Current Trends in Facelift and Necklift Procedures
Abstract
1. Introduction
2. Materials and Methods
3. Discussion
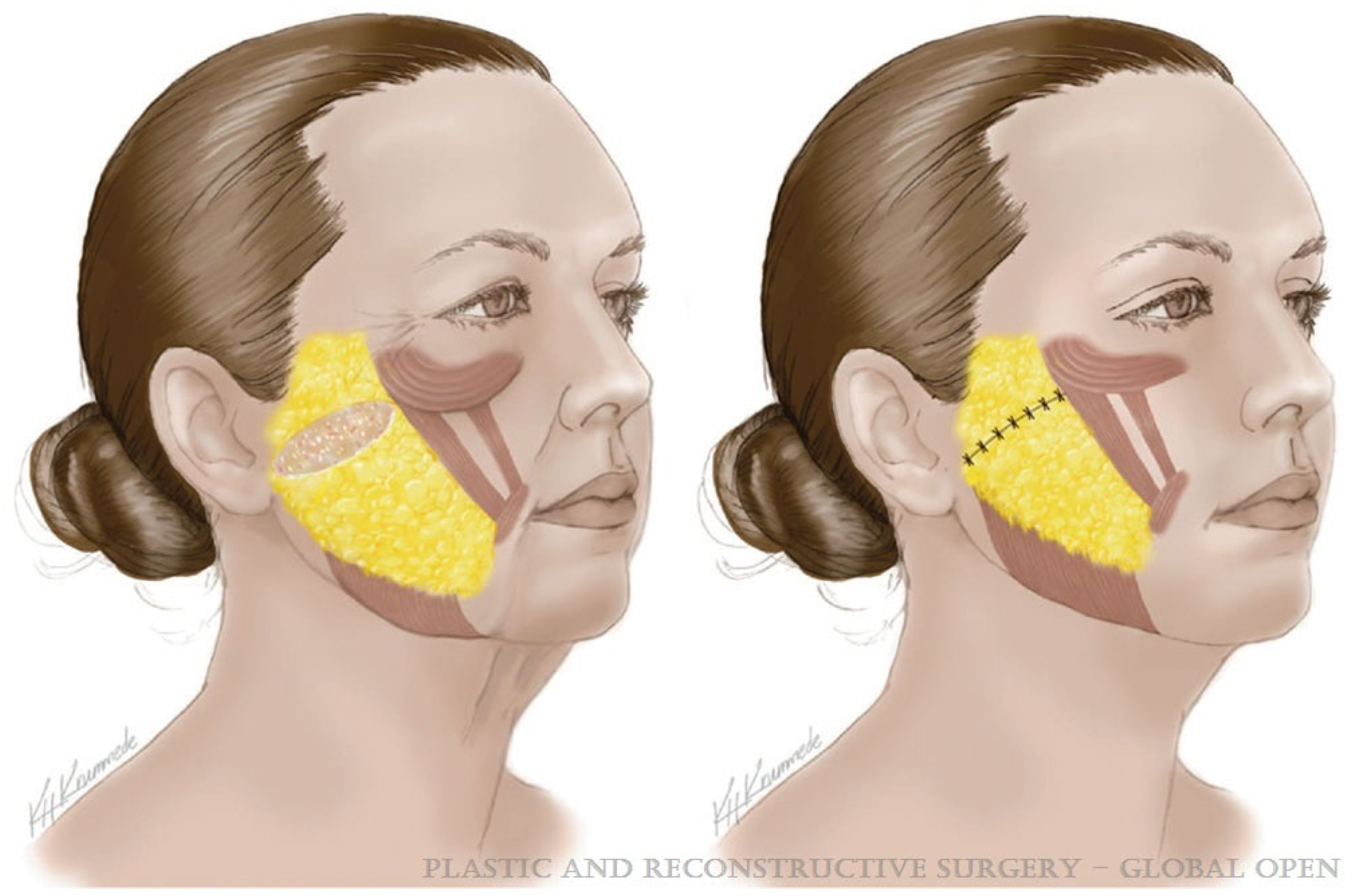
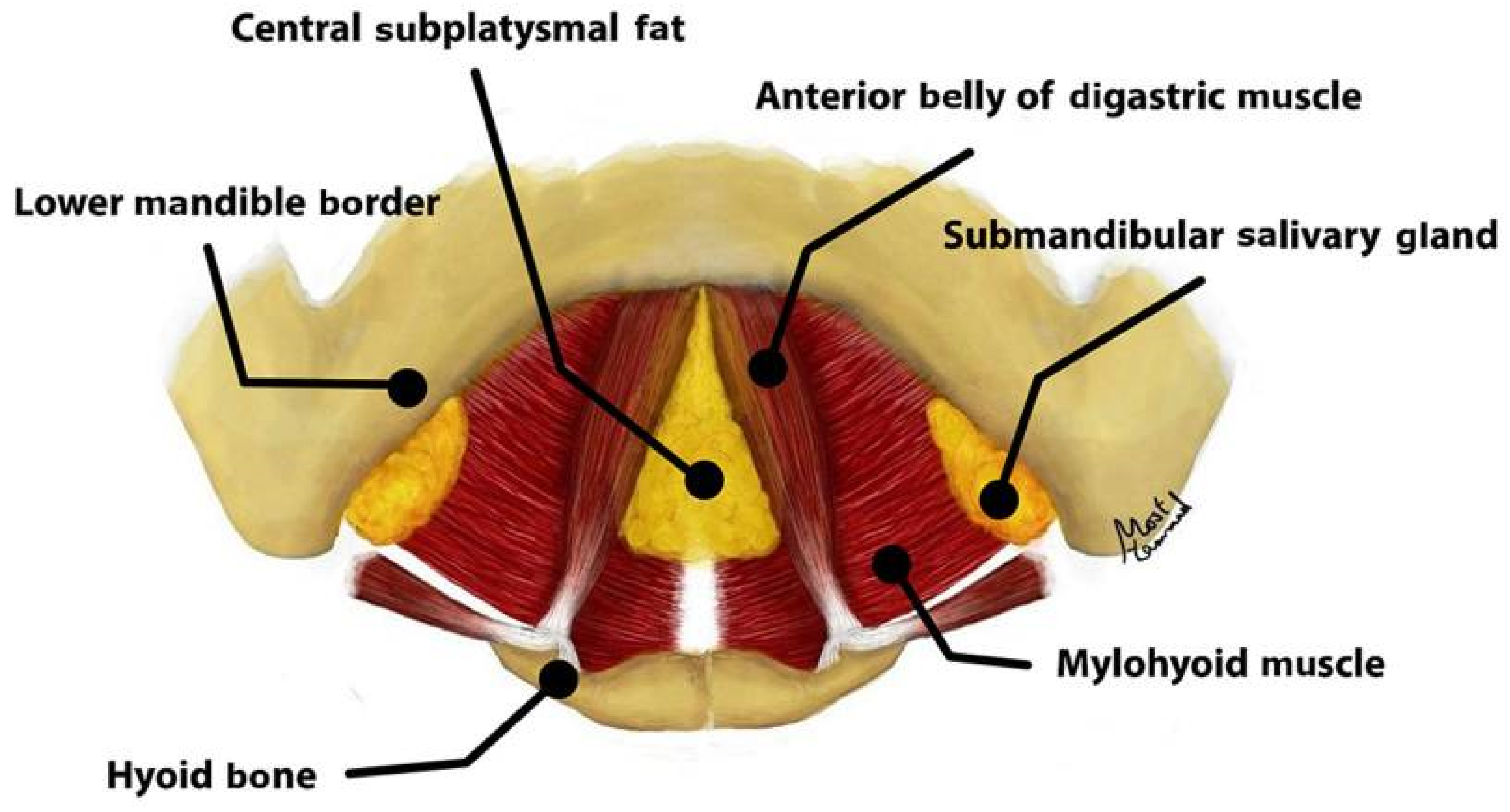
3.1. Renewed Attention to Anatomy
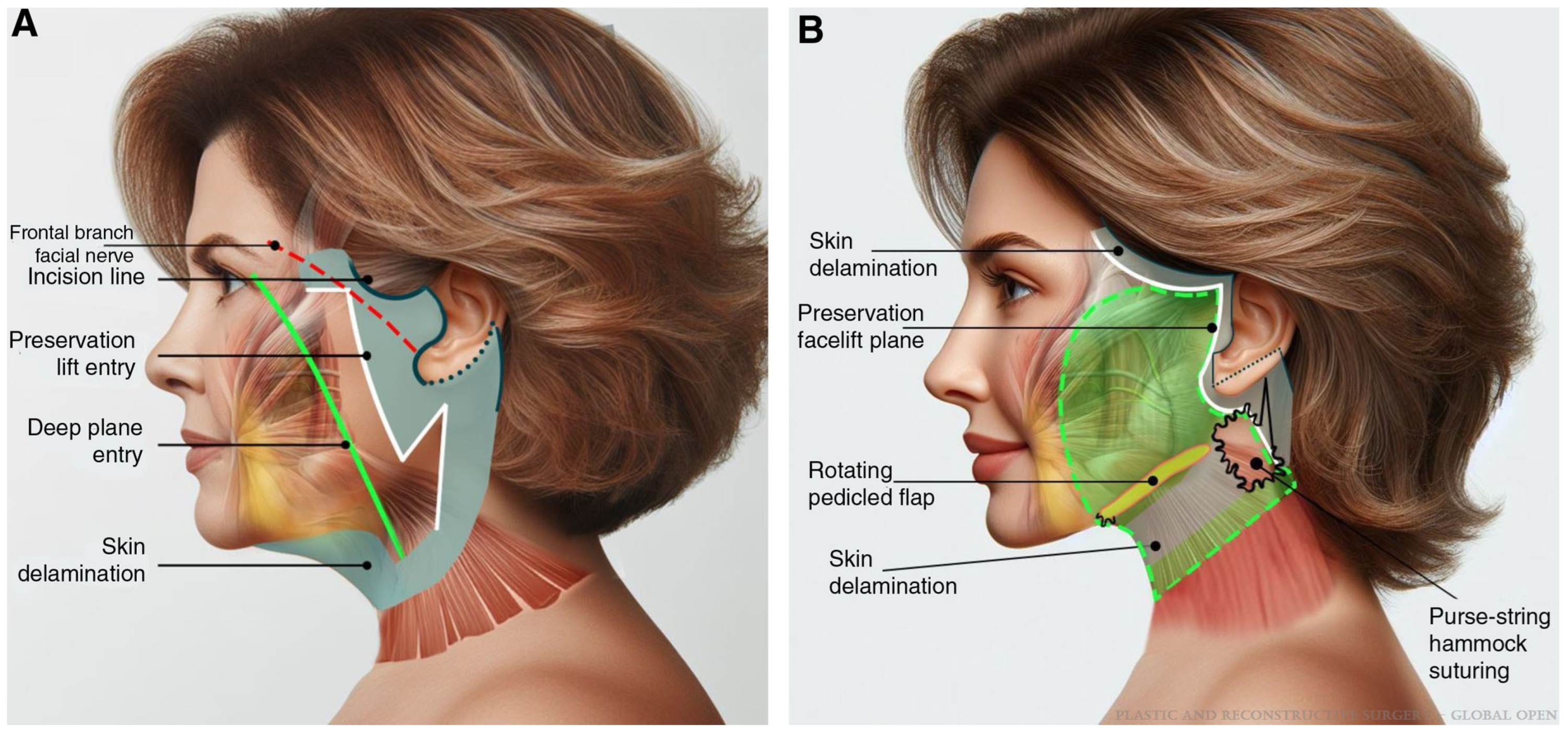
3.2. Facelift Technique
3.3. Management of the Neck
3.4. Other Considerations
3.5. Limitations and Future Directions
4. Conclusions
Author Contributions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Stein, M.J.; Aston, S.J. Ancillary Procedures to Facelift Surgery: What has Changed? Aesthet. Surg. J. Open Forum 2023, 5, ojad063. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.R.; Kennedy, P.M. The Aging Face. Med. Clin. N. Am. 2018, 102, 1041–1054. [Google Scholar] [CrossRef]
- Fang, A.H.; de la Torre, J. A Systematic Review of Rhytidectomy Complications and Prevention Methods: Evaluating the Trends. Ann. Plast. Surg. 2025, 94 (Suppl. S4), S502–S516. [Google Scholar] [CrossRef] [PubMed]
- Mirra, C.; Savani, L.; Botti, C.; Botti, G. Our 40 Years’ Experience on Face and Neck Lift Procedures with High-SMAS Flap Techniques: How to Manage Secondary and Tertiary Surgeries. Aesthet. Plast. Surg. 2025, 49, 462–469. [Google Scholar] [CrossRef]
- Jalalabadi, F.; Rohrich, R.J. The 10-7 Facial Analysis Method for Face Lifting and Facial Rejuvenation. Plast. Reconstr. Surg. 2024, 154, 275e–282e. [Google Scholar] [CrossRef] [PubMed]
- Nayak, L.M.; Linkov, G. Social Media Marketing in Facial Plastic Surgery: What Has Worked? Facial Plast. Surg. Clin. N. Am. 2019, 27, 373–377. [Google Scholar] [CrossRef]
- Corduff, N. Surgical or Nonsurgical Facial Rejuvenation: The Patients’ Choice. Plast. Reconstr. Surg.—Glob. Open 2023, 11, e5318. [Google Scholar] [CrossRef]
- Hashem, A.M.; Couto, R.A.; Duraes, E.F.; Çakmakoğlu, Ç.; Swanson, M.; Surek, C.; Zins, J.E. Facelift Part I: History, Anatomy, and Clinical Assessment. Aesthet. Surg. J. 2020, 40, 1–18. [Google Scholar] [CrossRef]
- O’Brien, J.X.; Rozen, W.M.; Whitaker, I.S.; Ashton, M.W. Lore’s fascia and the platysma-auricular ligament are distinct structures. J. Plast. Reconstr. Aesthet. Surg. 2012, 65, e241–e245. [Google Scholar] [CrossRef]
- Mitz, V.; Peyronie, M. The superficial musculo-aponeurotic system (SMAS) in the parotid and cheek area. Plast. Reconstr. Surg. 1976, 58, 80–88. [Google Scholar] [CrossRef]
- Minelli, L.; van der Lei, B.; Mendelson, B.C. The Superficial Musculoaponeurotic System: Does It Really Exist as an Anatomical Entity? Plast. Reconstr. Surg. 2024, 153, 1023–1034. [Google Scholar] [CrossRef] [PubMed]
- Stuzin, J.M.; Baker, T.J.; Gordon, H.L. The relationship of the superficial and deep facial fascias: Relevance to rhytidectomy and aging. Plast. Reconstr. Surg. 1992, 89, 441–449, discussion 450–451. [Google Scholar] [CrossRef] [PubMed]
