Subaxial Subluxation (SAS) and Cervical Deformity in Patients with Rheumatoid Arthritis in Relation to Selected Sagittal Balance Parameters
Abstract
1. Introduction
2. Materials and Methods
| Radiological Parameters Within the Skull | |
|---|---|
| Parameter | Definition |
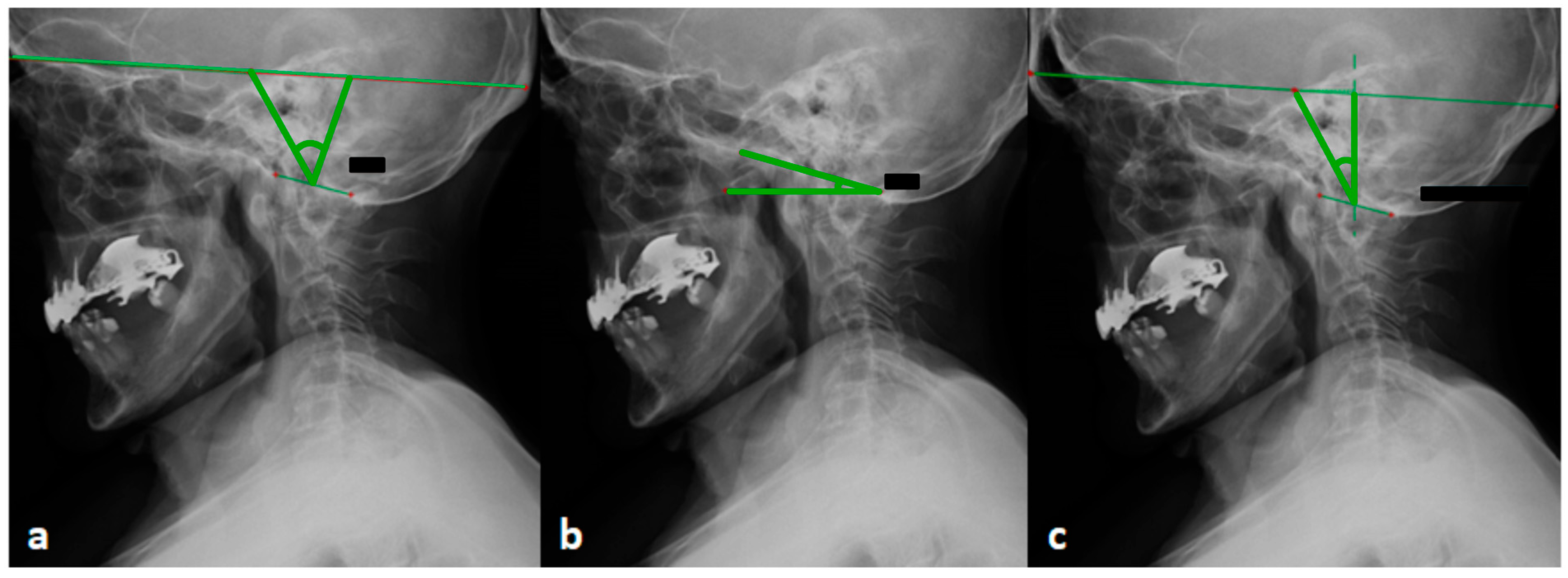
| OI (occipital incidence) | An angle between the line connecting the center of the skull and the center of foramen magnum, and the line perpendicular to the foramen magnum |
| OS (occipital slope) (mod. in W. Zhu) | An angle between the line parallel to the foremen magnum and the horizontal line (according to the W. Zhu modification) |
| OT (occipital tilt) | An angle between the line directed through the center of the skull and the center of the foramen magnum and SVA |
| McGS (McGregor slope) | An angle between the line from the posterosuperior aspect of the hard palate and the caudal aspect of the opisthion and the horizontal |
| CBVA (chin-brow vertical angle) | An angle measured between the lines from the brow and the chin to the vertical |
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Smolen, J.S.; Aletaha, D.; Barton, A.; Burmester, G.R.; Emery, P.; Firestein, G.S.; Kavanaugh, A.; McInnes, I.B.; Solomon, D.H.; Strand, V.; et al. Rheumatoid arthritis. Nat. Rev. Dis. Primers 2018, 4, 18001. [Google Scholar] [CrossRef] [PubMed]
- Szczeklik, A. Interna 2020; Medycyna Praktyczna: Kraków, Poland, 2020; pp. 2030–2045. [Google Scholar]
- Canale, S.T.; Beaty, J.H. Campbell’s Operative Orthopedics, 12th ed.; MediPage: Warszawa, Poland, 2016; pp. 2019–2022. [Google Scholar]
- Cunningham, S. Upper cervical instability associated with rheumatoid arthritis: A case report. J. Man. Manip. Ther. 2016, 24, 151–157. [Google Scholar] [CrossRef]
- Gillick, J.L.; Wainwright, J.; Das, K. Rheumatoid arthritis and the cervical spine: A review on the role of surgery. Int. J. Rheumatol. 2015, 2015, 252456. [Google Scholar] [CrossRef]
- Neva, M.H.; Myllykangas-Luosujarvi, R.; Kauppi, M. Mortality associated with cervical spine disorders: A population—Based study of 1666 patients with rheumatoid arthritis who died in Finland in 1989. Rheumatology 2001, 40, 123–127. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.V.; Ludwig, S.C.; Silber, J.; Gelb, D.E.; Anderson, P.A.; Frank, L.; Vaccaro, A.R. Rheumatoid arthritis of the cervical spine. Spine J. 2004, 4, 329–334. [Google Scholar] [CrossRef]
