Abstract
Secondary mitral regurgitation (sMR) is commonly understood to be secondary to heart failure (HF), left ventricular (LV) dilation, and altered coaptation of the mitral annulus. Three forms of sMR exist: non-ischemic sMR, ischemic sMR, and atrial functional sMR. In the past, there have been limited treatment options for this condition besides medication. Recently, the management of sMR has been revolutionized by the recent advances in percutaneous transcatheter edge-to-edge repair of the mitral valve (m-TEER). However, the major trials investigating this technology have shown that appropriate patient selection is of critical importance to achieve benefit. As such, there is a renewed interest in the accurate diagnosis of sMR. Herein, we review the etiology, management, and diagnosis of sMR in the era m-TEER.
Keywords:
secondary mitral regurgitation; ventricular functional mitral regurgitation; atrial functional mitral regurgitation; transcatheter edge-to-edge repair of the mitral valve; heart failure; MitraClip; echocardiography; semiquantitative methods; quantitative methods; cardiac magnetic resonance imaging 1. Introduction
This review will focus on the etiology, management, and diagnosis of sMR. As opposed to primary MR, which is a disease of the mitral valve (MV) apparatus, sMR is considered a distinct clinical entity with a worse prognosis and is a disease of the ventricle or atria leading to left atrial dilation and enlargement of the mitral annulus [1,2,3]. Traditionally, sMR is thought to be related to deleterious cardiac chamber remodeling, which affects a structurally normal valve leading to insufficient coaptation, after which a vicious cycle ensues wherein increasing MR begets further LV dilation, and thus further MR [2,4,5].
2. Etiology of Secondary MR
2.1. Non-Ischemic Secondary MR
The three major forms of sMR are summarized in Figure 1. Underlying dilated cardiomyopathy and decreased LV closing forces can lead to distortion of the LV geometry tethering the structurally normal mitral leaflets from papillary muscle displacement, leaflet tethering, or annular dilation, which can result in inadequate leaflet coaptation, and, consequently, non-ischemic sMR [6]. Reduced closing forces from reduced contractility, electrical or mechanical dyssynchrony of papillary muscles or of intra-left ventricular conduction system may also contribute [7]. Annular dilation and loss of annular contraction are thought to be the predominant mechanism in non-ischemic sMR, which leads to a central jet of MR [8].
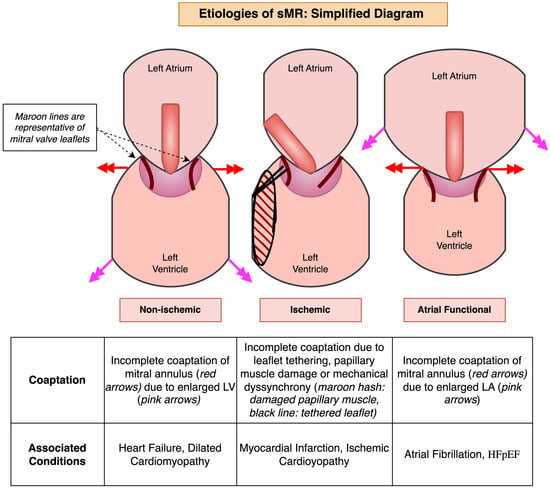
Figure 1.
A simplified diagram demonstrating the three major etiologies of secondary mitral regurgitation (sMR).
2.2. Ischemic Secondary MR
Ischemic sMR typically is secondary to chronic ischemia, resulting in post-infarction LV remodeling which has a similar mechanism as mentioned above but involves regional wall motion abnormalities and tethering of the posterior leaflet, often leading to a posteriorly directed jet of MR [4]. A central jet of MR can also be seen if there is global LV dysfunction related to multivessel ischemic disease [8]. Acute MR is rare and occurs after papillary muscle rupture or severe ischemia in the left circumflex and/or right coronary artery [9].
2.3. Atrial Functional MR
Atrial functional MR is commonly seen in patients with atrial dysfunction (from chronic atrial fibrillation or myopathy) and heart failure with a preserved ejection fraction (HFpEF) which leads to a dilated left atrium and, consequently, annular dilation and insufficient leaflets adaptation with macroscopically normal leaflets [10]. However, unlike the other mechanisms, the LV geometry and function is preserved [11,12]. Whereas leaflet motion in ischemic sMR is typically restricted, classified as Carpentier Type IIIb, leaflet motion in atrial functional MR and non-ischemic MR is typically normal, classified as Carpentier Type I [8,9,10]. An exception to this is ‘atriogenic hamstringing’, which is a form of atrial functional MR that resembles Carpentier Type IIIb leaflet motion due to posterior displacement of the mitral annulus from an enlarged LA, leading to the tethering of the posterior mitral leaflet [13,14,15]. LV ejection fraction (EF) is preserved in this form of sMR in contrast to other types of sMR.
3. Management of Secondary MR with Transcatheter Edge-to-Edge Repair (TEER) of Mitral Valve
Whereas isolated surgical intervention has been indicated for primary MR, it has not been strongly indicated for sMR [1,2,16]. Guideline-directed medical therapy (GDMT) and cardiac resynchronization therapy (CRT) are the mainstays of treatment in this population. As medical therapy is maximized and volume status and loading conditions improve, the severity of disease is likely to change. The need for intervention on MR is often evaluated only after optimizing GDMT, specifically the maximum tolerated dose of a beta-blocker and ACE inhibitor [17]. Therefore, complete imaging and assessment of MR should be performed after medical therapy is optimized, as this could change both the patient’s symptoms and technical severity of MR.
Certain cases of HF and MR are refractory to GDMT and CRT [3,7,18,19,20,21]. M-TEER is an emerging treatment for mitral regurgitation which reapproximates the A2 and P2 scallop of the MV leading to coaptation. Over the years, multiple trials with m-TEER devices have demonstrated a significant reduction in HF hospitalization [22,23,24] and cardiovascular mortality [22,23,25], as well as improvement in functional status and MR severity [24,26,27,28,29,30]. Initial trials utilized the Abbot MitraClip system [31,32], whereas more recent trials have utilized the Edwards PASCAL system [14,29,33,34]. Table 1 presents a summary of completed and ongoing trials for sMR. Endovascular Valve Edge-to-Edge Repair Study (EVERST II) included primary MR patients but is included as it was the first major randomized controlled trial (RCT) [35,36]. These trials were performed across different countries over almost two decades with a heterogeneous population with consistent findings of benefit across the spectrum of HF patients with significant sMR. Recent retrospective studies have also clarified the benefit of m-TEER in atrial functional MR [37,38,39]. The Cardiovascular Outcomes Assessment of the MitraClip Percutaneous Therapy for Heart Failure Patients with Functional Mitral Regurgitation Post Approval Study (COAPT PAS) registry is a multicenter prospective study which has included the most patients to date and has shown procedural success and efficacy of M-TEER in various sMR phenotypes [30]. There have been several RCTs which have led to a paradigm shift in sMR management with mTEER [22,23,35,40,41,42,43,44], some which have conflicting findings [45], and one which has demonstrated noninferiority and superior safety profile of m-TEER as compared to MV surgery [44]. Several other percutaneous therapies for sMR are also listed in Table 1 including transcatheter mitral loop cerclage, mitral valve replacement, and annuloplasty [46,47,48,49,50,51,52,53,54,55,56,57,58].

Table 1.
Summary of major completed and ongoing trials assessing transcatheter edge-to-edge repair for the mitral valve (m-TEER) and novel device therapy in secondary MR (sMR).
3.1. Pivotal RCTs That Transformed sMR Management with M-TEER
There have been three major RCTs that compared M-TEER and GDMT to GDMT alone in the patients with sMR. The Cardiovascular Outcomes Assessment of the MitraClip Percutaneous Therapy for Heart Failure Patients with Functional Mitral Regurgitation (COAPT) trial demonstrated that the addition of m-TEER leads to a significantly reduced HF hospitalization rate, all-cause mortality, and cardiovascular mortality at the 5-year follow-up [22,25]. The results of the COAPT trial were notably contrasted with the findings of the Percutaneous Repair with the MitraClip Device for Severe Functional/Secondary Mitral Regurgitation (MITRA-FR) trial. The MITRA-FR Trial investigated m-TEER in a similar patient population with apparent severe MR but did not show that m-TEER had a significant impact on mortality or HF hospitalizations as compared to GDMT alone [42]. Six years later, the Randomized Study of the MitraClip Device in Heart Failure Patients With Clinically Significant Functional Mitral Regurgitation (RESHAPE-HF2) trial showed that, at 2-year follow-up, m-TEER was associated with reduced hospitalization, increased quality of life, but no difference in mortality [43]. Interestingly, these three RCTs studied patients with similar pathology but the results of COAPT and RESHAPE-HF2 indicated remarkable efficacy and safety of m-TEER whereas MITRA-FR did not even show symptomatic or functional improvement [45,59]. It is also notable that COAPT demonstrated cardiovascular mortality and HF hospitalization benefit with M-TEER, whereas RESHAPE-HF2 only found HF hospitalization benefit [22,42,43,60]. Recently, a study level meta-analysis of these three RCTs was showed lower HF hospitalizations and improved functional capacity, but it did not show improvement in all-cause or cardiovascular mortality [61].
There are two other relevant RCTs that are important to mention. The Transcatheter Mitral Valve Repair in non-Responders to Cardiac Resynchronization Therapy (MITRA CRT) was a smaller RCT that investigated response to M-TEER in patients with dilated cardiomyopathy who were ‘nonresponders’ to GDMT and CRT (mean effective regurgitant orifice area [EROA] 54 ± 46 mm2). Despite the larger EROA, M-TEER was associated with a lower composite endpoint of cardiovascular death, heart transplantation, and HF hospitalization than the control group at 12 months (13% vs. 57%, respectively, p value 0.003) [23]. Lastly, The Multicenter Mitral Valve Reconstruction for Advanced Insufficiency of Functional or Ischemic Origin (MATTERHORN) trial expanded on the work of the above RCTs in that it compared m-TEER to surgical MV replacement in a study population with less advanced cardiomyopathy (EROA 20 ± 10 mm2, LV end diastolic volume [EDV] 164.6 ± 57.3 mL) [44,62]. MATTERHORN advanced the role of m-TEER as it was found to be noninferior in regard to efficacy and significantly safer than MV surgery at 1 year.
