1. Introduction
Patients with pre-existing glenohumeral arthritis are at an increased risk of nonunion in proximal humerus fractures as motion can lead to translation through the fracture site rather than the joint itself [
1]. It is well established that surgical neck nonunions are significantly debilitating for this population, and limit functional use of the shoulder [
2,
3,
4]. Various surgical treatments have been proposed, one of which is the utilization of reverse total shoulder arthroplasty (RTSA) which has shown promising clinical outcomes [
5,
6,
7]. Despite these positive results, there is data to suggest that there is a higher rate of post-operative shoulder dislocation associated with intraoperative resection of the greater and lesser tuberosities during this approach [
7]. The goal of this article is to describe a method for the preservation of the tuberosities and, thus, the rotator cuff attachment in order to maximize joint stability following RTSA for proximal humerus nonunion.
2. Surgical Technique
This technique describes the creation of greater and lesser tuberosity osteotomies for improved exposure, the implantation of both the glenoid and humeral implants, and a robust tuberosity reconstruction which includes cerclage fixation to increase stability and retain rotator cuff function. The senior author’s preferred method for positioning is beach-chair with a sterile arm holder. A standard deltopectoral approach is performed. Important aspects of this exposure include taking down the leading 1 cm of the pectoralis major tendon and clearing subdeltoid adhesions to allow maximal exposure. The axillary nerve is identified medially anterior to the subscapularis and medial to the conjoined tendon as well as its extension posteriorly and laterally in the subdeltoid plane. The rotator interval is entered, and a Darrah retractor is placed in the interval to assist with visualization of the tuberosities.
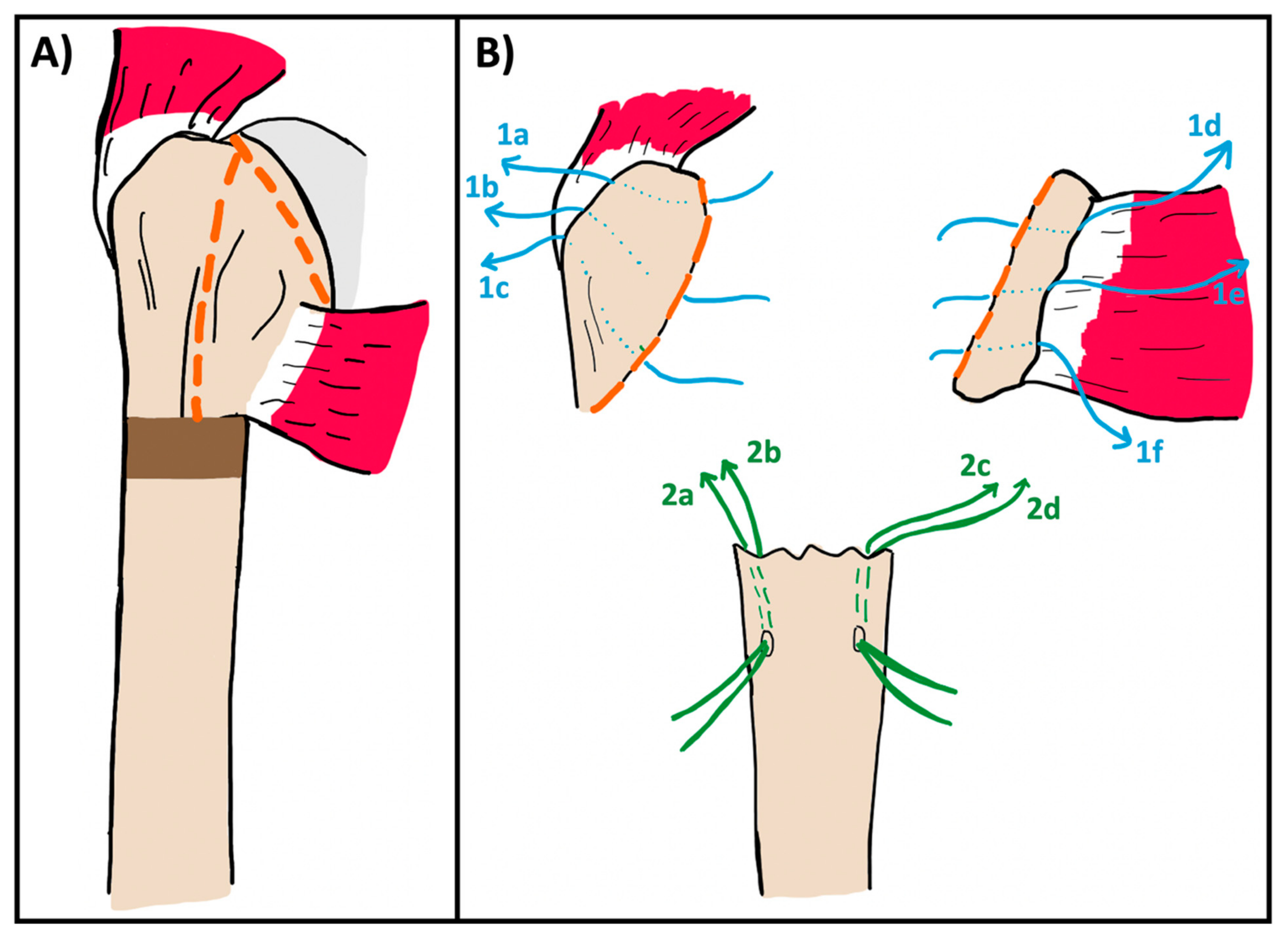
The greater/lesser tuberosity osteotomy begins at the bicipital groove anteriorly (
Figure 1A). The lesser tuberosity osteotomy is completed first using a large osteotome. After the osteotome penetrates the anterior cortex at the bicipital groove, it is angled medially and inferiorly to separate the lesser tuberosity from the humeral head. Completing the lesser tuberosity osteotomy allows for mobilization and debridement of the surgical neck nonunion, taking care to preserve any salvageable subscapularis tendon for repair. This tissue is then tagged along the bone–tendon juncture using three #5 Ethibond sutures (Ethicon Inc., Raritan, NJ, USA) (or any non-absorbable suture of the surgeon’s choice) which are clamped for later repair. This suture is passed, using an inside out technique, through the osteotomized lesser and then out through the subscapularis tendon (
