Predictors of Weaning Success in Patients on Prolonged Mechanical Ventilation: A Retrospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
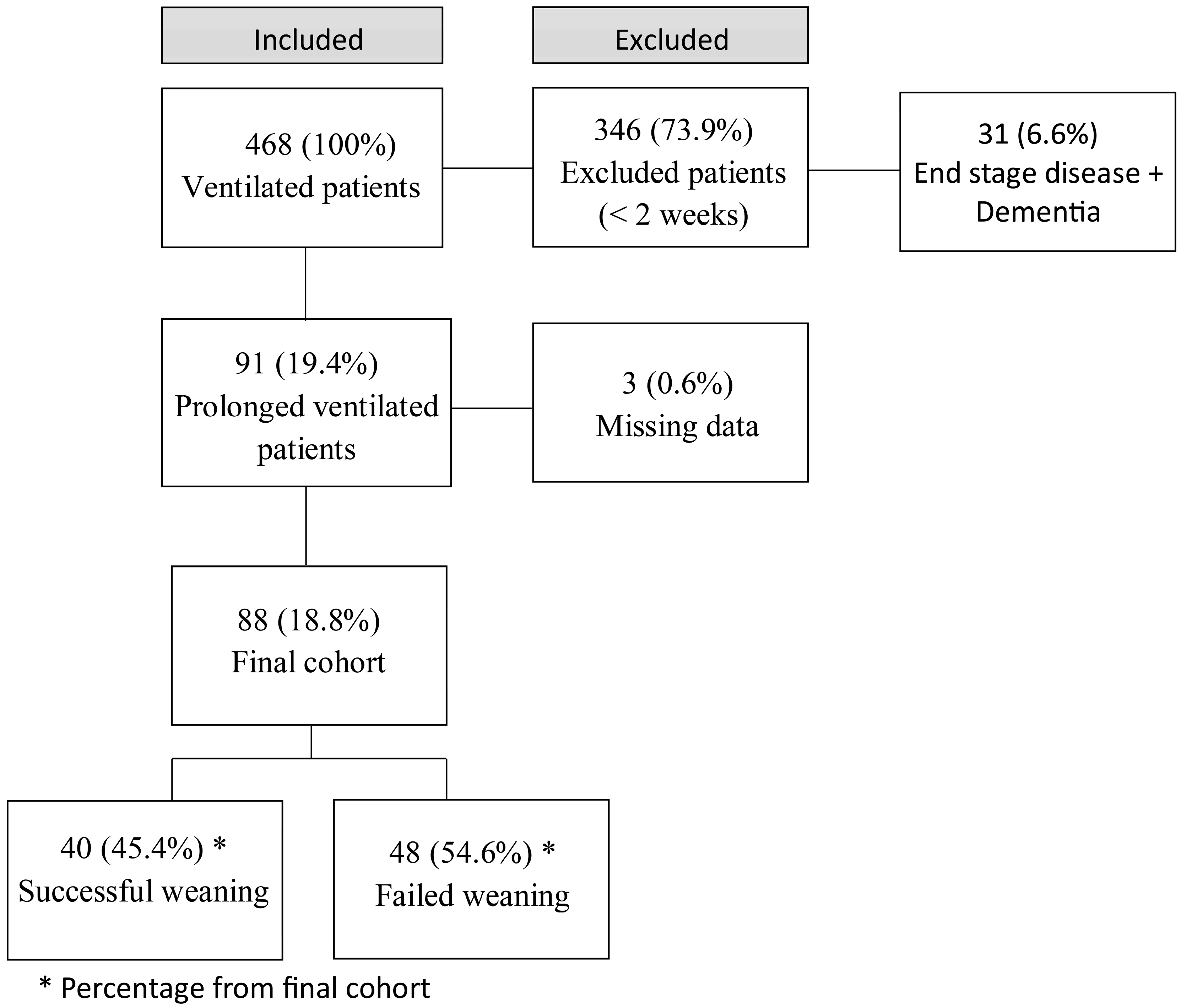
2.2. Study Population
2.3. Weaning Protocol and Definition of Weaning Success
2.4. Study Outcomes
2.5. Data Sources
2.6. Statistical Analysis
3. Results
4. Discussion
- Increased risk of infections: Hypoalbuminemia increases the risk of infections, sepsis, and multiorgan failure, particularly increasing the likelihood of ventilator-associated pneumonia. Conde’s 2008 study [28] identified hypoalbuminemia as a predictor of postoperative pulmonary infections;
- Altered pharmacokinetics and pharmacodynamics: The effectiveness of targeted antibiotic therapy is compromised by hypoalbuminemia, which affects treatment efficacy [20];
- Increased thromboembolic events: Hypoalbuminemia increases the risk of thromboembolic events, including large arterial and venous events such as deep vein thrombosis and pulmonary embolism;
- Indication of poor nutritional status: Hypoalbuminemia signifies poor caloric balance and malnutrition, often due to chronic illness;
- Critical for wound healing: Albumin is essential for wound healing. The presence of pressure ulcers in patients with hypoalbuminemia reduces the healing potential and worsens the prognosis.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BiPAP | Bilevel Positive Airway Pressure |
| CKD | Chronic Kidney Disease |
| COPD | Chronic Obstructive Pulmonary Disease |
| FW | Failed Weaning |
| ICU | Intensive Care Unit |
| IQR | Interquartile Range |
| MV | Mechanical Ventilation |
| OSA | Obstructive Sleep Apnea |
| P/F Ratio | Partial Pressure of Oxygen (PaO2)/ Fraction of Inspired Oxygen (FiO2) Ratio |
| SBT | Spontaneous Breathing Trial |
| SUMC | Soroka University Medical Center |
| SW | Successful Weaning |
| WIND | Weaning Outcome According to a New Definition |
References
- McConville, J.F.; Kress, J.P. Weaning patients from the ventilator. N. Engl. J. Med. 2012, 367, 2233–2239. [Google Scholar] [CrossRef] [PubMed]
- Boles, J.M.; Bion, J.; Connors, A.; Herridge, M.; Marsh, B.; Melot, C.; Pearl, R.; Silverman, H.; Stanchina, M.; Vieillard-Baron, A.; et al. Weaning from mechanical ventilation. Eur. Respir. J. 2007, 29, 1033–1056. [Google Scholar] [CrossRef]