3.2. Conceptualizing the Diverging Results of MITRA-FR with the Other Trials
The trial design, baseline characteristics, and outcomes of the RCTs mentioned above are listed in Table 2. As far as inclusion criteria, all three trials included moderate to severe MR but COAPT and RESHAPE-HF2 used guidelines that defined it at a lower threshold as compared to MITRA-FR [63,64,65]. Moreover, COAPT specifically excluded patients with non-ambulatory New York Heart Association Stage IV and LVESD > 70 mm in contrast to MITRA-FR and RESHAPE-HF2 [45,59,65,66,67,68]. Importantly, GDMT optimization was more rigorously performed pre-trial in COAPT and RESHAPE-HF2 as compared to MITRA-FR which utilized a more ‘real world’ approach to GDMT adjustment [65,67]. RESHAPE-HF2 had a higher proportion of patients on quadruple medical therapy, especially with ARNI, MRA, and SGLT-2 inhibitors, albeit SGLT-2 Inhibitor utilization was low [24,62]. Because of these reasons, it is widely thought that MITRA-FR’s study population had comparatively more advanced cardiomyopathy and worse medical optimization [24,68].

Table 2.
Comparison of major randomized control trials (RCTs) for transcatheter edge-to-edge repair for the mitral valve (m-TEER) with information regarding inclusion/exclusion criteria, clinical characteristics, and outcomes. EROA: effective regurgitant orifice area, RVol: regurgitant volume, NYHA: New York Heart Association, ACEI: angiotensin-converting enzyme inhibitor, ARB: angiotensin II receptor blocker, ARNI: angiotensin receptor/neprilysin inhibitor, MRA: mineralocorticoid receptor antagonist, SGLT-2: sodium glucose transport 2, ICD: implanted cardioverter-defibrillator, CRT: cardiac resynchronization therapy, PCI: percutaneous coronary intervention, CABG: coronary artery bypass grafting, eGFR: estimated glomerular filtration rate, KCCQ: Kansas City Cardiomyopathy Questionnaire.
In addition to the reasons above, the discordant results of MITRA-FR with the other abovementioned RCTs have been further conceptualized utilizing proportionate versus disproportionate hypothesis of sMR. This theory posits that sMR that is disproportionate to LV size or indirectly to the existing cardiomyopathy (lower EROA to LV EDV ratio) and is thought to be more amenable to MV intervention, whereas sMR proportionate to LV dilation (higher EROA to LV EDV ratio) is thought to be more amenable with pharmacologic therapy (Figure 2) [69]. The inclusion of patients with higher EROA and lower LV size in COAPT is hypothesized to represent disproportionate sMR caused by valvular dysfunction, as opposed to advanced LV disease and dysfunction, which is readily correctable by m-TEER. In contrast, MITRA-FR’s lower EROA and higher LV size is thought to represent proportionate sMR which is less likely to benefit m-TEER and probably more amenable to pharmacologic therapy, with the trial’s lack of response to M-TEER further supporting the theory (Figure 3) [70]. However, RESHAPE-HF2 study population demonstrated the lowest mean EROA value, but still benefited from m-TEER. Taken together, the results of the three respective RCTs are in part explained by the severity of their underlying cardiomyopathy, with the RESHAPE-HF2 study population being early stage deriving some benefit, the MITRA-FR study population being late stage deriving little to no benefit, and the COAPT study population being in the ‘sweet spot,’ deriving the most benefit [14,71].
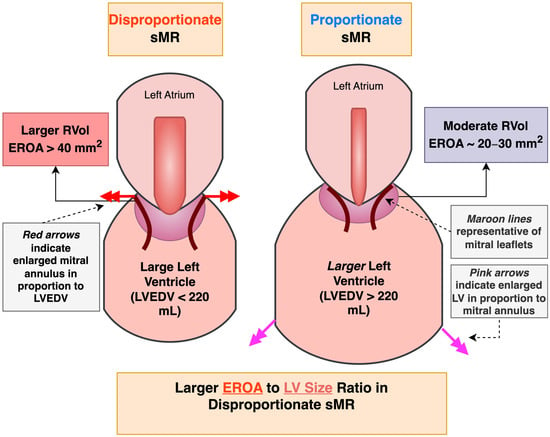
Figure 2.
A simplified diagram demonstrating depicting proportionate versus disproportionate secondary mitral regurgitation (sMR). RVol—regurgitant volume, EROA—effective regurgitant orifice area, LVEDV—left ventricular end diastolic volume.
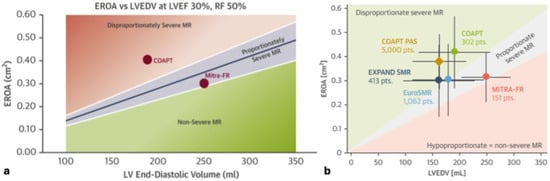
Figure 3.
[Reprinted with permission of Grayburn et al. 2019 [69] and Stolz et al. 2025 [31]]. (a) shows the graph that was initially proposed by Grayburn et al. to illustrate the proportionate versus disproportionate theory for secondary MR. (b) includes the major RCTs and real-world registries, charted according to their EROA/LVEDV ratio representing the hypothetical proportionality. EROA: effective regurgitant orifice area, LVEDV: left ventricular end diastolic volume.
Although the proportionate versus disproportionate sMR theory is widely cited as an explanation for the above differences, retrospective studies have mixed support. The findings of retrospective analysis of the EuroSMR registry appeared to support this hypothesis as it stratified patients by EROA/LVEDV ratio into MR dominant (correlating with disproportionate sMR), MR-LV co-dominant, and LV dominant groups (correlating with proportionate sMR), and found increased mortality after m-TEER noted in the LV dominant group [72]. Similarly, a sub-study of the COAPT which showed that patients that resembled a MITRA-FR ‘proportionate’ sMR phenotype with EROA < 30 mm2 and LVEDVI > 96 mL/mm2 did not derive any additional benefit with m-TEER after GDMT [66,73]. However, the reciprocal situation was studied in patients with a COAPT-like ‘disproportionate’ sMR phenotype (ERO/LVEDV ratio > 0.15) in a post hoc analysis of MITRA-FR, along with numerous other echocardiographic subsets, none of which found any benefit with M-TEER [74]. Moreover, a recent metanalysis of proportional versus disproportional MR showed that there was no association of MR proportionality (EROA:LVEDV) to all-cause mortality or HF hospitalizations [75]. Alternative parameters that may have contributed to the findings of the above RCTs that have not yet been analyzed include RV function, LV fibrosis, and LV contractile reserve [75,76].
3.3. Guideline Recommendations Regarding sMR Severity and M-TEER Candidacy
MV intervention, whether surgical or percutaneous is typically offered when sMR is severe. Prior guidelines defined sMR severity with a lower cutoff, EROA ≥ 20 mm2 or regurgitant volume (RVol) as ≥ 30 mL, since MR severity can be underestimated in the presence of an elliptical orifice and in the setting of low stroke volume [77,78,79]. Although EROA ≥ 20 mm2 has been associated with increased mortality in sMR, this finding may be attributed to multi-morbid conditions and LV dysfunction. Surgical intervention in patients with moderate ischemic MR (EROA 0.20–39 mm2) was not associated with improved outcome, but rather had increased hazard of neurologic events and supraventricular arrhythmias [80,81]. Similarly, MITRA-FR showed no benefit for m-TEER in patients with a lower EROA. For these reasons, the lower cutoff for severe MR was thought to expose patients to unnecessary risk [81]. Accordingly, the most recent ACC/ASE, ACC/AHA and ESC/EACTS Guidelines define severe sMR as an EROA ≥ 40 mm2, RVol ≥ 60 mL, or regurgitant fraction (RF) ≥ 50% [2,81,82]. In the presence of an elliptical orifice, the ACC/ASE guidelines define severity by EROA ≥ 30 mm2 or RVol as ≥ 45 mL, or RF ≥ 40% [81]. The ESC/EACTS similarly defines severity by EROA ≥ 30 mm2 in the presence of elliptical orifice and, in low flow conditions, defines RVol as ≥ 45 mL [82]. The most recent ACC/AHA guidelines listed m-TEER as a Class 2a recommendation for severe sMR (defined as above) if HF symptoms persist despite GDMT initiation and supervision by a HF specialist [2]. Furthermore, candidacy for m-TEER was limited to patients with suitable mitral anatomy, LVEF < 50%, LVESD ≤ 70 mm, and pulmonary artery systolic pressure (PASP) ≤ 70 mm Hg, which more closely resembles the criteria utilized by the COAPT trial. The most recent ESC/EACTS similarly designated m-TEER as a Class 2a recommendation [82]. Importantly, these guideline-based eligibility criteria do not reflect the findings of RESHAPE-HF2 or MATTERHORN, both of which represent benefit of m-TEER in less severe MR (compared to prior studies, both studies had lower mean EROA and MATTERHORN had a higher mean EF) [14,31].
4. Diagnostic Challenges of Heart Failure and Secondary Mitral Regurgitation in the Era of Transcatheter Edge-to-Edge Repair of the Mitral Valve
The advent of m-TEER has fueled interest in properly defining severity of sMR as patient selection is key to achieving clinical benefit with this technology [79]. Diagnosing sMR is more of a challenge than primary MR as the structural remodeling in HF patients with sMR may be related to advanced cardiomyopathy rather than the MR itself, with significant contributions from LA/LV changes, advanced cardiomyopathy, and scar tissue [13,83]. Additionally, the LV is often dilated but hyperdynamic in primary MR leading to higher RVol which can fulfill the guideline-defined cutoffs for severity whereas the LV EF is lower in sMR with lower overall stroke volumes making it less likely for RVol to reach severity cutoffs [84]. Lastly, sMR is more dynamic than primary MR and may vary based on volume status, blood pressure, and the presence of vasoactive agents, complicating MR assessment [80,81]. Ultimately, a dedicated protocol for identifying patient with significant sMR diagnosis is essential.
4.1. Defining Secondary MR
Currently, three guidelines exist to aid in diagnosing sMR in MR including those from the ACC/ASE, ACC/AHA, and ESC/EACTs, and all recommend an integrative approach with utilizes both semiquantitative and quantitate methods [2,81,82]. Transthoracic echocardiography (TTE) is the first-line imaging modality due to its convenience [85]. Several qualitative and semiquantitative methods for quantifying MR have been delineated by the ASE and are reproduced in Figure 4a [81]. These include color flow Doppler, continuous wave Doppler (CWD), LA/LV volume and size, proximal isovelocity surface area (PISA), mitral inflow velocity, and vena contracta width (VCW). If these parameters are unanimously unremarkable then mild MR can be diagnosed, and vice versa. If only some of these parameters are present, quantitative methods can be utilized and/or further imaging with transesophageal echocardiography and cardiac MRI (CMR) can be pursued.
