs. Finally, after carefully registering the system and with sufficient experience with the robotic software, acceptable coronal alignment results could be achieved with Persona TKA.
The accuracy of the ROSA Knee System in the sagittal plane is still debated. A good sagittal alignment is crucial to restoring knee flexion and function, significantly influencing patient satisfaction. The ROSA Knee System can be considered inaccurate for the sagittal cuts, reaching percentages of accuracy of 51% within 2° and 77% within 3° for the DFF and 57% within 2° and 74% within 3° for the TS [
17]. However, this study identified DFF angles even though there were no differences between planned and achieved angles, while a significant difference was observed in the TS angle. Indeed, the TS angle was lower in radiographs than in the planned robotic software. However, these results usually do not negatively influence the stability of the implant during knee flexion. The saw is not long enough to reach the posterior aspect of the tibia when inserted in the tibial jig, possibility explaining these findings. Another explanation of the result could be that in the case of the large and long tibial plateau, especially in men, the sclerotic bone bends the saw during tibia resection, resulting in reduced TS. Another hypothesis, also supported by Hax et al., is that the reduced TS could result from an excessive anterior positioning of the tibial plateau center landmark during ROSA System registration [
24]. The precision and accuracy of a robotic system are significantly related to landmark calibration, which can be prone to individual errors. Furthermore, as also reported by Hax et al., the reasons why the index robotic system demonstrated more accuracy in the coronal plane postoperatively rather than in the sagittal plane remain unclear. In this study, the surgeon chose to position tibial pins in the distal third of the tibia and femoral pins in the proximal portion, a not universally adopted practice. This approach could influence the software’s final alignment predictions and measurements. Finally, according to our results, after excluding the first ten patients as part of the surgeon’s learning curve, the number did not influence the alignment accuracy of the robotic system.
The small sample size and the lack of a formal control group (manual TKA or other robotic systems) impair the reliability of the results of the present investigation [
13,
14,
25,
26,
27]. Moreover, a cost–benefit analysis comparing robotic-assisted TKA to conventional manual techniques could provide additional insights. The main author performed all surgeries independently in a highly standardized fashion, which might not reflect outcomes in other surgery settings. Although the surgeon had not used ROSA before, he completed four hours of theoretical and three hours of cadaveric lab training during a Zimmer Biomet Institute course before his first robotic-assisted TKA. In our previous study [
28], we demonstrated a rapid reduction in surgical time and a high level of accuracy in component size prediction using ROSA, with a learning phase of only ten cases. For this reason, we decided to exclude the first ten patients in the present investigation. Measurement accuracy depends on the quality of radiographic images. Although these were standardized according to institutional protocols, minor errors, particularly in component rotation, cannot be ruled out. Comparing results with one-year postoperative images or computed tomography (CT) scans could address this issue [
17]. Strengths of this study are the use of a single implant model, reducing variability in prosthesis positioning, the consistent standardization of perioperative care, including anesthesia and postoperative analgesia, and a stable surgical team, enhancing this study’s reliability.