Diagnosis and Diagnostic Challenges of Secondary Mitral Regurgitation in the Era of Transcatheter Edge-to-Edge Repair of the Mitral Valve
Abstract
1. Introduction
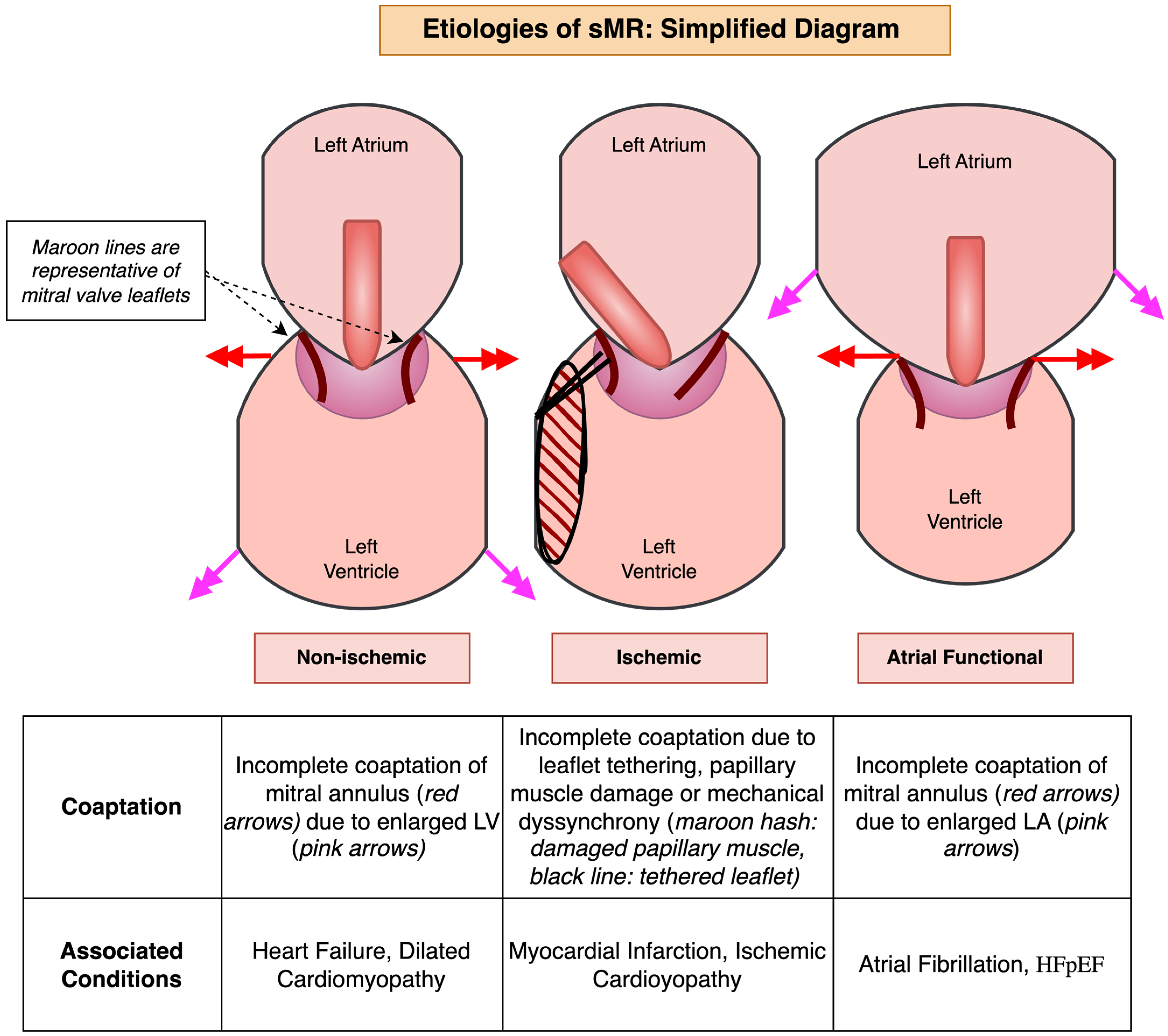
2. Etiology of Secondary MR
2.1. Non-Ischemic Secondary MR
2.2. Ischemic Secondary MR
2.3. Atrial Functional MR
3. Management of Secondary MR with Transcatheter Edge-to-Edge Repair (TEER) of Mitral Valve
3.1. Pivotal RCTs That Transformed sMR Management with M-TEER
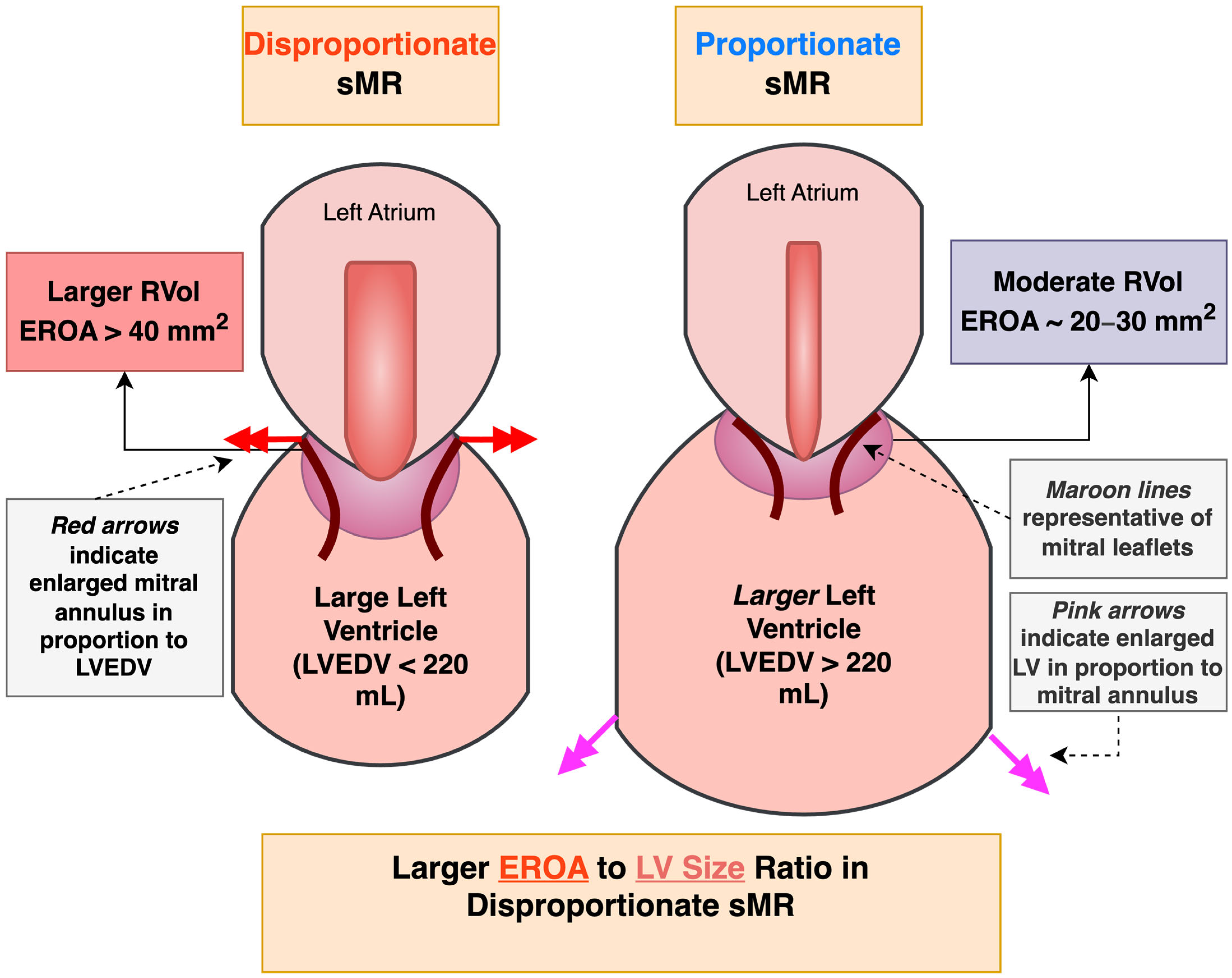
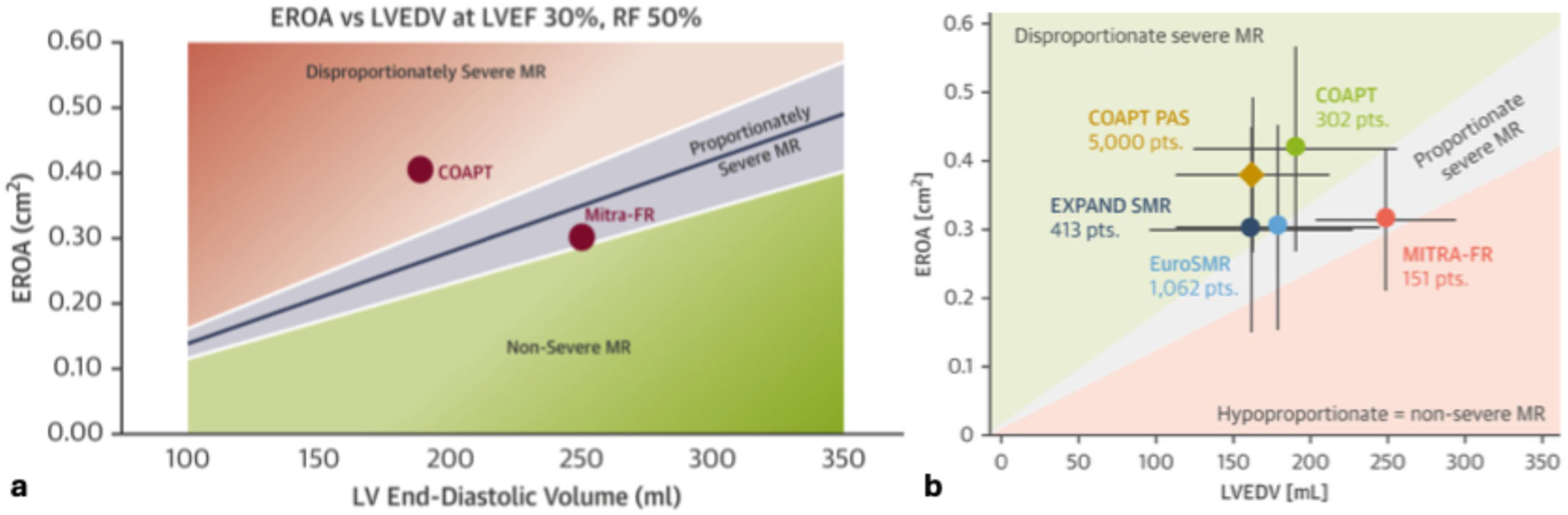
3.2. Conceptualizing the Diverging Results of MITRA-FR with the Other Trials
3.3. Guideline Recommendations Regarding sMR Severity and M-TEER Candidacy
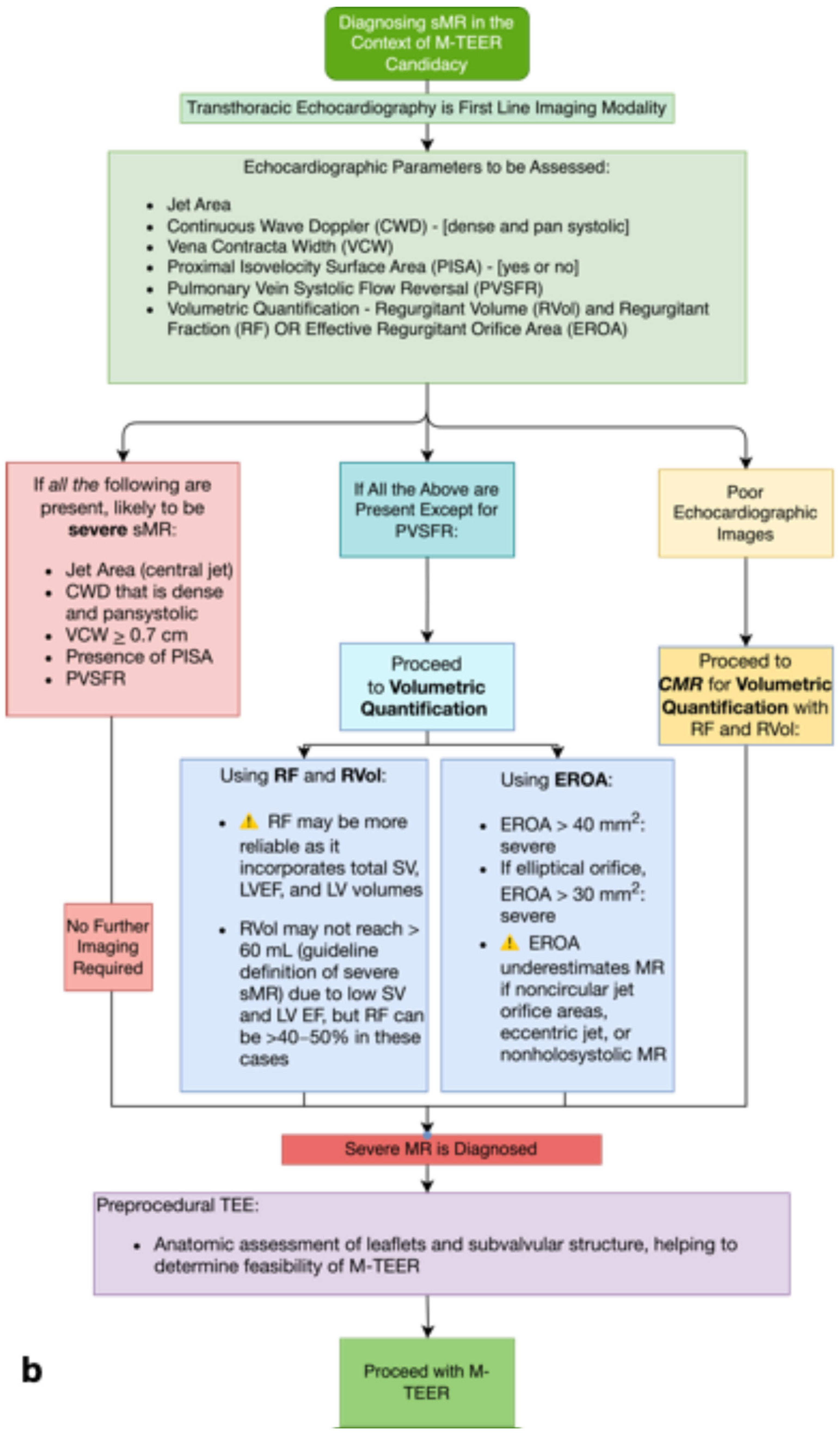
4. Diagnostic Challenges of Heart Failure and Secondary Mitral Regurgitation in the Era of Transcatheter Edge-to-Edge Repair of the Mitral Valve
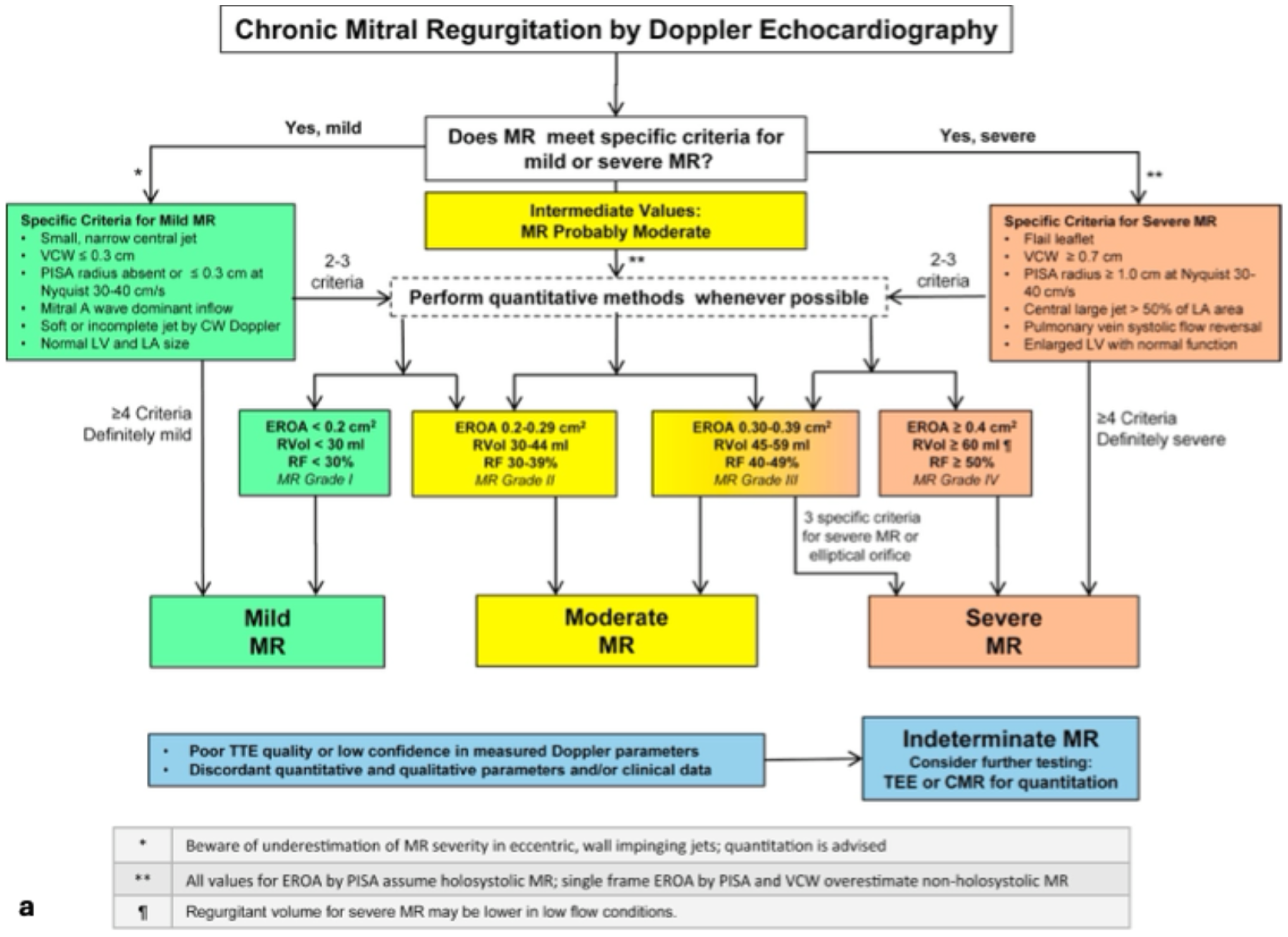
4.1. Defining Secondary MR
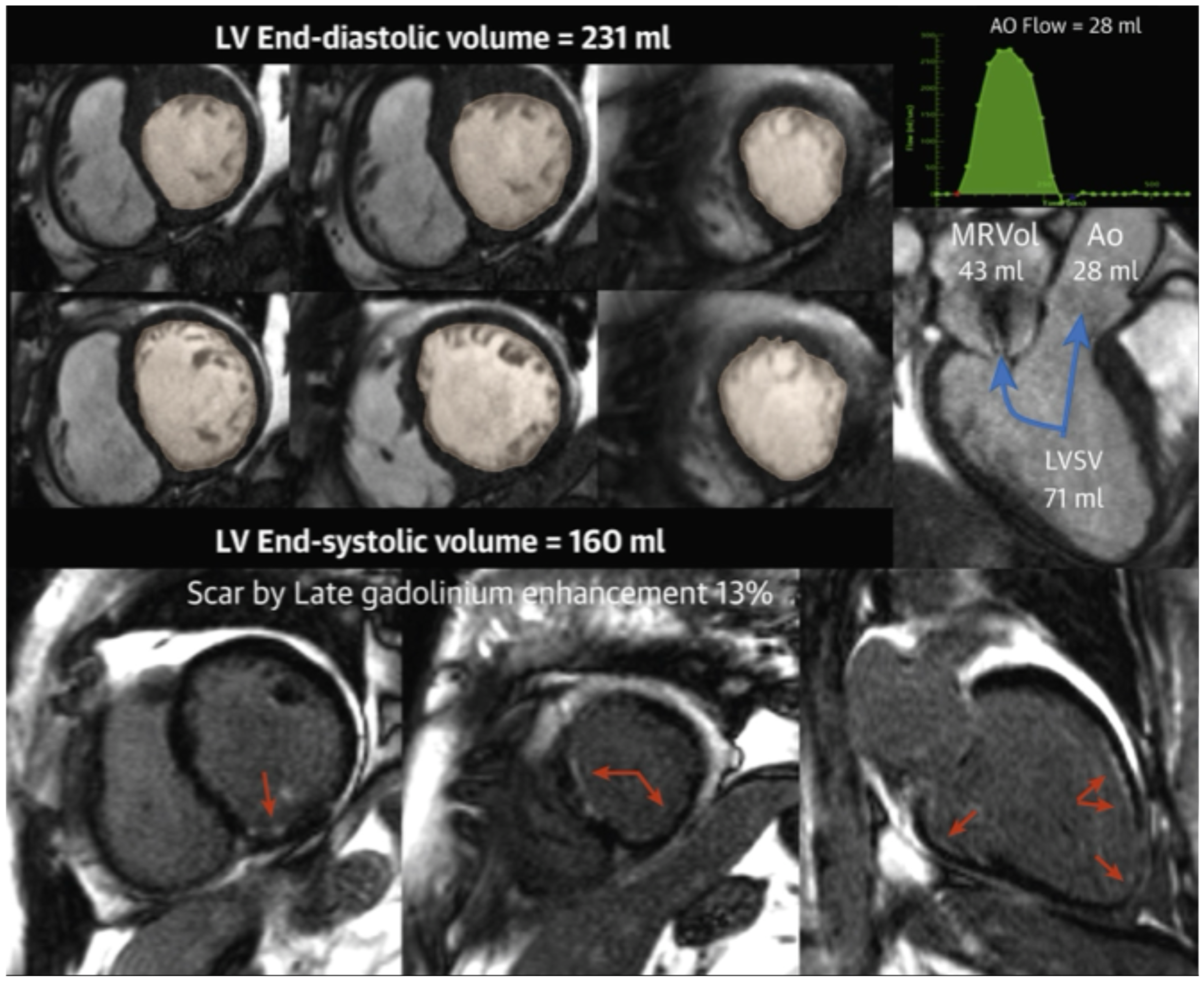
4.2. Emerging Role of Cardiac Magnetic Resonance Imaging
4.3. Future Role of Artificial Intelligence
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| MR | Mitral regurgitation |
| MV | Mitral valve |
| sMR | Secondary mitral regurgitation |
| HF | Heart failure |
| GDMT | Guideline-directed medical therapy |
| CRT | Cardiac resynchronization therapy |
| m-TEER | Transcatheter edge-to-edge repair of the mitral valve |
| RCT | Randomized control trial |
| EROA | Effective regurgitant orifice area |
| LVEDV | Left ventricular end diastolic volume |
| ARNI | Angiotensin receptor/neprilysin inhibitor |
| MRA | Mineralocorticoid receptor antagonist |
| SGLT-2 | Sodium glucose transporter—2 |
| RVol | Regurgitant volume |
| ACC/ASE | American College of Cardiology/American Society of Echocardiography |
| ACC/AHA | American College of Cardiology/American Heart Association |
| ESC/EACTS | European Society of Cardiology/European Association for Cardio-Thoracic Surgery |
| EACVI | European Association of Cardiovascular Imaging |
| RF | Regurgitant fraction |
| TTE | Transthoracic echocardiography |
| CMR | Cardiac magnetic resonance imaging |
References
- Nishimura, R.A.; Otto, C.M.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P.; Fleisher, L.A.; Jneid, H.; Mack, M.J.; McLeod, C.J.; O’Gara, P.T.; et al. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2017, 70, 252–289. [Google Scholar] [CrossRef] [PubMed]
- Otto, C.M.; Nishimura, R.A.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P., 3rd; Gentile, F.; Jneid, H.; Krieger, E.V.; Mack, M.; McLeod, C.; et al. 2020 ACC/AHA Guideline for the Management of Patients with Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Thorac. Cardiovasc. Surg. 2021, 162, e183–e353. [Google Scholar] [CrossRef]
- Bartko, P.E.; Pavo, N.; Pérez-Serradilla, A.; Arfsten, H.; Neuhold, S.; Wurm, R.; Lang, I.M.; Strunk, G.; Dal-Bianco, J.P.; Levine, R.A.; et al. Evolution of Secondary Mitral Regurgitation. Eur. Heart J. Cardiovasc. Imaging 2018, 19, 622–629. [Google Scholar] [CrossRef] [PubMed]
- Piérard, L.A.; Carabello, B.A. Ischaemic Mitral Regurgitation: Pathophysiology, Outcomes and the Conundrum of Treatment. Eur. Heart J. 2010, 31, 2996–3005. [Google Scholar] [CrossRef]
- Russo, E.; Russo, G.; Cassese, M.; Braccio, M.; Carella, M.; Compagnucci, P.; Dello Russo, A.; Casella, M. The Role of Cardiac Resynchronization Therapy for the Management of Functional Mitral Regurgitation. Cells 2022, 11, 2407. [Google Scholar] [CrossRef]
- Hausleiter, J.; Stocker, T.J.; Adamo, M.; Karam, N.; Swaans, M.J.; Praz, F. Mitral Valve Transcatheter Edge-to-Edge Repair. EuroIntervention 2023, 18, 957–976. [Google Scholar] [CrossRef] [PubMed]
- Packer, M. Disproportionate Functional Mitral Regurgitation: A New Therapeutic Target in Patients with Heart Failure and a Reduced Ejection Fraction. Eur. J. Heart Fail. 2020, 22, 23–25. [Google Scholar] [CrossRef]
- El Sabbagh, A.; Reddy, Y.N.; Nishimura, R.A. Mitral Valve Regurgitation in the Contemporary Era: Insights Into Diagnosis, Management, and Future Directions. JACC Cardiovasc. Imaging 2018, 11, 628–643. [Google Scholar] [CrossRef]
- Varma, P.K.; Krishna, N.; Jose, R.L.; Madkaiker, A.N. Ischemic Mitral Regurgitation. Ann. Card. Anaesth. 2017, 20, 432–439. [Google Scholar] [CrossRef]
- Zoghbi, W.A.; Levine, R.A.; Flachskampf, F.; Grayburn, P.; Gillam, L.; Leipsic, J.; Thomas, J.D.; Kwong, R.Y.; Vandervoort, P.; Chandrashekhar, Y. Atrial Functional Mitral Regurgitation: A JACC: Cardiovascular Imaging Expert Panel Viewpoint. JACC Cardiovasc. Imaging 2022, 15, 1870–1882. [Google Scholar] [CrossRef]
- Hirji, S.A.; Cote, C.L.; Javadikasgari, H.; Malarczyk, A.; McGurk, S.; Kaneko, T. Atrial Functional versus Ventricular Functional Mitral Regurgitation: Prognostic Implications. J. Thorac. Cardiovasc. Surg. 2022, 164, 1808–1815.e4. [Google Scholar] [CrossRef] [PubMed]
- Bove, T. Commentary: Functional Mitral Regurgitation: The 2 Sides of 1 Coin. J. Thorac. Cardiovasc. Surg. 2022, 164, 1816–1817. [Google Scholar] [CrossRef] [PubMed]
- Stolz, L.; Doldi, P.M.; Sannino, A.; Hausleiter, J.; Grayburn, P.A. The Evolving Concept of Secondary Mitral Regurgitation Phenotypes: Lessons From the M-TEER Trials. JACC Cardiovasc. Imaging 2024, 17, 659–668. [Google Scholar] [CrossRef]
- von Stein, P.; Iliadis, C. Transcatheter Edge-to-Edge Repair for Mitral Regurgitation. Trends Cardiovasc. Med. 2025, 35, 320–325. [Google Scholar] [CrossRef] [PubMed]
- von Stein, P.; von Stein, J.; Hohmann, C.; Wienemann, H.; Guthoff, H.; Körber, M.I.; Baldus, S.; Pfister, R.; Hahn, R.T.; Iliadis, C. Atrial Functional Mitral Regurgitation Subtypes Undergoing Transcatheter Edge-to-Edge Repair: Suboptimal Outcomes in Atriogenic Hamstringing. JACC Cardiovasc. Imaging 2025, 18, 16–29. [Google Scholar] [CrossRef]
- Goel, S.S.; Bajaj, N.; Aggarwal, B.; Gupta, S.; Poddar, K.L.; Ige, M.; Bdair, H.; Anabtawi, A.; Rahim, S.; Whitlow, P.L.; et al. Prevalence and Outcomes of Unoperated Patients with Severe Symptomatic Mitral Regurgitation and Heart Failure: Comprehensive Analysis to Determine the Potential Role of MitraClip for This Unmet Need. J. Am. Coll. Cardiol. 2014, 63, 185–186. [Google Scholar] [CrossRef]
