Training Interventions Used in Postmenopausal Women to Improve Pelvic Floor Muscle Function Related to Urinary Continence—A Systematic Review
Abstract
1. Introduction
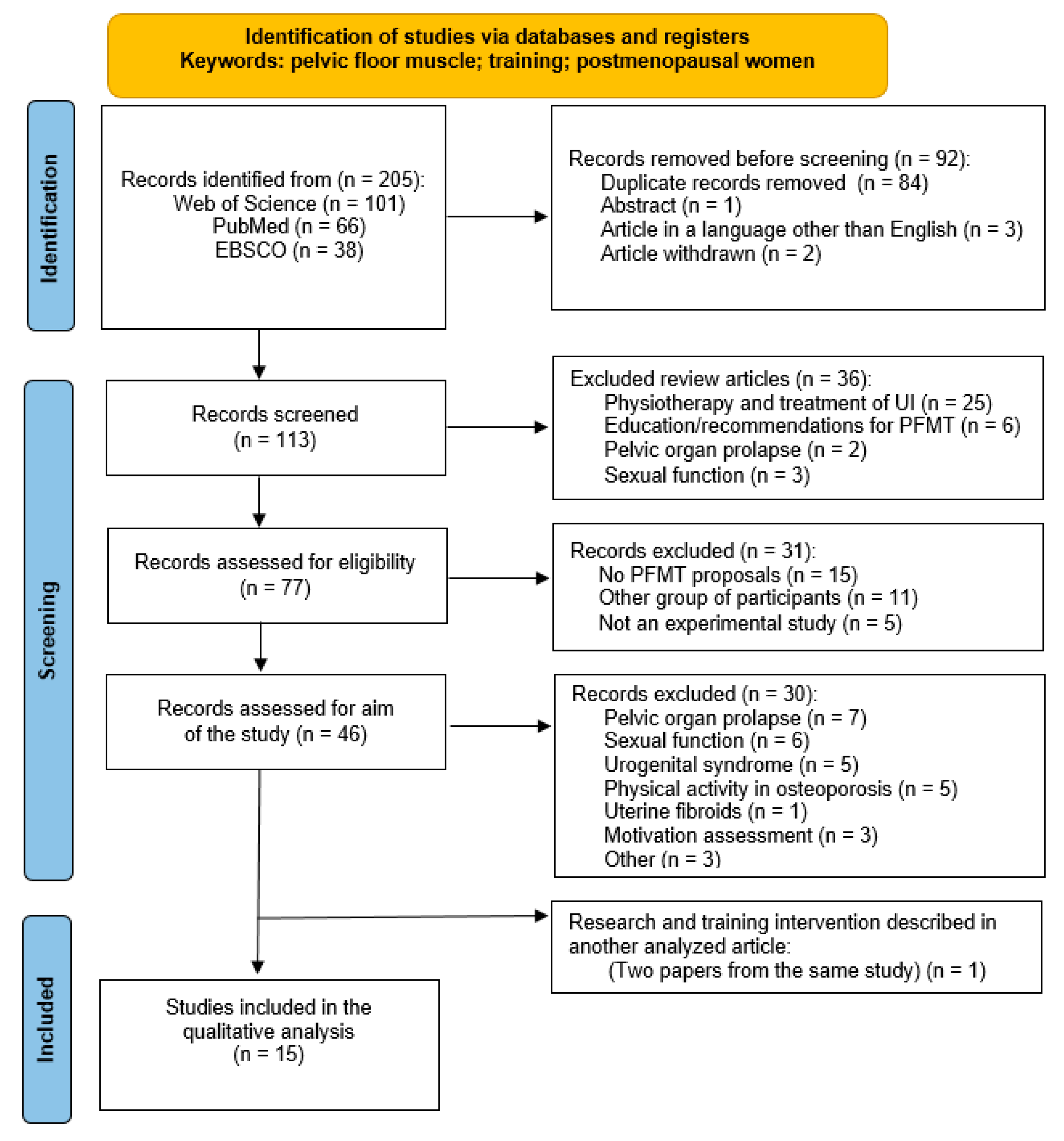
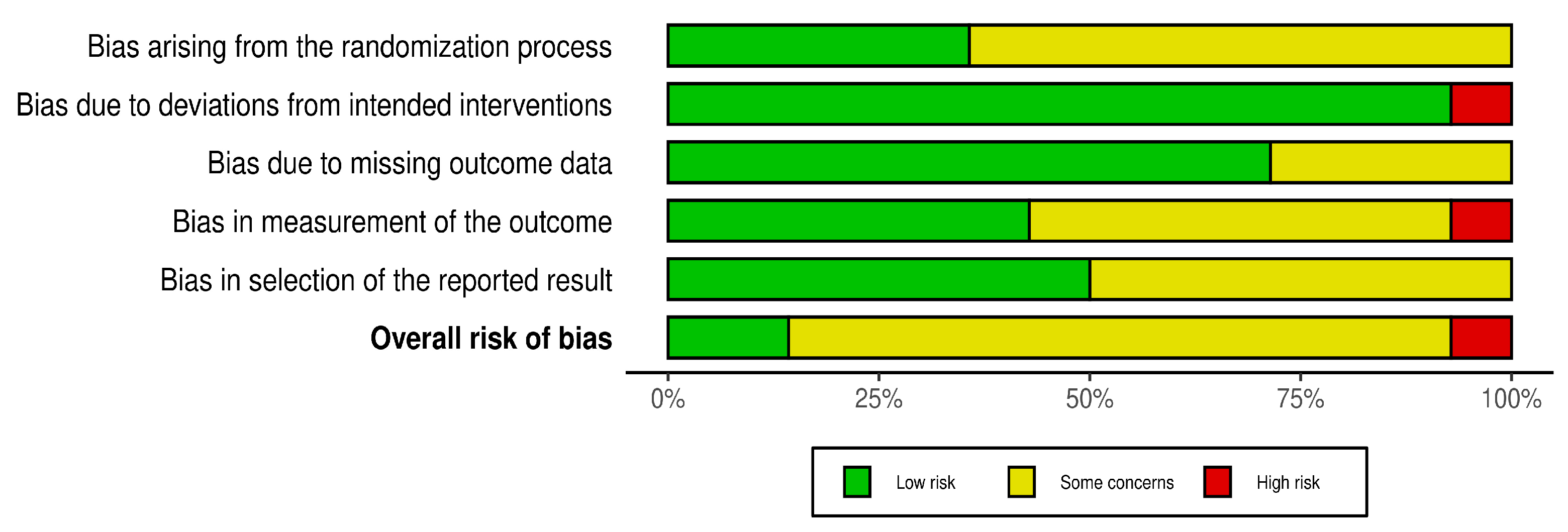
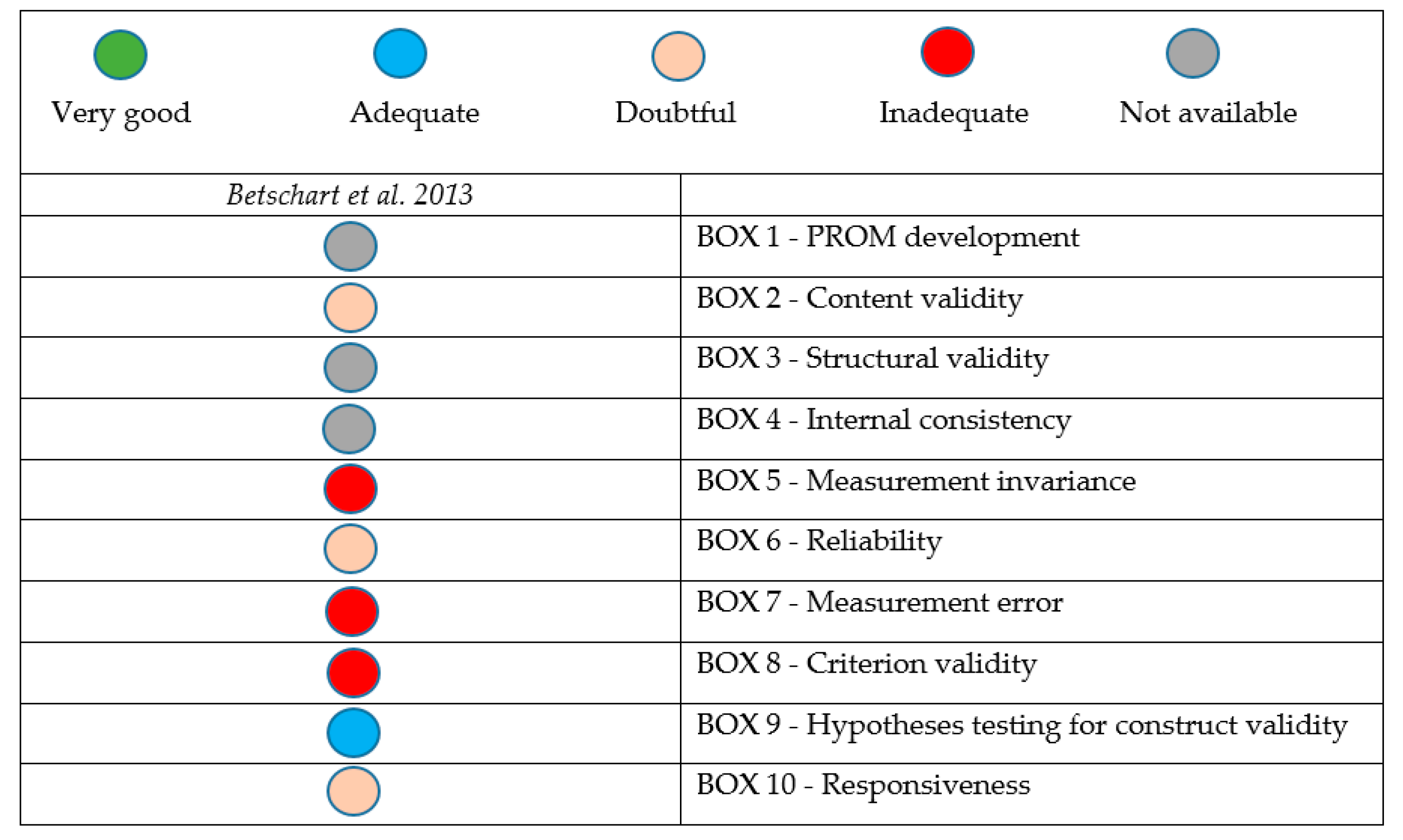
2. Materials and Methods
3. Results
4. Discussion
Limitations and Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BF | Biofeedback |
| BMI | Body mass index |
| ES | Electrical stimulation |
| G | Group |
| HIFEMT | High-intensity focused electromagnetic therapy |
| ICIQ-OAB | International Consultation on Incontinence Questionnaire Overactive Bladder |
| ICIQ-UI-SF | International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form |
| IIQ-7 | Incontinence Impact Questionnaire Short Form |
| KHQ | King’s Health Questionnaire |
| MENQOL | Menopause-specific quality of life questionnaire |
| MVC | Maximal voluntary contraction |
| NRCT | Non-randomized controlled trial |
| PFM | Pelvic floor muscle |
| PFMT | Pelvic floor muscle training |
| RCT | Randomized controlled trial |
| RoB | Risk of bias |
| RUIS | Revised Urinary Incontinence Scale |
| QoL | Quality of life |
| sEMG | Surface electromyography |
| UI | Urinary incontinence |
| UDS | Urodynamics |
| VLPP | Valsalva leak point pressure |
| VRP | Vaginal resting pressure |
References
- Bo, K.; Frawley, H.C.; Haylen, B.T.; Abramov, Y.; Almeida, F.G.; Berghmans, B.; Bortolini, M.; Dumoulin, C.; Gomes, M.; McClurg, D.; et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for the conservative and nonpharmacological management of female pelvic floor dysfunction. Int. Urogynecol. J. 2017, 28, 191–213. [Google Scholar] [CrossRef] [PubMed]
- Sam, P.; LaGrange, C. Anatomy, Abdomen and Pelvis, Penis. Available online: https://www.ncbi.nlm.nih.gov/books/NBK482236/ (accessed on 10 February 2025).
- Omodei, M.S.; Marques Gomes Delmanto, L.R.; Carvalho-Pessoa, E.; Schmitt, E.B.; Nahas, G.P.; Petri Nahas, E.A. Association Between Pelvic Floor Muscle Strength and Sexual Function in Postmenopausal Women. J. Sex. Med. 2019, 16, 1938–1946. [Google Scholar] [CrossRef] [PubMed]
- Zhuo, Z.H.; Wang, C.H.; Yu, H.M.; Li, J. The Relationship Between Pelvic Floor Function and Sexual Function in Perimenopausal Women. Sex. Med. 2021, 9, 100441. [Google Scholar] [CrossRef] [PubMed]
- Okeahialam, N.A.; Dworzynski, K.; Jacklin, P.; McClurg, D. Prevention and non-surgical management of pelvic floor dysfunction: Summary of NICE guidance. BMJ 2022, 376, n3049. [Google Scholar] [CrossRef]
- Mottola, M.F.; Davenport, M.H.; Ruchat, S.M.; Davies, G.A.; Poitras, V.J.; Gray, C.E.; Jaramillo Garcia, A.; Barrowman, N.; Adamo, K.B.; Duggan, M.; et al. 2019 Canadian guideline for physical activity throughout pregnancy. Br. J. Sports Med. 2018, 52, 1339–1346. [Google Scholar] [CrossRef]
- Gordon, S.; Ruivo, D.B.; Viscardi, L.G.A.; Oliveira, A.S.d. Effects of the Pilates method isolated and associated with manual therapy in women with urinary incontinence. Man. Ther. Posturology Rehabil. J. 2020, 18, 1–6. [Google Scholar] [CrossRef]
