V-CARE (Virtual Care After REsuscitation): Protocol for a Randomized Feasibility Study of a Virtual Psychoeducational Intervention After Cardiac Arrest—A STEPCARE Sub-Study
Abstract
1. Introduction
1.1. Rationale for a Psychoeducational Intervention
1.2. Study Aims
2. Methods
2.1. Study Design
2.2. Patient and Public Involvement
- (1)
- Running two semi-structured focus groups—one with survivors and one with key supporters—each lasting approximately 90 min, to gather in-depth insights from OHCA survivors and their key supporters regarding the ideal structure, content, and mode of delivery for the proposed psychoeducational intervention.
- (2)
- Themes emerging from the focus groups (Table S1) were used to develop a survey aimed at assessing the generalizability of the opinions expressed. This survey was distributed online via Sudden Cardiac Arrest UK and was available for one month between February and March 2022. A total of 95 responses were collected, comprising 62 survivors and 33 family members (70 women, 25 men). The survey included 26 questions, a mix of closed and open-ended items, to capture detailed feedback on the proposed intervention.
2.3. Study Population and Randomization
2.4. Interventions
2.4.1. V-CARE (Virtual CAre After REsuscitation)
2.4.2. Digital Information Booklet
2.5. Outcomes and Outcome Measures
2.5.1. Primary Outcomes
2.5.2. Secondary Outcomes
2.5.3. Additional Outcomes
2.6. Data Collection, Statistical Analyses, and Sample Size
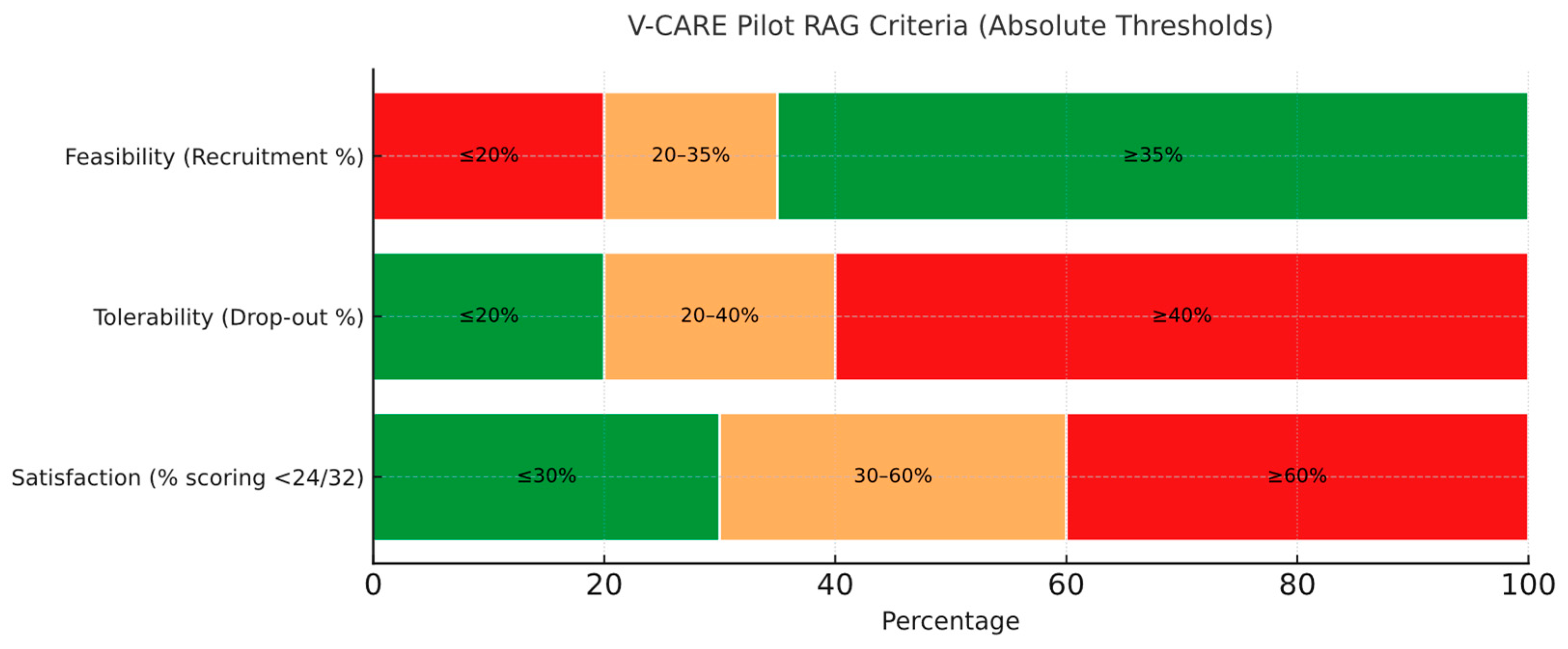
- Feasibility: At least 35% of patients screened as eligible should be recruited into the trial (green), but the trial will not be feasible if recruitment uptake is 20% or less (red). Recruitment of between 20% and 35% may require amendments (amber).