- Entezami, P.; Fox, D.A.; Clapham, P.J.; Chung, K.C. Historical perspective on the ethiology of rheumathoid arthritis. Hand. Clin. 2011, 27, 1–10. [Google Scholar] [CrossRef]
- Conlon, P.W.; Isdale, I.C.; Rose, B.S. Rheumatoid arthritis of the cervical spine. An analysis of 333 cases. Ann. Rheum. Dis. 1966, 25, 120–126. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Scheer, J.K.; Tang, J.A.; Smith, J.S.; Acosta, F.L., Jr.; Protopsaltis, T.S.; Blondel, B.; Bess, S.; Shaffrey, C.I.; Deviren, V.; Lafage, V.; et al. Cervical spine alignment, sagittal deformity, and clinical implications: A review. J. Neurosurg. Spine 2013, 19, 141–159. [Google Scholar] [CrossRef]
- White, A.A., 3rd; Panjabi, M.M. The basic kinematics of the human spine. A review of past and current knowledge. Spine 1978, 3, 12–20. [Google Scholar] [CrossRef]
- Wasserman, B.R.; Moskovich, R.; Razi, A.E. Rheumatoid arthritis of the cervical spine—Clinical considerations. Bull. NYU Hosp. Jt. Dis. 2011, 69, 136–148. [Google Scholar]
- Krauss, W.E.; Bledsoe, J.M.; Clarke, M.J.; Nottmeier, E.W.; Pichelmann, M.A. Rheumatoid arthritis of the craniovertebral junction. Neurosurgery 2010, 66 (Suppl. 3), 83–95. [Google Scholar] [CrossRef] [PubMed]
- Mańczak, M.; Gasik, R. Cervical spine instability in the course of rheumatoid arthritis—Imaging methods. Reumatologia 2017, 55, 201–207. [Google Scholar] [CrossRef]
- Ito, H.; Neo, M.; Sakamoto, T.; Fujibayashi, S.; Yoshitomi, H.; Nakamura, T. Subaxial subluxation after atlantoaxial transarticular screw fixation in rheumatoid patients. Eur. Spine J. 2009, 18, 869–876. [Google Scholar] [CrossRef] [PubMed]
- Ishii, K.; Matsumoto, M.; Takahashi, Y.; Okada, E.; Watanabe, K.; Tsuji, T.; Takaishi, H.; Nakamura, M.; Toyama, Y.; Chiba, K. Risk factors for development of subaxial subluxations following atlantoaxial arthrodesis for atlantoaxial subluxations in rheumatoid arthritis. Spine 2010, 35, 1551–1555. [Google Scholar] [CrossRef]
