Lumbar Tractions in Radicular Pain Caused by Herniated Disc: Randomised, Open-Label, Superiority, and Controlled Trial on 424 Participants
Abstract
1. Introduction
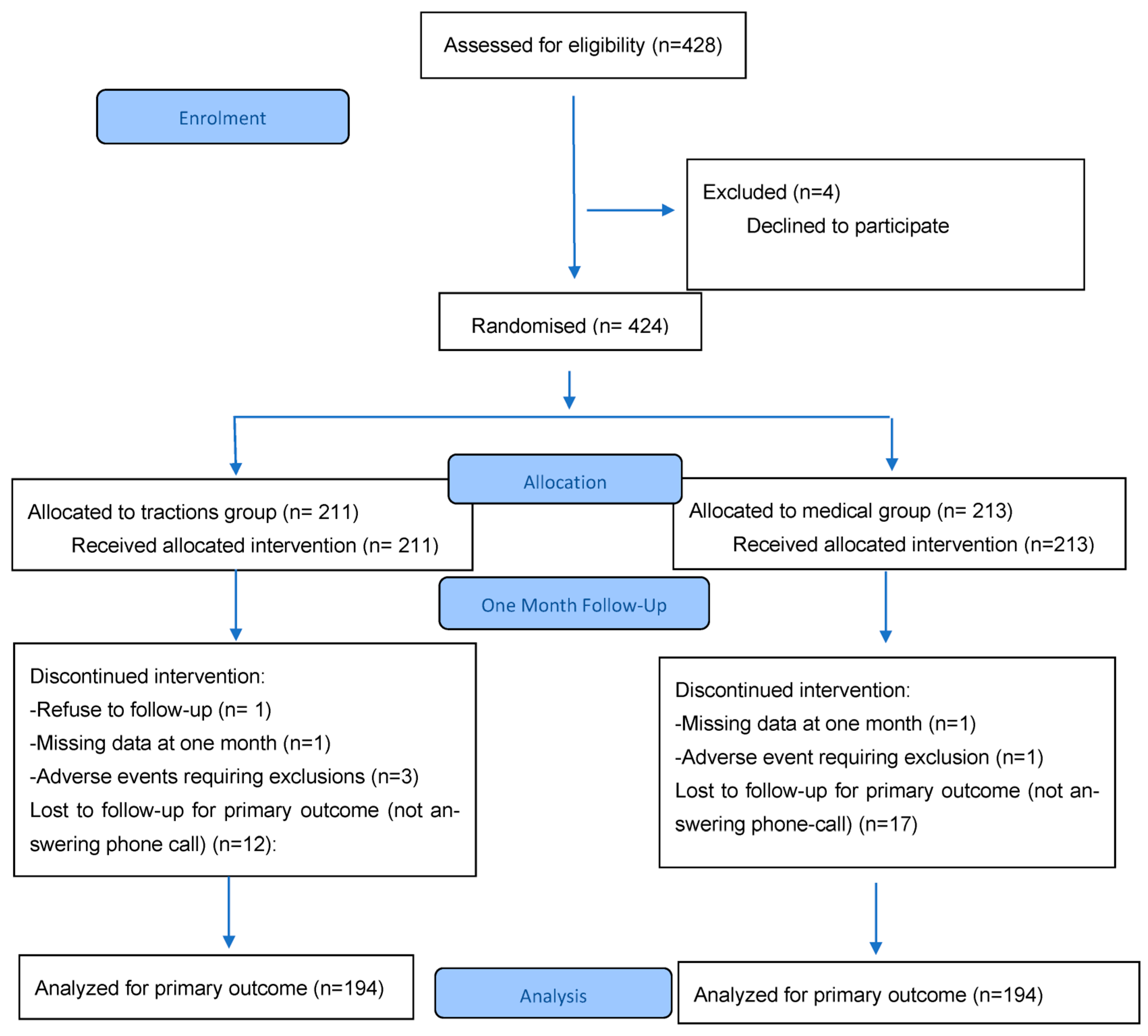
2. Materials and Methods
- (a)
- Design
- (b)
- Participants
- (c)
- Intervention
- (d)
- Outcome measures
- (e)
- Data analysis
3. Results
3.1. Study Population
3.2. Received Treatments
3.3. Primary Outcome
3.4. Secondary Outcomes
3.5. Tolerance
3.6. Subgroup Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BMI | Body Mass Index |
| CT | Computed Tomography |
| ITT | Intention To Treat |
| MG | Medical Group |
| MRC | Medical Research Council |
| MRI | Magnetic Resonance Imaging |
| NPS | Numeric Pain Scale |
| NSAIDs | Non-Steroidal Anti-Inflammatory Drugs |
| ODI | Oswestry Disability Index |
| OR | Odd Ratio |
| PP | per protocol |
| SD | Standard Deviation |
| SLR test | Straight Leg Rising test |
| TG | Tractions group |
References
- Radiculalgie et Syndrome Canalaire. Available online: http://www.lecofer.org/item-cours-1-4-0.php (accessed on 7 September 2022).