- Abufaraj, M.; Xu, T.; Cao, C.; Siyam, A.; Isleem, U.; Massad, A.; Soria, F.; Shariat, S.F.; Sutcliffe, S.; Yang, L. Prevalence and trends in urinary incontinence among women in the United States, 2005–2018. Am. J. Obs. Gynecol. 2021, 225, 166.e1–166.e12. [Google Scholar] [CrossRef]
- Milsom, I.; Gyhagen, M. The prevalence of urinary incontinence. Climacteric 2019, 22, 217–222. [Google Scholar] [CrossRef]
- El Khoudary, S.R.; Greendale, G.; Crawford, S.L.; Avis, N.E.; Brooks, M.M.; Thurston, R.C.; Karvonen-Gutierrez, C.; Waetjen, L.E.; Matthews, K. The menopause transition and women’s health at midlife: A progress report from the Study of Women’s Health Across the Nation (SWAN). Menopause-J. N. Am. Menopause Soc. 2019, 26, 1213–1227. [Google Scholar] [CrossRef]
- Prajapati, M.M. Awareness regarding menopausal symptoms and effect on daily life among postmenopausal women. J. Patan Acad. Health Sci. 2020, 7, 130–136. [Google Scholar] [CrossRef]
- Seyyedi, F.; Rafiean-Kopaei, M.; Miraj, S. Comparison of the Effects of Vaginal Royal Jelly and Vaginal Estrogen on Quality of Life, Sexual and Urinary Function in Postmenopausal Women. J. Clin. Diagn. Res. 2016, 10, Qc01–Qc05. [Google Scholar] [CrossRef] [PubMed]
- Oplawski, M.; Smoczynska, M.; Grabarek, B.O.; Boron, D. Assessment of Dysfunction in the Urinary System as Well as Comfort in the Life of Women during and after Combination Therapy Due to Ovarian and Endometrial Cancer Based on the SWL, II-Q7 and UDI-6 Scales. J. Clin. Med. 2021, 10, 1228. [Google Scholar] [CrossRef] [PubMed]
- KEGEL, A. Progressive resistance exercise in the functional restoration of the perineal muscles. Am. J. Obstet. Gynecol. 1948, 56, 238–248. [Google Scholar] [CrossRef] [PubMed]
- Hay-Smith, E.J.; LC, B.B.; Hendriks, H.J.; de Bie, R.A.; van Waalwijk van Doorn, E.S. Pelvic floor muscle training for urinary incontinence in women. Cochrane Database Syst. Rev. 2008, 2008, Cd001407. [Google Scholar] [CrossRef]
- Kolodynska, G.; Zalewski, M.; Mucha, A.; Andrzejewski, W. Assessment of the Effectiveness of the Sonofeedback Method in the Treatment of Stress Urinary Incontinence in Women-Preliminary Report. J. Clin. Med. 2022, 11, 659. [Google Scholar] [CrossRef]
- Elgayar, S. Combined effects of high-intensity focused electromagnetic therapy and pelvic floor exercises on pelvic floor muscles and sexual function in postmenopausal women. Obstet. Gynecol. Sci. 2024, 67, 574–585. [Google Scholar] [CrossRef]
- Campanini, I.; Disselhorst-Klug, C.; Rymer, W.Z.; Merletti, R. Surface EMG in Clinical Assessment and Neurorehabilitation: Barriers Limiting Its Use. Front. Neurol. 2020, 11, 934. [Google Scholar] [CrossRef]
- Hagen, S.; Elders, A.; Stratton, S.; Sergenson, N.; Bugge, C.; Dean, S.; Hay-Smith, J.; Kilonzo, M.; Dimitrova, M.; Abdel-Fattah, M.; et al. Effectiveness of pelvic floor muscle training with and without electromyographic biofeedback for urinary incontinence in women: Multicentre randomised controlled trial. BMJ-Br. Med. J. 2020, 371, 3719. [Google Scholar] [CrossRef]