- Yoshimoto, H.; Ito, M.; Abumi, K.; Kotani, Y.; Shono, Y.; Takada, T.; Minami, A. A retrospective radiographic analysis of subaxial sagittal alignment after posterior C1-C2 fusion. Spine 2004, 29, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Zhu, S.; Xu, W.; Luo, Y.; Zhao, Y.; Liu, Y. Cervical spine involvement risk factors in rheumatoid arthritis: A meta-analysis. Int. J. Rheum. Dis. 2017, 20, 541–549. [Google Scholar] [CrossRef]
- Yurube, T.; Sumi, M.; Nishida, K.; Miyamoto, H.; Kohyama, K.; Matsubara, T.; Miura, Y.; Hirata, H.; Sugiyama, D.; Doita, M. Accelerated development of cervical spine instabilities in rheumatoid arthritis: A prospective minimum 5-year cohort study. PLoS ONE 2014, 9, e88970. [Google Scholar] [CrossRef]
- Terashima, Y.; Yurube, T.; Hirata, H.; Sugiyama, D.; Sumi, M.; Hyogo Organization of Spinal Disorders. Predictive Risk Factors of Cervical Spine Instabilities in Rheumatoid Arthritis: A Prospective Multicenter Over 10-Year Cohort Study. Spine 2017, 42, 556–564. [Google Scholar] [CrossRef]
- Baek, I.W.; Joo, Y.B.; Park, K.S.; Kim, K.J. Risk factors for cervical spine instability in patients with rheumatoid arthritis. Clin. Rheumatol. 2021, 40, 547–555. [Google Scholar] [CrossRef]
- Honda, S.; Murata, K.; Fujibayashi, S.; Otsuki, B.; Shimizu, T.; Fujii, T.; Okuzu, Y.; Kawai, T.; Kuroda, Y.; Onishi, A.; et al. Effect of high disease activity on spinal sagittal malalignment in patients with rheumatoid arthritis. J. Neurosurg. Spine 2024, 41, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Kuai, J.; Shi, M.; Xu, Z.; Chen, F.; Ding, Y.; Ni, B.; Wu, Y.; Guo, Q. The Influence of Cervical Ossification of the Posterior Longitudinal Ligament on Retro-odontoid Soft Tissue Thickness and Cervical Sagittal Balance. Clin. Spine Surg. 2025. ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Dubousset, J. Spinal Alignment, Balance and Harmony through the Ages. Int. J. Orth. 2019, 2, 19–24. [Google Scholar]
- During, J.; Goudfrooij, H.; Keessen, W.; Beeker, T.W.; Crowe, A. Toward standards for posture. Postural characteristics of the lower back system in normal and pathologic conditions. Spine 1985, 10, 83–87. [Google Scholar] [CrossRef] [PubMed]
- Stagnara, P.; De Mauroy, J.C.; Dran, G.; Gonon, G.P.; Costanzo, G.; Dimnet, J.; Pasquet, A. Reciprocal angulation of vertebral bodies in a sagittal plane: Approach to references for the evaluation of kyphosis and lordosis. Spine 1982, 7, 335–342. [Google Scholar] [CrossRef]