- Pilcher, D.V.; Bailey, M.J.; Treacher, D.F.; Hamid, S.; Williams, A.J.; Davidson, A.C. Outcomes, cost and long term survival of patients referred to a regional weaning centre. Thorax 2005, 60, 187–192. [Google Scholar] [CrossRef]
- Epstein, S.K.; Ciubotaru, R.L. Independent effects of etiology of failure and time to reintubation on outcome for patients failing extubation. Am. J. Respir. Crit. Care Med. 1998, 158, 489–493. [Google Scholar] [CrossRef] [PubMed]
- Thille, A.W.; Richard, J.C.M.; Brochard, L. The decision to extubate in the intensive care unit. Am. J. Respir. Crit. Care Med. 2013, 187, 1294–1302. [Google Scholar] [CrossRef] [PubMed]
- Peñuelas, O.; Frutos-Vivar, F.; Fernández, C.; Anzueto, A.; Epstein, S.K.; Apezteguía, C.; González, M.; Nin, N.; Raymondos, K.; Tomicic, V.; et al. Characteristics and outcomes of ventilated patients according to time to liberation from mechanical ventilation. Am. J. Respir. Crit. Care Med. 2011, 184, 430–437. [Google Scholar] [CrossRef]
- Tonnelier, A.; Tonnelier, J.M.; Nowak, E.; Gut-Gobert, C.; Prat, G.; Renault, A.; Boles, J.M.; L’Her, E. Clinical relevance of classification according to weaning difficulty. Respir. Care 2011, 56, 583–590. [Google Scholar] [CrossRef]
- Funk, G.C.; Anders, S.; Breyer, M.K.; Burghuber, O.C.; Edelmann, G.; Heindl, W.; Hinterholzer, G.; Kohansal, R.; Schuster, R.; Hartl, S.; et al. Incidence and outcome of weaning from mechanical ventilation according to new categories. Eur. Respir. J. 2010, 35, 88–94. [Google Scholar] [CrossRef]
- Pu, L.; Zhu, B.; Jiang, L.; Du, B.; Zhu, X.; Li, A.; Li, G.; He, Z.; Chen, W.; Ma, P.; et al. Weaning critically ill patients from mechanical ventilation: A prospective cohort study. J. Crit. Care 2015, 30, 862.e7-13. [Google Scholar] [CrossRef]
- Jeong, B.H.; Ko, M.G.; Nam, J.; Yoo, H.; Chung, C.R.; Suh, G.Y.; Jeon, K. Differences in clinical outcomes according to weaning classifications in medical intensive care units. PLoS ONE 2015, 10, e0122810. [Google Scholar] [CrossRef]
- Schönhofer, B.; Euteneuer, S.; Nava, S.; Suchi, S.; Köhler, D. Survival of mechanically ventilated patients admitted to a specialised weaning centre. Intensive Care Med. 2002, 28, 908–916. [Google Scholar] [CrossRef] [PubMed]
- Lago, A.F.; Gastaldi, A.C.; Mazzoni, A.A.S.; Tanaka, V.B.; Siansi, V.C.; Reis, I.S.; Basile-Filho, A. Comparison of International Consensus Conference guidelines and WIND classification for weaning from mechanical ventilation in Brazilian critically ill patients: A retrospective cohort study. Medicine 2019, 98, e17534. [Google Scholar] [CrossRef]