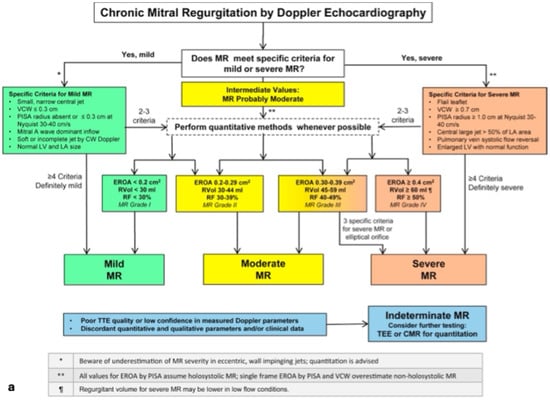
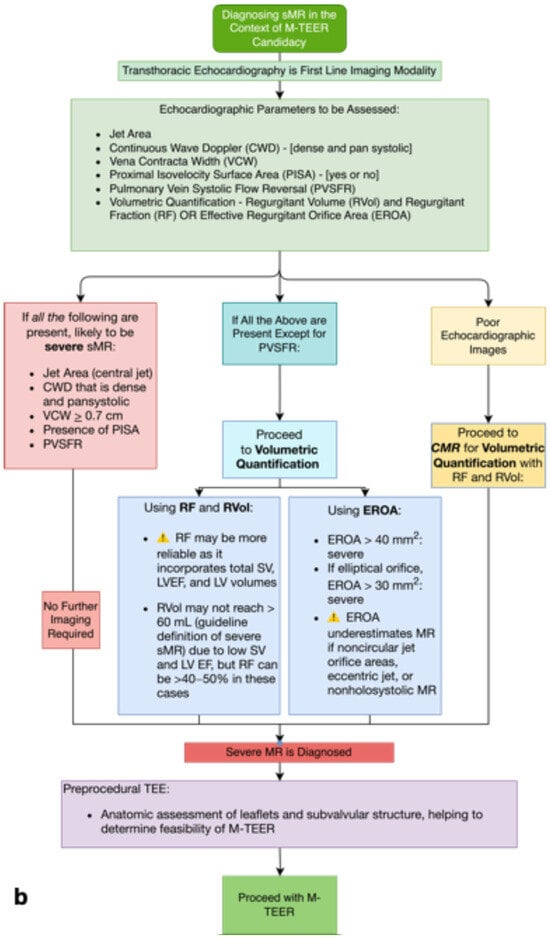
Figure 4.
[Reprinted with permission from Zoghbi et al. 2017 [81]]—(a) is the 2017 ASE diagnostic algorithm for assessing MR severity presented side by side with (b) which is our proposed algorithm for diagnosing sMR in the context of m-TEER candidacy.
Despite the utility of the ASE algorithm (Figure 4a), we believe it may not be applicable to sMR as several of the qualitative and semiquantitative variables are affected by HF, independent of MR. We propose an algorithm specific to diagnosing sMR in Figure 4b. In our opinion, LA/LV size and volume and mitral inflow velocity are often unreliable in HF patients due to existing volume overload and variability with loading conditions. Color flow Doppler and CWD provide helpful visual estimates for MR severity, however they both may underestimate the MR severity in the presence of an eccentric jet. CWD showing a dense and complete jet suggests significant MR [81]. VCW is a surrogate marker for regurgitant orifice size with size ≥ 0.7 cm considered severe and size ≥ 0.4 cm considered moderate, which has been associated with higher mortality [80,86]. However, the threshold of 0.7 cm may need a revision as it may be too high to achieve in patients with sMR. Pulmonary vein systolic flow reversal (PVSFR) can be a very specific marker of significant sMR as it is recommended by ESC/EACTS [82]; however, a recent retrospective analysis of the COAPT trial found that presence of PVSFR was not an independent predictor of 2-year prognosis after m-TEER [87]. The presence or absence of PISA is also useful. Recently, RV dysfunction and RV-PA uncoupling have been associated with worse prognosis following M-TEER [88,89,90]. We feel that PVSFR and CWD (showing a dense, triangular, contoured wave) have the most utility in identifying sMR that is greater than mild in severity, assuming the regurgitant jet is not eccentric. If all the aforementioned parameters are present, this is sufficient for a diagnosis of severe sMR.
If all are absent except PVSFR or if there is ambiguity, we recommend further assessment with quantitative volumetric methods utilizing volume tracing or pulsed Doppler to measure RVol and RF or PISA-derived EROA calculation (Figure 4b). Importantly, volume tracing and pulsed Doppler rely on the continuity principle and are valid in the case of multiple or eccentric jets (in contrast to PISA-derived EROA) but are limited by nonlaminar flow, improper placement of sample volume, or atrial fibrillation which is common in HF [91].
Notably, the PISA-derived EROA method is the most commonly used approach for calculating sMR as it has been validated against LV angiography, has been shown to be prognostically meaningful after ischemic MR and can predict treatment response to m-TEER [22,42,92,93,94]. Accordingly, we feel that EROA ≥ 30 mm2 predicts a higher likelihood of response to therapy [22,42,43]. Importantly, a retrospective study of 177 patients with both ischemic and non-ischemic sMR showed superiority of the quantitative volumetric method over the PISA method in predicting mortality or heart transplant at a mean follow up of 3.7 years [95]. These findings may be attributed to the fact that the PISA method underestimates MR severity in the presence of noncircular jet orifice areas, eccentric jets, or nonholosystolic MR [80,85,96], or to its significant interobserver variability [80,81,97]. For these reasons, we prefer volume-tracing-derived RVol and RF for quantitation and utilize contrast to prevent underestimation of LV volumes or foreshortening of the LV apex [98]. Notably, calculation of both RVol and RF values is prudent as RVol ≥ 60 mL may not be observed due to underlying cardiomyopathy and low stroke volumes in sMR whereas RF may reach 40–50% [84]. Essentially, the RF differentiates between disproportionate versus proportionate MR as it is a reflection of RVol over total LV volumes. To this point, an observational study showed that outcomes of patients with intermediate severity sMR (EROA 20–29 mm2 and RVol as 30–44 mL) and RF ≥ 50% have been noticeably worse outcomes as compared to those with RF < 50% [79]. Some studies describe the incorporation of chest wall shape assessment using the modified Haller Index (MHI) to assess cardiovascular risk in patients with MR [99]. Given the simplicity of the MHI, it would be beneficial for future studies to explore its use in evaluating patients with sMR. For patients with multivalvular disease, intervention on a single valve will likely decrease the severity of disease on other valves. This has been demonstrated in sMR patients with concomitant aortic stenosis in multiple studies. Some have demonstrated the greatest improvement in sMR when there is not patient–prosthesis mismatch of the AVR [100,101,102]. This data suggests intervention on a diseased aortic valve should be performed prior to or in conjunction with intervention on a diseased mitral valve.
Overall, since accurate assessment of sMR informs candidacy for m-TEER and other MV interventions, a multiparametric, integrative approach should be utilized [103]. If 2-dimensional (2D) echocardiographic images are poor or nondiagnostic, we prefer CMR in these cases to accurately quantitate the MR. Transesophageal echocardiography (TEE) may offer higher resolution, but it is more commonly used for preprocedural and intraprocedural purposes as it provides detailed views of the MV apparatus [81].
Three-dimensional (3D) echocardiography may improve accuracy as compared to 2D as it can better quantify EROA and the vena contracta area. Three-dimensional echocardiography quantification of eccentric jets and complex MR make this imaging modality superior to 2D, which relies on geometric assumptions that commonly underestimate MR severity [94,104,105]. Three-dimensional imaging more frequently aligns with cardiac MR findings further proving its superiority to 2D echocardiography, but is ultimately limited by imaging complexity and expertise [106].
4.2. Emerging Role of Cardiac Magnetic Resonance Imaging
CMR is increasingly regarded as the gold standard for morphologic, volumetric, flow, and viability assessment and has been shown to have increased accuracy than 2D volumetric methods [97,107,108]. The two main techniques for MR quantification using CMR are the volumetric method and the phase-contrast method as shown in Figure 5 [109,110]. It has been demonstrated that EROA ≥ 40 mm2 on echocardiography was unable to predict indication for MV surgery as compared to CMR quantified RVol > 55mL in patients with moderate to severe primary MR [111]. As compared to echocardiographic parameters, RVol quantified by CMR is associated with prognostic significance regarding mortality, indication for MV surgery, and LV reverse remodeling after MV repair [107,108,109,110,111,112,113]. CMR also accurately and reliably quantifies LA volume and function and aids in identifying the etiology of cardiomyopathy and MR [97,108,109,114]. Furthermore, CMR plays a significant role in the assessment of myocardial scar and papillary muscle infarct, which carry prognostic information [110,115,116,117,118]. The presence of scars in both ischemic cardiomyopathy (ICM) and non-ischemic cardiomyopathy (NICM) significantly worsened outcomes in patients with sMR and RF ≥ 30% as compared to < 30% [106]. An observational study associated significantly worse outcome in patients with ICM with RF ≥ 35% and late gadolinium enhancement ≥ 5%, and in patients with NICM with RF ≥ 35% and late gadolinium enhancement ≥ 2%. All subgroups of ICM were found to have worsened outcomes as compared to NICM [116]. Lastly, MR severity on CMR has been defined as RVol ≥ 60 mL and RF ≥ 50% but the severity thresholds are not well established and may need revision [8,81,119].
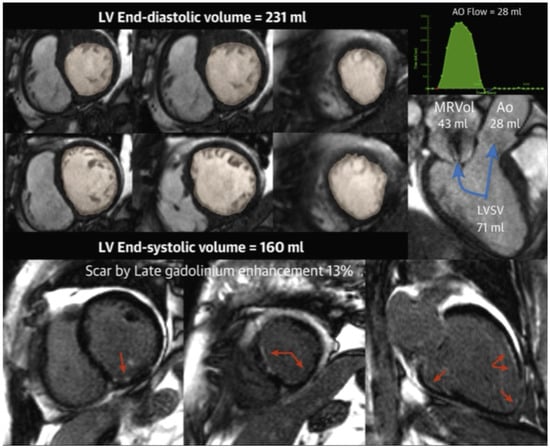
Figure 5.