- Legaye, J.; Duval-Beaupère, G.; Hecquet, J.; Marty, C. Pelvic incidence: A fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur. Spine J. 1998, 7, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Vital, J.M.; Seneges, J.; Castelain, J.E. From the head to the feet: Anatomy of upright position. In Sagittal Balance of the Spine: From Normal to Pathology: A Key for Treatment Strategy, 1st ed.; Roussouly, P., Pinheiro-Franco, J., Labelle, H., Gechren, M., Eds.; Normative Values Following Age and Populations. Thieme: New York, NY, USA, 2019; pp. 24–42. [Google Scholar]
- Le Huec, J.C.; Thompson, W.; Mohsinaly, Y.; Barrey, C.; Faundez, A. Sagittal balance of the spine. Eur. Spine J. 2019, 28, 1889–1905. [Google Scholar] [CrossRef]
- Rajnics, P.; Pomero, V.; Templier, A.; Lavaste, F.; Illes, T. Computer-assisted assessment of spinal sagittal plane radiographs. J. Spinal Disord. 2001, 14, 135–142. [Google Scholar] [CrossRef]
- Colebatch, A.N.; Edwards, C.J.; Østergaard, M.; van der Heijde, D.; Balint, P.V.; D’Agostino, M.-A.; Forslind, K.; Grassi, W.; Haavardsholm, E.A.; Haugeberg, G.; et al. EULAR recommendations for the use of imaging of the joints in the clinical management of rheumatoid arthritis. Ann. Rheum. Dis. 2013, 72, 804–814. [Google Scholar] [CrossRef]
- Siempis, T.; Tsakiris, C.; Anastasia, Z.; Alexiou, G.A.; Voulgaris, S.; Argyropoulou, M.I. Radiological assessment and surgical management of cervical spine involvement in patients with rheumatoid arthritis. Rheumatol. Int. 2023, 43, 195–208. [Google Scholar] [CrossRef]
- Aletaha, D.; Neogi, T.; Silman, A.J.; Funovits, J.; Felson, D.T.; Bingham, C.O., 3rd; Birnbaum, N.S.; Burmester, G.R.; Bykerk, V.P.; Cohen, M.D.; et al. 2010 rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann. Rheum. Dis. 2010, 69, 1580–1588. [Google Scholar] [CrossRef]
- Joaquim, A.F.; Ghizoni, E.; Tedeschi, H.; Appenzeller, S.; Riew, K.D. Radiological evaluation of cervical spine involvement in rheumatoid arthritis. Neurosurg. Focus. 2015, 38, E4. [Google Scholar] [CrossRef]
- Yurube, T.; Sumi, M.; Nishida, K.; Miyamoto, H.; Kohyama, K.; Matsubara, T.; Miura, Y.; Sugiyama, D.; Doita, M.; Kobe Spine Conference. Incidence and aggravation of cervical spine instabilities in rheumatoid arthritis: A prospective minimum 5-year follow-up study of patients initially without cervical involvement. Spine 2012, 37, 2136–2144. [Google Scholar] [CrossRef]