- Piernicka, M.; Ossowski, Z.; Kortas, J.; Bojar, D.; Labun, J.; Szumilewicz, A. Can We Improve the Technique of Pelvic Floor Muscle Exercises in Postmenopausal Women Using a Single Electromyography Biofeedback Session? An Experimental Study. J. Clin. Med. 2024, 13, 3062. [Google Scholar] [CrossRef]
- Romeikienė, K.E.; Bartkevičienė, D. Pelvic-Floor Dysfunction Prevention in Prepartum and Postpartum Periods. Medicina 2021, 57, 387. [Google Scholar] [CrossRef]
- Medicine, A.C.o.S. ACS’M Resources for the Personal Trainer, 5th ed.; Wolters Kluwer: Philadelphia, PA, USA, 2017. [Google Scholar]
- Page, M.; McKenzie, J.; Bossuyt, P.; Boutron, I.; Hoffmann, T.; Mulrow, C.; Shamseer, L.; Tetzlaff, J.; Akl, E.; Brennan, S.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.; Savovic, J.; Page, M.; Elbers, R.; Blencowe, N.; Boutron, I.; Cates, C.; Cheng, H.; Corbett, M.; Eldridge, S.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ-Br. Med. J. 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- McGuinness, L.; Higgins, J. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 2021, 12, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Mokkink, L.; Boers, M.; van der Vleuten, C.; Bouter, L.; Alonso, J.; Patrick, D.; de Vet, H.; Terwee, C. COSMIN Risk of Bias tool to assess the quality of studies on reliability or measurement error of outcome measurement instruments: A Delphi study. BMC Med. Res. Methodol. 2020, 20, 1–13. [Google Scholar] [CrossRef]
- Pereira, V.S.; de Melo, M.V.; Correia, G.N.; Driusso, P. Long-term effects of pelvic floor muscle training with vaginal cone in post-menopausal women with urinary incontinence: A randomized controlled trial. Neurourol. Urodyn. 2013, 32, 48–52. [Google Scholar] [CrossRef]
- Pereira, V.; de Melo, M.; Correia, G.; Driusso, P. Vaginal cone for postmenopausal women with stress urinary incontinence: Randomized, controlled trial. Climacteric 2012, 15, 45–51. [Google Scholar] [CrossRef]
- Alves, F.; Riccetto, C.; Adami, D.; Marques, J.; Pereira, L.; Palma, P.; Botelho, S. A pelvic floor muscle training program in postmenopausal women: A randomized controlled trial. Maturitas 2015, 81, 300–305. [Google Scholar] [CrossRef]
- Antônio, F.; Herbert, R.; Bo, K.; Rosa-e-Silva, A.; Lara, L.; Franco, M.; Ferreira, C. Pelvic floor muscle training increases pelvic floor muscle strength more in post-menopausal women who are not using hormone therapy than in women who are using hormone therapy: A randomised trial. J. Physiother. 2018, 64, 166–171. [Google Scholar] [CrossRef]
- Castellani, D.; Saldutto, P.; Galica, V.; Pace, G.; Biferi, D.; Galatioto, G.; Vicentini, C. Low-Dose Intravaginal Estriol and Pelvic Floor Rehabilitation in Post-Menopausal Stress Urinary Incontinence. Urol. Int. 2015, 95, 417–421. [Google Scholar] [CrossRef]
- Tosun, Ö.; Mutlu, E.; Tosun, G.; Ergenoglu, A.; Yeniel, A.; Malkoç, M.; Askar, N.; Itil, I. Do stages of menopause affect the outcomes of pelvic floor muscle training? Menopause-J. N. Am. Menopause Soc. 2015, 22, 175–184. [Google Scholar] [CrossRef]