- Enriquez-Sarano, M.; Akins, C.W.; Vahanian, A. Mitral Regurgitation. Lancet 2009, 373, 1382–1394. [Google Scholar] [CrossRef]
- de Groot-de Laat, L.E.; Huizer, J.; Lenzen, M.; Spitzer, E.; Ren, B.; Geleijnse, M.L.; Caliskan, K. Evolution of Mitral Regurgitation in Patients with Heart Failure Referred to a Tertiary Heart Failure Clinic. ESC Heart Fail. 2019, 6, 936–943. [Google Scholar] [CrossRef]
- Nasser, R.; Van Assche, L.; Vorlat, A.; Vermeulen, T.; Van Craenenbroeck, E.; Conraads, V.; Van der Meiren, V.; Shivalkar, B.; Van Herck, P.; Claeys, M.J. Evolution of Functional Mitral Regurgitation and Prognosis in Medically Managed Heart Failure Patients With Reduced Ejection Fraction. JACC Heart Fail. 2017, 5, 652–659. [Google Scholar] [CrossRef]
- Sannino, A.; Sudhakaran, S.; Milligan, G.; Chowdhury, A.; Haq, A.; Szerlip, M.; Packer, M.; Grayburn, P.A. Effectiveness of Medical Therapy for Functional Mitral Regurgitation in Heart Failure With Reduced Ejection Fraction. J. Am. Coll. Cardiol. 2020, 76, 883–884. [Google Scholar] [CrossRef]
- Adamo, M.; Tomasoni, D.; Stolz, L.; Stocker, T.J.; Pancaldi, E.; Koell, B.; Karam, N.; Besler, C.; Giannini, C.; Sampaio, F.; et al. Impact of Transcatheter Edge-to-Edge Mitral Valve Repair on Guideline-Directed Medical Therapy Uptitration. JACC Cardiovasc. Interv. 2023, 16, 896–905. [Google Scholar] [CrossRef] [PubMed]
- Stone, G.W.; Lindenfeld, J.; Abraham, W.T.; Kar, S.; Lim, D.S.; Mishell, J.M.; Whisenant, B.; Grayburn, P.A.; Rinaldi, M.; Kapadia, S.R.; et al. Transcatheter Mitral-Valve Repair in Patients with Heart Failure. N. Engl. J. Med. 2018, 379, 2307–2318. [Google Scholar] [CrossRef] [PubMed]
- Freixa, X.; Tolosana, J.M.; Cepas-Guillen, P.L.; Hernández-Enríquez, M.; Sanchis, L.; Flores-Umanzor, E.; Farrero, M.; Andrea, R.; Roqué, M.; Carretero, M.J.; et al. Edge-to-Edge Transcatheter Mitral Valve Repair Versus Optimal Medical Treatment in Nonresponders to Cardiac Resynchronization Therapy: The MITRA-CRT Trial. Circ. Heart Fail. 2022, 15, e009501. [Google Scholar] [CrossRef]
- Anker, S.D.; Friede, T.; von Bardeleben, R.S.; Butler, J.; Khan, M.S.; Diek, M.; Heinrich, J.; Geyer, M.; Placzek, M.; Ferrari, R.; et al. Percutaneous Repair of Moderate-to-Severe or Severe Functional Mitral Regurgitation in Patients with Symptomatic Heart Failure: Baseline Characteristics of Patients in the RESHAPE-HF2 Trial and Comparison to COAPT and MITRA-FR Trials. Eur. J. Heart Fail. 2024, 26, 1608–1615. [Google Scholar] [CrossRef] [PubMed]
- Stone, G.W.; Abraham, W.T.; Lindenfeld, J.; Kar, S.; Grayburn, P.A.; Lim, D.S.; Mishell, J.M.; Whisenant, B.; Rinaldi, M.; Kapadia, S.R.; et al. Five-Year Follow-up after Transcatheter Repair of Secondary Mitral Regurgitation. N. Engl. J. Med. 2023, 388, 2037–2048. [Google Scholar] [CrossRef]
- Kalbacher, D.; Schäfer, U.; Bardeleben, R.S.V.; Eggebrecht, H.; Sievert, H.; Nickenig, G.; Butter, C.; May, A.E.; Bekeredjian, R.; Ouarrak, T.; et al. Long-Term Outcome, Survival and Predictors of Mortality after MitraClip Therapy: Results from the German Transcatheter Mitral Valve Interventions (TRAMI) Registry. Int. J. Cardiol. 2019, 277, 35–41. [Google Scholar] [CrossRef]
- Kar, S.; von Bardeleben, R.S.; Rottbauer, W.; Mahoney, P.; Price, M.J.; Grasso, C.; Williams, M.; Lurz, P.; Ahmed, M.; Hausleiter, J.; et al. Contemporary Outcomes Following Transcatheter Edge-to-Edge Repair: 1-Year Results From the EXPAND Study. JACC Cardiovasc. Interv. 2023, 16, 589–602. [Google Scholar] [CrossRef]
- von Bardeleben, R.S.; Mahoney, P.; Morse, M.A.; Price, M.J.; Denti, P.; Maisano, F.; Rogers, J.H.; Rinaldi, M.; De Marco, F.; Rollefson, W.; et al. 1-Year Outcomes With Fourth-Generation Mitral Valve Transcatheter Edge-to-Edge Repair From the EXPAND G4 Study. JACC Cardiovasc. Interv. 2023, 16, 2600–2610. [Google Scholar] [CrossRef]
- Lurz, P.; Schmitz, T.; Geisler, T.; Hausleiter, J.; Eitel, I.; Rudolph, V.; Lubos, E.; von Bardeleben, R.S.; Brambilla, N.; De Marco, F.; et al. Mitral Valve Transcatheter Edge-to-Edge Repair: 1-Year Outcomes From the MiCLASP Study. JACC Cardiovasc. Interv. 2024, 17, 890–903. [Google Scholar] [CrossRef] [PubMed]
- Goel, K.; Lindenfeld, J.; Makkar, R.; Naik, H.; Atmakuri, S.; Mahoney, P.; Morse, M.A.; Thourani, V.H.; Yadav, P.; Batchelor, W.; et al. Transcatheter Edge-to-Edge Repair in 5,000 Patients With Secondary Mitral Regurgitation: COAPT Post-Approval Study. J. Am. Coll. Cardiol. 2023, 82, 1281–1297. [Google Scholar] [CrossRef]
- Stolz, L.; Stocker, T.J.; Lurz, P.; Hausleiter, J. Growing Evidence for Edge-to-Edge Repair in Secondary Mitral Regurgitation: What to Learn From COAPT, MITRA-FR, and RESHAPE-HF2. JACC Cardiovasc. Interv. 2025, 18, 927–932. [Google Scholar] [CrossRef] [PubMed]
- Makkar, R.R.; Chikwe, J.; Chakravarty, T.; Chen, Q.; O’Gara, P.T.; Gillinov, M.; Mack, M.J.; Vekstein, A.; Patel, D.; Stebbins, A.L.; et al. Transcatheter Mitral Valve Repair for Degenerative Mitral Regurgitation. JAMA 2023, 329, 1778–1788. [Google Scholar] [CrossRef]
- Garcia, S.; Elmariah, S.; Cubeddu, R.J.; Zahr, F.; Eleid, M.F.; Kodali, S.K.; Seshiah, P.; Sharma, R.; Lim, D.S. Mitral Transcatheter Edge-to-Edge Repair with the PASCAL Precision System: Device Knobology and Review of Advanced Steering Maneuvers. Struct. Heart 2024, 8, 100234. [Google Scholar] [CrossRef] [PubMed]
- Zahr, F.; Smith, R.L.; Gillam, L.D.; Chadderdon, S.; Makkar, R.; von Bardeleben, R.S.; Ruf, T.F.; Kipperman, R.M.; Rassi, A.N.; Szerlip, M.; et al. One-Year Outcomes From the CLASP IID Randomized Trial for Degenerative Mitral Regurgitation. JACC Cardiovasc. Interv. 2023, 16, 2803–2816. [Google Scholar] [CrossRef] [PubMed]
- Feldman, T.; Kar, S.; Elmariah, S.; Smart, S.C.; Trento, A.; Siegel, R.J.; Apruzzese, P.; Fail, P.; Rinaldi, M.J.; Smalling, R.W.; et al. Randomized Comparison of Percutaneous Repair and Surgery for Mitral Regurgitation: 5-Year Results of EVEREST II. J. Am. Coll. Cardiol. 2015, 66, 2844–2854. [Google Scholar] [CrossRef]