- Ropper, A.H.; Zafonte, R.D. Sciatica. N. Engl. J. Med. 2015, 372, 1240–1248. [Google Scholar] [CrossRef] [PubMed]
- SPF Troubles Musculo-Squelettiques Liés au Travail: Nombre de cas Evitables par L’application d’un Scénario Théorique de Prévention. Available online: https://www.santepubliquefrance.fr/import/troubles-musculo-squelettiques-lies-au-travail-nombre-de-cas-evitables-par-l-application-d-un-scenario-theorique-de-prevention (accessed on 18 September 2022).
- Corniola, M.-V.; Tessitore, E.; Schaller, K.; Gautschi, O.P. Hernie discale lombaire—Diagnostic et prise en charge. Rev. Med. Suisse 2014, 10, 2376–2382. [Google Scholar] [CrossRef] [PubMed]
- de Sèze, M.; Saliba, L.; Mazaux, J.-M. Percutaneous Treatment of Sciatica Caused by a Herniated Disc: An Exploratory Study on the Use of Gaseous Discography and Discogel® in 79 Patients. Ann. Phys. Rehabil. Med. 2013, 56, 143–154. [Google Scholar] [CrossRef] [PubMed]
- Jordon, J.; Konstantinou, K.; O’Dowd, J. Herniated Lumbar Disc. BMJ Clin. Evid. 2009, 2009, 1118. [Google Scholar][Green Version]
- Prise en Charge du Patient Présentant une Lombalgie Commune. Available online: https://www.has-sante.fr/jcms/c_2961499/fr/prise-en-charge-du-patient-presentant-une-lombalgie-commune (accessed on 11 September 2022).
- Ostelo, R.W. Physiotherapy Management of Sciatica. J. Physiother. 2020, 66, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Khorami, A.K.; Oliveira, C.B.; Maher, C.G.; Bindels, P.J.E.; Machado, G.C.; Pinto, R.Z.; Koes, B.W.; Chiarotto, A. Recommendations for Diagnosis and Treatment of Lumbosacral Radicular Pain: A Systematic Review of Clinical Practice Guidelines. J. Clin. Med. 2021, 10, 2482. [Google Scholar] [CrossRef]
- Verheijen, E.J.A.; Bonke, C.A.; Amorij, E.M.J.; Vleggeert-Lankamp, C.L.A. Epidural Steroid Compared to Placebo Injection in SciaticaA Systematic Review and Meta-Analysis. Eur. Spine J. 2021, 30, 3255–3264. [Google Scholar] [CrossRef] [PubMed]
- Meadeb, J.; Rozenberg, S.; Duquesnoy, B.; Kuntz, J.L.; Le Loët, X.; Sebert, J.L.; Le Goff, P.; Fallut, M.; Marty, M.; Blévin, S.; et al. Forceful Sacrococcygeal Injections in the Treatment of Postdiscectomy Sciatica. A Controlled Study versus Glucocorticoid Injections. Jt. Bone Spine 2001, 68, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Ozturk, B.; Gunduz, O.H.; Ozoran, K.; Bostanoglu, S. Effect of Continuous Lumbar Traction on the Size of Herniated Disc Material in Lumbar Disc Herniation. Rheumatol. Int. 2006, 26, 622–626. [Google Scholar] [CrossRef] [PubMed]
- Cyriax, J. The Treatment of Lumbar Disk Lesions. Br. Med. J. 1950, 2, 1434–1438. [Google Scholar] [CrossRef] [PubMed]
- Mckee, G.K. Traction-Manipulation and Plastic Corsets in the Treatment of Disc Lesions of the Lumbar Spine. Lancet 1956, 267, 472–475. [Google Scholar] [CrossRef] [PubMed]