- Tolerability: The drop-out rate of patients recruited in the trial should be 20% or less (successful completion of the trial is defined as taking part in at least 3 out of 4 sessions of the intervention and complete outcome measures). A drop-out rate of 40% or more will indicate that the full trial is not feasible (red), with a percentage between 20% and 40% suggesting that amendments may be required (amber).
- Satisfaction with care: No more than 30% of participants in the V-CARE arm should score less than 24/32 on the CSQ-8 (green); if more than 60% of participants score less than 24/32, this will indicate that the trial is not feasible (red), with a percentage between 30% and 60% suggesting that amendments to the protocol may be required (amber) (Figure 1).
2.7. Ethics and Consent
3. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Jean-Philippe, E.; Lerner, I.; Valentin, E.; Folke, F.; Böttiger, B.; Gislason, G.; Jonsson, M.; Ringh, M.; Beganton, F.; Bougouin, W.; et al. Incidence of Sudden Cardiac Death in the European Union. J. Am. Coll. Cardiol. 2022, 79, 1818–1827. [Google Scholar] [CrossRef]
- Gräsner, J.T.; Herlitz, J.; Tjelmeland, I.B.M.; Wnent, J.; Masterson, S.; Lilja, G.; Bein, B.; Böttiger, B.W.; Rosell-Ortiz, F.; Nolan, J.P.; et al. European Resuscitation Council Guidelines 2021: Epidemiology of Cardiac Arrest in Europe. Resuscitation 2021, 161, 61–79. [Google Scholar] [CrossRef]
- Lilja, G.; Nielsen, N.; Friberg, H.; Horn, J.; Kjaergaard, J.; Nilsson, F.; Pellis, T.; Wetterslev, J.; Wise, M.P.; Bosch, F.; et al. Cognitive Function in Survivors of Out-of-Hospital Cardiac Arrest after Target Temperature Management at 33 °C Versus 36 °C. Circulation 2015, 131, 1340–1349. [Google Scholar] [CrossRef] [PubMed]
- Lilja, G. Follow-up of Cardiac Arrest Survivors: Why, How, and When? A Practical Approach. Semin. Neurol. 2017, 37, 88–93. [Google Scholar] [CrossRef] [PubMed]
- Moulaert, V.R.; Verbunt, J.A.; Van Heugten, C.M.; Wade, D.T. Cognitive Impairments in Survivors of Out-of-Hospital Cardiac Arrest: A Systematic Review. Resuscitation 2009, 80, 297–305. [Google Scholar] [CrossRef]
- Zook, N.; Voss, S.; Blennow Nordström, E.; Brett, S.J.; Jenkinson, E.; Shaw, P.; White, P.; Benger, J. Neurocognitive Function Following Out-of-Hospital Cardiac Arrest: A Systematic Review. Resuscitation 2022, 170, 238–246. [Google Scholar] [CrossRef]
- Blennow Nordström, E.; Lilja, G. Assessment of Neurocognitive Function after Cardiac Arrest. Curr. Opin. Crit. Care 2019, 25, 234–239. [Google Scholar] [CrossRef]
- Yaow, C.Y.L.; Teoh, S.E.; Lim, W.S.; Wang, R.S.Q.; Han, M.X.; Pek, P.P.; Tan, B.Y.Q.; Ong, M.E.H.; Ng, Q.X.; Ho, A.F.W. Prevalence of Anxiety, Depression, and Post-Traumatic Stress Disorder after Cardiac Arrest: A Systematic Review and Meta-Analysis. Resuscitation 2022, 170, 82–91. [Google Scholar] [CrossRef]