[Reprinted with permission from Tayal et al. 2020 [110]]: This example case outlines how cardiac magnetic resonance (CMR) can be used to quantitate secondary mitral regurgitation and scar. (Top) Left ventricular and total stroke volume (SV) quantification. (Top right) Phase contrast images are used to calculate the forward SV quantification. (Bottom) Late gadolinium enhancement was used to quantitate. This patient in this example was a 69-year-old woman with ischemic cardiomyopathy and secondary MR with RVol = 43 mL and RF = 52%. Scar burden = 13%. The patient expired 0.27 months after CMR. Blue arrows point towards the numeric values, which represent volumes quantitation. Red arrows represent scar tissue. Ao = aorta; LVSV = left ventricular stroke volume; MRVol = mitral regurgitant volume.
4.3. Future Role of Artificial Intelligence
Machine learning has been utilized to integrate numerous clinical and imaging variables into distinct sMR phenotypes in order to prognosticate and predict treatment response [83,120]. In a cohort of HFrEF sMR patients on GDMT (n = 382), 32 morphologic and functional parameters of LV, LA, and RV were subjected to unsupervised machine learning principal component analysis, revealing four clusters of sMR patients [83]. The authors suggested that cluster 3 and 4 correlated with disproportionate and proportionate sMR, providing support to this theory [83]. The MITRA-AI study similarly utilized machine learning in a group of patients who underwent m-TEER (n = 822) and identified four clusters which each had differing mortality and hospitalization rates following m-TEER [121]. Lastly, the European Registry of Transcatheter Repair of Secondary Mitral Regurgitation (EuroSMR) registry has developed an artificial-intelligence-based risk score that utilizes 18 clinical, echocardiographic, laboratory, and medication parameters to predict a 1-year outcome following m-TEER that has outperformed existing scores [122]. In summary, artificial intelligence is allowing for a deeper understanding of m-TEER phenotypes, thereby improving risk stratification and patient selection.
5. Conclusions
In the past decade, there has been a significant advancement in the management of sMR with the advent of m-TEER. An accurate grading of sMR is of critical importance for the consideration of these novel percutaneous interventions. However, it is challenging to accurately quantify sMR and it may be underestimated in the presence of low flow status due to HF. Standard echocardiographic guidelines to quantify MR is widely available but may have to be tailored to apply them in the setting of HF. CMR can be a very useful tool in selected cases where sMR is ambiguous. Moreover, CMR adds prognostic information in patients with sMR, including etiologic, morphologic, volumetric, and viability assessment. Referral to high-volume centers is advisable when sMR presentation and quantification are equivocal, as these institutions possess specialized expertise in navigating the subtle complexities inherent in the diagnosis and management of this condition.
Author Contributions
Conceptualization, Y.B.S. and B.T.; writing—original draft preparation, Y.B.S. and B.T.; writing—review and editing, Y.B.S., K.D., A.H. and B.T.; visualization, Y.B.S. and B.T.; supervision, B.T.; project administration, B.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| MR | Mitral regurgitation |
| MV | Mitral valve |
| sMR | Secondary mitral regurgitation |
| HF | Heart failure |
| GDMT | Guideline-directed medical therapy |
| CRT | Cardiac resynchronization therapy |
| m-TEER | Transcatheter edge-to-edge repair of the mitral valve |
| RCT | Randomized control trial |
| EROA | Effective regurgitant orifice area |
| LVEDV | Left ventricular end diastolic volume |
| ARNI | Angiotensin receptor/neprilysin inhibitor |
| MRA | Mineralocorticoid receptor antagonist |
| SGLT-2 | Sodium glucose transporter—2 |
| RVol | Regurgitant volume |
| ACC/ASE | American College of Cardiology/American Society of Echocardiography |
| ACC/AHA | American College of Cardiology/American Heart Association |
| ESC/EACTS | European Society of Cardiology/European Association for Cardio-Thoracic Surgery |
| EACVI | European Association of Cardiovascular Imaging |
| RF | Regurgitant fraction |
| TTE | Transthoracic echocardiography |
| CMR | Cardiac magnetic resonance imaging |
References
- Nishimura, R.A.; Otto, C.M.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P.; Fleisher, L.A.; Jneid, H.; Mack, M.J.; McLeod, C.J.; O’Gara, P.T.; et al. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2017, 70, 252–289. [Google Scholar] [CrossRef] [PubMed]
- Otto, C.M.; Nishimura, R.A.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P., 3rd; Gentile, F.; Jneid, H.; Krieger, E.V.; Mack, M.; McLeod, C.; et al. 2020 ACC/AHA Guideline for the Management of Patients with Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Thorac. Cardiovasc. Surg. 2021, 162, e183–e353. [Google Scholar] [CrossRef]
- Bartko, P.E.; Pavo, N.; Pérez-Serradilla, A.; Arfsten, H.; Neuhold, S.; Wurm, R.; Lang, I.M.; Strunk, G.; Dal-Bianco, J.P.; Levine, R.A.; et al. Evolution of Secondary Mitral Regurgitation. Eur. Heart J. Cardiovasc. Imaging 2018, 19, 622–629. [Google Scholar] [CrossRef] [PubMed]
- Piérard, L.A.; Carabello, B.A. Ischaemic Mitral Regurgitation: Pathophysiology, Outcomes and the Conundrum of Treatment. Eur. Heart J. 2010, 31, 2996–3005. [Google Scholar] [CrossRef]
- Russo, E.; Russo, G.; Cassese, M.; Braccio, M.; Carella, M.; Compagnucci, P.; Dello Russo, A.; Casella, M. The Role of Cardiac Resynchronization Therapy for the Management of Functional Mitral Regurgitation. Cells 2022, 11, 2407. [Google Scholar] [CrossRef]
- Hausleiter, J.; Stocker, T.J.; Adamo, M.; Karam, N.; Swaans, M.J.; Praz, F. Mitral Valve Transcatheter Edge-to-Edge Repair. EuroIntervention 2023, 18, 957–976. [Google Scholar] [CrossRef] [PubMed]
- Packer, M. Disproportionate Functional Mitral Regurgitation: A New Therapeutic Target in Patients with Heart Failure and a Reduced Ejection Fraction. Eur. J. Heart Fail. 2020, 22, 23–25. [Google Scholar] [CrossRef]
- El Sabbagh, A.; Reddy, Y.N.; Nishimura, R.A. Mitral Valve Regurgitation in the Contemporary Era: Insights Into Diagnosis, Management, and Future Directions. JACC Cardiovasc. Imaging 2018, 11, 628–643. [Google Scholar] [CrossRef]
- Varma, P.K.; Krishna, N.; Jose, R.L.; Madkaiker, A.N. Ischemic Mitral Regurgitation. Ann. Card. Anaesth. 2017, 20, 432–439. [Google Scholar] [CrossRef]
- Zoghbi, W.A.; Levine, R.A.; Flachskampf, F.; Grayburn, P.; Gillam, L.; Leipsic, J.; Thomas, J.D.; Kwong, R.Y.; Vandervoort, P.; Chandrashekhar, Y. Atrial Functional Mitral Regurgitation: A JACC: Cardiovascular Imaging Expert Panel Viewpoint. JACC Cardiovasc. Imaging 2022, 15, 1870–1882. [Google Scholar] [CrossRef]
- Hirji, S.A.; Cote, C.L.; Javadikasgari, H.; Malarczyk, A.; McGurk, S.; Kaneko, T. Atrial Functional versus Ventricular Functional Mitral Regurgitation: Prognostic Implications. J. Thorac. Cardiovasc. Surg. 2022, 164, 1808–1815.e4. [Google Scholar] [CrossRef] [PubMed]
- Bove, T. Commentary: Functional Mitral Regurgitation: The 2 Sides of 1 Coin. J. Thorac. Cardiovasc. Surg. 2022, 164, 1816–1817. [Google Scholar] [CrossRef] [PubMed]
- Stolz, L.; Doldi, P.M.; Sannino, A.; Hausleiter, J.; Grayburn, P.A. The Evolving Concept of Secondary Mitral Regurgitation Phenotypes: Lessons From the M-TEER Trials. JACC Cardiovasc. Imaging 2024, 17, 659–668. [Google Scholar] [CrossRef]
- von Stein, P.; Iliadis, C. Transcatheter Edge-to-Edge Repair for Mitral Regurgitation. Trends Cardiovasc. Med. 2025, 35, 320–325. [Google Scholar] [CrossRef] [PubMed]
- von Stein, P.; von Stein, J.; Hohmann, C.; Wienemann, H.; Guthoff, H.; Körber, M.I.; Baldus, S.; Pfister, R.; Hahn, R.T.; Iliadis, C. Atrial Functional Mitral Regurgitation Subtypes Undergoing Transcatheter Edge-to-Edge Repair: Suboptimal Outcomes in Atriogenic Hamstringing. JACC Cardiovasc. Imaging 2025, 18, 16–29. [Google Scholar] [CrossRef]