Figure 1B). The subscapularis is further mobilized with the use of heavy scissors through the capsule and superior glenohumeral ligament on the upper border of the subscapularis and the anteroinferior edge of the glenoid. A finger is placed over the axillary nerve for protection during inferior dissection. In fracture work, the nerve may be more scarred down than in standard arthroplasty cases, so careful dissection is warranted.
Once the lesser tuberosity has been freed and tagged, and the subscapularis has been adequately mobilized, attention is turned to the greater tuberosity. A large osteotome is again used following a similar path through the bicipital groove and then angling laterally and superiorly to detach the greater tuberosity, preserving the supraspinatus and infraspinatus attachments. Care must be taken during this step to avoid skiving with the osteotome and cutting into the glenoid. Once the greater is freed, it is also tagged with three #5 Ethibonds using an inside-out technique at the bone–tendon junction for later repair (
Figure 1B). The remaining fracture fragments and humeral head are removed. In some cases, the humeral head may remain attached to the calcar medially and posteriorly, and an osteotomy at the anatomic neck can be used to release it (
Figure 1A). Two drill tunnels are then placed in the humeral shaft just distal to the nonunion site and two #5 Ethibond sutures are passed through each drill tunnel using an outside in technique. These sutures are then passed through the bone–tendon junction of the greater and lesser tuberosities and tagged for later repair (
Figure 1B).
Osteotomies of the tuberosities and removal of the humeral head provides ample glenoid exposure for routine glenosphere insertion using the surgeons’ preferred choice of implant (
Figure 2). Once this is placed, attention is turned towards humeral component and polyethylene trialing. A trauma-specific humeral stem—the Lima SMR Trauma in this case—is used as this allows for multiple sites of suture fixation through the stem. Trials of increasing polyethylene size are placed until the shoulder is no longer easily reducible, then one size is subtracted for the final component. This method ensures stability while preventing overstuffing. The trial construct should be stable to manual stress and shuck testing prior to proceeding final implant placement.