- Cotofana, S.; Fratila, A.A.; Schenck, T.L.; Redka-Swoboda, W.; Zilinsky, I.; Pavicic, T. The Anatomy of the Aging Face: A Review. Facial Plast. Surg. 2016, 32, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Minelli, L.; van der Lei, B.; Mendelson, B.C. The Deep Fascia of the Head and Neck Revisited: Relationship with the Facial Nerve and Implications for Rhytidectomy. Plast. Reconstr. Surg. 2024, 153, 1273–1288. [Google Scholar] [CrossRef] [PubMed]
- Andretto Amodeo, C.; Eggerstedt, M.; Kim, I.A.; Nabili, V.; Keller, G.S. The Deep Fascia of the Infraorbital Region, Deep Plane, and Suprafibromuscular Facelift: New Anatomy for Safer Facelifting. Facial Plast. Surg. 2022, 38, 623–629. [Google Scholar] [CrossRef]
- Stuzin, J.M.; Rohrich, R.J. Facial Nerve Danger Zones. Plast. Reconstr. Surg. 2020, 145, 99–102. [Google Scholar] [CrossRef]
- Lindsey, J.T., Jr.; Lee, J.J.; Phan, H.T.P.; Lindsey, J.T., Sr. Defining the Cervical Line in Face-Lift Surgery: A Three-Dimensional Study of the Cervical and Marginal Mandibular Branches of the Facial Nerve. Plast. Reconstr. Surg. 2023, 152, 977–985. [Google Scholar] [CrossRef]
- Cakmak, O.; Buyuklu, F.; Kaya, K.S.; Babakurban, S.T.; Bogari, A.; Tunalı, S. Anatomical Insights on the Cervical Nerve for Contemporary Face and Neck Lifting: A Cadaveric Study. Aesthet. Surg. J. 2024, 44, NP532–NP539. [Google Scholar] [CrossRef]
- Malins, W.L.E.; Walker, H.; Guirguis, J.; Riaz, M.; Saleh, D.B. Defining a Safe Corridor of Cervical Branch Preservation in Lateral Platysmaplasty Surgery During Facial Rejuvenation Surgery. Aesthet. Surg. J. 2022, 42, NP93–NP98. [Google Scholar] [CrossRef]
- Azizzadeh, B.; Lu, R.J. Facial Nerve Considerations for the Deep Plane Facelift and Neck Lift. Facial Plast. Surg. 2024, 40, 687–693. [Google Scholar] [CrossRef]
- Surek, C.C.; Moorefield, A. Deep Plane Anatomy for the Facelift Surgeon: A Comprehensive Three-Dimensional Journey. Facial Plast. Surg. Clin. N. Am. 2022, 30, 205–214. [Google Scholar] [CrossRef] [PubMed]
- Talei, B.; Shauly, O.; Marxen, T.; Menon, A.; Gould, D.J. The Mastoid Crevasse and 3-Dimensional Considerations in Deep Plane Neck Lifting. Aesthet. Surg. J. 2024, 44, NP132–NP148. [Google Scholar] [CrossRef] [PubMed]
- Talei, B.; Ziai, H. The Detailed Anatomy of the Deep Plane of the Face and Neck with Current Nomenclature. Facial Plast. Surg. 2024, 40, 680–686. [Google Scholar] [CrossRef] [PubMed]
- Gordon, N.A.; Sawan, T.G. Deep-Plane Rhytidectomy: Pearls in Maximizing Outcomes while Minimizing Recovery. Facial Plast. Surg. 2025, 41, 2–11. [Google Scholar] [CrossRef]
- Sykes, J.; Dilger, A.; Cotofana, S. Demystifying the Deep Plane Facelift: What It Means Anatomically and Why It Works. Facial Plast. Surg. 2020, 36, 351–357. [Google Scholar] [CrossRef]
- Narasimhan, K.; Stuzin, J.M.; Rohrich, R.J. Five-step neck lift: Integrating anatomy with clinical practice to optimize results. Plast. Reconstr. Surg. 2013, 132, 339–350. [Google Scholar] [CrossRef]