- Goel, S.S.; Bajaj, N.; Aggarwal, B.; Gupta, S.; Poddar, K.L.; Ige, M.; Bdair, H.; Anabtawi, A.; Rahim, S.; Whitlow, P.L.; et al. Prevalence and Outcomes of Unoperated Patients with Severe Symptomatic Mitral Regurgitation and Heart Failure: Comprehensive Analysis to Determine the Potential Role of MitraClip for This Unmet Need. J. Am. Coll. Cardiol. 2014, 63, 185–186. [Google Scholar] [CrossRef]
- Enriquez-Sarano, M.; Akins, C.W.; Vahanian, A. Mitral Regurgitation. Lancet 2009, 373, 1382–1394. [Google Scholar] [CrossRef]
- de Groot-de Laat, L.E.; Huizer, J.; Lenzen, M.; Spitzer, E.; Ren, B.; Geleijnse, M.L.; Caliskan, K. Evolution of Mitral Regurgitation in Patients with Heart Failure Referred to a Tertiary Heart Failure Clinic. ESC Heart Fail. 2019, 6, 936–943. [Google Scholar] [CrossRef]
- Nasser, R.; Van Assche, L.; Vorlat, A.; Vermeulen, T.; Van Craenenbroeck, E.; Conraads, V.; Van der Meiren, V.; Shivalkar, B.; Van Herck, P.; Claeys, M.J. Evolution of Functional Mitral Regurgitation and Prognosis in Medically Managed Heart Failure Patients With Reduced Ejection Fraction. JACC Heart Fail. 2017, 5, 652–659. [Google Scholar] [CrossRef]
- Sannino, A.; Sudhakaran, S.; Milligan, G.; Chowdhury, A.; Haq, A.; Szerlip, M.; Packer, M.; Grayburn, P.A. Effectiveness of Medical Therapy for Functional Mitral Regurgitation in Heart Failure With Reduced Ejection Fraction. J. Am. Coll. Cardiol. 2020, 76, 883–884. [Google Scholar] [CrossRef]
- Adamo, M.; Tomasoni, D.; Stolz, L.; Stocker, T.J.; Pancaldi, E.; Koell, B.; Karam, N.; Besler, C.; Giannini, C.; Sampaio, F.; et al. Impact of Transcatheter Edge-to-Edge Mitral Valve Repair on Guideline-Directed Medical Therapy Uptitration. JACC Cardiovasc. Interv. 2023, 16, 896–905. [Google Scholar] [CrossRef] [PubMed]
- Stone, G.W.; Lindenfeld, J.; Abraham, W.T.; Kar, S.; Lim, D.S.; Mishell, J.M.; Whisenant, B.; Grayburn, P.A.; Rinaldi, M.; Kapadia, S.R.; et al. Transcatheter Mitral-Valve Repair in Patients with Heart Failure. N. Engl. J. Med. 2018, 379, 2307–2318. [Google Scholar] [CrossRef] [PubMed]
- Freixa, X.; Tolosana, J.M.; Cepas-Guillen, P.L.; Hernández-Enríquez, M.; Sanchis, L.; Flores-Umanzor, E.; Farrero, M.; Andrea, R.; Roqué, M.; Carretero, M.J.; et al. Edge-to-Edge Transcatheter Mitral Valve Repair Versus Optimal Medical Treatment in Nonresponders to Cardiac Resynchronization Therapy: The MITRA-CRT Trial. Circ. Heart Fail. 2022, 15, e009501. [Google Scholar] [CrossRef]
- Anker, S.D.; Friede, T.; von Bardeleben, R.S.; Butler, J.; Khan, M.S.; Diek, M.; Heinrich, J.; Geyer, M.; Placzek, M.; Ferrari, R.; et al. Percutaneous Repair of Moderate-to-Severe or Severe Functional Mitral Regurgitation in Patients with Symptomatic Heart Failure: Baseline Characteristics of Patients in the RESHAPE-HF2 Trial and Comparison to COAPT and MITRA-FR Trials. Eur. J. Heart Fail. 2024, 26, 1608–1615. [Google Scholar] [CrossRef] [PubMed]
- Stone, G.W.; Abraham, W.T.; Lindenfeld, J.; Kar, S.; Grayburn, P.A.; Lim, D.S.; Mishell, J.M.; Whisenant, B.; Rinaldi, M.; Kapadia, S.R.; et al. Five-Year Follow-up after Transcatheter Repair of Secondary Mitral Regurgitation. N. Engl. J. Med. 2023, 388, 2037–2048. [Google Scholar] [CrossRef]
- Kalbacher, D.; Schäfer, U.; Bardeleben, R.S.V.; Eggebrecht, H.; Sievert, H.; Nickenig, G.; Butter, C.; May, A.E.; Bekeredjian, R.; Ouarrak, T.; et al. Long-Term Outcome, Survival and Predictors of Mortality after MitraClip Therapy: Results from the German Transcatheter Mitral Valve Interventions (TRAMI) Registry. Int. J. Cardiol. 2019, 277, 35–41. [Google Scholar] [CrossRef]
- Kar, S.; von Bardeleben, R.S.; Rottbauer, W.; Mahoney, P.; Price, M.J.; Grasso, C.; Williams, M.; Lurz, P.; Ahmed, M.; Hausleiter, J.; et al. Contemporary Outcomes Following Transcatheter Edge-to-Edge Repair: 1-Year Results From the EXPAND Study. JACC Cardiovasc. Interv. 2023, 16, 589–602. [Google Scholar] [CrossRef]
- von Bardeleben, R.S.; Mahoney, P.; Morse, M.A.; Price, M.J.; Denti, P.; Maisano, F.; Rogers, J.H.; Rinaldi, M.; De Marco, F.; Rollefson, W.; et al. 1-Year Outcomes With Fourth-Generation Mitral Valve Transcatheter Edge-to-Edge Repair From the EXPAND G4 Study. JACC Cardiovasc. Interv. 2023, 16, 2600–2610. [Google Scholar] [CrossRef]
- Lurz, P.; Schmitz, T.; Geisler, T.; Hausleiter, J.; Eitel, I.; Rudolph, V.; Lubos, E.; von Bardeleben, R.S.; Brambilla, N.; De Marco, F.; et al. Mitral Valve Transcatheter Edge-to-Edge Repair: 1-Year Outcomes From the MiCLASP Study. JACC Cardiovasc. Interv. 2024, 17, 890–903. [Google Scholar] [CrossRef] [PubMed]
- Goel, K.; Lindenfeld, J.; Makkar, R.; Naik, H.; Atmakuri, S.; Mahoney, P.; Morse, M.A.; Thourani, V.H.; Yadav, P.; Batchelor, W.; et al. Transcatheter Edge-to-Edge Repair in 5,000 Patients With Secondary Mitral Regurgitation: COAPT Post-Approval Study. J. Am. Coll. Cardiol. 2023, 82, 1281–1297. [Google Scholar] [CrossRef]
- Stolz, L.; Stocker, T.J.; Lurz, P.; Hausleiter, J. Growing Evidence for Edge-to-Edge Repair in Secondary Mitral Regurgitation: What to Learn From COAPT, MITRA-FR, and RESHAPE-HF2. JACC Cardiovasc. Interv. 2025, 18, 927–932. [Google Scholar] [CrossRef] [PubMed]
- Makkar, R.R.; Chikwe, J.; Chakravarty, T.; Chen, Q.; O’Gara, P.T.; Gillinov, M.; Mack, M.J.; Vekstein, A.; Patel, D.; Stebbins, A.L.; et al. Transcatheter Mitral Valve Repair for Degenerative Mitral Regurgitation. JAMA 2023, 329, 1778–1788. [Google Scholar] [CrossRef]
- Garcia, S.; Elmariah, S.; Cubeddu, R.J.; Zahr, F.; Eleid, M.F.; Kodali, S.K.; Seshiah, P.; Sharma, R.; Lim, D.S. Mitral Transcatheter Edge-to-Edge Repair with the PASCAL Precision System: Device Knobology and Review of Advanced Steering Maneuvers. Struct. Heart 2024, 8, 100234. [Google Scholar] [CrossRef] [PubMed]
- Zahr, F.; Smith, R.L.; Gillam, L.D.; Chadderdon, S.; Makkar, R.; von Bardeleben, R.S.; Ruf, T.F.; Kipperman, R.M.; Rassi, A.N.; Szerlip, M.; et al. One-Year Outcomes From the CLASP IID Randomized Trial for Degenerative Mitral Regurgitation. JACC Cardiovasc. Interv. 2023, 16, 2803–2816. [Google Scholar] [CrossRef] [PubMed]
- Feldman, T.; Kar, S.; Elmariah, S.; Smart, S.C.; Trento, A.; Siegel, R.J.; Apruzzese, P.; Fail, P.; Rinaldi, M.J.; Smalling, R.W.; et al. Randomized Comparison of Percutaneous Repair and Surgery for Mitral Regurgitation: 5-Year Results of EVEREST II. J. Am. Coll. Cardiol. 2015, 66, 2844–2854. [Google Scholar] [CrossRef]
- Feldman, T.; Foster, E.; Glower, D.D.; Kar, S.; Rinaldi, M.J.; Fail, P.S.; Smalling, R.W.; Siegel, R.; Rose, G.A.; Engeron, E.; et al. Percutaneous Repair or Surgery for Mitral Regurgitation. N. Engl. J. Med. 2011, 364, 1395–1406. [Google Scholar] [CrossRef]
- Doldi, P.; Stolz, L.; Orban, M.; Karam, N.; Praz, F.; Kalbacher, D.; Lubos, E.; Braun, D.; Adamo, M.; Giannini, C.; et al. Transcatheter Mitral Valve Repair in Patients With Atrial Functional Mitral Regurgitation. JACC Cardiovasc. Imaging 2022, 15, 1843–1851. [Google Scholar] [CrossRef]
- Yoshida, J.; Ikenaga, H.; Nagaura, T.; Utsunomiya, H.; Kawai, M.; Makar, M.; Rader, F.; Siegel, R.J.; Kar, S.; Makkar, R.R.; et al. Impact of Percutaneous Edge-to-Edge Repair in Patients With Atrial Functional Mitral Regurgitation. Circ. J. 2021, 85, 1001–1010. [Google Scholar] [CrossRef]
- Rudolph, F.; Geyer, M.; Baldus, S.; De Luca, V.M.; Doenst, T.; Pfister, R.; Gummert, J.; Kessler, M.; Boekstegers, P.; Lubos, E.; et al. Transcatheter Repair Versus Surgery for Atrial Versus Ventricular Functional Mitral Regurgitation: A Post Hoc Analysis of the MATTERHORN Trial. Circulation 2025, 151, 418–420. [Google Scholar] [CrossRef]
- Mauri, L.; Garg, P.; Massaro, J.M.; Foster, E.; Glower, D.; Mehoudar, P.; Powell, F.; Komtebedde, J.; McDermott, E.; Feldman, T. The EVEREST II Trial: Design and Rationale for a Randomized Study of the Evalve Mitraclip System Compared with Mitral Valve Surgery for Mitral Regurgitation. Am. Heart J. 2010, 160, 23–29. [Google Scholar] [CrossRef]