- Sellares, J.; Ferrer, M.; Cano, E.; Loureiro, H.; Valencia, M.; Torres, A. Predictors of prolonged weaning and survival during ventilator weaning in a respiratory ICU. Intensive Care Med. 2011, 37, 775–784. [Google Scholar] [CrossRef] [PubMed]
- Upadya, A.; Tilluckdharry, L.; Muralidharan, V.; Amoateng-Adjepong, Y.; Manthous, C.A. Fluid balance and weaning outcomes. Intensive Care Med. 2005, 31, 1643–1647. [Google Scholar] [CrossRef] [PubMed]
- National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network; Wiedemann, H.P.; Wheeler, A.P.; Bernard, G.R.; Thompson, B.T.; Hayden, D.; deBoisblanc, B.; Connors, A.F.; Hite, R.D.; Harabin, A.L. Comparison of two fluid-management strategies in acute lung injury. N. Engl. J. Med. 2006, 354, 2564–2575. [Google Scholar] [CrossRef]
- Hjortrup, P.B.; Haase, N.; Bundgaard, H.; Thomsen, S.L.; Winding, R.; Pettilä, V.; Aaen, A.; Lodahl, D.; Berthelsen, R.E.; Christensen, H.; et al. Restricting volumes of resuscitation fluid in adults with septic shock after initial management: The Classic randomised, parallel-group, multicentre feasibility trial. Intensive Care Med. 2016, 42, 1695–1705. [Google Scholar] [CrossRef]
- Cinotti, R.; Lascarrou, J.B.; Azais, M.A.; Colin, G.; Quenot, J.P.; Mahé, P.J.; Roquilly, A.; Gaultier, A.; Asehnoune, K.; Reignier, J. Diuretics decrease fluid balance in patients on invasive mechanical ventilation: The randomized-controlled single blind, IRIHS study. Crit. Care 2021, 25, 98. [Google Scholar] [CrossRef]
- Virole, S.; Duceau, B.; Morawiec, E.; Nierat, M.C.; Paifait, M.; Decaveie, M.; Demoule, A.; Delemazure, J.; Dres, M. Contribution and evolution of respiratory muscles function in weaning outcome of ventilator-dependent patients. Crit. Care 2024, 28, 421. [Google Scholar] [CrossRef]
- Pham, T.; Heunks, L.; Bellani, G.; Madotto, F.; Aragao, I.; Beduneau, G.; Goligher, E.C.; Grasselli, G.; Laake, J.H.; Mancebo, J.; et al. Weaning from mechanical ventilation in intensive care units across 50 countries (WEAN-SAFE): A multicentre, prospective, observational cohort study. Lancet Respir. Med. 2023, 11, 465–476. [Google Scholar] [CrossRef]