- Feldman, T.; Foster, E.; Glower, D.D.; Kar, S.; Rinaldi, M.J.; Fail, P.S.; Smalling, R.W.; Siegel, R.; Rose, G.A.; Engeron, E.; et al. Percutaneous Repair or Surgery for Mitral Regurgitation. N. Engl. J. Med. 2011, 364, 1395–1406. [Google Scholar] [CrossRef]
- Doldi, P.; Stolz, L.; Orban, M.; Karam, N.; Praz, F.; Kalbacher, D.; Lubos, E.; Braun, D.; Adamo, M.; Giannini, C.; et al. Transcatheter Mitral Valve Repair in Patients With Atrial Functional Mitral Regurgitation. JACC Cardiovasc. Imaging 2022, 15, 1843–1851. [Google Scholar] [CrossRef]
- Yoshida, J.; Ikenaga, H.; Nagaura, T.; Utsunomiya, H.; Kawai, M.; Makar, M.; Rader, F.; Siegel, R.J.; Kar, S.; Makkar, R.R.; et al. Impact of Percutaneous Edge-to-Edge Repair in Patients With Atrial Functional Mitral Regurgitation. Circ. J. 2021, 85, 1001–1010. [Google Scholar] [CrossRef]
- Rudolph, F.; Geyer, M.; Baldus, S.; De Luca, V.M.; Doenst, T.; Pfister, R.; Gummert, J.; Kessler, M.; Boekstegers, P.; Lubos, E.; et al. Transcatheter Repair Versus Surgery for Atrial Versus Ventricular Functional Mitral Regurgitation: A Post Hoc Analysis of the MATTERHORN Trial. Circulation 2025, 151, 418–420. [Google Scholar] [CrossRef]
- Mauri, L.; Garg, P.; Massaro, J.M.; Foster, E.; Glower, D.; Mehoudar, P.; Powell, F.; Komtebedde, J.; McDermott, E.; Feldman, T. The EVEREST II Trial: Design and Rationale for a Randomized Study of the Evalve Mitraclip System Compared with Mitral Valve Surgery for Mitral Regurgitation. Am. Heart J. 2010, 160, 23–29. [Google Scholar] [CrossRef]
- Feldman, T.; Fernandes, E.; Levisay, J.P. Transcatheter Mitral Valve Repair/Replacement for Primary Mitral Regurgitation. Ann. Cardiothorac. Surg. 2018, 7, 755–763. [Google Scholar] [CrossRef] [PubMed]
- Jean-François, O.; David, M.-Z.; Guillaume, L.; Bernard, I.; Guillaume, B.; Nicolas, P.; Thierry, L.; Christophe, P.; Frédéric, R.; Didier, C.; et al. Percutaneous Repair or Medical Treatment for Secondary Mitral Regurgitation. N. Engl. J. Med. 2018, 379, 2297–2306. [Google Scholar] [CrossRef]
- Anker, S.D.; Friede, T.; von Bardeleben, R.-S.; Butler, J.; Khan, M.-S.; Diek, M.; Heinrich, J.; Geyer, M.; Placzek, M.; Ferrari, R.; et al. Transcatheter Valve Repair in Heart Failure with Moderate to Severe Mitral Regurgitation. N. Engl. J. Med. 2024, 391, 1799–1809. [Google Scholar] [CrossRef] [PubMed]
- Baldus, S.; Doenst, T.; Pfister, R.; Gummert, J.; Kessler, M.; Boekstegers, P.; Lubos, E.; Schröder, J.; Thiele, H.; Walther, T.; et al. Transcatheter Repair versus Mitral-Valve Surgery for Secondary Mitral Regurgitation. N. Engl. J. Med. 2024, 391, 1787–1798. [Google Scholar] [CrossRef]
- Armoiry, X.; Obadia, J.-F.; Auguste, P.; Connock, M. Conflicting Findings between the Mitra-Fr and the Coapt Trials: Implications Regarding the Cost-Effectiveness of Percutaneous Repair for Heart Failure Patients with Severe Secondary Mitral Regurgitation. PLoS ONE 2020, 15, e0241361. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.-H.; Chon, M.-K.; Lederman, R.J.; Sung, S.-C.; Je, H.-G.; Choo, K.-S.; Lee, S.-H.; Shin, E.-S.; Kim, J.-S.; Hwang, K.-W.; et al. Mitral Loop Cerclage Annuloplasty for Secondary Mitral Regurgitation: First Human Results. JACC Cardiovasc. Interv. 2017, 10, 597–610. [Google Scholar] [CrossRef]
- Messika-Zeitoun, D.; Nickenig, G.; Latib, A.; Kuck, K.-H.; Baldus, S.; Schueler, R.; La Canna, G.; Agricola, E.; Kreidel, F.; Huntgeburth, M.; et al. Transcatheter Mitral Valve Repair for Functional Mitral Regurgitation Using the Cardioband System: 1 Year Outcomes. Eur. Heart J. 2019, 40, 466–472. [Google Scholar] [CrossRef]
- Siminiak, T.; Hoppe, U.C.; Schofer, J.; Haude, M.; Herrman, J.-P.; Vainer, J.; Firek, L.; Reuter, D.G.; Goldberg, S.L.; Van Bibber, R. Effectiveness and Safety of Percutaneous Coronary Sinus-Based Mitral Valve Repair in Patients With Dilated Cardiomyopathy (from the AMADEUS Trial). Am. J. Cardiol. 2009, 104, 565–570. [Google Scholar] [CrossRef]
- Lipiecki, J.; Siminiak, T.; Sievert, H.; Müller-Ehmsen, J.; Degen, H.; Wu, J.C.; Schandrin, C.; Kalmucki, P.; Hofmann, I.; Reuter, D.; et al. Coronary Sinus-Based Percutaneous Annuloplasty as Treatment for Functional Mitral Regurgitation: The TITAN II Trial. Open Heart 2016, 3, e000411. [Google Scholar] [CrossRef][Green Version]
- Goldberg, S.L.; Lipiecki, J.; Sievert, H. The CARILLON Mitral Contour Transcatheter Indirect Mitral Valve Annuloplasty System. EuroIntervention 2015, 11, W64–W66. [Google Scholar] [CrossRef]
- Goldberg, S.L.; Meredith, I.; Marwick, T.; Haluska, B.A.; Lipiecki, J.; Siminiak, T.; Mehta, N.; Kaye, D.M.; Sievert, H. A Randomized Double-Blind Trial of an Interventional Device Treatment of Functional Mitral Regurgitation in Patients with Symptomatic Congestive Heart Failure—Trial Design of the REDUCE FMR Study. Am. Heart J. 2017, 188, 167–174. [Google Scholar] [CrossRef] [PubMed]
- Maisano, F.; Taramasso, M. The Cardioband Transcatheter Direct Mitral Valve Annuloplasty System. EuroIntervention 2015, 11, W58–W59. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bapat, V.; Rajagopal, V.; Meduri, C.; Farivar, R.S.; Walton, A.; Duffy, S.J.; Gooley, R.; Almeida, A.; Reardon, M.J.; Kleiman, N.S.; et al. Early Experience With New Transcatheter Mitral Valve Replacement. J. Am. Coll. Cardiol. 2018, 71, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Zahr, F.; Song, H.K.; Chadderdon, S.M.; Gada, H.; Mumtaz, M.; Byrne, T.; Kirshner, M.; Bajwa, T.; Weiss, E.; Kodali, S.; et al. 30-Day Outcomes Following Transfemoral Transseptal Transcatheter Mitral Valve Replacement: Intrepid TMVR Early Feasibility Study Results. JACC Cardiovasc. Interv. 2022, 15, 80–89. [Google Scholar] [CrossRef]
- Alkhouli, M.; Guerrero, M.; Rihal, C.S. Transseptal TMVR: An Intrepid Journey. JACC Cardiovasc. Interv. 2022, 15, 90–92. [Google Scholar] [CrossRef]
- Rodés-Cabau, J. Transcatheter Mitral Valve Replacement: First Steps on a Long Road. J. Am. Coll. Cardiol. 2018, 71, 22–24. [Google Scholar] [CrossRef]