- Feldman, T.; Fernandes, E.; Levisay, J.P. Transcatheter Mitral Valve Repair/Replacement for Primary Mitral Regurgitation. Ann. Cardiothorac. Surg. 2018, 7, 755–763. [Google Scholar] [CrossRef] [PubMed]
- Jean-François, O.; David, M.-Z.; Guillaume, L.; Bernard, I.; Guillaume, B.; Nicolas, P.; Thierry, L.; Christophe, P.; Frédéric, R.; Didier, C.; et al. Percutaneous Repair or Medical Treatment for Secondary Mitral Regurgitation. N. Engl. J. Med. 2018, 379, 2297–2306. [Google Scholar] [CrossRef]
- Anker, S.D.; Friede, T.; von Bardeleben, R.-S.; Butler, J.; Khan, M.-S.; Diek, M.; Heinrich, J.; Geyer, M.; Placzek, M.; Ferrari, R.; et al. Transcatheter Valve Repair in Heart Failure with Moderate to Severe Mitral Regurgitation. N. Engl. J. Med. 2024, 391, 1799–1809. [Google Scholar] [CrossRef] [PubMed]
- Baldus, S.; Doenst, T.; Pfister, R.; Gummert, J.; Kessler, M.; Boekstegers, P.; Lubos, E.; Schröder, J.; Thiele, H.; Walther, T.; et al. Transcatheter Repair versus Mitral-Valve Surgery for Secondary Mitral Regurgitation. N. Engl. J. Med. 2024, 391, 1787–1798. [Google Scholar] [CrossRef]
- Armoiry, X.; Obadia, J.-F.; Auguste, P.; Connock, M. Conflicting Findings between the Mitra-Fr and the Coapt Trials: Implications Regarding the Cost-Effectiveness of Percutaneous Repair for Heart Failure Patients with Severe Secondary Mitral Regurgitation. PLoS ONE 2020, 15, e0241361. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.-H.; Chon, M.-K.; Lederman, R.J.; Sung, S.-C.; Je, H.-G.; Choo, K.-S.; Lee, S.-H.; Shin, E.-S.; Kim, J.-S.; Hwang, K.-W.; et al. Mitral Loop Cerclage Annuloplasty for Secondary Mitral Regurgitation: First Human Results. JACC Cardiovasc. Interv. 2017, 10, 597–610. [Google Scholar] [CrossRef]
- Messika-Zeitoun, D.; Nickenig, G.; Latib, A.; Kuck, K.-H.; Baldus, S.; Schueler, R.; La Canna, G.; Agricola, E.; Kreidel, F.; Huntgeburth, M.; et al. Transcatheter Mitral Valve Repair for Functional Mitral Regurgitation Using the Cardioband System: 1 Year Outcomes. Eur. Heart J. 2019, 40, 466–472. [Google Scholar] [CrossRef]
- Siminiak, T.; Hoppe, U.C.; Schofer, J.; Haude, M.; Herrman, J.-P.; Vainer, J.; Firek, L.; Reuter, D.G.; Goldberg, S.L.; Van Bibber, R. Effectiveness and Safety of Percutaneous Coronary Sinus-Based Mitral Valve Repair in Patients With Dilated Cardiomyopathy (from the AMADEUS Trial). Am. J. Cardiol. 2009, 104, 565–570. [Google Scholar] [CrossRef]
- Lipiecki, J.; Siminiak, T.; Sievert, H.; Müller-Ehmsen, J.; Degen, H.; Wu, J.C.; Schandrin, C.; Kalmucki, P.; Hofmann, I.; Reuter, D.; et al. Coronary Sinus-Based Percutaneous Annuloplasty as Treatment for Functional Mitral Regurgitation: The TITAN II Trial. Open Heart 2016, 3, e000411. [Google Scholar] [CrossRef][Green Version]
- Goldberg, S.L.; Lipiecki, J.; Sievert, H. The CARILLON Mitral Contour Transcatheter Indirect Mitral Valve Annuloplasty System. EuroIntervention 2015, 11, W64–W66. [Google Scholar] [CrossRef]
- Goldberg, S.L.; Meredith, I.; Marwick, T.; Haluska, B.A.; Lipiecki, J.; Siminiak, T.; Mehta, N.; Kaye, D.M.; Sievert, H. A Randomized Double-Blind Trial of an Interventional Device Treatment of Functional Mitral Regurgitation in Patients with Symptomatic Congestive Heart Failure—Trial Design of the REDUCE FMR Study. Am. Heart J. 2017, 188, 167–174. [Google Scholar] [CrossRef] [PubMed]
- Maisano, F.; Taramasso, M. The Cardioband Transcatheter Direct Mitral Valve Annuloplasty System. EuroIntervention 2015, 11, W58–W59. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bapat, V.; Rajagopal, V.; Meduri, C.; Farivar, R.S.; Walton, A.; Duffy, S.J.; Gooley, R.; Almeida, A.; Reardon, M.J.; Kleiman, N.S.; et al. Early Experience With New Transcatheter Mitral Valve Replacement. J. Am. Coll. Cardiol. 2018, 71, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Zahr, F.; Song, H.K.; Chadderdon, S.M.; Gada, H.; Mumtaz, M.; Byrne, T.; Kirshner, M.; Bajwa, T.; Weiss, E.; Kodali, S.; et al. 30-Day Outcomes Following Transfemoral Transseptal Transcatheter Mitral Valve Replacement: Intrepid TMVR Early Feasibility Study Results. JACC Cardiovasc. Interv. 2022, 15, 80–89. [Google Scholar] [CrossRef]
- Alkhouli, M.; Guerrero, M.; Rihal, C.S. Transseptal TMVR: An Intrepid Journey. JACC Cardiovasc. Interv. 2022, 15, 90–92. [Google Scholar] [CrossRef]
- Rodés-Cabau, J. Transcatheter Mitral Valve Replacement: First Steps on a Long Road. J. Am. Coll. Cardiol. 2018, 71, 22–24. [Google Scholar] [CrossRef]
- Rogers, J.H.; Thomas, M.; Morice, M.-C.; Narbute, I.; Zabunova, M.; Hovasse, T.; Poupineau, M.; Rudzitis, A.; Kamzola, G.; Zvaigzne, L.; et al. Treatment of Heart Failure with Associated Functional Mitral Regurgitation Using the ARTO System: Initial Results of the First-in-Human MAVERIC Trial (Mitral Valve Repair Clinical Trial). JACC Cardiovasc. Interv. 2015, 8, 1095–1104. [Google Scholar] [CrossRef]
- Patterson, T.; Gregson, J.; Erglis, A.; Joseph, J.; Rajani, R.; Wilson, K.; Prendergast, B.; Worthley, S.; Hildick-Smith, D.; Rafter, T.; et al. Two-Year Outcomes from the MitrAl ValvE RepaIr Clinical (MAVERIC) Trial: A Novel Percutaneous Treatment of Functional Mitral Regurgitation. Eur. J. Heart Fail. 2021, 23, 1775–1783. [Google Scholar] [CrossRef]
- Senni, M.; Adamo, M.; Metra, M.; Alfieri, O.; Vahanian, A. Treatment of Functional Mitral Regurgitation in Chronic Heart Failure: Can We Get a ‘Proof of Concept’ from the MITRA-FR and COAPT Trials? Eur. J. Heart Fail. 2019, 21, 852–861. [Google Scholar] [CrossRef]
- Ponikowski, P.; Friede, T.; von Bardeleben, R.S.; Butler, J.; Shahzeb Khan, M.; Diek, M.; Heinrich, J.; Geyer, M.; Placzek, M.; Ferrari, R.; et al. Hospitalization of Symptomatic Patients With Heart Failure and Moderate to Severe Functional Mitral Regurgitation Treated With MitraClip: Insights from RESHAPE-HF2. J. Am. Coll. Cardiol. 2024, 84, 2347–2363. [Google Scholar] [CrossRef]
- Anker, M.S.; Porthun, J.; Bonnet, G.; Schulze, P.C.; Rassaf, T.; Landmesser, U. Percutaneous Transcatheter Edge-to-Edge Repair for Functional Mitral Regurgitation in Heart Failure: A Meta-Analysis of 3 Randomized Controlled Trials. J. Am. Coll. Cardiol. 2024, 84, 2364–2368. [Google Scholar] [CrossRef] [PubMed]
- Lancellotti, P.; Sugimoto, T.; Bäck, M. Revisiting Secondary Mitral Regurgitation Threshold Severity: Insights and Lessons from the RESHAPE-HF2 Trial. Eur. Heart J. Open 2024, 4, oeae084. [Google Scholar] [CrossRef]
- Bonow, R.O.; Carabello, B.A.; Chatterjee, K.; de Leon, A.C.; Faxon, D.P.; Freed, M.D.; Gaasch, W.H.; Lytle, B.W.; Nishimura, R.A.; O’Gara, P.T.; et al. ACC/AHA 2006 Guidelines for the Management of Patients With Valvular Heart Disease. Circulation 2006, 114, e84–e231. [Google Scholar] [CrossRef] [PubMed]
- Members, A.F.; Vahanian, A.; Alfieri, O.; Andreotti, F.; Antunes, M.J.; Barón-Esquivias, G.; Baumgartner, H.; Borger, M.A.; Carrel, T.P.; De Bonis, M.; et al. Guidelines on the Management of Valvular Heart Disease (Version 2012): The Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2012, 33, 2451–2496. [Google Scholar] [CrossRef]
- Pibarot, P.; Delgado, V.; Bax, J.J. MITRA-FR vs. COAPT: Lessons from Two Trials with Diametrically Opposed Results. Eur. Heart J. Cardiovasc. Imaging 2019, 20, 620–624. [Google Scholar] [CrossRef] [PubMed]
- Atianzar, K.; Zhang, M.; Newhart, Z.; Gafoor, S. Why Did COAPT Win While MITRA-FR Failed? Defining the Appropriate Patient Population for MitraClip. Interv. Cardiol. 2019, 14, 45–47. [Google Scholar] [CrossRef]
- Mauricio, R.; Kumbhani, D.J. MitraClip: How Do We Reconcile the Inconsistent Findings of MITRA-FR and COAPT? Curr. Cardiol. Rep. 2019, 21, 150. [Google Scholar] [CrossRef]
- Betz, J.; Lilly, S.M.; Abraham, W.T. Managing Mitral Regurgitation in Heart Failure-Perspectives After COAPT. Curr. Treat. Options Cardiovasc. Med. 2019, 21, 86. [Google Scholar] [CrossRef]
- Grayburn, P.A.; Sannino, A.; Packer, M. Proportionate and Disproportionate Functional Mitral Regurgitation: A New Conceptual Framework That Reconciles the Results of the MITRA-FR and COAPT Trials. JACC Cardiovasc. Imaging 2019, 12, 353–362. [Google Scholar] [CrossRef]