- Blennow Nordström, E.; Birk, J.L.; Rojas, D.A.; Sheehy, T.S.O.; Domínguez-Imbert Nieto, C.I.; Cruz, G.J.; Ten Brink, M.; Vargas, W.; Karas, M.; Agarwal, S. Prospective Evaluation of the Relationship between Cognition and Recovery Outcomes after Cardiac Arrest. Resuscitation 2024, 202, 110343. [Google Scholar] [CrossRef]
- Agarwal, S.; Birk, J.L.; Abukhadra, S.L.; Rojas, D.A.; Cornelius, T.M.; Bergman, M.; Chang, B.P.; Edmondson, D.E.; Kronish, I.M. Psychological Distress After Sudden Cardiac Arrest and Its Impact on Recovery. Curr. Cardiol. Rep. 2022, 24, 1351–1360. [Google Scholar] [CrossRef]
- Agarwal, S.; Wagner, M.K.; Mion, M. Psychological and Behavioral Dimensions in Cardiac Arrest Survivors and Their Families: A State-of-the-Art Review. Neurotherapeutics 2024, 22, e00509. [Google Scholar] [CrossRef] [PubMed]
- Joshi, V.L.; Tang, L.H.; Mikkelsen, T.B.; Nielsen, J.F.; Zinckernagel, L.; Borregaard, B.; Agarwal, S.; Kjær Ersbøll, A.; Yonis, H.; Kragholm, K.; et al. Does Time Heal Fatigue, Psychological, Cognitive and Disability Problems in People Who Experience an out-of-Hospital Cardiac Arrest? Results from the DANCAS Survey Study. Resuscitation 2023, 182, 109639. [Google Scholar] [CrossRef]
- Kragholm, K.; Wissenberg, M.; Mortensen, R.N.; Fonager, K.; Jensen, S.E.; Rajan, S.; Lippert, F.K.; Christensen, E.F.; Hansen, P.A.; Lang-Jensen, T.; et al. Return to Work in Out-of-Hospital Cardiac Arrest Survivors: A Nationwide Register-Based Follow-up Study. Circulation 2015, 131, 1682–1690. [Google Scholar] [CrossRef]
- Kearney, J.; Dyson, K.; Andrew, E.; Bernard, S.; Smith, K. Factors Associated with Return to Work among Survivors of Out-of-Hospital Cardiac Arrest. Resuscitation 2020, 146, 203–212. [Google Scholar] [CrossRef] [PubMed]
- Lilja, G.; Ullén, S.; Dankiewicz, J.; Friberg, H.; Levin, H.; Nordström, E.B.; Heimburg, K.; Jakobsen, J.C.; Ahlqvist, M.; Bass, F.; et al. Effects of Hypothermia vs Normothermia on Societal Participation and Cognitive Function at 6 Months in Survivors After Out-of-Hospital Cardiac Arrest. JAMA Neurol. 2023, 80, 1070–1079. [Google Scholar] [CrossRef] [PubMed]
- Lilja, G.; Nielsen, N.; Bro-Jeppesen, J.; Dunford, H.; Friberg, H.; Hofgren, C.; Horn, J.; Insorsi, A.; Kjaergaard, J.; Nilsson, F.; et al. Return to Work and Participation in Society After Out-of-Hospital Cardiac Arrest. Circ. Cardiovasc. Qual. Outcomes 2018, 11, e003566. [Google Scholar] [CrossRef]
- Holm, M.S.; Norekvål, T.M.; Fålun, N.; Gjengedal, E. Partners’ Ambivalence towards Cardiac Arrest and Hypothermia Treatment: A Qualitative Study. Nurs. Crit. Care 2012, 17, 231–238. [Google Scholar] [CrossRef]
- Dichman, C.K.; Wagner, M.K.; Joshi, L.V.; Bernild, C. Feeling Responsible but Unsupported: How Relatives of Cardiac Arrest Survivors Experience the Transition from Hospital to Daily Life—A Focus Group Study. Nurs. Open 2020, 8, 2520–2527. [Google Scholar] [CrossRef]