- Rogers, J.H.; Thomas, M.; Morice, M.-C.; Narbute, I.; Zabunova, M.; Hovasse, T.; Poupineau, M.; Rudzitis, A.; Kamzola, G.; Zvaigzne, L.; et al. Treatment of Heart Failure with Associated Functional Mitral Regurgitation Using the ARTO System: Initial Results of the First-in-Human MAVERIC Trial (Mitral Valve Repair Clinical Trial). JACC Cardiovasc. Interv. 2015, 8, 1095–1104. [Google Scholar] [CrossRef]
- Patterson, T.; Gregson, J.; Erglis, A.; Joseph, J.; Rajani, R.; Wilson, K.; Prendergast, B.; Worthley, S.; Hildick-Smith, D.; Rafter, T.; et al. Two-Year Outcomes from the MitrAl ValvE RepaIr Clinical (MAVERIC) Trial: A Novel Percutaneous Treatment of Functional Mitral Regurgitation. Eur. J. Heart Fail. 2021, 23, 1775–1783. [Google Scholar] [CrossRef]
- Senni, M.; Adamo, M.; Metra, M.; Alfieri, O.; Vahanian, A. Treatment of Functional Mitral Regurgitation in Chronic Heart Failure: Can We Get a ‘Proof of Concept’ from the MITRA-FR and COAPT Trials? Eur. J. Heart Fail. 2019, 21, 852–861. [Google Scholar] [CrossRef]
- Ponikowski, P.; Friede, T.; von Bardeleben, R.S.; Butler, J.; Shahzeb Khan, M.; Diek, M.; Heinrich, J.; Geyer, M.; Placzek, M.; Ferrari, R.; et al. Hospitalization of Symptomatic Patients With Heart Failure and Moderate to Severe Functional Mitral Regurgitation Treated With MitraClip: Insights from RESHAPE-HF2. J. Am. Coll. Cardiol. 2024, 84, 2347–2363. [Google Scholar] [CrossRef]
- Anker, M.S.; Porthun, J.; Bonnet, G.; Schulze, P.C.; Rassaf, T.; Landmesser, U. Percutaneous Transcatheter Edge-to-Edge Repair for Functional Mitral Regurgitation in Heart Failure: A Meta-Analysis of 3 Randomized Controlled Trials. J. Am. Coll. Cardiol. 2024, 84, 2364–2368. [Google Scholar] [CrossRef] [PubMed]
- Lancellotti, P.; Sugimoto, T.; Bäck, M. Revisiting Secondary Mitral Regurgitation Threshold Severity: Insights and Lessons from the RESHAPE-HF2 Trial. Eur. Heart J. Open 2024, 4, oeae084. [Google Scholar] [CrossRef]
- Bonow, R.O.; Carabello, B.A.; Chatterjee, K.; de Leon, A.C.; Faxon, D.P.; Freed, M.D.; Gaasch, W.H.; Lytle, B.W.; Nishimura, R.A.; O’Gara, P.T.; et al. ACC/AHA 2006 Guidelines for the Management of Patients With Valvular Heart Disease. Circulation 2006, 114, e84–e231. [Google Scholar] [CrossRef] [PubMed]
- Members, A.F.; Vahanian, A.; Alfieri, O.; Andreotti, F.; Antunes, M.J.; Barón-Esquivias, G.; Baumgartner, H.; Borger, M.A.; Carrel, T.P.; De Bonis, M.; et al. Guidelines on the Management of Valvular Heart Disease (Version 2012): The Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2012, 33, 2451–2496. [Google Scholar] [CrossRef]
- Pibarot, P.; Delgado, V.; Bax, J.J. MITRA-FR vs. COAPT: Lessons from Two Trials with Diametrically Opposed Results. Eur. Heart J. Cardiovasc. Imaging 2019, 20, 620–624. [Google Scholar] [CrossRef] [PubMed]
- Atianzar, K.; Zhang, M.; Newhart, Z.; Gafoor, S. Why Did COAPT Win While MITRA-FR Failed? Defining the Appropriate Patient Population for MitraClip. Interv. Cardiol. 2019, 14, 45–47. [Google Scholar] [CrossRef]
- Mauricio, R.; Kumbhani, D.J. MitraClip: How Do We Reconcile the Inconsistent Findings of MITRA-FR and COAPT? Curr. Cardiol. Rep. 2019, 21, 150. [Google Scholar] [CrossRef]
- Betz, J.; Lilly, S.M.; Abraham, W.T. Managing Mitral Regurgitation in Heart Failure-Perspectives After COAPT. Curr. Treat. Options Cardiovasc. Med. 2019, 21, 86. [Google Scholar] [CrossRef]
- Grayburn, P.A.; Sannino, A.; Packer, M. Proportionate and Disproportionate Functional Mitral Regurgitation: A New Conceptual Framework That Reconciles the Results of the MITRA-FR and COAPT Trials. JACC Cardiovasc. Imaging 2019, 12, 353–362. [Google Scholar] [CrossRef]
- Packer, M.; Grayburn, P.A. Contrasting Effects of Pharmacological, Procedural, and Surgical Interventions on Proportionate and Disproportionate Functional Mitral Regurgitation in Chronic Heart Failure. Circulation 2019, 140, 779–789. [Google Scholar] [CrossRef]
- Gupta, A.; Packer, M.; Makkar, R.; Grayburn, P. A Volume-Based Framework Reconciling COAPT, MITRA-FR, and RESHAPE-HF2. J. Am. Coll. Cardiol. 2024, 84, 2376–2379. [Google Scholar] [CrossRef] [PubMed]
- Orban, M.; Karam, N.; Lubos, E.; Kalbacher, D.; Braun, D.; Deseive, S.; Neuss, M.; Butter, C.; Praz, F.; Kassar, M.; et al. Impact of Proportionality of Secondary Mitral Regurgitation on Outcome After Transcatheter Mitral Valve Repair. JACC Cardiovasc. Imaging 2021, 14, 715–725. [Google Scholar] [CrossRef]
- Lindenfeld, J.; Abraham, W.T.; Grayburn, P.A.; Kar, S.; Asch, F.M.; Lim, D.S.; Nie, H.; Singhal, P.; Sundareswaran, K.S.; Weissman, N.J.; et al. Association of Effective Regurgitation Orifice Area to Left Ventricular End-Diastolic Volume Ratio With Transcatheter Mitral Valve Repair Outcomes: A Secondary Analysis of the COAPT Trial. JAMA Cardiol. 2021, 6, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Messika-Zeitoun, D.; Iung, B.; Armoiry, X.; Trochu, J.-N.; Donal, E.; Habib, G.; Brochet, E.; Thibault, H.; Piriou, N.; Cormier, B.; et al. Impact of Mitral Regurgitation Severity and Left Ventricular Remodeling on Outcome After MitraClip Implantation: Results From the Mitra-FR Trial. JACC Cardiovasc. Imaging 2021, 14, 742–752. [Google Scholar] [CrossRef]
- Moonen, A.; Cao, J.; Celermajer, D.S.; Ng, M.K.C. Mitral Regurgitation “Proportionality” in Functional Mitral Regurgitation and Outcomes After Mitral Valve Transcatheter Edge-to-Edge Repair: A Systematic Review and Meta-Analysis. Struct. Heart 2024, 8, 100284. [Google Scholar] [CrossRef]
- Cimino, S.; Agati, L.; Filomena, D.; Maestrini, V.; Monosilio, S.; Birtolo, L.I.; Mocci, M.; Mancone, M.; Sardella, G.; Grayburn, P.; et al. 3D Echo Characterization of Proportionate and Disproportionate Functional Mitral Regurgitation before and after Percutaneous Mitral Valve Repair. J. Clin. Med. 2022, 11, 645. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, H.; Falk, V.; Bax, J.J.; De Bonis, M.; Hamm, C.; Holm, P.J.; Iung, B.; Lancellotti, P.; Lansac, E.; Rodriguez Muñoz, D.; et al. 2017 ESC/EACTS Guidelines for the Management of Valvular Heart Disease. Eur. Heart J. 2017, 38, 2739–2791. [Google Scholar] [CrossRef]
- Nishimura, R.A.; Otto, C.M.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P.; Guyton, R.A.; O’Gara, P.T.; Ruiz, C.E.; Skubas, N.J.; Sorajja, P.; et al. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary. Circulation 2014, 129, 2440–2492. [Google Scholar] [CrossRef]