- Packer, M.; Grayburn, P.A. Contrasting Effects of Pharmacological, Procedural, and Surgical Interventions on Proportionate and Disproportionate Functional Mitral Regurgitation in Chronic Heart Failure. Circulation 2019, 140, 779–789. [Google Scholar] [CrossRef]
- Gupta, A.; Packer, M.; Makkar, R.; Grayburn, P. A Volume-Based Framework Reconciling COAPT, MITRA-FR, and RESHAPE-HF2. J. Am. Coll. Cardiol. 2024, 84, 2376–2379. [Google Scholar] [CrossRef] [PubMed]
- Orban, M.; Karam, N.; Lubos, E.; Kalbacher, D.; Braun, D.; Deseive, S.; Neuss, M.; Butter, C.; Praz, F.; Kassar, M.; et al. Impact of Proportionality of Secondary Mitral Regurgitation on Outcome After Transcatheter Mitral Valve Repair. JACC Cardiovasc. Imaging 2021, 14, 715–725. [Google Scholar] [CrossRef]
- Lindenfeld, J.; Abraham, W.T.; Grayburn, P.A.; Kar, S.; Asch, F.M.; Lim, D.S.; Nie, H.; Singhal, P.; Sundareswaran, K.S.; Weissman, N.J.; et al. Association of Effective Regurgitation Orifice Area to Left Ventricular End-Diastolic Volume Ratio With Transcatheter Mitral Valve Repair Outcomes: A Secondary Analysis of the COAPT Trial. JAMA Cardiol. 2021, 6, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Messika-Zeitoun, D.; Iung, B.; Armoiry, X.; Trochu, J.-N.; Donal, E.; Habib, G.; Brochet, E.; Thibault, H.; Piriou, N.; Cormier, B.; et al. Impact of Mitral Regurgitation Severity and Left Ventricular Remodeling on Outcome After MitraClip Implantation: Results From the Mitra-FR Trial. JACC Cardiovasc. Imaging 2021, 14, 742–752. [Google Scholar] [CrossRef]
- Moonen, A.; Cao, J.; Celermajer, D.S.; Ng, M.K.C. Mitral Regurgitation “Proportionality” in Functional Mitral Regurgitation and Outcomes After Mitral Valve Transcatheter Edge-to-Edge Repair: A Systematic Review and Meta-Analysis. Struct. Heart 2024, 8, 100284. [Google Scholar] [CrossRef]
- Cimino, S.; Agati, L.; Filomena, D.; Maestrini, V.; Monosilio, S.; Birtolo, L.I.; Mocci, M.; Mancone, M.; Sardella, G.; Grayburn, P.; et al. 3D Echo Characterization of Proportionate and Disproportionate Functional Mitral Regurgitation before and after Percutaneous Mitral Valve Repair. J. Clin. Med. 2022, 11, 645. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, H.; Falk, V.; Bax, J.J.; De Bonis, M.; Hamm, C.; Holm, P.J.; Iung, B.; Lancellotti, P.; Lansac, E.; Rodriguez Muñoz, D.; et al. 2017 ESC/EACTS Guidelines for the Management of Valvular Heart Disease. Eur. Heart J. 2017, 38, 2739–2791. [Google Scholar] [CrossRef]
- Nishimura, R.A.; Otto, C.M.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P.; Guyton, R.A.; O’Gara, P.T.; Ruiz, C.E.; Skubas, N.J.; Sorajja, P.; et al. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary. Circulation 2014, 129, 2440–2492. [Google Scholar] [CrossRef]
- Bartko, P.E.; Arfsten, H.; Heitzinger, G.; Pavo, N.; Toma, A.; Strunk, G.; Hengstenberg, C.; Hülsmann, M.; Goliasch, G. A Unifying Concept for the Quantitative Assessment of Secondary Mitral Regurgitation. J. Am. Coll. Cardiol. 2019, 73, 2506–2517. [Google Scholar] [CrossRef]
- Grayburn, P.A.; Carabello, B.; Hung, J.; Gillam, L.D.; Liang, D.; Mack, M.J.; McCarthy, P.M.; Miller, D.C.; Trento, A.; Siegel, R.J. Defining “Severe” Secondary Mitral Regurgitation: Emphasizing an Integrated Approach. J. Am. Coll. Cardiol. 2014, 64, 2792–2801. [Google Scholar] [CrossRef]
- Zoghbi, W.A.; Adams, D.; Bonow, R.O.; Enriquez-Sarano, M.; Foster, E.; Grayburn, P.A.; Hahn, R.T.; Han, Y.; Hung, J.; Lang, R.M.; et al. Recommendations for Noninvasive Evaluation of Native Valvular Regurgitation: A Report from the American Society of Echocardiography Developed in Collaboration with the Society for Cardiovascular Magnetic Resonance. J. Am. Soc. Echocardiogr. 2017, 30, 303–371. [Google Scholar] [CrossRef] [PubMed]
- Vahanian, A.; Beyersdorf, F.; Praz, F.; Milojevic, M.; Baldus, S.; Bauersachs, J.; Capodanno, D.; Conradi, L.; De Bonis, M.; De Paulis, R.; et al. 2021 ESC/EACTS Guidelines for the Management of Valvular Heart Disease: Developed by the Task Force for the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2022, 43, 561–632. [Google Scholar] [CrossRef]
- Bartko, P.E.; Heitzinger, G.; Spinka, G.; Pavo, N.; Prausmüller, S.; Kastl, S.; Winter, M.-P.; Arfsten, H.; Tan, T.C.; Gebhard, C.; et al. Principal Morphomic and Functional Components of Secondary Mitral Regurgitation. JACC Cardiovasc. Imaging 2021, 14, 2288–2300. [Google Scholar] [CrossRef]
- Gaasch, W.H.; Meyer, T.E. Secondary Mitral Regurgitation (Part 1): Volumetric Quantification and Analysis. Heart 2018, 104, 634. [Google Scholar] [CrossRef]
- Grayburn, P.A.; Weissman, N.J.; Zamorano, J.L. Quantitation of Mitral Regurgitation. Circulation 2012, 126, 2005–2017. [Google Scholar] [CrossRef] [PubMed]
- Grayburn, P.A.; Appleton, C.P.; DeMaria, A.N.; Greenberg, B.; Lowes, B.; Oh, J.; Plehn, J.F.; Rahko, P.; Sutton, M.S.J.; Eichhorn, E.J. Echocardiographic Predictors of Morbidity and Mortality in Patients with Advanced Heart Failure: The Beta-Blocker Evaluation of Survival Trial (BEST). J. Am. Coll. Cardiol. 2005, 45, 1064–1071. [Google Scholar] [CrossRef]
- Bohra, C.; Asch, F.M.; Lerakis, S.; Little, S.H.; Redfors, B.; Zhou, Z.; Li, Y.; Weissman, N.J.; Grayburn, P.A.; Kar, S.; et al. Pulmonary Vein Systolic Flow Reversal and Outcomes in Patients From the Cardiovascular Outcomes Assessment of the MitraClip Percutaneous Therapy for Heart Failure Patients With Functional Mitral Regurgitation (COAPT) Trial. Struct. Heart 2024, 8, 100333. [Google Scholar] [CrossRef] [PubMed]
- Karam, N.; Stolz, L.; Orban, M.; Deseive, S.; Praz, F.; Kalbacher, D.; Westermann, D.; Braun, D.; Näbauer, M.; Neuss, M.; et al. Impact of Right Ventricular Dysfunction on Outcomes After Transcatheter Edge-to-Edge Repair for Secondary Mitral Regurgitation. JACC Cardiovasc. Imaging 2021, 14, 768–778. [Google Scholar] [CrossRef]
- Doldi, P.M.; Stolz, L.; Kalbacher, D.; Köll, B.; Geyer, M.; Ludwig, S.; Orban, M.; Braun, D.; Weckbach, L.T.; Stocker, T.J.; et al. Right Ventricular Dysfunction Predicts Outcome after Transcatheter Mitral Valve Repair for Primary Mitral Valve Regurgitation. Eur. J. Heart Fail. 2022, 24, 2162–2171. [Google Scholar] [CrossRef]
- Brener, M.I.; Grayburn, P.; Lindenfeld, J.; Burkhoff, D.; Liu, M.; Zhou, Z.; Alu, M.C.; Medvedofsky, D.A.; Asch, F.M.; Weissman, N.J.; et al. Right Ventricular–Pulmonary Arterial Coupling in Patients With HF Secondary MR: Analysis from the COAPT Trial. JACC Cardiovasc. Interv. 2021, 14, 2231–2242. [Google Scholar] [CrossRef]
- Blanco, P. Rationale for Using the Velocity–Time Integral and the Minute Distance for Assessing the Stroke Volume and Cardiac Output in Point-of-Care Settings. Ultrasound J. 2020, 12, 21. [Google Scholar] [CrossRef]
- Dujardin, K.S.; Enriquez-Sarano, M.; Bailey, K.R.; Nishimura, R.A.; Seward, J.B.; Tajik, A.J. Grading of Mitral Regurgitation by Quantitative Doppler Echocardiography. Circulation 1997, 96, 3409–3415. [Google Scholar] [CrossRef] [PubMed]
- Grigioni, F.; Enriquez-Sarano, M.; Zehr, K.J.; Bailey, K.R.; Tajik, A.J. Ischemic Mitral Regurgitation. Circulation 2001, 103, 1759–1764. [Google Scholar] [CrossRef]
- Huang, A.L.; Dal-Bianco, J.P.; Levine, R.A.; Hung, J.W. Secondary Mitral Regurgitation: Cardiac Remodeling, Diagnosis, and Management. Struct. Heart 2023, 7, 100129. [Google Scholar] [CrossRef]
- Igata, S.; Cotter, B.R.; Hang, C.T.; Morikawa, N.; Strachan, M.; Raisinghani, A.; Blanchard, D.G.; Demaria, A.N. Optimal Quantification of Functional Mitral Regurgitation: Comparison of Volumetric and Proximal Isovelocity Surface Area Methods to Predict Outcome. J. Am. Heart Assoc. Cardiovasc. Cerebrovasc. Dis. 2021, 10, 18553. [Google Scholar] [CrossRef] [PubMed]
- Smer, A.; Nanda, N.C.; Akdogan, R.E.; Elmarzouky, Z.M.; Dulal, S. Echocardiographic Evaluation of Mitral Valve Regurgitation. Mini-invasive Surg. 2020, 4, 52. [Google Scholar] [CrossRef]