- Yonezawa, T.; Tsuji, H.; Matsui, H.; Hirano, N. Subaxial lesions in rheumatoid arthritis. Radiographic factors suggestive of lower cervical myelopathy. Spine 1995, 20, 208–215. [Google Scholar] [CrossRef] [PubMed]
- White, A.A., 3rd; Johnson, R.M.; Panjabi, M.M.; Southwick, W.O. Biomechanical analysis of clinical stability in the cervical spine. Clin. Orthop. Relat. Res. 1975, 109, 85–96. [Google Scholar] [CrossRef] [PubMed]
- Ranawat, C.S.; O’Leary, P.; Pellicci, P.; Tsairis, P.; Marchisello, P.; Dorr, L. Cervical fusion in rheumatoid arthritis. J. Bone Jt. Surg. Am. 1979, 61, 1003–1010. [Google Scholar] [CrossRef] [PubMed]
- Riew, K.D.; Hilibrand, A.S.; Palumbo, M.A.; Sethi, N.; Bohlman, H.H. Diagnosing basilar invagination in the rheumatoid patient. The reliability of radiographic criteria. J. Bone Jt. Surg. Am. 2001, 83, 194–200. [Google Scholar] [CrossRef]
- Faro, F.D.; Marks, M.C.; Pawelek, J.; Newton, P.O. Evaluation of a functional position for lateral radiograph acquisition in adolescent idiopathic scoliosis. Spine 2004, 29, 2284–2289. [Google Scholar] [CrossRef]
- Zhu, W.; Sha, S.; Liu, Z.; Li, Y.; Xu, L.; Zhang, W.; Qiu, Y.; Zhu, Z. Influence of the Occipital Orientation on Cervical Sagittal Alignment: A Prospective Radiographic Study on 335 Normal Subjects. Sci. Rep. 2018, 8, 15336. [Google Scholar] [CrossRef]
- Kim, H.J.; Lenke, L.; Riew, D.; Oshima, Y.; Mesfin AFogelson, J.; Hershman, S.; Sides, B. Occipital incidence–a novel morphometric parameter for understanding occipitocervical spinal alignment. J. Spinal Disord. Tech. 2013, 13, 102–107. [Google Scholar]
- Moses, M.J.; Tishelman, J.C.; Zhou, P.L.; Moon, J.Y.; Beaubrun, B.M.; Buckland, A.J.; Protopsaltis, T.S. McGregor’s slope and slope of line of sight: Two surrogate markers for Chin-Brow vertical angle in the setting of cervical spine pathology. Spine J. 2019, 19, 1512–1517. [Google Scholar] [CrossRef]
- Ames, C.P.; Smith, J.S.; Scheer, J.K.; Shaffrey, C.I.; Lafage, V.; Deviren, V.; Moal, B.; Protopsaltis, T.; Mummaneni, P.V.; Mundis, G.M., Jr.; et al. A standardized nomenclature for cervical spine soft-tissue release and osteotomy for deformity correction: Clinical article. J. Neurosurg. Spine 2013, 19, 269–278. [Google Scholar] [CrossRef] [PubMed]