- Minelli, L.; Wilson, J.L.; Bravo, F.G.; Hodgkinson, D.J.; O’Daniel, T.G.; van der Lei, B.; Mendelson, B.C. The Functional Anatomy and Innervation of the Platysma is Segmental: Implications for Lower Lip Dysfunction, Recurrent Platysmal Bands, and Surgical Rejuvenation. Aesthet. Surg. J. 2023, 43, 1091–1105. [Google Scholar] [CrossRef]
- Sinno, S.; Thorne, C.H. Cervical Branch of Facial Nerve: An Explanation for Recurrent Platysma Bands Following Necklift and Platysmaplasty. Aesthet. Surg. J. 2019, 39, 1–7. [Google Scholar] [CrossRef]
- Medhurst, R.; Tremblay, C.; Marrelli, K.; Best, C.; Jadeski, L.; Brace, M. Defining the Safe Entry Point in Deep Plane Facelifting with Novel Landmark for the Buccal Branch of the Facial Nerve. Plast. Reconstr. Surg.—Glob. Open 2024, 12, e5749. [Google Scholar] [CrossRef]
- Timberlake, A.T.; Cameron Brawley, C.; Paul, B.C.; Rosenberg, D.B. Complete Platysma Muscle Suspension in Deep-Plane Face-Lift Surgery. Plast. Reconstr. Surg. 2025, 155, 699e–703e. [Google Scholar] [CrossRef]
- Minelli, L.; Brown, C.P.; van der Lei, B.; Mendelson, B. Anatomy of the Facial Glideplanes, Deep Plane Spaces, and Ligaments: Implications for Surgical and Nonsurgical Lifting Procedures. Plast. Reconstr. Surg. 2024, 154, 95–110. [Google Scholar] [CrossRef]
- Jacono, A.A.; Parikh, S.S.; Kennedy, W.A. Anatomical comparison of platysmal tightening using superficial musculoaponeurotic system plication vs. deep-plane rhytidectomy techniques. Arch. Facial Plast. Surg. 2011, 13, 395–397. [Google Scholar] [CrossRef] [PubMed]
- Ozdemir, R.; Kilinç, H.; Unlü, R.E.; Uysal, A.C.; Sensöz, O.; Baran, C.N. Anatomicohistologic study of the retaining ligaments of the face and use in face lift: Retaining ligament correction and SMAS plication. Plast. Reconstr. Surg. 2002, 110, 1134–1147, discussion 1148–1149. [Google Scholar] [CrossRef] [PubMed]
- Furnas, D.W. The retaining ligaments of the cheek. Plast. Reconstr. Surg. 1989, 83, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Talei, B.; Ziai, H. Mandibular Ligament and the Prejowl Sulcus Explained. Aesthet. Surg. J. 2024, 44, 1131–1139. [Google Scholar] [CrossRef]
- Minelli, L.; Yang, H.M.; van der Lei, B.; Mendelson, B. The Surgical Anatomy of the Jowl and the Mandibular Ligament Reassessed. Aesthet. Plast. Surg. 2023, 47, 170–180. [Google Scholar] [CrossRef]
- Larson, J.D.; Tierney, W.S.; Ozturk, C.N.; Zins, J.E. Defining the fat compartments in the neck: A cadaver study. Aesthet. Surg. J. 2014, 34, 499–506. [Google Scholar] [CrossRef]
- Stuzin, J.M.; Rohrich, R.J.; Dayan, E. The Facial Fat Compartments Revisited: Clinical Relevance to Subcutaneous Dissection and Facial Deflation in Face Lifting. Plast. Reconstr. Surg. 2019, 144, 1070–1078. [Google Scholar] [CrossRef]
- O’Daniel, T.G. Understanding Deep Neck Anatomy and Its Clinical Relevance. Clin. Plast. Surg. 2018, 45, 447–454. [Google Scholar] [CrossRef]