- Martinho, N.; Silva, V.; Marques, J.; Carvalho, L.; Iunes, D.; Botelho, S. The effects of training by virtual reality or gym ball on pelvic floor muscle strength in postmenopausal women: A randomized controlled trial. Braz. J. Phys. Ther. 2016, 20, 248–257. [Google Scholar] [CrossRef] [PubMed]
- Bertotto, A.; Schvartzman, R.; Uchôa, S.; Wender, M. Effect of electromyographic biofeedback as an add-on to pelvic floor muscle exercises on neuromuscular outcomes and quality of life in postmenopausal women with stress urinary incontinence: A randomized controlled trial. Neurourol. Urodyn. 2017, 36, 2142–2147. [Google Scholar] [CrossRef]
- Elbandrawy, A.M.; Mahmoud, S.G.; AboElinin, M.F.; Yousef, A.M. Effect of Aerobic Walking Exercise on Stress Urinary Incontinence in Postmenopausal Women. Women Sport. Phys. Act. J. 2022, 30, 11–17. [Google Scholar] [CrossRef]
- Tang, Y.; Guo, X.; Wang, Y.; Liu, Z.; Cao, G.; Zhou, Y.; Chen, M.; Liu, J.; Mu, J.; Yuan, M. Rumba Dance Combined with Breathing Training as an Exercise Intervention in the Management of Stress Urinary Incontinence in Postmenopausal Women: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2022, 20, 522. [Google Scholar] [CrossRef] [PubMed]
- Gonzaga, S.; de Oliveira, R.; Dutra, L.; Oliveira, L.; de Oliveira, L. Comparative analysis of pelvic floor muscle training and Pilates in managing urinary incontinence among postmenopausal women: A randomized controlled trial. Int. Urogynecol. J. 2024, 35, 561–569. [Google Scholar] [CrossRef]
- Betschart, C.; Mol, S.; Lütolf-Keller, B.; Fink, D.; Perucchini, D.; Scheiner, D. Pelvic Floor Muscle Training for Urinary Incontinence: A Comparison of Outcomes in Premenopausal Versus Postmenopausal Women. Female Pelvic Med. Reconstr. Surg. 2013, 19, 219–224. [Google Scholar] [CrossRef]
- Botelho, S.; Martinho, N.; Silva, V.; Marques, J.; Carvalho, L.; Riccetto, C. Virtual reality: A proposal for pelvic floor muscle training. Int. Urogynecol. J. 2015, 26, 1709–1712. [Google Scholar] [CrossRef] [PubMed]
- Botelho, S.; Martinho, N.; Silva, V.; Marques, J.; Alves, F.; Riccetto, C. Abdominopelvic kinesiotherapy for pelvic floor muscle training: A tested proposal in different groups. Int. Urogynecol. J. 2015, 26, 1867–1869. [Google Scholar] [CrossRef]
- Bludnicka, M.; Piernicka, M.; Kortas, J.; Biernacka, B.D.; Szumilewicz, A. Effects of a One-Time Biofeedback EMG Session on Neuromuscular Activity of the Pelvic Floor Muscles in Pregnant Women. Neurophysiology 2020, 52, 438–445. [Google Scholar] [CrossRef]
- Villani, F.; Petre, I.; Buleu, F.; Iurciuc, S.; Marc, L.; Apostol, A.; Valentini, C.; Donati, E.; Simoncini, T.; Furau, C. Pelvic Floor Muscle Training vs. Vaginal Vibration Cone Therapy for Postpartum Dyspareunia and Vaginal Laxity. Medicina 2024, 61, 23. [Google Scholar] [CrossRef]
- Gameiro, M.O.; Moreira, E.H.; Gameiro, F.O.; Moreno, J.C.; Padovani, C.R.; Amaro, J.L. Vaginal weight cone versus assisted pelvic floor muscle training in the treatment of female urinary incontinence. A prospective, single-blind, randomized trial. Int. Urogynecol. J. 2010, 21, 395–399. [Google Scholar] [CrossRef] [PubMed]