- Béduneau, G.; Pham, T.; Schortgen, F.; Piquilloud, L.; Zogheib, E.; Jonas, M.; Grelon, F.; Runge, I.; Terzi, N.; Grangé, S.; et al. Epidemiology of Weaning Outcome According to a New Definition. The WIND study. Am. J. Respir. Crit. Care Med. 2017, 195, 772–783. [Google Scholar] [CrossRef]
- Windisch, W.; Dellweg, D.; Geiseler, J.; Westhoff, M.; Pfeifer, M.; Suchi, S.; Schönhofer, B. Prolonged weaning from mechanical ventilation. Dtsch Ärztebl Int. 2020, 117, 197–204. [Google Scholar] [CrossRef]
- Warnke, C.; Heine, A.; Müller-Heinrich, A.; Knaak, C.; Friesecke, S.; Obst, A.; Bollmann, T.; Desole, S.; Boesche, M.; Stubbe, B.; et al. Predictors of survival after prolonged weaning from mechanical ventilation. J. Crit. Care 2020, 60, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Saber, H.; Palla, M.; Kazemlou, S.; Navi, B.B.; Yoo, A.J.; Simonsen, C.Z.; Sandio, A.; Rajah, G.; Khatibi, K.; Liebeskind, D.S.; et al. Prevalence, predictors, and outcomes of prolonged mechanical ventilation after endovascular stroke therapy. Neurocrit. Care 2021, 34, 1009–1016. [Google Scholar] [CrossRef]
- Magnet, F.S.; Bleichroth, H.; Huttmann, S.E.; Callegari, J.; Schwarz, S.B.; Schmoor, C.; Windisch, W.; Storre, J.H. Clinical evidence for respiratory insufficiency type II predicts weaning failure in long-term ventilated, tracheotomised patients: A retrospective analysis. J. Intensive Care. 2018, 6, 67. [Google Scholar] [CrossRef]
- Ghauri, S.K.; Javaeed, A.; Mustafa, K.J.; Khan, A.S. Predictors of prolonged mechanical ventilation in patients admitted to intensive care units: A systematic review. Int. J. Health Sci. (Qassim) 2019, 13, 31–38. [Google Scholar] [PubMed]
- Huang, M.; Ong, B.H.; Hoo, A.E.E.; Gao, F.; Chao, V.T.T.; Lim, C.H.; Tan, T.E.; Sin, K.Y.K. Prognostic factors for survival after extracorporeal membrane oxygenation for cardiogenic shock. ASAIO J. 2020, 66, 141–145. [Google Scholar] [CrossRef] [PubMed]
- Wiedermann, C.J. Hypoalbuminemia as surrogate and culprit of infections. Int. J. Mol. Sci. 2021, 22, 4496. [Google Scholar] [CrossRef]
- Conde, M.; Lawrence, V. Postoperative pulmonary infections. BMJ Clin. Evid. 2008, 2008, 2201. [Google Scholar]
- Moodie, L.; Reeve, J.; Elkins, M. Inspiratory muscle training increases inspiratory muscle strength in patients weaning from mechanical ventilation: A systematic review. J. Physiother. 2011, 57, 213–221. [Google Scholar] [CrossRef]
| Overall, N = 881 | Failed Weaning Group (N = 48) 1 | Successful Weaning Group (N = 40) 1 | p-Value 2 | |