- Aston, S.J.; Hanna, S.A. Platysma Hammock or Sling: Are They Different? Aesthet. Surg. J. 2023, 43, NP391–NP392. [Google Scholar] [CrossRef]
- Charafeddine, A.H.; Drake, R.; McBride, J.; Zins, J.E. Facelift: History and Anatomy. Clin. Plast. Surg. 2019, 46, 505–513. [Google Scholar] [CrossRef] [PubMed]
- Lemmon, M.L.; Hamra, S.T. Skoog rhytidectomy: A five-year experience with 577 patients. Plast. Reconstr. Surg. 1980, 65, 283–297. [Google Scholar] [CrossRef] [PubMed]
- Kaya, K.S.; Cakmak, O. Facelift Techniques: An Overview. Facial Plast. Surg. 2022, 38, 540–545. [Google Scholar] [CrossRef]
- Mariani, M.; Fabbri, M.; Serra, P.L.; Murone, V.; Scucchi, B.; Botti, C.; Botti, G. A Long-Term Evaluation: Deep Plane Versus High SMAS Face Lift. Facial Plast. Surg. 2025; Online ahead of print. [Google Scholar] [CrossRef]
- Hamra, S.T. The deep-plane rhytidectomy. Plast. Reconstr. Surg. 1990, 86, 53–61, discussion 62–63. [Google Scholar] [CrossRef]
- Hamra, S.T. Building the Composite Face Lift: A Personal Odyssey. Plast. Reconstr. Surg. 2016, 138, 85–96. [Google Scholar] [CrossRef]
- Jacono, A.A.; Bryant, L.M.; Ahmedli, N.N. A Novel Extended Deep Plane Facelift Technique for Jawline Rejuvenation and Volumization. Aesthet. Surg. J. 2019, 39, 1265–1281. [Google Scholar] [CrossRef]
- Zoumalan, R.; Rizk, S.S. Hematoma rates in drainless deep-plane face-lift surgery with and without the use of fibrin glue. Arch. Facial Plast. Surg. 2008, 10, 103–107. [Google Scholar] [CrossRef] [PubMed]
- Roskies, M.; Bray, D.; Gordon, N.A.; Gualdi, A.; Nayak, L.M.; Talei, B. Limited Delamination Modifications to the Extended Deep Plane Rhytidectomy: An Anatomical Basis for Improved Outcomes. Facial Plast. Surg. Aesthet. Med. 2024, 26, 657–664. [Google Scholar] [CrossRef]
- Sadati, K.; Mathieu, O.; Cetrulo, C.L., Jr.; Lellouch, A.G. Advancements in Face Lift Techniques: Preservation Face Lift With a Rotating Pedicle Flap. Plast. Reconstr. Surg.-Glob. Open. 2025, 13, e6619. [Google Scholar] [CrossRef]
- Baker, D.C. Deep dissection rhytidectomy: A plea for caution. Plast. Reconstr. Surg. 1994, 93, 1498–1499. [Google Scholar] [CrossRef]
- Jacono, A.A.; Alemi, A.S.; Russell, J.L. A Meta-Analysis of Complication Rates Among Different SMAS Facelift Techniques. Aesthet. Surg. J. 2019, 39, 927–942. [Google Scholar] [CrossRef] [PubMed]
- Webster, R.C.; Smith, R.C.; Smith, K.F. Face lift, Part 3: Plication of the superficial musculoaponeurotic system. Head Neck Surg. 1983, 6, 696–701. [Google Scholar] [CrossRef]
- Baker, D.C. Lateral SMASectomy. Plast. Reconstr. Surg. 1997, 100, 509–513. [Google Scholar] [CrossRef] [PubMed]
- Marten, T.J. High SMAS facelift: Combined single flap lifting of the jawline, cheek, and midface. Clin. Plast. Surg. 2008, 35, 569–603. [Google Scholar] [CrossRef]