- Zimmerli, M.; Tisljar, K.; Balestra, G.M.; Langewitz, W.; Marsch, S.; Hunziker, S. Prevalence and Risk Factors for Post-Traumatic Stress Disorder in Relatives of out-of-Hospital Cardiac Arrest Patients. Resuscitation 2014, 85, 801–808. [Google Scholar] [CrossRef]
- Jensen, A.N.; Bonnén, K.B.; Kristiansen, M. “We Don’t Talk about His Heart”: Narrative Sense-Making and Long-Term Readjustment among Older out-of-Hospital Cardiac Arrest Survivors and Their Spouses. Resusc. Plus 2020, 3, 100024. [Google Scholar] [CrossRef]
- van’t Wout Hofland, J.; Moulaert, V.; van Heugten, C.; Verbunt, J. Long-Term Quality of Life of Caregivers of Cardiac Arrest Survivors and the Impact of Witnessing a Cardiac Event of a Close Relative. Resuscitation 2018, 128, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Southern, C.; Greif, R.T.; Abelairas-Gómez, C. Healing Hearts and Minds: The Need for Mental Health Support for Co-Survivors of Cardiac Arrest Patients. Resuscitation 2025, 209, 110580. [Google Scholar] [CrossRef] [PubMed]
- Presciutti, A.; Siry-Bove, B.; Newman, M.M.; Elmer, J.; Grigsby, J.; Masters, K.S.; Shaffer, J.A.; Vranceanu, A.; Perman, S.M. Qualitative Study of Long-Term Cardiac Arrest Survivors’ Challenges and Recommendations for Improving Survivorship. J. Am. Heart Assoc. 2022, 11, 25713. [Google Scholar] [CrossRef]
- Dainty, K.N.; Seaton, M.B.; Cowan, K.; Laupacis, A.; Dorian, P.; Douma, M.; Garner, J.; Goldstein, J.; Shire, D.; Sinclair, D.; et al. Partnering with Survivors & Families to Determine Research Priorities for Adult Out-of-Hospital Cardiac Arrest: A James Lind Alliance Priority Setting Partnership. Resusc. Plus 2021, 7, 100148. [Google Scholar] [CrossRef] [PubMed]
- Cardiac Arrest (Canada) | NIHR JLA. Available online: https://www.jla.nihr.ac.uk/priority-setting-partnerships/cardiac-arrest (accessed on 23 April 2025).
- Sawyer, K.N.; Camp-Rogers, T.R.; Kotini-Shah, P.; Del Rios, M.; Gossip, M.R.; Moitra, V.K.; Haywood, K.L.; Dougherty, C.M.; Lubitz, S.A.; Rabinstein, A.A.; et al. Sudden Cardiac Arrest Survivorship: A Scientific Statement from the American Heart Association. Circulation 2020, 141, E654–E685. [Google Scholar] [CrossRef] [PubMed]
- Nolan, J.P.; Sandroni, C.; Böttiger, B.W.; Cariou, A.; Cronberg, T.; Friberg, H.; Genbrugge, C.; Haywood, K.; Lilja, G.; Moulaert, V.R.M.; et al. European Resuscitation Council and European Society of Intensive Care Medicine Guidelines 2021: Post-Resuscitation Care. Resuscitation 2021, 161, 220–269. [Google Scholar] [CrossRef]
- Mion, M.; Simpson, R.; Johnson, T.; Oriolo, V.; Gudde, E.; Rees, P.; Quinn, T.; Von Vopelius-Feldt, J.; Gallagher, S.; Mozid, A.; et al. British Cardiovascular Intervention Society Consensus Position Statement on Out-of-Hospital Cardiac Arrest 2: Post-Discharge Rehabilitation. Interv. Cardiol. Rev. Res. Resour. 2022, 17, e19. [Google Scholar] [CrossRef]