|---|---|---|---|---|
| Age (years) | 73 (63, 80) | 77 (67, 82) | 64 (57, 76) | 0.002 |
| Sex—Male | 44 (50%) | 24 (50%) | 20 (50%) | >0.9 |
| Weaning attempts | 3.00 (1.00, 3.50) | 3.00 (2.00, 4.00) | 2.00 (1.00, 3.00) | 0.026 |
| Hypertension | 51 (58%) | 32 (67%) | 19 (48%) | 0.070 |
| Dyslipidemia | 43 (49%) | 24 (50%) | 19 (48%) | 0.8 |
| Ischemic heart disease | 34 (39%) | 22 (46%) | 12 (30%) | 0.13 |
| Diabetes mellitus | 32 (36%) | 18 (38%) | 14 (35%) | 0.8 |
| COPD | 23 (26%) | 14 (29%) | 9 (23%) | 0.5 |
| Obesity | 22 (25%) | 15 (31%) | 7 (18%) | 0.14 |
| CKD | 13 (15%) | 7 (15%) | 6 (15%) | >0.9 |
| Malignancy | 13 (15%) | 9 (19%) | 4 (10%) | 0.08 |
| Pulmonary hypertension | 9 (10%) | 6 (13%) | 3 (7.5%) | 0.5 |
| Thyroid dysfunction | 7 (8.0%) | 3 (6.3%) | 4 (10%) | 0.7 |
| OSA | 5 (5.7%) | 2 (4.2%) | 3 (7.5%) | 0.7 |
| Dementia | 5 (5.7%) | 4 (8.3%) | 1 (2.5%) | 0.4 |
| Smoking | 17 (19%) | 7 (15%) | 10 (25%) | 0.2 |
| Alcohol | 9 (10%) | 5 (10%) | 4 (10%) | >0.9 |
| Drug use | 6 (6.8%) | 2 (4.2%) | 4 (10%) | 0.4 |
| Chronic steroid use | 1 (1.1%) | 0 (0%) | 1 (2.5%) | 0.5 |
| Failed Weaning Group (N = 48) 1 | Successful Weaning Group (N = 40) 1 | p-Value 2 | |
|---|---|---|---|
| SOFA score | 0.011 | ||
| Mean [SD] | 8.31 [1.47] | 7.41 [1.36] | |
| Median (IQR) | 8.00 (7.00, 9.00) | 7.50 (6.00, 8.00) | |
| P/F ratio | 89 (65, 145) | 142 (67, 250) | 0.052 |
| pCO2 | 48 (38, 57) | 47 (40, 55) | 0.7 |
| White blood cells (*103/uL) | 10.5 (8.7, 12.3) | 11.5 (9.6, 13.9) | 0.3 |
| Hemoglobin (mg/dL) | 9.30 (8.15, 10.68) | 9.75 (8.90, 11.20) | 0.086 |
| Platelets (*103/uL) | 282 (217, 372) | 319 (227, 412) | 0.2 |
| Glucose (mg/dL) | 123 (102, 191) | 133 (117, 165) | 0.5 |
| Urea (mg/dL) | 74 (49, 109) | 43 (33, 82) | 0.008 |
| Total bilirubin (mg/dL) | 0.56 (0.43, 0.74) | 0.47 (0.38, 0.60) | 0.047 |
| Creatinine (mg/dL) | 0.85 (0.55, 1.40) | 0.74 (0.43, 1.22) | 0.12 |
| Albumin (g/dL) | 2.40 (2.15, 2.85) | 2.70 (2.50, 3.20) | 0.002 |
| INR | 1.17 (1.10, 1.39) | 1.12 (1.07, 1.15) | 0.066 |
| Duration of diuretic (days) | 13 (5, 26) | 22 (13, 32) | 0.078 |
| Diuretic agents daily dose (total amount/duration [mg/day]) | 52 (37, 84) | 38 (33, 53) | 0.089 |
| BMI (kg/m2) | 29(25,37) | 27(23,34) | 0.16 |
| Vasoactive agents | 17 (35%) | 10 (25%) | 0.3 |
| Atracurium (once) | 2 (4.2%) | 1 (2.5%) | >0.9 |
| Atracurium (twice or more) | 0 (0%) | 0 (0%) | |