- Rohrich, R.J.; Ghavami, A.; Lemmon, J.A.; Brown, S.A. The individualized component face lift: Developing a systematic approach to facial rejuvenation. Plast. Reconstr. Surg. 2009, 123, 1050–1063. [Google Scholar] [CrossRef]
- Stuzin, J.M.; Baker, T.J.; Gordon, H.L.; Baker, T.M. Extended SMAS dissection as an approach to midface rejuvenation. Clin. Plast. Surg. 1995, 22, 295–311. [Google Scholar] [CrossRef]
- Avashia, Y.J.; Stuzin, J.M.; Cason, R.W.; Savetsky, I.L.; Rohrich, R.J. An Evidence-Based and Case-Based Comparison of Modern Face Lift Techniques. Plast. Reconstr. Surg. 2023, 152, 51e–65e. [Google Scholar] [CrossRef]
- Rohrich, R.J.; Sinno, S.; Vaca, E.E. Getting Better Results in Facelifting. Plast. Reconstr. Surg. Glob. Open 2019, 7, e2270. [Google Scholar] [CrossRef] [PubMed]
- Quatela, V.C.; Azzi, J.P.; Antunes, M.B. Endoscopic-assisted facelifting. Facial Plast. Surg. 2014, 30, 413–421. [Google Scholar] [CrossRef]
- Ramirez, O.M. Endoscopic full facelift. Aesthet. Plast. Surg. 1994, 18, 363–371. [Google Scholar] [CrossRef]
- Tonnard, P.; Verpaele, A.; Monstrey, S.; Van Landuyt, K.; Blondeel, P.; Hamdi, M.; Matton, G. Minimal access cranial suspension lift: A modified S-lift. Plast. Reconstr. Surg. 2002, 109, 2074–2086. [Google Scholar] [CrossRef] [PubMed]
- Kao, C.C.; Duscher, D. The Ponytail Lift: 22 Years of Experience in 600 Cases of Endoscopic Deep Plane Facial Rejuvenation. Aesthet. Surg. J. 2024, 44, 671–692. [Google Scholar] [CrossRef]
- Mani, M. Endoscopic, “Scarless” Composite Flap Face and Neck Lift. Facial Plast. Surg. 2025, 41, 43–53. [Google Scholar] [CrossRef] [PubMed]
- Alpert, B.S.; Baker, D.C.; Hamra, S.T.; Owsley, J.Q.; Ramirez, O. Identical twin face lifts with differing techniques: A 10-year follow-up. Plast. Reconstr. Surg. 2009, 123, 1025–1033. [Google Scholar] [CrossRef]
- Ivy, E.J.; Lorenc, Z.P.; Aston, S.J. Is there a difference? A prospective study comparing lateral and standard SMAS face lifts with extended SMAS and composite rhytidectomies. Plast. Reconstr. Surg. 1996, 98, 1135–1143, discussion 1144–1147. [Google Scholar] [CrossRef]
- Aston, S.J. Platysma-SMAS cervicofacial rhytidoplasty. Clin. Plast. Surg. 1983, 10, 507–520. [Google Scholar] [CrossRef] [PubMed]
- Sedgh, J.; Fedok, F.G. Different Faces: Different Facelift Techniques. Facial Plast. Surg. 2020, 36, 386–394. [Google Scholar] [CrossRef]
- Marten, T.; Elyassnia, D. Management of the Platysma in Neck Lift. Clin. Plast. Surg. 2018, 45, 555–570. [Google Scholar] [CrossRef]
- Chinta, S.R.; Brydges, H.T.; Laspro, M.; Shah, A.R.; Cohen, J.; Ceradini, D.J. Current Trends in Deep Plane Neck Lifting: A Systematic Review. Ann. Plast. Surg. 2025, 94, 222–228. [Google Scholar] [CrossRef]
- Ghoraba, S.M. Deep Tissue Sculpture in Neck Rejuvenation: Review of 641 Consecutive Cases. Plast. Reconstr. Surg.—Glob. Open. 2024, 12, e6364. [Google Scholar] [CrossRef]