- Schulz, K.F.; Altman, D.G.; Moher, D.; CONSORT Group. CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomised Trials. BMJ 2010, 340, c332. [Google Scholar] [CrossRef] [PubMed]
- Osama, M.; Afridi, S.; Rathore, F.A. Prone Lumbar Traction: An Underexplored Alternative for Lumbar Radiculopathy and Discogenic Low Back Pain. J. Pak. Med. Assoc. 2025, 75, 514–517. [Google Scholar] [CrossRef] [PubMed]
- Clarke, J.A.; van Tulder, M.W.; Blomberg, S.E.I.; de Vet, H.C.W.; van der Heijden, G.J.; Brønfort, G.; Bouter, L.M. Traction for Low-Back Pain with or without Sciatica. Cochrane Database Syst. Rev. 2007, CD003010. [Google Scholar] [CrossRef]
- Wegner, I.; Widyahening, I.S.; van Tulder, M.W.; Blomberg, S.E.; de Vet, H.C.; Brønfort, G.; Bouter, L.M.; van der Heijden, G.J. Traction for Low-back Pain with or without Sciatica. Cochrane Database Syst. Rev. 2013, 2013, CD003010. [Google Scholar] [CrossRef]
- Meszaros, T.F.; Olson, R.; Kulig, K.; Creighton, D.; Czarnecki, E. Effect of 10%, 30%, and 60% Body Weight Traction on the Straight Leg Raise Test of Symptomatic Patients With Low Back Pain. J. Orthop. Sports Phys. Ther. 2000, 30, 595–601. [Google Scholar] [CrossRef] [PubMed]
- Kumari, A.; Quddus, N.; Meena, P.R.; Alghadir, A.H.; Khan, M. Effects of One-Fifth, One-Third, and One-Half of the Bodyweight Lumbar Traction on the Straight Leg Raise Test and Pain in Prolapsed Intervertebral Disc Patients: A Randomized Controlled Trial. Biomed Res. Int. 2021, 2021, 2561502. [Google Scholar] [CrossRef] [PubMed]
- Kotb, H.A.; Effat, D.A.; Awad, M.R.; Derbala, S.H. CT-Guided Transforaminal Epidural Steroid Injection and Vertebral Axial Decompression in Management of Acute Lumbar Disc Herniation. Egypt. Rheumatol. 2018, 40, 67–72. [Google Scholar] [CrossRef]
- Sherry, E.; Kitchener, P.; Smart, R. A Prospective Randomized Controlled Study of VAX-D and TENS for the Treatment of Chronic Low Back Pain. Neurol. Res. 2001, 23, 780–784. [Google Scholar] [CrossRef] [PubMed]
- Thackeray, A.; Fritz, J.M.; Childs, J.D.; Brennan, G.P. The Effectiveness of Mechanical Traction Among Subgroups of Patients With Low Back Pain and Leg Pain: A Randomized Trial. J. Orthop. Sports. Phys. Ther. 2016, 46, 144–154. [Google Scholar] [CrossRef]
- Lewandrowski, K.-U.; Ransom, N.A.; Yeung, A. Return to Work and Recovery Time Analysis after Outpatient Endoscopic Lumbar Transforaminal Decompression Surgery. J. Spine Surg. 2020, 6, S100–S115. [Google Scholar] [CrossRef] [PubMed]
- Dépistage et Prévention Des Affections Rhumatologiques En Milieu de Travail|Elsevier Enhanced Reader. Available online: https://www.sciencedirect.com/science/article/pii/S1878622722000765 (accessed on 6 October 2022).