- Hamine, S.; Gerth-Guyette, E.; Faulx, D.; Green, B.B.; Ginsburg, A.S. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: A systematic review. J. Med. Internet Res. 2015, 17, e52. [Google Scholar] [CrossRef]
- -Ahmed, R.; Taithongchai, A.; da Silva, A.; Robinson, D.; Cardozo, L. Treating and Managing Urinary Incontinence: Evolving and Potential Multicomponent Medical and Lifestyle Interventions. Res. Rep. Urol. 2023, 15, 193–203. [Google Scholar] [CrossRef]
- Asklund, I.; Nyström, E.; Sjöström, M.; Umefjord, G.; Stenlund, H.; Samuelsson, E. Mobile app for treatment of stress urinary incontinence: A randomized controlled trial. Neurourol. Urodyn. 2017, 36, 1369–1376. [Google Scholar] [CrossRef] [PubMed]
- Harper, R.; Sheppard, S.; Stewart, C.; Clark, C. Exploring Adherence to Pelvic Floor Muscle Training in Women Using Mobile Apps: Scoping Review. JMIR Mhealth Uhealth 2023, 11, e45947. [Google Scholar] [CrossRef]
- Piernicka, M.; Bludnicka, M.; Kortas, J.; Duda-Biernacka, B.; Szumilewicz, A. High-impact aerobics programme supplemented by pelvic floor muscle training does not impair the function of pelvic floor muscles in active nulliparous women A randomized control trial. Medicine 2021, 100, e26989. [Google Scholar] [CrossRef]
- Bapir, R.; Bhatti, K.H.; Eliwa, A.; García-Perdomo, H.A.; Gherabi, N.; Hennessey, D.; Magri, V.; Mourmouris, P.; Ouattara, A.; Perletti, G.; et al. Treatment of urge incontinence in postmenopausal women: A systematic review. Arch. Ital. di Urol. e Androl. 2023, 95, 11718. [Google Scholar] [CrossRef] [PubMed]
- Woodley, S.J.; Boyle, R.; Cody, J.D.; Morkved, S.; Hay-Smith, E.J.C. Pelvic floormuscle training for prevention and treatment of urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst. Rev. 2017, 12, CD007471. [Google Scholar] [CrossRef]
- Piernicka, M.; Duda-Biernacka, B.; Bludnicka, M.; Szumilewicz, A. The Characteristics of the Pelvic Floor Muscle Training Programs Used in Experimental Studies with Surface Electromyography in Non-Pregnant Women: A Systematic Review. Iran. J. Public Health 2020, 49, 1022–1032. [Google Scholar] [CrossRef]

| Author, Year | Characteristics of the Study | Research Tools | Training Effectiveness |
|---|---|---|---|
| Pereira et al. 2012 [28] 2013 [27] | Treatment of stress urinary incontinence, n = 45 G1 (n = 15)—Vaginal cones (age: 66 ± 11; BMI: 27.89 ± 1.93) G2 (n = 15)—PFMT (age: 63 ± 11; BMI: 25.65 ± 2.79) G3 (n = 15)—Control (age: 63 ± 9; BMI: 26.04 ± 1.84) | (a) 1 h pad test (b) perineometer (c) questionnaires: QoL KHQ | Statistically significant improvement in both intervention groups (G1 and G2) in both decreased urine leakage and increase in PFM pressure. Both groups noticed an improvement in the quality of life. |
| Betschart et al. 2013 [38] | Treatment of urinary incontinence, n = 120 G1 (n = 41)—Premenopausal women (PFMT) (age: 41 ± 4; BMI: 27.0 ± 6.8) G2 (n = 79)—Postmenopausal women (PFMT) (age: 74 ± 6; BMI: 27.4 ± 5.6) | UI questionnaire based on a four-point Likert scale | There was a noticeable improvement in both groups, and no differences were observed between the groups. Changes were not statistically significant. |