- Marten, T.; Elyassnia, D. Deep Neck Lift: Defining Anatomical Problems and Choosing Appropriate Treatment Strategies. Facial Plast. Surg. 2022, 38, 630–649. [Google Scholar] [CrossRef] [PubMed]
- Aston, S.J. Platysma muscle in rhytidoplasty. Ann. Plast. Surg. 1979, 3, 529–539. [Google Scholar] [CrossRef]
- Sozer, S.O.; Sibar, S.; Kachare, M.D. Progressive Contouring of the Platysma With Barbed Sutures. Aesthet. Surg. J. 2024, 44, 449–462. [Google Scholar] [CrossRef] [PubMed]
- Jacono, A.A.; Talei, B. Vertical neck lifting. Facial Plast. Surg. Clin. N. Am. 2014, 22, 285–316. [Google Scholar] [CrossRef] [PubMed]
- Jacono, A.A.; Alemi, A.S.; Harmon, J.J.; Ahmedli, N. The Effect of a Novel Platysma Hammock Flap During Extended Deep Plane Facelift on the Signs of Aging in the Neck. Aesthet. Surg. J. 2022, 42, 845–857. [Google Scholar] [CrossRef]
- Bartow, M.J.; Core, G. Effective Recontouring of the Neck by Complete Platysmal Transection. Aesthet. Surg. J. 2025, 45, 448–453. [Google Scholar] [CrossRef]
- Benslimane, F.; Kleidona, I.A.; Cintra, H.P.L.; Ghanem, A.M. Partial Removal of the Submaxillary Gland for Aesthetic Indications: A Systematic Review and Critical Analysis of the Evidence. Aesthet. Plast. Surg. 2020, 44, 339–348. [Google Scholar] [CrossRef]
- Grotting, J.C.; O’Daniel, T.G. Discussion: LigaSure-Assisted Submandibular Gland Excision in Deep-Plane Neck Lift: Review of 83 Patients. Plast. Reconstr. Surg. 2025, 155, 46–48. [Google Scholar] [CrossRef]
- Basaran, K.; Comert, M. LigaSure-Assisted Submandibular Gland Excision in Deep-Plane Neck Lift: Review of 83 Patients. Plast. Reconstr. Surg. 2025, 155, 35–45. [Google Scholar] [CrossRef]
- Pupić-Bakrač, J.; Pupić-Bakrač, A. LigaSure-Assisted Submandibular Gland Excision in Deep-Plane Neck Lift: Review of 83 Patients. Plast. Reconstr. Surg. 2025; ahead of printing. [Google Scholar] [CrossRef]
- Wever, C.C. Deep Neck Lifting. Facial Plast. Surg. 2024, 40, 710–716. [Google Scholar] [CrossRef]
- Jacono, A.A.; Malone, M.H.; Lavin, T.J. Nonsurgical Facial Rejuvenation Procedures in Patients Under 50 Prior to Undergoing Facelift: Habits, Costs, and Results. Aesthet. Surg. J. 2017, 37, 448–453. [Google Scholar] [CrossRef] [PubMed]
- Hammoudeh, Z.S.; Stevens, W.G. Nonsurgical Adjuncts Following Facelift to Achieve Optimal Aesthetic Outcomes: “Icing on the Cake”. Clin. Plast. Surg. 2019, 46, 613–623. [Google Scholar] [CrossRef]
- Talei, B.; Gould, D.; Ziai, H. Vectorial Analysis of Deep Plane Face and Neck Lift. Aesthet. Surg. J. 2024, 44, 1015–1022. [Google Scholar] [CrossRef]
- Viterbo, F.; Auersvald, A.; O’Daniel, T.G. Gliding Brow Lift (GBL): A New Concept. Aesthet. Plast. Surg. 2019, 43, 1536–1546. [Google Scholar] [CrossRef]
- Zins, J.E.; Coombs, D.M. Endoscopic Brow Lift. Clin. Plast. Surg. 2022, 49, 357–363. [Google Scholar] [CrossRef]