- Chow, D.H.K.; Yuen, E.M.K.; Xiao, L.; Leung, M.C.P. Mechanical Effects of Traction on Lumbar Intervertebral Discs: A Magnetic Resonance Imaging Study. Musculoskelet. Sci. Pract. 2017, 29, 78–83. [Google Scholar] [CrossRef] [PubMed]
- Unlu, Z.; Tascı, S.; Tarhan, S.; Pabuscu, Y.; Islak, S. Comparison of 3 Physical Therapy Modalities For Acute Pain in Lumbar Disc Herniation Measured by Clinical Evaluation and Magnetic Resonance Imaging. J. Manip. Physiol. Ther. 2008, 31, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Li, L.C.; Bombardier, C. Physical Therapy Management of Low Back Pain: An Exploratory Survey of Therapist Approaches. Phys. Ther. 2001, 81, 1018–1028. [Google Scholar] [CrossRef] [PubMed]
- Schimmel, J.J.P.; de Kleuver, M.; Horsting, P.P.; Spruit, M.; Jacobs, W.C.H.; van Limbeek, J. No Effect of Traction in Patients with Low Back Pain: A Single Centre, Single Blind, Randomized Controlled Trial of Intervertebral Differential Dynamics Therapy®. Eur. Spine J. 2009, 18, 1843–1850. [Google Scholar] [CrossRef] [PubMed]


| TG 1 (N = 211) | MG 2 (N = 213) | Total (N = 424) | ||
|---|---|---|---|---|
| Female sex (%) | 96 (45) | 89 (42) | 185 (44) | |
| Mean age (years and SD) | 43·7 (±12.63) | 42·9 (±11.59) | 42·7 (±12.24) | |
| Professional activity (%) | Working patients | 60 (28) | 69 (32) | 129 (30) |
| Sick leave | 104 (49) | 103 (48) | 207 (49) | |
| Students, retired, unemployed | 47 (22) | 41 (19) | 88 (21) | |
| Duration (%) | >3 months | 120 (57) | 115 (54) | 235 (55) |
| 1–3 months | 51 (24) | 55 (26) | 106 (25) | |
| <1 month | 40 (19) | 43 (20) | 83 (20) | |
| Previous injections (%) | 108 (51) | 94 (44) | 202 (48) | |
| Mean NPS radicular pain (SD) | 62·81 (±24.47) | 59·08 (±23.47) | 60·94 (±23.52) | |
| Mean NPS lumbar pain (SD) | 48·17 (±27.48) | 47·29 (±28.07) | 47·73 (±27.75) | |
| Previous anti-inflammatory use (%) | NSAIDs 3 | 128 (61) | 125 (59) | 253 (60) |
| Corticosteroids | 89 (42) | 87 (41) | 176 (42) | |
| Radicular pain (%) | L3/L4 | 15 (7) | 18 (8) | 33 (7) |
| L5 | 86 (41) | 84 (39) | 170 (40) | |
| S1 | 110 (52) | 111 (52) | 221 (52) | |
| Disc herniation position (%) | Paramedian | 122 (58) | 130 (61) | 252 (59) |
| Median | 60 (28) | 46 (22) | 106 (25) | |
| Foraminal | 29 (14) | 37 (17) | 66 (16) | |
| TG 1 (211) | MG 2 (213) | Total (424) | ||
|---|---|---|---|---|
| Traction | 5 tractions | 41 | - | 41 |
| 4 tractions | 84 | - | 86 | |
| 3 tractions | 77 | - | 80 | |
| 2 tractions | 7 | - | 7 | |
| 1 traction | 2 | - | 2 | |
| NSAIDs 3 | 121 | 126 | 247 | |
| Cortico-steroids | 37 | 39 | 76 | |
| Injections | 3 injections | 50 | 49 | 99 |
| 2 injections | 133 | 123 | 256 | |
| 1 injection | 3 | 6 | 9 | |
| Missing data | 25 | 35 | 60 | |
| Analgesics treatments (strongest) | 1 | 32 | 42 | 74 |