| Steroids (at least once) | 22 (46%) | 22 (55%) | 0.4 |
| Characteristic | Overall, N = 88 1 | Failed Weaning Group, N = 48 1 | Successful Weaning Group, N = 40 1 | p-Value 2 |
|---|---|---|---|---|
| Hospitalization length of stay (days) | 45 (32, 59) | 39 (31, 56) | 52 (32, 61) | 0.10 |
| Duration of mechanical ventilation (days) | 31 (19, 41) | 35 (25, 48) | 28 (18, 37) | 0.040 |
| In-hospital tracheostomy | 69 (78%) | 38 (79%) | 31 (78%) | 0.8 |
| ICU days | 15 (9, 25), n = 59 | 13 (9, 23), n = 32 | 16 (10, 26), n = 27 | 0.4 |
| Mortality during hospitalization | 25 (28%) | 25 (52%) | 0 (0%) | <0.001 |
| All-cause mortality within 30 days since hospital discharge | 10 (11%) | 3 (6.3%) | 7 (18%) | 0.2 |
| All-cause mortality within 1 year since hospital discharge | 25 (28%) | 12 (25%) | 13 (33%) | 0.4 |
| Status at discharge | <0.001 | |||
| Mechanical ventilation | 23 (37%) | 23 (100%) | 0 (0%) | |
| Non-support | 23 (37%) | 0 (0%) | 23 (58%) | |
| Oxygen | 15 (24%) | 0 (0%) | 15 (38%) | |
| Oxygen + BiPAP | 2 (3.2%) | 0 (0%) | 2 (5.0%) |
| Characteristic | OR | 95% CI | p-Value |
|---|---|---|---|
| SOFA score | 0.54 | 0.32, 0.85 | 0.012 |
| Albumin | 5.71 | 1.79, 21.4 | 0.005 |
| Age | 0.97 | 0.93, 1.01 | 0.2 |
| Urea | 1.01 | 0.99, 1.02 | 0.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amir, B.; Mai, O.; Shira, T.; Ido, P.; Nave, P.; Carmi, B. Predictors of Weaning Success in Patients on Prolonged Mechanical Ventilation: A Retrospective Cohort Study. J. Clin. Med. 2025, 14, 4427. https://doi.org/10.3390/jcm14134427
Amir B, Mai O, Shira T, Ido P, Nave P, Carmi B. Predictors of Weaning Success in Patients on Prolonged Mechanical Ventilation: A Retrospective Cohort Study. Journal of Clinical Medicine. 2025; 14(13):4427. https://doi.org/10.3390/jcm14134427
Chicago/Turabian StyleAmir, Bartal, Ofri Mai, Turgeman Shira, Peles Ido, Paran Nave, and Bartal Carmi. 2025. "Predictors of Weaning Success in Patients on Prolonged Mechanical Ventilation: A Retrospective Cohort Study" Journal of Clinical Medicine 14, no. 13: 4427. https://doi.org/10.3390/jcm14134427
APA StyleAmir, B., Mai, O., Shira, T., Ido, P., Nave, P., & Carmi, B. (2025). Predictors of Weaning Success in Patients on Prolonged Mechanical Ventilation: A Retrospective Cohort Study. Journal of Clinical Medicine, 14(13), 4427. https://doi.org/10.3390/jcm14134427