- Orra, S.; Bald, M.; Wagner, G.; Grotting, J.C. The Gliding Brow Lift: An Analysis of Outcomes and Maintenance of Lift in a Single Surgeon’s Practice. Aesthet. Surg. J. 2025, 45, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Pascali, M.; Massarelli, O. The Temporal Subcutaneous Brow Lift with Orbicularis Oculi Muscle Elastic Flap: Technical Considerations, Systematic Review, and Terminology Standardization. Facial Plast. Surg. 2023, 39, 691–702. [Google Scholar] [CrossRef]
- Savetsky, I.L.; Cohen, J.M.; Matarasso, A. Subcutaneous Lateral Temporal Lift. Clin. Plast. Surg. 2022, 49, 365–375. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; Wang, X.; Qiao, Z.; Yang, K. Different Techniques and Quantitative Measurements in Upper lip lift: A Systematic Review. Aesthet. Plast. Surg. 2023, 47, 1364–1376. [Google Scholar] [CrossRef]
- Kubo, T. Buccal Fat Pad Excision for Facial Rejuvenation: The Relationship Between the Resected Position and Its Influence on Facial Shape and Volume. Aesthet. Surg. J. Open Forum. 2023, 5, ojad089. [Google Scholar] [CrossRef]
- Roberts, T.L., III. The emerging role of laser resurfacing in combination with traditional aesthetic facial plastic surgery. Aesthet. Plast. Surg. 1998, 22, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Britt, C.J.; Marcus, B. Energy-Based Facial Rejuvenation: Advances in Diagnosis and Treatment. JAMA Facial Plast. Surg. 2017, 19, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Zimbler, M.S.; Nassif, P.S. Adjunctive applications for botulinum toxin in facial aesthetic surgery. Facial Plast. Surg. Clin. N. Am. 2003, 11, 477–482. [Google Scholar] [CrossRef] [PubMed]
- Fisher, S.M.; Borab, Z.; Weir, D.; Rohrich, R.J. The emerging role of biostimulators as an adjunct in facial rejuvenation: A systematic review. J. Plast. Reconstr. Aesthet. Surg. 2024, 92, 118–129. [Google Scholar] [CrossRef]
- Cruciani, M.; Masiello, F.; Pati, I.; Pupella, S.; De Angelis, V. Platelet rich plasma for facial rejuvenation: An overview of systematic reviews. Blood Transfus. 2024, 22, 429–440. [Google Scholar] [CrossRef]
- Wisniewski, J.D.; Ellis, D.L.; Lupo, M.P. Facial rejuvenation: Combining cosmeceuticals with cosmetic procedures. Cutis 2014, 94, 122–126. [Google Scholar]
- Nahai, F.; Bassiri-Tehrani, B.; Santosa, K.B. Hematomas and the Facelift Surgeon: It’s Time for Us to Break Up for Good. Aesthet. Surg. J. 2023, 43, 1207–1209. [Google Scholar] [CrossRef]
- Baker, D.C.; Stefani, W.A.; Chiu, E.S. Reducing the incidence of hematoma requiring surgical evacuation following male rhytidectomy: A 30-year review of 985 cases. Plast. Reconstr. Surg. 2005, 116, 1973–1985, discussion 1986–1987. [Google Scholar] [CrossRef]
- Rees, T.D.; Barone, C.M.; Valauri, F.A.; Ginsberg, G.D.; Nolan, W.B., III. Hematomas requiring surgical evacuation following face lift surgery. Plast. Reconstr. Surg. 1994, 93, 1185–1190. [Google Scholar] [CrossRef]