| Alves et al. 2015 [29] | Treatment of urinary incontinence, n = 42 G1 (n = 18)—Treatment (PFMT) (age: 66 ± 9; BMI: 29.43 ± 3.91) G2 (n = 12)—Control (age: 66 ± 9; BMI: 31.52 ± 5.71) | (a) digital palpation; (b) sEMG assessment; questionnaires: ICIQ-UI SF | (a–c) Statistically significant improvement in G1 |
| Botelho et al. 2015a [40] | Improving the function of the PFM, (PFMT) n = 82 G1 (n = 11)—Nulliparous women (age: 25 ± 4) G2 (n = 13)—Primiparous pregnant (age: 23 ± 6) G3 (n = 20)—Primiparous postpartum (age: 23 ± 6) G4 (n = 38)—Postmenopausal women (age: 65 ± 8) | (a) digital palpation; (b) sEMG or vaginal dynamometry; (c) questionnaires: ICIQ-UI SF; ICIQ-OAB | Statistically significant improvement in all intervention groups in both decreased urine leakage and increase in PFM pressure. All groups noticed an improvement in their quality of life. |
| Botelho et al. 2015b [39] | Improving the function of the PFM, n = 46 (video game on a pressure base platform) G1 (n = 19)—Nulliparous women without urinary incontinence (age: 25 ± 4) G2 (n = 27)—Postmenopausal women with urinary incontinence (age: 62 ± 8) | (a) G1: digital palpation; sEMG G2: vaginal dynamometry and digital palpation; (b) questionnaires: ICIQ-UI SF; ICIQ-OAB | In G1, a significant increase in strength was noted on palpation, which was not confirmed by sEMG. In G2, there were no changes in digital palpation, but there was improvement in dynamometer assessment and questionnaires. |
| Castellani et al. 2015 [31] | Treatment of urinary incontinence, n = 69 G1 (n = 35)—PFMT + ES + BF (age: 55 ± 5; BMI: 25.2 ± 2.1) G2 (n = 34)—PFMT + ES + BF + 1 mg intravaginal estriol ovule once daily for 4 weeks and then two ovules once weekly for 20 weeks (age: 55 ± 6; BMI: 24.7 ± 2.2) | (a) UDS/VLPP 1 h pad test (b) questionnaires: IIQ-7 | (a) Symptoms scores and incontinence status were statistically significant better in G2; (b) Statistically significant improvement in both groups. |
| Tosun et al. 2015 [32] | Treatment of urinary incontinence, n = 103 G1 (n = 41)—Late reproductive age/early transitional (age: 46 ± 6; BMI: 30.23 ± 6.64) G2 (n = 32)—Final menstrual bleeding 2–5 years ago (age: 52 ± 5; BMI: 30.55 ± 5.5) G3 (n = 30)—Final menstrual bleeding more than 5 years ago (age: 67 ± 7; BMI: 27.06 ± 5.0) | 1 h pad test; PERFECT scheme; Brink scale; perineometry; ultrasound | Statistically significant increase in PERFECT scheme, Brink scale, perineometry, and ultrasound values among the three groups. |
| Martinho et al. 2016 [33] | Improving the function of the PFM, n = 47 G1 (n = 27)—Abdominopelvic training by virtual reality (age: 62 ± 9; BMI: 28.1 ± 3.9) G2 (n = 20)—PFMT using by gym ball (age: 62 ± 9; BMI: 28 ± 3.7) | digital palpation; vaginal dynamometry | Only the endurance parameter showed a significant difference between groups, given that the G1 had a significant improvement after training, while the G2 had a significant decrease in the same parameter. |