| 2 | 128 | 120 | 248 | |
| 3 | 42 | 44 | 86 | |
| Missing data | 9 | 7 | 16 | |
| TG | MG | p | OR [95% Confidence Interval] | |
|---|---|---|---|---|
| Diminution at least 25% for radicular NPS at 3 months (%) | 114/181 (63) | 96/179 (54) | 0.072 | 1.471 [0.966; 2.241] |
| Diminution at least 25% for lumbar NPS at one month (%) | 99/194 (51) | 98/194 (51) | 0.919 | 1.021 [0.686; 1.520] |
| Diminution at least 25% for lumbar NPS at 3 months (%) | 91/181 (50) | 77/179 (43) | 0.168 | 1.339 [0.884; 2.029] |
| Back-to-work delay at one month (%) | 30/88 (34) | 14/87 (16) | 0.008 | 2.682 [1.245; 6.013] |
| Back-to-work delay at 3 months (%) | 44/88 (50) | 23/87 (26) | 0.002 | 2.766 [1.411; 5.528] |
| SLR test (%) | 120/194 (62) | 108/199 (54) | 0.128 | 1.366 [0.914; 2.043] |
| Spinal surgery at one month (%) | 10/194 (5) | 7/194 (4) | 0.621 | 1.451 [0.486; 4.592] |
| Spinal surgery at 3 months (%) | 27/181(15) | 34/179 (19) | 0.327 | 0.748 [0.412; 1.349] |
| Analgesics diminution at one month (%) | 55/157 (35) | 55/144 (38) | 0.632 | 0.873 [0.531; 1.434] |
| Analgesics diminution at three months (%) | 69/157 (44) | 53/144 (37) | 0.240 | 1.345 [0.826; 2.197] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bernhard, E.; Hittinger-Roux, A.; Delaplace, H.; Pauvele, L.; Charlot, I.; Geoffroy, M.; Kanagaratnam, L.; Eap, C.; Mensa, C.; Bolko, L.; et al. Lumbar Tractions in Radicular Pain Caused by Herniated Disc: Randomised, Open-Label, Superiority, and Controlled Trial on 424 Participants. J. Clin. Med. 2025, 14, 5192. https://doi.org/10.3390/jcm14155192
Bernhard E, Hittinger-Roux A, Delaplace H, Pauvele L, Charlot I, Geoffroy M, Kanagaratnam L, Eap C, Mensa C, Bolko L, et al. Lumbar Tractions in Radicular Pain Caused by Herniated Disc: Randomised, Open-Label, Superiority, and Controlled Trial on 424 Participants. Journal of Clinical Medicine. 2025; 14(15):5192. https://doi.org/10.3390/jcm14155192
Chicago/Turabian StyleBernhard, Elsa, Ambre Hittinger-Roux, Helene Delaplace, Loïc Pauvele, Isabelle Charlot, Marion Geoffroy, Lukshe Kanagaratnam, Christophe Eap, Christophe Mensa, Loïs Bolko, and et al. 2025. "Lumbar Tractions in Radicular Pain Caused by Herniated Disc: Randomised, Open-Label, Superiority, and Controlled Trial on 424 Participants" Journal of Clinical Medicine 14, no. 15: 5192. https://doi.org/10.3390/jcm14155192
APA StyleBernhard, E., Hittinger-Roux, A., Delaplace, H., Pauvele, L., Charlot, I., Geoffroy, M., Kanagaratnam, L., Eap, C., Mensa, C., Bolko, L., & Salmon, J.-H. (2025). Lumbar Tractions in Radicular Pain Caused by Herniated Disc: Randomised, Open-Label, Superiority, and Controlled Trial on 424 Participants. Journal of Clinical Medicine, 14(15), 5192. https://doi.org/10.3390/jcm14155192