- Joshi, V.L.; Christensen, J.; Lejsgaard, E.; Taylor, R.S.; Zwisler, A.D.; Tang, L.H. Effectiveness of Rehabilitation Interventions on the Secondary Consequences of Surviving a Cardiac Arrest: A Systematic Review and Meta-Analysis. BMJ Open 2021, 11, e047251. [Google Scholar] [CrossRef]
- Moulaert, V.R.; van Haastregt, J.C.; Wade, D.T.; Van Heugten, C.M.; Verbunt, J.A. “Stand Still …, and Move on”, an Early Neurologically-Focused Follow-up for Cardiac Arrest Survivors and Their Caregivers: A Process Evaluation. BMC Health Serv. Res. 2014, 14, 34. [Google Scholar] [CrossRef]
- Moulaert, V.R.M.; Goossens, M.; Heijnders, I.L.C.; Verbunt, J.A.; van Heugten, C.M. Early Neurologically Focused Follow-up after Cardiac Arrest Is Cost-Effective: A Trial-Based Economic Evaluation. Resuscitation 2016, 106, 30–36. [Google Scholar] [CrossRef]
- Cowan, M.J.; Pike, K.C.; Budzynski, H.K. Psychosocial Nursing Therapy Following Sudden Cardiac Arrest: Impact on Two-Year Survival. Nurs. Res. 2001, 50, 68–76. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.J.; Rogers, J.C.; Raina, K.D.; Callaway, C.W.; Rittenberger, J.C.; Leibold, M.L.; Holm, M.B. An Intervention for Cardiac Arrest Survivors with Chronic Fatigue: A Feasibility Study with Preliminary Outcomes. Resuscitation 2016, 105, 109–115. [Google Scholar] [CrossRef]
- Joshi, V.L.; Tang, L.H.; Kim, Y.J.; Wagner, M.K.; Nielsen, J.F.; Tjoernlund, M.; Zwisler, A.D. Promising Results from a Residential Rehabilitation Intervention Focused on Fatigue and the Secondary Psychological and Physical Consequences of Cardiac Arrest: The SCARF Feasibility Study. Resuscitation 2022, 173, 12–22. [Google Scholar] [CrossRef] [PubMed]
- Bergman, M.; Markowitz, J.C.; Kronish, I.M.; Agarwal, S.; Fisch, C.T.; Eder-Moreau, E.; Neria, Y. Acceptance and Mindfulness-Based Exposure Therapy for PTSD After Cardiac Arrest: An Open Feasibility Trial. J. Clin. Psychiatry 2023, 85, 50449. [Google Scholar] [CrossRef]
- Christensen, J.; Winkel, B.G.; Kirkeskov, L.; Folke, F.; Winther-Jensen, M.; Eckhardt-Bentsen, C.; Kjærgaard, J.; Hassager, C.; Wagner, M.K. The ROCK Trial-a Multidisciplinary Rehabilitation Intervention for Sudden Out-of-Hospital Cardiac Arrest Survivors Focusing on Return-to-WorK: A Pragmatic Randomized Controlled Trial Protocol. Trials 2024, 25, 99. [Google Scholar] [CrossRef]
- Gamberini, L.; Rucci, P.; Dolcini, C.; Masi, M.; Simoncini, L.; Tartaglione, M.; Del Giudice, D.; Domina, R.; Fagiolini, A.; Salucci, P. ENFORCER, Internet-Based Interventions for Cardiac Arrest Survivors: A Study Protocol for a Randomised, Parallel-Group, Multicentre Clinical Trial. Resusc. Plus 2024, 20, 100772. [Google Scholar] [CrossRef] [PubMed]
- The Cardiac Arrest Recovery Enablement and Self-Management Support Feasibility (CARESS-f) Study—NIHR Funding and Awards. Available online: https://fundingawards.nihr.ac.uk/award/NIHR204049 (accessed on 21 March 2025).