| Bertotto et al. 2017 [34] | Treatment of urinary incontinence, n = 45 G1 (n = 15)—PFMT (age: 59 ± 5; BMI: 27.7 ± 3.6) G2 (n = 16)—PFMT + biofeedback (age: 58 ± 7; BMI: 27.5 ± 2.6) G3 (n = 14)—Control group (age: 57 ± 5; BMI: 26.8 ± 3.6) | digital palpation; sEMG + biofeedback; questionnaire: QoL | Significant improvement in both intervention groups. The duration of endurance contraction and MVC showed significantly greater improvement in G2. |
| Antônio et al. 2018 [30] | Improving the function of the PFM, n = 99 G1 * (n = 51)—PFMT (age: 53 ± 4; BMI: 28.5 ± 5.4) G2 * (n = 48)—Control group (age: 53 ± 4; BMI: 28.3 ± 4.8) * both subgroups included women using hormone therapy | (a) manometry (b) questionnaire: ICIQ-UI SF | (a,b) Statistically significant improvement in subgroups not using hormone therapy. |
| Elbandrawy et al. 2022 [35] | Effect of aerobic walking exercise on stress urinary incontinence, n = 30 G1 (n = 15)—PFMT (age: 56 ± 3; BMI: 26.9 ± 1.8) G2 (n = 15)—PFMT in addition to aerobic walking exercise (age: 53 ± 4; BMI: 28.5 ± 5.4) | (a) sEMG (b) questionnaire: RUIS | (a,b) Statistically significant improvement in G2. |
| Kolodynska et al. 2022 [16] | Treatment of stress urinary incontinence, n = 60 (age: 57 ± 6; BMI: 27.07 ± 4.69): G1 (n = 20)—Sonofeedback G2 (n = 20)—ES +BF G3 (n = 20)—Control | (a) Gaudenz questionnaire (b) modified 1 h pad test | (a + b) Statistically significant improvement in G2. During laughter and coughing, there was a significant reduction in urine leakage in G1. |
| Tang et al. 2023 [36] | Treatment of stress urinary incontinence, n = 24 G1 (n = 13)—Rumba dance combined with breathing training (age: 53 ± 6; BMI: 23.8 ± 2.9) G2 (n = 11)—Control group (age: 57 ± 5; BMI: 23.3 ± 2.9) | (a) 1 h pad test (b) VRP (c) questionnaire: ICIQ-UI SF; QoL | (a–c) Statistically significant improvement in G1. |
| Gonzaga et al. 2024 [37] | Treatment of stress urinary incontinence, n = 40 G1 (n = 20)—PFMT G2 (n = 20)—Pilates | (a) 1 h pad test (b) manometry (c) questionnaire: ICIQ-UI SF | (a,c) Statistically significant improvement in both groups. (b) Peak strength manometry was significantly improved only in the Pilates group, and the mean strength manometry in both groups. |
| Elgayar, 2024 [17] | Improving the function of the PFM, n = 43 G1 (n = 22)—HIFEMT + PFMT (age: 50 ± 5; BMI: 26.3 ± 2.9) G2 (n = 21)—Control (Only PFMT) (age: 51 ± 4; BMI: 25.3 ± 2.8) | (a) perineometer (b) questionnaire: MENQOL | (a,b) Statistically significant improvement in both groups. Significantly greater changes were noted in G1. |
| Author, Year | Type (Description of Exercise) Contraction/Rest (s.) | Intensity of PFM Contraction | Frequency (n Times per Week) | Duration/Time of a Single Session (Minutes/Repetitions) | Duration of Entire Program (Number of Weeks/Sessions) |
|---|---|---|---|---|---|
| Pereira et al. 2012 [28] 2013 [27] | 3 s./6 s. 5-10 s./10–20 s. | maximum contraction | 2 | 40′ 100 repetitions | 6 weeks (12 sessions) |
| Betschart et al. 2013 [38] | - | - | on average once every two weeks | 30–45′ | 3 months (5–9 sessions) |
| Alves et al. 2015 [29] | 8 s./16 s. | maximum contraction | 2 | 30′ four sets of 10 repetitions of each exercise | 6 weeks (12 sessions) |