- Bartko, P.E.; Arfsten, H.; Heitzinger, G.; Pavo, N.; Toma, A.; Strunk, G.; Hengstenberg, C.; Hülsmann, M.; Goliasch, G. A Unifying Concept for the Quantitative Assessment of Secondary Mitral Regurgitation. J. Am. Coll. Cardiol. 2019, 73, 2506–2517. [Google Scholar] [CrossRef]
- Grayburn, P.A.; Carabello, B.; Hung, J.; Gillam, L.D.; Liang, D.; Mack, M.J.; McCarthy, P.M.; Miller, D.C.; Trento, A.; Siegel, R.J. Defining “Severe” Secondary Mitral Regurgitation: Emphasizing an Integrated Approach. J. Am. Coll. Cardiol. 2014, 64, 2792–2801. [Google Scholar] [CrossRef]
- Zoghbi, W.A.; Adams, D.; Bonow, R.O.; Enriquez-Sarano, M.; Foster, E.; Grayburn, P.A.; Hahn, R.T.; Han, Y.; Hung, J.; Lang, R.M.; et al. Recommendations for Noninvasive Evaluation of Native Valvular Regurgitation: A Report from the American Society of Echocardiography Developed in Collaboration with the Society for Cardiovascular Magnetic Resonance. J. Am. Soc. Echocardiogr. 2017, 30, 303–371. [Google Scholar] [CrossRef] [PubMed]
- Vahanian, A.; Beyersdorf, F.; Praz, F.; Milojevic, M.; Baldus, S.; Bauersachs, J.; Capodanno, D.; Conradi, L.; De Bonis, M.; De Paulis, R.; et al. 2021 ESC/EACTS Guidelines for the Management of Valvular Heart Disease: Developed by the Task Force for the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2022, 43, 561–632. [Google Scholar] [CrossRef]
- Bartko, P.E.; Heitzinger, G.; Spinka, G.; Pavo, N.; Prausmüller, S.; Kastl, S.; Winter, M.-P.; Arfsten, H.; Tan, T.C.; Gebhard, C.; et al. Principal Morphomic and Functional Components of Secondary Mitral Regurgitation. JACC Cardiovasc. Imaging 2021, 14, 2288–2300. [Google Scholar] [CrossRef]
- Gaasch, W.H.; Meyer, T.E. Secondary Mitral Regurgitation (Part 1): Volumetric Quantification and Analysis. Heart 2018, 104, 634. [Google Scholar] [CrossRef]
- Grayburn, P.A.; Weissman, N.J.; Zamorano, J.L. Quantitation of Mitral Regurgitation. Circulation 2012, 126, 2005–2017. [Google Scholar] [CrossRef] [PubMed]
- Grayburn, P.A.; Appleton, C.P.; DeMaria, A.N.; Greenberg, B.; Lowes, B.; Oh, J.; Plehn, J.F.; Rahko, P.; Sutton, M.S.J.; Eichhorn, E.J. Echocardiographic Predictors of Morbidity and Mortality in Patients with Advanced Heart Failure: The Beta-Blocker Evaluation of Survival Trial (BEST). J. Am. Coll. Cardiol. 2005, 45, 1064–1071. [Google Scholar] [CrossRef]
- Bohra, C.; Asch, F.M.; Lerakis, S.; Little, S.H.; Redfors, B.; Zhou, Z.; Li, Y.; Weissman, N.J.; Grayburn, P.A.; Kar, S.; et al. Pulmonary Vein Systolic Flow Reversal and Outcomes in Patients From the Cardiovascular Outcomes Assessment of the MitraClip Percutaneous Therapy for Heart Failure Patients With Functional Mitral Regurgitation (COAPT) Trial. Struct. Heart 2024, 8, 100333. [Google Scholar] [CrossRef] [PubMed]
- Karam, N.; Stolz, L.; Orban, M.; Deseive, S.; Praz, F.; Kalbacher, D.; Westermann, D.; Braun, D.; Näbauer, M.; Neuss, M.; et al. Impact of Right Ventricular Dysfunction on Outcomes After Transcatheter Edge-to-Edge Repair for Secondary Mitral Regurgitation. JACC Cardiovasc. Imaging 2021, 14, 768–778. [Google Scholar] [CrossRef]
- Doldi, P.M.; Stolz, L.; Kalbacher, D.; Köll, B.; Geyer, M.; Ludwig, S.; Orban, M.; Braun, D.; Weckbach, L.T.; Stocker, T.J.; et al. Right Ventricular Dysfunction Predicts Outcome after Transcatheter Mitral Valve Repair for Primary Mitral Valve Regurgitation. Eur. J. Heart Fail. 2022, 24, 2162–2171. [Google Scholar] [CrossRef]
- Brener, M.I.; Grayburn, P.; Lindenfeld, J.; Burkhoff, D.; Liu, M.; Zhou, Z.; Alu, M.C.; Medvedofsky, D.A.; Asch, F.M.; Weissman, N.J.; et al. Right Ventricular–Pulmonary Arterial Coupling in Patients With HF Secondary MR: Analysis from the COAPT Trial. JACC Cardiovasc. Interv. 2021, 14, 2231–2242. [Google Scholar] [CrossRef]
- Blanco, P. Rationale for Using the Velocity–Time Integral and the Minute Distance for Assessing the Stroke Volume and Cardiac Output in Point-of-Care Settings. Ultrasound J. 2020, 12, 21. [Google Scholar] [CrossRef]
- Dujardin, K.S.; Enriquez-Sarano, M.; Bailey, K.R.; Nishimura, R.A.; Seward, J.B.; Tajik, A.J. Grading of Mitral Regurgitation by Quantitative Doppler Echocardiography. Circulation 1997, 96, 3409–3415. [Google Scholar] [CrossRef] [PubMed]
- Grigioni, F.; Enriquez-Sarano, M.; Zehr, K.J.; Bailey, K.R.; Tajik, A.J. Ischemic Mitral Regurgitation. Circulation 2001, 103, 1759–1764. [Google Scholar] [CrossRef]
- Huang, A.L.; Dal-Bianco, J.P.; Levine, R.A.; Hung, J.W. Secondary Mitral Regurgitation: Cardiac Remodeling, Diagnosis, and Management. Struct. Heart 2023, 7, 100129. [Google Scholar] [CrossRef]
- Igata, S.; Cotter, B.R.; Hang, C.T.; Morikawa, N.; Strachan, M.; Raisinghani, A.; Blanchard, D.G.; Demaria, A.N. Optimal Quantification of Functional Mitral Regurgitation: Comparison of Volumetric and Proximal Isovelocity Surface Area Methods to Predict Outcome. J. Am. Heart Assoc. Cardiovasc. Cerebrovasc. Dis. 2021, 10, 18553. [Google Scholar] [CrossRef] [PubMed]
- Smer, A.; Nanda, N.C.; Akdogan, R.E.; Elmarzouky, Z.M.; Dulal, S. Echocardiographic Evaluation of Mitral Valve Regurgitation. Mini-invasive Surg. 2020, 4, 52. [Google Scholar] [CrossRef]
- Uretsky, S.; Argulian, E.; Narula, J.; Wolff, S.D. Use of Cardiac Magnetic Resonance Imaging in Assessing Mitral Regurgitation: Current Evidence. J. Am. Coll. Cardiol. 2018, 71, 547–563. [Google Scholar] [CrossRef]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2015, 28, 1–39.e14. [Google Scholar] [CrossRef]
- Sonaglioni, A.; Nicolosi, G.L.; Rigamonti, E.; Lombardo, M. Impact of Chest Wall Conformation on the Outcome of Primary Mitral Regurgitation Due to Mitral Valve Prolapse. J. Cardiovasc. Echogr. 2022, 32, 29–37. [Google Scholar] [CrossRef]
- Bilbija, I.; Matkovic, M.; Cubrilo, M.; Aleksic, N.; Milin Lazovic, J.; Cumic, J.; Tutus, V.; Jovanovic, M.; Putnik, S. The Prospects of Secondary Moderate Mitral Regurgitation after Aortic Valve Replacement—Meta-Analysis. Int. J. Environ. Res. Public Heal. 2020, 17, 7335. [Google Scholar] [CrossRef]