- Uretsky, S.; Argulian, E.; Narula, J.; Wolff, S.D. Use of Cardiac Magnetic Resonance Imaging in Assessing Mitral Regurgitation: Current Evidence. J. Am. Coll. Cardiol. 2018, 71, 547–563. [Google Scholar] [CrossRef]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2015, 28, 1–39.e14. [Google Scholar] [CrossRef]
- Sonaglioni, A.; Nicolosi, G.L.; Rigamonti, E.; Lombardo, M. Impact of Chest Wall Conformation on the Outcome of Primary Mitral Regurgitation Due to Mitral Valve Prolapse. J. Cardiovasc. Echogr. 2022, 32, 29–37. [Google Scholar] [CrossRef]
- Bilbija, I.; Matkovic, M.; Cubrilo, M.; Aleksic, N.; Milin Lazovic, J.; Cumic, J.; Tutus, V.; Jovanovic, M.; Putnik, S. The Prospects of Secondary Moderate Mitral Regurgitation after Aortic Valve Replacement—Meta-Analysis. Int. J. Environ. Res. Public Heal. 2020, 17, 7335. [Google Scholar] [CrossRef]
- Unger, P.; Magne, J.; Eynden, F.V.; Plein, D.; Van Camp, G.; Pasquet, A.; Cosyns, B.; Dedobbeleer, C.; Lancellotti, P. Impact of Prosthesis–Patient Mismatch on Mitral Regurgitation after Aortic Valve Replacement. Heart 2010, 96, 1627–1632. [Google Scholar] [CrossRef]
- Dabic, P.; Vucurevic, B.; Sevkovic, M.; Andric, D.; Pesic, S.; Neskovic, M.; Borovic, S.; Petrovic, J. Functional Mitral Regurgitation Post-Isolated Aortic Valve Replacement. J. Clin. Med. 2024, 13, 6971. [Google Scholar] [CrossRef] [PubMed]
- Hu, R.; Chen, T. Leaning Too Much on the Power of Proximal Isovelocity Surface Area? Don’t Forget the Volumetric Method for Quantifying Functional Mitral Regurgitation. J. Am. Heart Assoc. 2021, 10, e021914. [Google Scholar] [CrossRef]
- Harm, T.; Schwarz, F.-J.; Zdanyte, M.; Goldschmied, A.; Baas, L.; Aidery, P.; Shcherbyna, S.; Toskas, I.; Keller, T.; Kast, I.; et al. Novel 3-Dimensional Effective Regurgitation Orifice Area Quantification Serves as a Reliable Tool to Identify Severe Mitral Valve Regurgitation. Sci. Rep. 2024, 14, 22067. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Heo, R.; Hong, G.-R.; Chang, H.-J.; Sung, J.M.; Shin, S.H.; Cho, I.J.; Shim, C.-Y.; Chung, N. Differential Effect of 3-Dimensional Color Doppler Echocardiography for the Quantification of Mitral Regurgitation According to the Severity and Characteristics. Circ. Cardiovasc. Imaging 2014, 7, 535–544. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Heo, R.; Son, J.-W.; ó Hartaigh, B.; Chang, H.-J.; Kim, Y.-J.; Datta, S.; Cho, I.-J.; Shim, C.Y.; Hong, G.-R.; Ha, J.-W.; et al. Clinical Implications of Three-Dimensional Real-Time Color Doppler Transthoracic Echocardiography in Quantifying Mitral Regurgitation: A Comparison with Conventional Two-Dimensional Methods. J. Am. Soc. Echocardiogr. 2017, 30, 393–403.e7. [Google Scholar] [CrossRef]
- Sköldborg, V.; Madsen, P.L.; Dalsgaard, M.; Abdulla, J. Quantification of Mitral Valve Regurgitation by 2D and 3D Echocardiography Compared with Cardiac Magnetic Resonance a Systematic Review and Meta-Analysis. Int. J. Cardiovasc. Imaging 2020, 36, 279–289. [Google Scholar] [CrossRef]
- Garg, P.; Pavon, A.G.; Penicka, M.; Uretsky, S. Cardiovascular Magnetic Resonance Imaging in Mitral Valve Disease. Eur. Heart J. 2024, 46, ehae801. [Google Scholar] [CrossRef]
- Garg, P.; Swift, A.J.; Zhong, L.; Carlhäll, C.J.; Ebbers, T.; Westenberg, J.; Hope, M.D.; Bucciarelli-Ducci, C.; Bax, J.J.; Myerson, S.G. Assessment of Mitral Valve Regurgitation by Cardiovascular Magnetic Resonance Imaging. Nat. Rev. Cardiol. 2019, 17, 298–312. [Google Scholar] [CrossRef]
- Tayal, B.; Debs, D.; Nabi, F.; Malahfji, M.; Little, S.H.; Reardon, M.; Zoghbi, W.; Kleiman, N.; Shah, D.J. Impact of Myocardial Scar on Prognostic Implication of Secondary Mitral Regurgitation in Heart Failure. JACC Cardiovasc. Imaging 2021, 14, 812–822. [Google Scholar] [CrossRef]
- Myerson, S.G.; D’Arcy, J.; Christiansen, J.P.; Dobson, L.E.; Mohiaddin, R.; Francis, J.M.; Prendergast, B.; Greenwood, J.P.; Karamitsos, T.D.; Neubauer, S. Determination of Clinical Outcome in Mitral Regurgitation With Cardiovascular Magnetic Resonance Quantification. Circulation 2016, 133, 2287–2296. [Google Scholar] [CrossRef] [PubMed]
- Penicka, M.; Vecera, J.; Mirica, D.C.; Kotrc, M.; Kockova, R.; Van Camp, G. Prognostic Implications of Magnetic Resonance-Derived Quantification in Asymptomatic Patients with Organic Mitral Regurgitation: Comparison with Doppler Echocardiography-Derived Integrative Approach. Circulation 2018, 137, 1349–1360. [Google Scholar] [CrossRef] [PubMed]
- Uretsky, S.; Gillam, L.; Lang, R.; Chaudhry, F.A.; Argulian, E.; Supariwala, A.; Gurram, S.; Jain, K.; Subero, M.; Jang, J.J.; et al. Discordance Between Echocardiography and MRI in the Assessment of Mitral Regurgitation Severity: A Prospective Multicenter Trial. J. Am. Coll. Cardiol. 2015, 65, 1078–1088. [Google Scholar] [CrossRef]
- Suinesiaputra, A.; Bluemke, D.A.; Cowan, B.R.; Friedrich, M.G.; Kramer, C.M.; Kwong, R.; Plein, S.; Schulz-Menger, J.; Westenberg, J.J.M.; Young, A.A.; et al. Quantification of LV Function and Mass by Cardiovascular Magnetic Resonance: Multi-Center Variability and Consensus Contours. J. Cardiovasc. Magn. Reson. 2015, 17, 63. [Google Scholar] [CrossRef]
- Cavalcante, J.L.; Lopes, B.B.C. Left Ventricular Scar Burden as a Modulator of Risk in Functional Mitral Regurgitation. JACC Cardiovasc. Imaging 2021, 14, 823–825. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.K.M.; Kocyigit, D.; Choi, H.; Anthony, C.M.; Chan, N.; Bullen, J.; Popović, Z.B.; Kapadia, S.R.; Krishnaswamy, A.; Griffin, B.P.; et al. Prognostic Power of Quantitative Assessment of Functional Mitral Regurgitation and Myocardial Scar Quantification by Cardiac Magnetic Resonance. Circ. Cardiovasc. Imaging 2023, 16, e015134. [Google Scholar] [CrossRef]
- Ivanov, A.; Bhumireddy, G.P.; Dabiesingh, D.S.; Khan, S.A.; Ho, J.; Krishna, N.; Dontineni, N.; Socolow, J.A.; Briggs, W.M.; Klem, I.; et al. Importance of Papillary Muscle Infarction Detected by Cardiac Magnetic Resonance Imaging in Predicting Cardiovascular Events. Int. J. Cardiol. 2016, 220, 558–563. [Google Scholar] [CrossRef]
- Ikeda, Y.; Inomata, T.; Fujita, T.; Iida, Y.; Nabeta, T.; Ishii, S.; Maekawa, E.; Yanagisawa, T.; Mizutani, T.; Naruke, T.; et al. Cardiac Fibrosis Detected by Magnetic Resonance Imaging on Predicting Time Course Diversity of Left Ventricular Reverse Remodeling in Patients with Idiopathic Dilated Cardiomyopathy. Heart Vessels 2016, 31, 1817–1825. [Google Scholar] [CrossRef]
- Zoghbi, W.A.; Asch, F.M.; Bruce, C.; Gillam, L.D.; Grayburn, P.A.; Hahn, R.T.; Inglessis, I.; Islam, A.M.; Lerakis, S.; Little, S.H.; et al. Guidelines for the Evaluation of Valvular Regurgitation After Percutaneous Valve Repair or Replacement: A Report from the American Society of Echocardiography Developed in Collaboration with the Society for Cardiovascular Angiography and Interventions, Japanese Society of Echocardiography, and Society for Cardiovascular Magnetic Resonance. J. Am. Soc. Echocardiogr. 2019, 32, 431–475. [Google Scholar] [CrossRef]
- Trenkwalder, T.; Lachmann, M.; Stolz, L.; Fortmeier, V.; Covarrubias, H.A.A.; Rippen, E.; Schürmann, F.; Presch, A.; von Scheidt, M.; Ruff, C.; et al. Machine Learning Identifies Pathophysiologically and Prognostically Informative Phenotypes among Patients with Mitral Regurgitation Undergoing Transcatheter Edge-to-Edge Repair. Eur. Heart J. Cardiovasc. Imaging 2023, 24, 574–587. [Google Scholar] [CrossRef]
- D’Ascenzo, F.; Angelini, F.; Pancotti, C.; Bocchino, P.P.; Giannini, C.; Finizio, F.; Adamo, M.; Camman, V.; Morici, N.; Perl, L.; et al. Machine-Learning Phenotyping of Patients with Functional Mitral Regurgitation Undergoing Transcatheter Edge-to-Edge Repair: The MITRA-AI Study. Eur. Hearh J. Digit. Health 2025, 6, ztaf006. [Google Scholar] [CrossRef] [PubMed]
- Hausleiter, J.; Lachmann, M.; Stolz, L.; Bedogni, F.; Rubbio, A.P.; Estévez-Loureiro, R.; Raposeiras-Roubin, S.; Boekstegers, P.; Karam, N.; Rudolph, V. Artificial Intelligence-Derived Risk Score for Mortality in Secondary Mitral Regurgitation Treated by Transcatheter Edge-to-Edge Repair: The EuroSMR Risk Score. Eur. Heart J. 2024, 45, 922–936. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).