- Ames, C.P.; Smith, J.S.; Eastlack, R.; Blaskiewicz, D.J.; Shaffrey, C.I.; Schwab, F.; Bess, S.; Kim, H.J.; Mundis, G.M., Jr.; Klineberg, E.; et al. Reliability assessment of a novel cervical spine deformity classification system. J. Neurosurg. Spine 2015, 23, 673–683. [Google Scholar] [CrossRef] [PubMed]
- Koller, H.; Ames, C.; Mehdian, H.; Bartels, R.; Ferch, R.; Deriven, V.; Toyone, H.; Shaffrey, C.; Smith, J.; Hitzl, W.; et al. Characteristics of deformity surgery in patients with severe and rigid cervical kyphosis (CK): Results of the CSRS-Europe multi-centre study project. Eur. Spine J. 2019, 28, 324–344. [Google Scholar] [CrossRef]
- Kim, H.J.; Virk, S.; Elysee, J.; Ames, C.; Passias, P.; Shaffrey, C.; Mundis, G.; Protopsaltis, T.; Gupta, M.; Klineberg, E.; et al. Surgical strategy for the management of cervical deformity is based on type of cervical deformity. J. Clin. Med. 2021, 10, 4826. [Google Scholar] [CrossRef]
- Błaszczyk, J. Biomechanika Kliniczna, Podręcznik dla Studentów Medycyny i Fizjoterapii; WydawnictwoLekarskie PZWL: Warszawa, Poland, 2004; pp. 19–23. [Google Scholar]
- Knott, P.T.; Mardjetko, S.M.; Techy, F. The use of the T1 sagittal angle in predicting overall sagittal balance of the spine. Spine J. 2010, 10, 994–998. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Kim, K.T.; Seo, E.M.; Suk, K.S.; Kwack, Y.H.; Son, E.S. The influence of thoracic inlet alignment on the craniocervical sagittal balance in asymptomatic adults. J. Spinal Disord. Tech. 2012, 25, E41–E47. [Google Scholar] [CrossRef]
- Ames, C.P.; Blondel, B.; Scheer, J.K.; Schwab, F.J.; Le Huec, J.C.; Massicotte, E.M.; Patel, A.A.; Traynelis, V.C.; Kim, H.J.; Shaffrey, C.I.; et al. Cervical radiographical alignment: Comprehensive assessment techniques and potential importance in cervical myelopathy. Spine 2013, 38 (22 Suppl. 1), S149–S160. [Google Scholar] [CrossRef]
- Kapica, Z. Studia nad zmiennością wybranych właściwości taksonomiczno-antropometrycznych w kategoriach wieku dojrzałego. Acta Univ. Lodz. Folia Zool. Anthropol. 1981, 1, 3–15. [Google Scholar]