- Unger, P.; Magne, J.; Eynden, F.V.; Plein, D.; Van Camp, G.; Pasquet, A.; Cosyns, B.; Dedobbeleer, C.; Lancellotti, P. Impact of Prosthesis–Patient Mismatch on Mitral Regurgitation after Aortic Valve Replacement. Heart 2010, 96, 1627–1632. [Google Scholar] [CrossRef]
- Dabic, P.; Vucurevic, B.; Sevkovic, M.; Andric, D.; Pesic, S.; Neskovic, M.; Borovic, S.; Petrovic, J. Functional Mitral Regurgitation Post-Isolated Aortic Valve Replacement. J. Clin. Med. 2024, 13, 6971. [Google Scholar] [CrossRef] [PubMed]
- Hu, R.; Chen, T. Leaning Too Much on the Power of Proximal Isovelocity Surface Area? Don’t Forget the Volumetric Method for Quantifying Functional Mitral Regurgitation. J. Am. Heart Assoc. 2021, 10, e021914. [Google Scholar] [CrossRef]
- Harm, T.; Schwarz, F.-J.; Zdanyte, M.; Goldschmied, A.; Baas, L.; Aidery, P.; Shcherbyna, S.; Toskas, I.; Keller, T.; Kast, I.; et al. Novel 3-Dimensional Effective Regurgitation Orifice Area Quantification Serves as a Reliable Tool to Identify Severe Mitral Valve Regurgitation. Sci. Rep. 2024, 14, 22067. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Heo, R.; Hong, G.-R.; Chang, H.-J.; Sung, J.M.; Shin, S.H.; Cho, I.J.; Shim, C.-Y.; Chung, N. Differential Effect of 3-Dimensional Color Doppler Echocardiography for the Quantification of Mitral Regurgitation According to the Severity and Characteristics. Circ. Cardiovasc. Imaging 2014, 7, 535–544. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Heo, R.; Son, J.-W.; ó Hartaigh, B.; Chang, H.-J.; Kim, Y.-J.; Datta, S.; Cho, I.-J.; Shim, C.Y.; Hong, G.-R.; Ha, J.-W.; et al. Clinical Implications of Three-Dimensional Real-Time Color Doppler Transthoracic Echocardiography in Quantifying Mitral Regurgitation: A Comparison with Conventional Two-Dimensional Methods. J. Am. Soc. Echocardiogr. 2017, 30, 393–403.e7. [Google Scholar] [CrossRef]
- Sköldborg, V.; Madsen, P.L.; Dalsgaard, M.; Abdulla, J. Quantification of Mitral Valve Regurgitation by 2D and 3D Echocardiography Compared with Cardiac Magnetic Resonance a Systematic Review and Meta-Analysis. Int. J. Cardiovasc. Imaging 2020, 36, 279–289. [Google Scholar] [CrossRef]
- Garg, P.; Pavon, A.G.; Penicka, M.; Uretsky, S. Cardiovascular Magnetic Resonance Imaging in Mitral Valve Disease. Eur. Heart J. 2024, 46, ehae801. [Google Scholar] [CrossRef]
- Garg, P.; Swift, A.J.; Zhong, L.; Carlhäll, C.J.; Ebbers, T.; Westenberg, J.; Hope, M.D.; Bucciarelli-Ducci, C.; Bax, J.J.; Myerson, S.G. Assessment of Mitral Valve Regurgitation by Cardiovascular Magnetic Resonance Imaging. Nat. Rev. Cardiol. 2019, 17, 298–312. [Google Scholar] [CrossRef]
- Tayal, B.; Debs, D.; Nabi, F.; Malahfji, M.; Little, S.H.; Reardon, M.; Zoghbi, W.; Kleiman, N.; Shah, D.J. Impact of Myocardial Scar on Prognostic Implication of Secondary Mitral Regurgitation in Heart Failure. JACC Cardiovasc. Imaging 2021, 14, 812–822. [Google Scholar] [CrossRef]
- Myerson, S.G.; D’Arcy, J.; Christiansen, J.P.; Dobson, L.E.; Mohiaddin, R.; Francis, J.M.; Prendergast, B.; Greenwood, J.P.; Karamitsos, T.D.; Neubauer, S. Determination of Clinical Outcome in Mitral Regurgitation With Cardiovascular Magnetic Resonance Quantification. Circulation 2016, 133, 2287–2296. [Google Scholar] [CrossRef] [PubMed]
- Penicka, M.; Vecera, J.; Mirica, D.C.; Kotrc, M.; Kockova, R.; Van Camp, G. Prognostic Implications of Magnetic Resonance-Derived Quantification in Asymptomatic Patients with Organic Mitral Regurgitation: Comparison with Doppler Echocardiography-Derived Integrative Approach. Circulation 2018, 137, 1349–1360. [Google Scholar] [CrossRef] [PubMed]
- Uretsky, S.; Gillam, L.; Lang, R.; Chaudhry, F.A.; Argulian, E.; Supariwala, A.; Gurram, S.; Jain, K.; Subero, M.; Jang, J.J.; et al. Discordance Between Echocardiography and MRI in the Assessment of Mitral Regurgitation Severity: A Prospective Multicenter Trial. J. Am. Coll. Cardiol. 2015, 65, 1078–1088. [Google Scholar] [CrossRef]
- Suinesiaputra, A.; Bluemke, D.A.; Cowan, B.R.; Friedrich, M.G.; Kramer, C.M.; Kwong, R.; Plein, S.; Schulz-Menger, J.; Westenberg, J.J.M.; Young, A.A.; et al. Quantification of LV Function and Mass by Cardiovascular Magnetic Resonance: Multi-Center Variability and Consensus Contours. J. Cardiovasc. Magn. Reson. 2015, 17, 63. [Google Scholar] [CrossRef]
- Cavalcante, J.L.; Lopes, B.B.C. Left Ventricular Scar Burden as a Modulator of Risk in Functional Mitral Regurgitation. JACC Cardiovasc. Imaging 2021, 14, 823–825. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.K.M.; Kocyigit, D.; Choi, H.; Anthony, C.M.; Chan, N.; Bullen, J.; Popović, Z.B.; Kapadia, S.R.; Krishnaswamy, A.; Griffin, B.P.; et al. Prognostic Power of Quantitative Assessment of Functional Mitral Regurgitation and Myocardial Scar Quantification by Cardiac Magnetic Resonance. Circ. Cardiovasc. Imaging 2023, 16, e015134. [Google Scholar] [CrossRef]
- Ivanov, A.; Bhumireddy, G.P.; Dabiesingh, D.S.; Khan, S.A.; Ho, J.; Krishna, N.; Dontineni, N.; Socolow, J.A.; Briggs, W.M.; Klem, I.; et al. Importance of Papillary Muscle Infarction Detected by Cardiac Magnetic Resonance Imaging in Predicting Cardiovascular Events. Int. J. Cardiol. 2016, 220, 558–563. [Google Scholar] [CrossRef]
- Ikeda, Y.; Inomata, T.; Fujita, T.; Iida, Y.; Nabeta, T.; Ishii, S.; Maekawa, E.; Yanagisawa, T.; Mizutani, T.; Naruke, T.; et al. Cardiac Fibrosis Detected by Magnetic Resonance Imaging on Predicting Time Course Diversity of Left Ventricular Reverse Remodeling in Patients with Idiopathic Dilated Cardiomyopathy. Heart Vessels 2016, 31, 1817–1825. [Google Scholar] [CrossRef]
- Zoghbi, W.A.; Asch, F.M.; Bruce, C.; Gillam, L.D.; Grayburn, P.A.; Hahn, R.T.; Inglessis, I.; Islam, A.M.; Lerakis, S.; Little, S.H.; et al. Guidelines for the Evaluation of Valvular Regurgitation After Percutaneous Valve Repair or Replacement: A Report from the American Society of Echocardiography Developed in Collaboration with the Society for Cardiovascular Angiography and Interventions, Japanese Society of Echocardiography, and Society for Cardiovascular Magnetic Resonance. J. Am. Soc. Echocardiogr. 2019, 32, 431–475. [Google Scholar] [CrossRef]