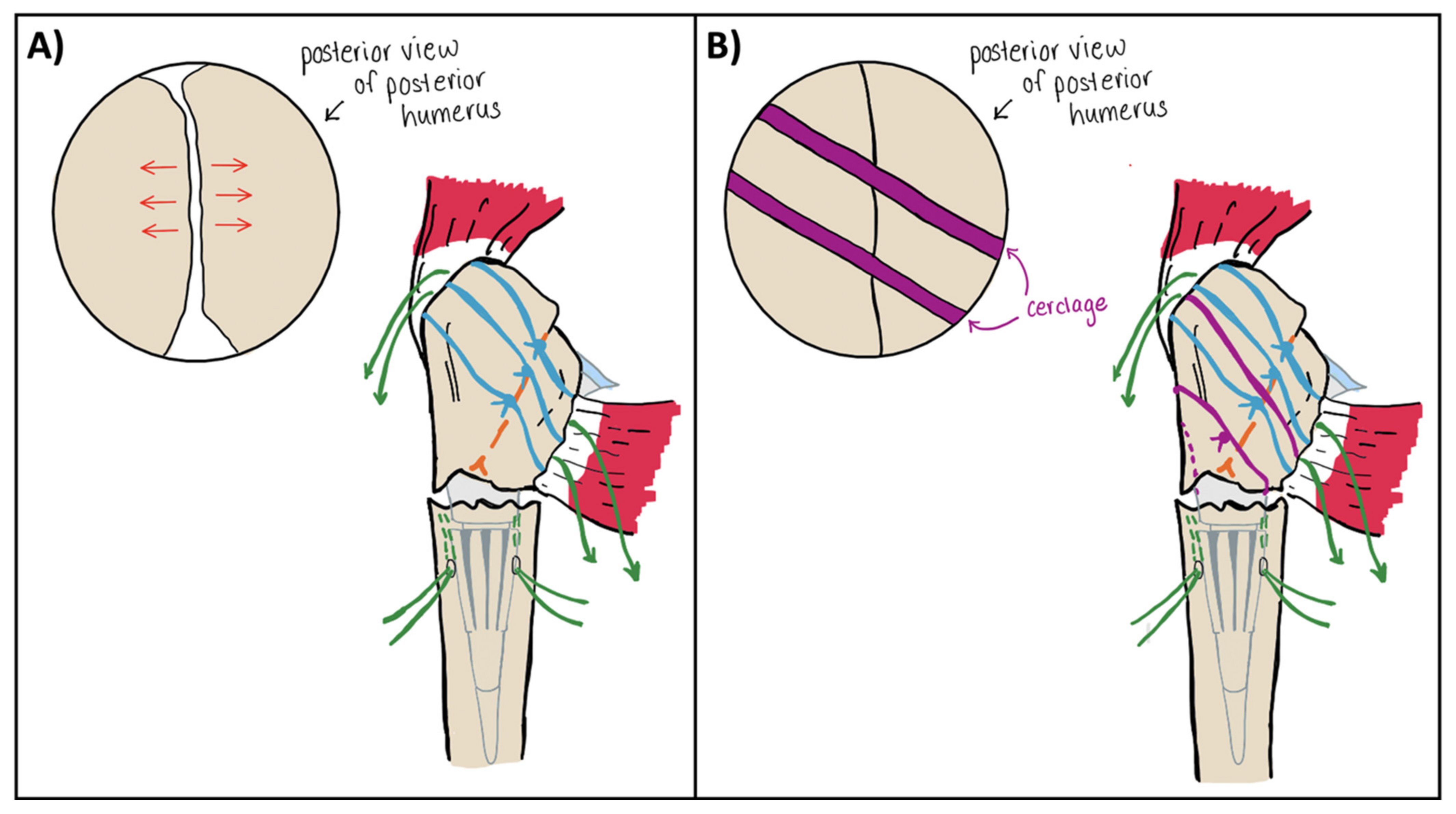
As the final humeral implant is introduced into the canal, a single Ethibond suture is passed posteriorly around the humeral stem as a passing suture for subsequent cerclage (
Figure 3A). This is performed prior to final spacer and polyethylene placement to ensure proper placement within the implant groove. Once the implant is seated, the lesser and greater tuberosity osteotomies are meticulously reapproximated using the cerclage and the previously passed tuberosity and humeral shaft sutures (
Figure 3B).
The cerclage suture—in this case Arthrex FiberTape (Arthrex, Naples, FL, USA)—is passed using the previously placed Ethibond suture. Care is taken to ensure the cerclage sits in the implant groove at the medial neck. If desired, a second passing suture can be pulled around the tuberosities with the cerclage to allow a second cerclage pass. The previously placed Ethibond sutures at the bone–tendon interface of the greater and lesser tuberosities are then passed through anchor holes in the humeral implant stem. Of note, there is typically only room for 4 of these 6 sutures to pass through the stem. At this point the cerclage is tensioned to fixate the greater and lesser tuberosities to each other. It is critical to pass sutures 1a–f through the implant and bring the tails out anteriorly before the cerclage is tightened, as tightening of the cerclage will lead to loss of access to the stem. After cerclage tensioning, the six tuberosity sutures (1a–f) are tied to their tails anteriorly, tightly securing the tuberosities to the implant. As these sutures are brought together, the previously tightened cerclage serves to prevent posterior gaping of the tuberosities (
Figure 4). At this point, the tuberosities are fixed to each other and to the implant. Finally, the sutures passed through the humeral shaft are tied, fixing the construct to the humeral shaft. With this technique, the tuberosities are secured to one another, the implant, and the humeral shaft to achieve maximal stability (
Figure 5). Additional Ethibond sutures are placed in a figure-of-eight fashion as needed for further reinforcement of the subscapularis tendon. At this point, the final construct should move as a singular unit with forward flexion and internal/external rotation. The wound is then thoroughly irrigated and closed in a layered fashion.