| Botelho et al. 2015a [40] | Quick flicks; 8 s./16 s. | maximum contraction | 3 | 60′ four sets of 10 repetitions of each exercise | 10 sessions |
| Botelho et al. 2015b [39] | Video game: pelvic anteversion, retroversion, lateral tilting, and circumduction movements. | - | 2 | 30′ | 5 weeks (10 sessions) |
| Castellani et al. 2015 [31] | 5 s./5 s. 2 s./2 s. 1 s./1 s. 10 s./10 s. | - | 2 | 30′ 10 repetitions 20 repetitions 20 repetitions 5 repetitions | 24 weeks (48 sessions) |
| Tosun et al. 2015 [32] | - | - | 3 | 30′ | 12 weeks (36 sessions) |
| Martinho et al. 2016 [33] | G1—Video game: 300 s./90 s. pelvic anteversion, retroversion, lateral tilting, and circumduction movements. | - | 2 | 30′ four sets | 5 weeks (10 sessions) |
| G2: quick flicks 8 s./16 s. | four sets four sets | ||||
| Bertotto et al. 2017 [34] | 6-10 s./6–10 s. 2 s./4 s. 3-5 s./6–10 s. | maximum contraction | 2 | 20′ 10 repetitions; two sets | 4 weeks (8 sessions) |
| Antônio et al. 2018 [30] | 6 s./6 s. Quick flicks/6 s. | maximum contraction | 2—therapy 5—home | 10 repetitions | 12 weeks (84 sessions) |
| Elbandrawy et al. 2022 [35] | 6-8 s./6 s. 3-4 quick flicks/6 s. | maximum contraction | 2—therapy | 8–12 repetitions | 12 weeks (84 sessions) |
| 3–10 s. | 5—home | five sets of 10 repetitions | |||
| Kolodynska et al. 2022 [16] | 5 s./10 s. | maximum contraction G2—max. Current up to 100 mA (1 ms) | 5 | 30′ 10 sets of 10 repetitions | 2 weeks (10 sessions) |
| Tang et al. 2023 [36] | Rumba dance combined with breathing training | - | 3 | 90′: 5′ warm-up 20′ abdominal breathing exercise 60′ Rumba dance 5′ relaxation | 16 weeks (48 sessions) |
| Gonzaga et al. 2024 [37] | PFMT/Pilates | maximum contraction | 3 | - | 12 weeks (36 sessions) |
| Elgayar, 2024 [17] | Quick flicks/6 s. | maximum contraction | 2 | Three sets of 8–12 repetitions | 12 weeks (24 sessions) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piernicka, M.; Labun, J.; Szumilewicz, A. Training Interventions Used in Postmenopausal Women to Improve Pelvic Floor Muscle Function Related to Urinary Continence—A Systematic Review. J. Clin. Med. 2025, 14, 4800. https://doi.org/10.3390/jcm14134800
Piernicka M, Labun J, Szumilewicz A. Training Interventions Used in Postmenopausal Women to Improve Pelvic Floor Muscle Function Related to Urinary Continence—A Systematic Review. Journal of Clinical Medicine. 2025; 14(13):4800. https://doi.org/10.3390/jcm14134800
Chicago/Turabian StylePiernicka, Magdalena, Justyna Labun, and Anna Szumilewicz. 2025. "Training Interventions Used in Postmenopausal Women to Improve Pelvic Floor Muscle Function Related to Urinary Continence—A Systematic Review" Journal of Clinical Medicine 14, no. 13: 4800. https://doi.org/10.3390/jcm14134800
APA StylePiernicka, M., Labun, J., & Szumilewicz, A. (2025). Training Interventions Used in Postmenopausal Women to Improve Pelvic Floor Muscle Function Related to Urinary Continence—A Systematic Review. Journal of Clinical Medicine, 14(13), 4800. https://doi.org/10.3390/jcm14134800