- Trenkwalder, T.; Lachmann, M.; Stolz, L.; Fortmeier, V.; Covarrubias, H.A.A.; Rippen, E.; Schürmann, F.; Presch, A.; von Scheidt, M.; Ruff, C.; et al. Machine Learning Identifies Pathophysiologically and Prognostically Informative Phenotypes among Patients with Mitral Regurgitation Undergoing Transcatheter Edge-to-Edge Repair. Eur. Heart J. Cardiovasc. Imaging 2023, 24, 574–587. [Google Scholar] [CrossRef]
- D’Ascenzo, F.; Angelini, F.; Pancotti, C.; Bocchino, P.P.; Giannini, C.; Finizio, F.; Adamo, M.; Camman, V.; Morici, N.; Perl, L.; et al. Machine-Learning Phenotyping of Patients with Functional Mitral Regurgitation Undergoing Transcatheter Edge-to-Edge Repair: The MITRA-AI Study. Eur. Hearh J. Digit. Health 2025, 6, ztaf006. [Google Scholar] [CrossRef] [PubMed]
- Hausleiter, J.; Lachmann, M.; Stolz, L.; Bedogni, F.; Rubbio, A.P.; Estévez-Loureiro, R.; Raposeiras-Roubin, S.; Boekstegers, P.; Karam, N.; Rudolph, V. Artificial Intelligence-Derived Risk Score for Mortality in Secondary Mitral Regurgitation Treated by Transcatheter Edge-to-Edge Repair: The EuroSMR Risk Score. Eur. Heart J. 2024, 45, 922–936. [Google Scholar] [CrossRef] [PubMed]
| M-TEER Trials | |||||
|---|---|---|---|---|---|
| Study Name (Years of Inclusion) | Design | Number of Patients | Comparison | Primary Endpoints | Conclusions |
| EVEREST II (2005–2008) | Multicenter RCT | 279 | M-TEER versus MV surgical repair or replacement in primary MR | Primary efficacy: composite of freedom from death, from surgery for MV dysfunction, and from grade 3+ or 4+ at 12 months; primary safety: composite of major adverse events within 30 days after procedure | M-TEER has a superior safety profile and comparable symptomatic improvement, but was less efficacious than MV surgery; M-TEER patients who were event free during the 1st year had more comparable efficacy outcomes to the MV surgery patients |
| TRAMI (2010–2013) | Prospective, Single Arm, Multicenter | 722 | Abbott MitraClip | Long-term mortality rates, cardiac rehospitalization, and reintervention | M-TEER demonstrated efficacy, improved functional status, and low re-intervention rates at 4 years; mortality was similar for ischemic and non-ischemic sMR |
| MITRA-FR (2013–2017) | Multicenter RCT | 304 | M-TEER + GDMT versus GDMT in sMR | Composite of death from any cause or unplanned HF hospitalization at 12 months | M-TEER did not demonstrate improvement in death or heart failure hospitalization |
| COAPT (2012–2017) | Multicenter RCT | 614 | M-TEER + GDMT versus GDMT in sMR | Primary efficacy endpoint: HF hospitalizations within 24 months; primary safety endpoint: freedom from device-related complications at 12 months | M-TEER demonstrated improvement in cardiovascular death, heart failure hospitalization, and symptoms at trial end and at 5 years |
| MITRA CRT (2015–2019) | Single Center RCT | 31 | M-TEER versus GDMT in ‘nonresponder’ patients with dilated cardiomyopathy + CRT + GDMT | Combination of CV death, heart transplantation, or HF hospitalization at 12 months | M-TEER demonstrated a reduction in the combined endpoint of CV death, heart transplantation, and HF hospitalizations |
| EURO SMR (2008–2020) | Multicenter, Retrospective registry | 1628 | M-TEER | MR severity, functional capacity, survival, and predictors of all-cause mortality | M-TEER is associated with long-term reduction in MR severity but the 5-year survival rate in this real-world registry was lower than that observed in the COAPT trial |
| COAPT-PAS (2019–2020) | Prospective, Single Arm, Multicenter | 5000 | Abbott MitraClip for sMR | Procedure success, MR severity, quality of life, HF hospitalization | High procedural success rates were demonstrated with COAPT-like and MITRA-FR like subgroups having lower hospitalizations at 1 year as compared to that of the COAPT and MITRA-FR RCTs, respectively |
| EXPAND (2018–2019) | Prospective, Single Arm, Multicenter | 1041 | Abbott MitraClip NTR or XTR Third Generation System | MR severity, functional capacity, quality of life, HF hospitalization, all-cause mortality | M-TEER demonstrated a greater degree of MR reduction as compared to EVERST II and COAPT |
| EXPAND G4 (2020–2022) | Prospective, Single Arm, Multicenter | 1164 | Abbott MitraClip Fourth Generation System | MR severity, functional capacity, quality of life, heart failure hospitalization, all-cause mortality | Fourth Generation M-TEER was demonstrated to be safe and effective with improvement in quality of life |
| MATTERHORN (2015–2022) | Multicenter RCT | 210 | M-TEER + GDMT versus surgical mitral valve repair or replacement + GDMT in sMR | Primary efficacy endpoint: composite of death, hospitalization for heart failure, MV reintervention, implantation of assist device, or stroke within 1 year after procedure; primary safety endpoint: composite of major adverse events within 30 days after the procedure | M-TEER is noninferior to mitral valve surgery in regard to efficacy, and had a superior safety profile within and after the periprocedural period |
| RESHAPE-HF2 (2017–2023) | Multicenter RCT | 505 | M-TEER + GDMT versus GDMT in sMR | Composite of first or recurrent hospitalization for heart failure or cardiovascular death during 24 months; rate of first or recurrent hospitalization for heart failure during 24 months; change from baseline to 12 months for quality of life | M-TEER demonstrated improvement in heart failure hospitalization and symptoms |
| CLASP IID (2018–2019) | Multicenter RCT | 300 | Abbot MitraClip versus Edwards PASCAL in primary MR | Primary efficacy: MR severity at 6 months; primary safety: adverse events within 30 days | Edwards PASCAL demonstrated noninferiority to Abbott MitraClip |
| miCLASP (2019–2024) | Prospective, Single Arm, Multicenter | 544 | Edwards PASCAL | Primary efficacy endpoint: MR severity; primary safety endpoint: major adverse event within 30 days | M-TEER demonstrated safety and efficacy with reduction in MR, hospitalization, and symptoms |
| Other Percutaneous Treatments for sMR | |||||