3. Results
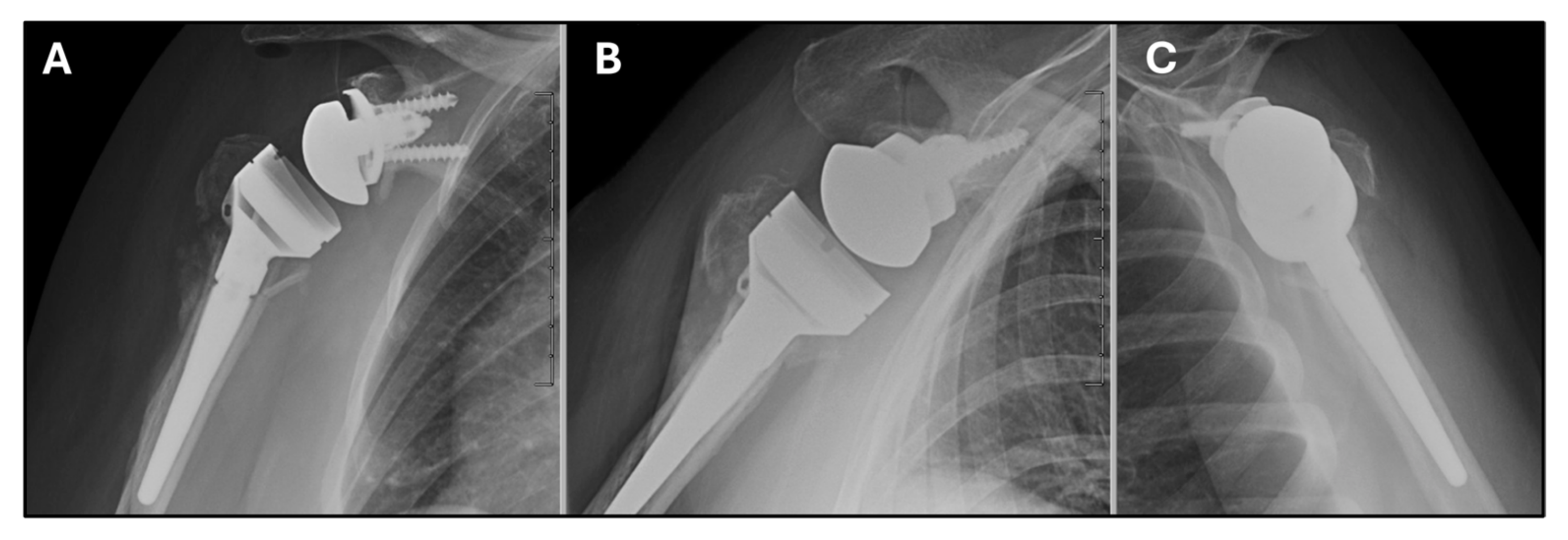
We present the case of a 74-year-old, right-hand dominant, Caucasian female who sustained a displaced surgical neck fracture of the right proximal humerus (
Figure 6A,B). Prior to this injury, she functioned independently and was able to perform all daily activities of living but she did use a rolling walker for gait assistance. Her medical co-morbidities included obesity (BMI 35), hypertension, hyperlipidemia, hypothyroidism, osteopenia, stage 2 chronic kidney disease, and obstructive lung disease, and multiple spine surgeries for lumbar pathology. She initially was treated at an outside facility and underwent a trial of non-operative management in a cuff and collar for 6 weeks followed by physical therapy; however, after 11 weeks of ongoing conservative measures there was continued lack of radiographic healing and progressive varus displacement (
Figure 6C,D). A CT scan was subsequently obtained, and this showed no significant bridging callus at the fracture site and underlying glenohumeral arthritis (
Figure 6E–G) and she was referred to our office for discussion of surgical management. At this point, the patient was three months out from her initial injury with significant ongoing pain and functional limitations. She was having issues supporting herself with her walker and performing overhead activities such as doing her hair. She was only able to achieve 70 degrees of active forward elevation, 10 degrees of external rotation, and internal rotation to the lumbosacral junction. She was indicated for a right RTSA and underwent the procedure described above. An STD glenoid baseplate and a 40 mm glenosphere were utilized and offset inferiorly. A Lima finned, uncemented diaphyseal-fit stem sized to 15 mm was placed in addition to one +9 spacer and a +6 polyethylene to idealize periarticular soft-tissue tension.
Overall, she had an uncomplicated post-operative course and reported gradual resolution of pain. She was seen back in the office at 2 weeks for suture removal. At the 6-week follow-up, her radiographs showed evidence of maintained tuberosity reduction and alignment (
Figure 7), and physical therapy was started at this time. At 3 months she had improvement in her pain but continued to have some weakness with forward elevation. By her final in-office visit at 5 months postop, she was able to achieve 110 degrees of active forward elevation, unfortunately we do not have internation and external rotation values recorded in the chart for this final visit. At this visit she reported return to her pre-injury activities including independence with ADLs, ambulation with a rolling walker for assistance, and the ability to perform overhead hygiene such as curling her hair.