- Roy, I.B. Anthropology. The Study of Man; S Chand & Co Ltd.: New Delhi, India, 2016. [Google Scholar]
- Bogduk, N.; Mercer, S. Biomechanics of the cervical spine. I: Normal kinematics. Clin. Biomech. 2000, 15, 633–648. [Google Scholar]
- Mukerji, N.; Todd, N.V. Cervical myelopathy in rheumatoid arthritis. Neurol. Res. Int. 2011, 2011, 153628. [Google Scholar] [CrossRef]
- Iyer, S.; Kim, H.J. Cervical radiculopathy. Curr. Rev. Musculoskelet. Med. 2016, 9, 272–280. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Van Mameren, H. Motion Patterns in the Cervical Spine. Ph.D. Thesis, Maastricht University, Maastricht, The Netherlands, 1988. [Google Scholar] [CrossRef]
- Anderst, W.J.; Donaldson, W.F.; Lee, J.Y.; Kang, J.D. Cervical spine intervertebral kinematics with respect to the head are different during flexion and extension motions. J. Biomech. 2013, 46, 1471–1475. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wróblewski, R.; Koszela, K.; Mańczak, M.; Sudoł-Szopińska, I.; Gasik, R. Relationship between Cervical Instability in the Course of Rheumatoid Arthritis and Pelvic Parameters of Sagittal Balance. J. Clin. Med. 2023, 12, 6507. [Google Scholar] [CrossRef]
- Wróblewski, R.; Mańczak, M.; Gasik, R. Atlantoaxial Instability in the Course of Rheumatoid Arthritis in Relation to Selected Parameters of Sagittal Balance. J. Clin. Med. 2024, 13, 4441. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chen, Y.H.; Chen, K.H.; Ma, K.S. Finite element analysis of joints involved in rheumatoid arthritis. Int. J. Rheum. Dis. 2023, 26, 1393–1394. [Google Scholar] [CrossRef] [PubMed]
- Mena, A.; Wollstein, R.; Baus, J.; Yang, J. Finite Element Modeling of the Human Wrist: A Review. J. Wrist Surg. 2023, 12, 478–487. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Naoum, S.; Vasiliadis, A.V.; Koutserimpas, C.; Mylonakis, N.; Kotsapas, M.; Katakalos, K. Finite Element Method for the Evaluation of the Human Spine: A Literature Overview. J. Funct. Biomater. 2021, 12, 43. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lin, M.; Paul, R.; Dhar, U.K.; Doulgeris, J.; O’Connor, T.E.; Tsai, C.T.; Vrionis, F.D. A Review of Finite Element Modeling for Anterior Cervical Discectomy and Fusion. Asian Spine J. 2023, 17, 949–963. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]