| Transcatheter mitral loop cerclage (2015–2016) | Prospective, Single Arm, Single Center | 5 | Mitral Loop Cerclage Annuloplasty for sMR | MR severity and chamber dimensions over 6 months | Procedural success in 4 out of 5 patients with reverse remodeling and electrical remodeling |
| Cardioband (2013–2016) | Prospective, Single Arm, Multicenter | 60 | Edwards Lifesciences Cardioband for sMR | MR severity, survival, and functional capacity at 1 year | Cardioband demonstrated improvement in MR and functional capacity |
| Intrepid TMVR (2015–2017) | Prospective Single Arm, Multicenter | 50 | Transcatheter Mitral Valve Replacement for sMR | Procedural success, MR severity, and symptoms improvement | TMVR is feasible in high or extreme risk patients; APOLLO RCT comparing TMVR to m-TEER is ongoing |
| MAVERIC (2013–2017) | Prospective, Single Arm, Multicenter | 45 | ARTO System (transcatheter annular reduction device) for sMR | Primary efficacy: MR reduction at 30 days; primary safety: adverse event within 30 days after procedure | ARTO System is safe and had sustained efficacy with reduction in MR, LVEDV, and heart failure hospitalizations at 2 years |
| REDUCE-FMR (2014–2018) | Multicenter RCT | 120 | Carillion Mitral Contour System (coronary-sinus-based percutaneous annuloplasty) +GDMT vs. GDMT for sMR | MR severity at 12 months | The Carrilion device significantly reduced sMR as compared to GDMT |
| Comparison of Trial Design of Major m-TEER RCTs | |||
|---|---|---|---|
| Inclusion Criteria | COAPT | MITRA-FR | RESHAPE-HF2 |
| MR Severity | At least moderate to severe | At least moderate to severe | MR Severity |
| Definition for moderate to severe (3+) MR | EROA > 30 mm2 and/or RVol > 45 mL (As per ACC/AHA 2006/2008 Guideline) | EROA > 20 mm2 and/or RVol > 30 mL (As per ESC/EACT 2012 Guidelines) | EROA > 30 mm2 and/or RVol > 45 mL (As per EACVI 2012 Guidelines) |
| NYHA Stage | II, III, IVa (ambulatory) | II, III, or IV | II, III, IV |
| LV EF (%) | 15–40 | 20–50 | 15–35 if NYHA II, 15–45 if NYHA III or IV |
| GDMT at baseline | Uptitrated to maximum dose, stable dosage, CRT if eligible | Variable GDMT adjustment, ‘real world’ practice | Uptitrated to maximum dose, stable dosage, CRT if eligible |
| Exclusion Criteria | |||
| LV end systolic dimension (mm) | >70 mm | - | - |
| Primary Endpoint(s) | Primary efficacy: HF hospitalization within 24 months | Composite rate of all-cause mortality or HF hospitalization at 12 months | Composite rate of recurrent HF hospitalizations and cardiovascular death within 24 months |
| Primary safety: Freedom from device related complications at 12 months | - | HF hospitalizations within 24 months | |
| - | - | Change in KCCQ score at 12 months | |
| Comparison of Clinical Characteristics | |||
| Clinical Characteristics (Average) | COAPT (n = 614) | MITRA-FR (n = 304) | RESHAPE-HF2 (n = 505) |
| ACEI, ARB, or ARNI (% of total) | 67% | - | 82% |
| ACEI or ARB | - | 74% | 74% |
| Beta Blocker (% of total) | 90% | 90% | 96% |
| Diuretics (% of total) | 89% | 99% | 95% |
| MRA (% of total) | 50.2% | 54.6% | 82.4% |
| SGLT-2 Inhibitor (% of total) | - | - | 9% |
| Previous ICD (% of total) | 31.3% | 34.5% | 35.2% |
| Previous CRT (% of total) | 36.5% | 26.6% | 29.1% |
| Previous PCI (% of total) | 48.2% | 46.1% | 44.4% |
| Previous CABG (% of total) | 26.3% | 40.2% | - |
| EROA (mm2) | 41 ± 15 | 31 ± 15 | 25 |
| LV end-diastolic volume (mL) | 194 | 252 | 211 |
| LVEF (%) | 31 ± 9 | 33 ± 6 | 31 ± 8 |
| eGFR (mL/min/1.73 m2) | 49 ± 26 | 50 ± 20 | 56 ± 21 |
| NT-proBNP (pg/mL) | 5174 ± 6567 | 3407 (1948–6790) | 4185 ± 4340 |
| Proportion of patients with severe MR, EROA ≥ 40 mm2 (% of total) | 41 | 16 | 14 |
| Non-ischemic cause of cardiomyopathy (%) | 39.3 | 59.2 | 50.6 |
| Outcomes | |||
| Outcome | COAPT | MITRA-FR | RESHAPE-HF2 |
| Primary Efficacy | 0.3 (0.40–0.70) p < 0.001 | 1.16 (0.69 –1.84) p = 0.53 | 0.64 (0.48–0.85) p = 0.002 *** |
| Primary Safety | 96.6% freedom vs. performance goal of 88%, p < 0.001 | - ** | - **** |
| All-cause Mortality | 0.62 (0.46–0.82) p < 0.001 0.72 (0.58–0.89) at 5 years* | 1.11 (0.69–1.77) | 0.90 (0.71–1.13) [per 100 patient years] |
| Cardiovascular Mortality | 0.59 (0.43–0.81) p = 0.001 0.71 (0.56–0.90) at 5 years * | 1.09 (0.67–1.78) | 0.84 (0.55–1.28) p = 0.43 |
| Any-cause Hospitalization | 0.77 (0.64–0.93) p = 0.01 0.75 (0.63–0.89) at 5 years * | - | 0.82 (0.63–1.07) p = 0.15 [per 100 patient years] |
| HF Hospitalization | 0.53 (0.40–0.67) p < 0.001 0.49 (0.40–0.61) at 5 years * | 1.13 (0.81–1.56) | 0.59 (0.42–0.82) p = 0.002 [per 100 patient years] |
| Change in KCCQ score at 12 months | 16.1 (11.0–21.2) p < 0.001 | No significant difference on EQ5D Score | 10.9 (6.8–15.0) p < 0.001 |
| Change in 6 Minute Walk Distance from Baseline to 12 months (meters) | 57.9 (32.7–83.1) p < 0.001 | No significant difference | 20.5 (0.3–40.7) p = 0.05 |
| MV Surgery at 24 months | 0.14 (0.02–1.17) p = 0.57 | - | 0.51 (0.05–5.58) p = 0.57 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saeed, Y.B.; Deep, K.; Hagendorff, A.; Tayal, B. Diagnosis and Diagnostic Challenges of Secondary Mitral Regurgitation in the Era of Transcatheter Edge-to-Edge Repair of the Mitral Valve. J. Clin. Med. 2025, 14, 4518. https://doi.org/10.3390/jcm14134518
Saeed YB, Deep K, Hagendorff A, Tayal B. Diagnosis and Diagnostic Challenges of Secondary Mitral Regurgitation in the Era of Transcatheter Edge-to-Edge Repair of the Mitral Valve. Journal of Clinical Medicine. 2025; 14(13):4518. https://doi.org/10.3390/jcm14134518
Chicago/Turabian StyleSaeed, Yusef B., Kyra Deep, Andreas Hagendorff, and Bhupendar Tayal. 2025. "Diagnosis and Diagnostic Challenges of Secondary Mitral Regurgitation in the Era of Transcatheter Edge-to-Edge Repair of the Mitral Valve" Journal of Clinical Medicine 14, no. 13: 4518. https://doi.org/10.3390/jcm14134518
APA StyleSaeed, Y. B., Deep, K., Hagendorff, A., & Tayal, B. (2025). Diagnosis and Diagnostic Challenges of Secondary Mitral Regurgitation in the Era of Transcatheter Edge-to-Edge Repair of the Mitral Valve. Journal of Clinical Medicine, 14(13), 4518. https://doi.org/10.3390/jcm14134518