- Shapira, S.; Yeshua-Katz, D.; Cohn-Schwartz, E.; Aharonson-Daniel, L.; Sarid, O.; Clarfield, A.M. A Pilot Randomized Controlled Trial of a Group Intervention via Zoom to Relieve Loneliness and Depressive Symptoms among Older Persons during the COVID-19 Outbreak. Internet Interv. 2021, 24, 100368. [Google Scholar] [CrossRef]
- Jørgensen, B.B.; Gregersen, M.; Pallesen, S.H.; Damsgaard, E.M. A Group-Based Real-Time Videoconferencing Telerehabilitation Programme in Recently Discharged Geriatric Patients: A Feasibility Study. Eur. Geriatr. Med. 2021, 12, 801–808. [Google Scholar] [CrossRef]
- Kamp, C.B.; Dankiewicz, J.; Harboe Olsen, M.; Holgersson, J.; Saxena, M.; Young, P.; Niemelä, V.H.; Hästbacka, J.; Levin, H.; Lilja, G.; et al. Sedation, Temperature and Pressure after Cardiac Arrest and Resuscitation—The STEPCARE Trial: A Statistical Analysis Plan. Acta Anaesthesiol. Scand. 2025, 69, e70033. [Google Scholar] [CrossRef]
- Öberg, U.; Hörnsten, Å.; Isaksson, U. The Self-Management Assessment Scale: Development and Psychometric Testing of a Screening Instrument for Person-centred Guidance and Self-management Support. Nurs. Open 2019, 6, 504–513. [Google Scholar] [CrossRef]
- Extended Follow-Up | Stepcare. Available online: https://stepcare.org/extended-follow (accessed on 2 May 2025).
- Lewis, M.; Bromley, K.; Sutton, C.J.; McCray, G.; Myers, H.L.; Lancaster, G.A. Determining Sample Size for Progression Criteria for Pragmatic Pilot RCTs: The Hypothesis Test Strikes Back! Pilot Feasibility Stud. 2021, 7, 40. [Google Scholar] [CrossRef] [PubMed]
- Rothman, K.J. No Adjustments Are Needed for Multiple Comparisons. Epidemiology 1990, 1, 43–46. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mion, M.; Lilja, G.; Bohm, M.; Nordström, E.B.; Töniste, D.; Heimburg, K.; Swindell, P.; Dankiewicz, J.; Skrifvars, M.B.; Nielsen, N.; et al. V-CARE (Virtual Care After REsuscitation): Protocol for a Randomized Feasibility Study of a Virtual Psychoeducational Intervention After Cardiac Arrest—A STEPCARE Sub-Study. J. Clin. Med. 2025, 14, 4429. https://doi.org/10.3390/jcm14134429
Mion M, Lilja G, Bohm M, Nordström EB, Töniste D, Heimburg K, Swindell P, Dankiewicz J, Skrifvars MB, Nielsen N, et al. V-CARE (Virtual Care After REsuscitation): Protocol for a Randomized Feasibility Study of a Virtual Psychoeducational Intervention After Cardiac Arrest—A STEPCARE Sub-Study. Journal of Clinical Medicine. 2025; 14(13):4429. https://doi.org/10.3390/jcm14134429
Chicago/Turabian StyleMion, Marco, Gisela Lilja, Mattias Bohm, Erik Blennow Nordström, Dorit Töniste, Katarina Heimburg, Paul Swindell, Josef Dankiewicz, Markus B. Skrifvars, Niklas Nielsen, and et al. 2025. "V-CARE (Virtual Care After REsuscitation): Protocol for a Randomized Feasibility Study of a Virtual Psychoeducational Intervention After Cardiac Arrest—A STEPCARE Sub-Study" Journal of Clinical Medicine 14, no. 13: 4429. https://doi.org/10.3390/jcm14134429
APA StyleMion, M., Lilja, G., Bohm, M., Nordström, E. B., Töniste, D., Heimburg, K., Swindell, P., Dankiewicz, J., Skrifvars, M. B., Nielsen, N., Jakobsen, J. C., White, J., Wise, M. P., Gorgoraptis, N., Keenan, M., Hopkins, P., Pareek, N., Maccaroni, M., & Keeble, T. R. (2025). V-CARE (Virtual Care After REsuscitation): Protocol for a Randomized Feasibility Study of a Virtual Psychoeducational Intervention After Cardiac Arrest—A STEPCARE Sub-Study. Journal of Clinical Medicine, 14(13), 4429. https://doi.org/10.3390/jcm14134429