| Number of Cases SAS and Percentage of Recognized Instability. | ||
|---|---|---|
| Type of Instability | Cases of Instability | Percentage |
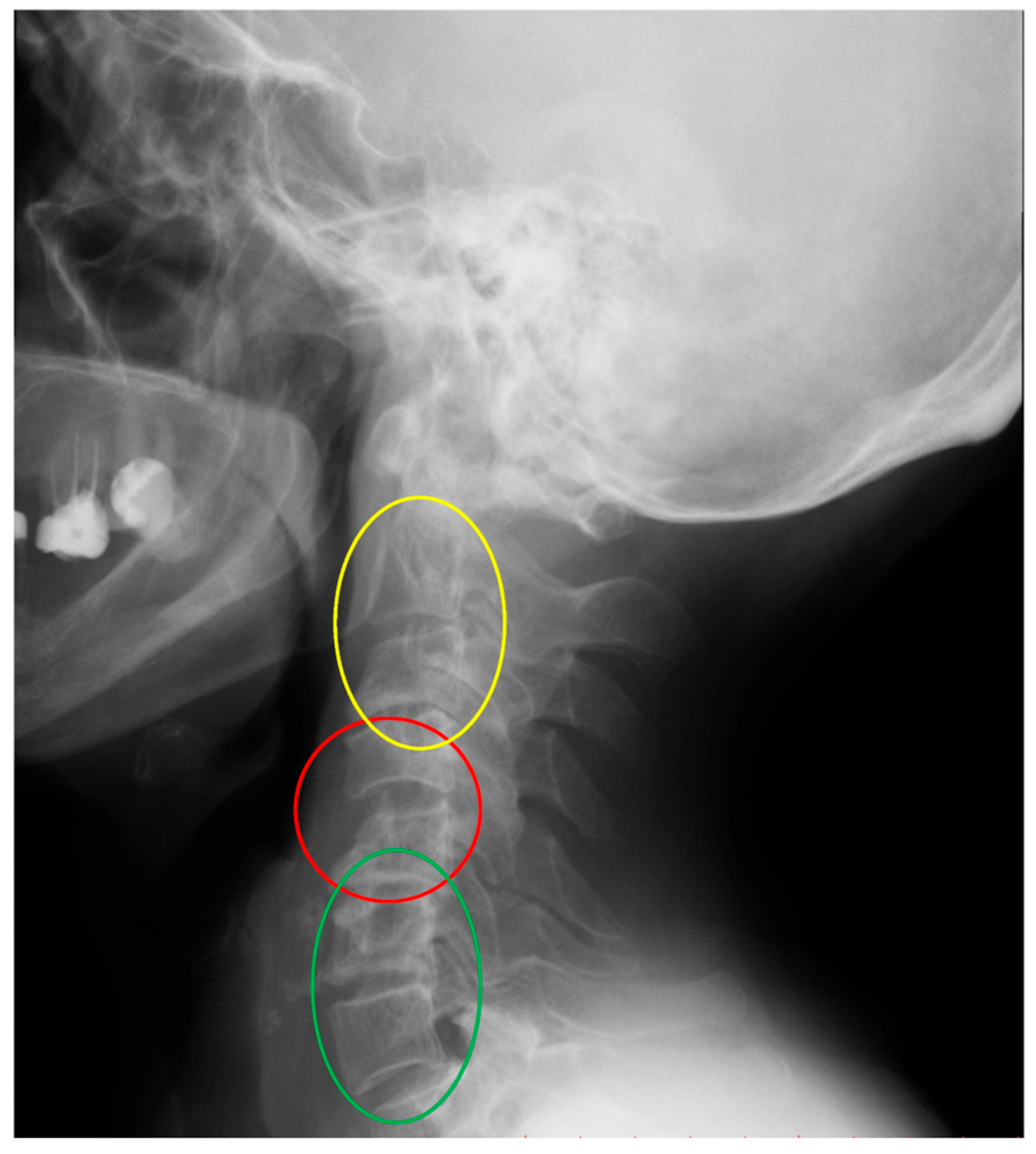
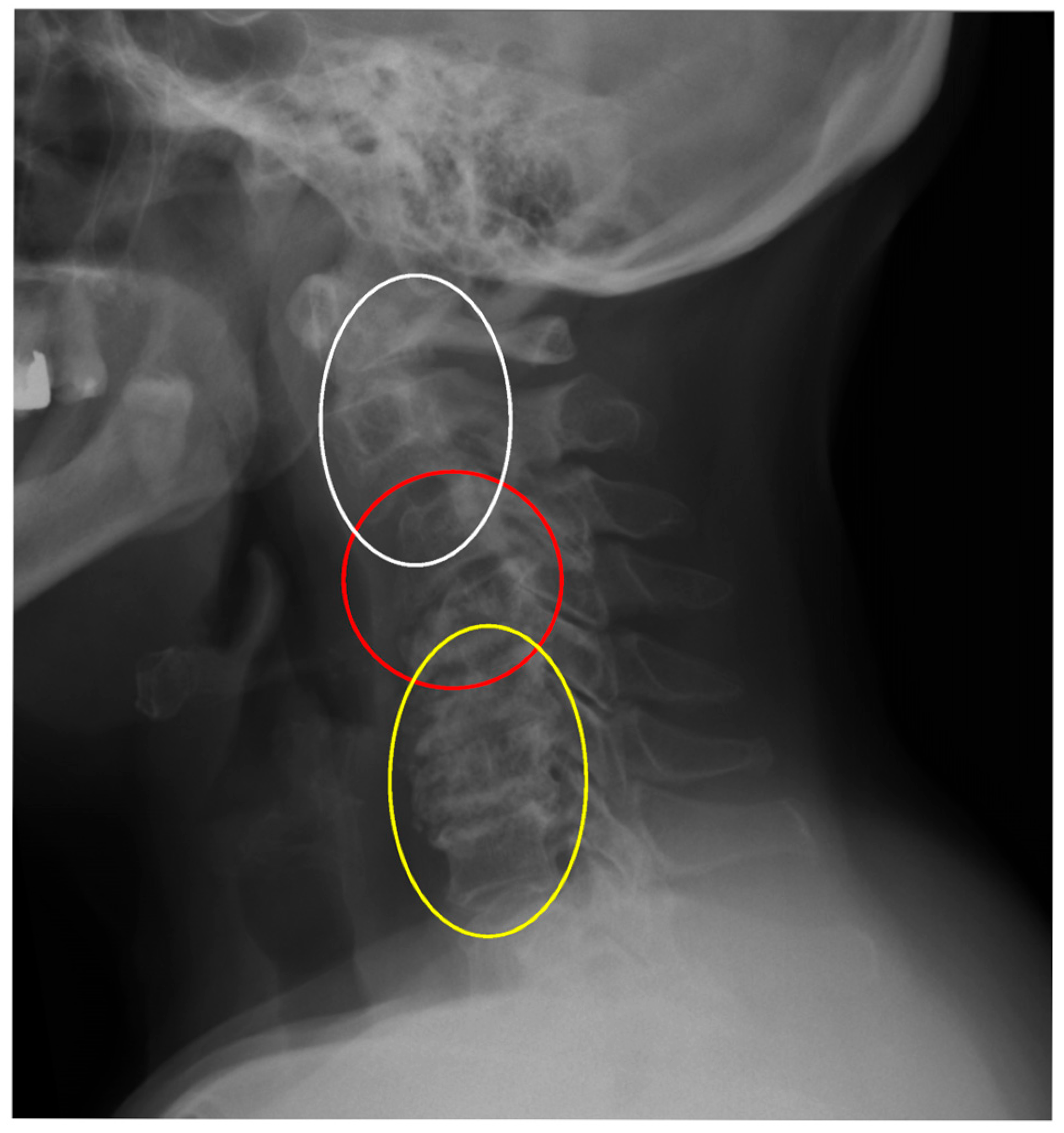
| C2–C3 | 11 | 17.4% |
| C3–C4 | 17 | 27% |
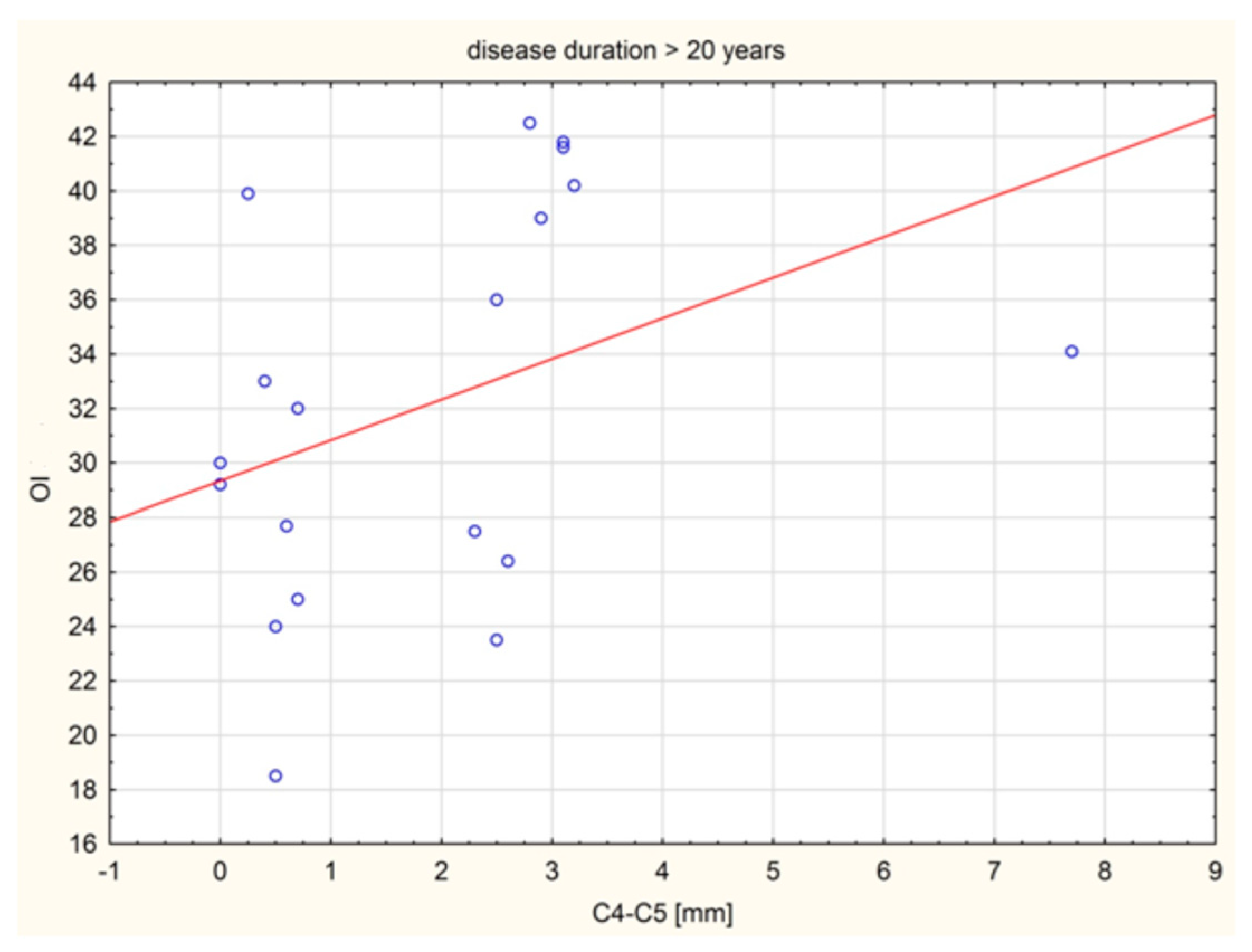
| C4–C5 | 23 | 36.5% |
| C5–C6 | 10 | 15.9% |
| C6–C7 | 2 | 3.2% |
| Variable | Spearman’s Correlation Coefficients | ||
|---|---|---|---|
| Number of Cases n = 54 | Patients with Duration of RA > 20 y n = 21 | Patients with Duration of RA ≤ 20 y n = 24 | |
| COG–C7 SVA (mm) | −0.030 | −0.051 | −0.167 |
| C2–C7 SVA (mm) | 0.122 | 0.084 | 0.042 |
| C7 SVA (mm) | −0.101 | −0.085 | −0.118 |
| OI (deg.) | 0.216 | 0.477 | −0.197 |
| OS(deg.) (mod. in W. Zhu) | −0.075 | 0.264 | −0.302 |
| OT (deg.) | 0.201 | 0.313 | 0.021 |
| McGS (deg.) | 0.015 | 0.069 | 0.032 |
| C1–C7 Cobb angle | 0.091 | 0.243 | 0.022 |
| C0–C2 Cobb angle | −0.192 | −0.202 | −0.254 |
| C2–C7 Cobb angle | −0.061 | −0.016 | 0.143 |
| C7S (deg.) | 0.053 | 0.122 | 0.092 |
| T1S (deg.) | 0.180 | 0.084 | 0.110 |
| ThK Cobb angle | −0.142 | 0.148 | −0.147 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wróblewski, R.; Mańczak, M.; Gasik, R. Subaxial Subluxation (SAS) and Cervical Deformity in Patients with Rheumatoid Arthritis in Relation to Selected Sagittal Balance Parameters. J. Clin. Med. 2025, 14, 4954. https://doi.org/10.3390/jcm14144954
Wróblewski R, Mańczak M, Gasik R. Subaxial Subluxation (SAS) and Cervical Deformity in Patients with Rheumatoid Arthritis in Relation to Selected Sagittal Balance Parameters. Journal of Clinical Medicine. 2025; 14(14):4954. https://doi.org/10.3390/jcm14144954
Chicago/Turabian StyleWróblewski, Robert, Małgorzata Mańczak, and Robert Gasik. 2025. "Subaxial Subluxation (SAS) and Cervical Deformity in Patients with Rheumatoid Arthritis in Relation to Selected Sagittal Balance Parameters" Journal of Clinical Medicine 14, no. 14: 4954. https://doi.org/10.3390/jcm14144954
APA StyleWróblewski, R., Mańczak, M., & Gasik, R. (2025). Subaxial Subluxation (SAS) and Cervical Deformity in Patients with Rheumatoid Arthritis in Relation to Selected Sagittal Balance Parameters. Journal of Clinical Medicine, 14(14), 4954. https://doi.org/10.3390/jcm14144954