- Ramanadham, S.R.; Mapula, S.; Costa, C.; Narasimhan, K.; Coleman, J.E.; Rohrich, R.J. Evolution of hypertension management in face lifting in 1089 patients: Optimizing safety and outcomes. Plast. Reconstr. Surg. 2015, 135, 1037–1043. [Google Scholar] [CrossRef]
- Trussler, A.P.; Hatef, D.A.; Rohrich, R.J. Management of hypertension in the facelift patient: Results of a national consensus survey. Aesthet. Surg. J. 2011, 31, 493–500. [Google Scholar] [CrossRef] [PubMed]
- Jones, B.M.; Grover, R. Avoiding hematoma in cervicofacial rhytidectomy: A personal 8-year quest. Reviewing 910 patients. Plast. Reconstr. Surg. 2004, 113, 381–387, discussion 388–390. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.T.; Blackwell, S.J.; Lewis, S.R. Routine use of a suction drain in facial rhytidoplasty. Ann. Plast. Surg. 1987, 18, 30–33. [Google Scholar] [CrossRef] [PubMed]
- Jones, B.M.; Grover, R.; Hamilton, S. The efficacy of surgical drainage in cervicofacial rhytidectomy: A prospective, randomized, controlled trial. Plast. Reconstr. Surg. 2007, 120, 263–270. [Google Scholar] [CrossRef]
- Flemming, I. Fibrin glue in face lifts. Facial Plast. Surg. 1992, 8, 79–88. [Google Scholar] [CrossRef] [PubMed]
- Fezza, J.P.; Cartwright, M.; Mack, W.; Flaharty, P. The use of aerosolized fibrin glue in face-lift surgery. Plast. Reconstr. Surg. 2002, 110, 658–664, discussion 665–666. [Google Scholar] [CrossRef]
- Auersvald, A.; Auersvald, L.A. Hemostatic net in rhytidoplasty: An efficient and safe method for preventing hematoma in 405 consecutive patients. Aesthet. Plast. Surg. 2014, 38, 1–9. [Google Scholar] [CrossRef]
- Janssen, T.J.; Maheshwari, K.; Sivadasan, A.; Waterhouse, N. Hemostatic Net in Facelift Surgery: A 5-Year Single-Surgeon Experience. Aesthet. Surg. J. 2023, 43, 1106–1111. [Google Scholar] [CrossRef]
- Brown, S.; Brown, T.; Rohrich, R.J. Clinical Applications of Tranexamic Acid in Plastic and Reconstructive Surgery. Plast. Reconstr. Surg. 2024, 154, 1253e–1263e. [Google Scholar] [CrossRef]
- Couto, R.A.; Charafeddine, A.; Sinclair, N.R.; Nayak, L.M.; Zins, J.E. Local Infiltration of Tranexamic Acid With Local Anesthetic Reduces Intraoperative Facelift Bleeding: A Preliminary Report. Aesthet. Surg. J. 2020, 40, 587–593. [Google Scholar] [CrossRef]
- Cohen, J.C.; Glasgold, R.A.; Alloju, L.M.; Glasgold, M.J. Effects of Intravenous Tranexamic Acid During Rhytidectomy: A Randomized, Controlled, Double-Blind Pilot Study. Aesthet. Surg. J. 2021, 41, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Davison, S.P.; Ellor, M.; Hedicke, C.; Groth, J.; Grimmer, K. Comparison of Tranexamic Acid Administration Methods in Rhytidectomy: A Prospective, Randomized, Double-blind Study. Plast. Reconstr. Surg.—Glob. Open. 2025, 13, e6559. [Google Scholar] [CrossRef] [PubMed]
- ElAbd, R.; Richa, Y.; Pu, L.; Hiyzajie, T.; Safran, T.; Gilardino, M. Evaluation of the safety and efficacy of tranexamic acid use in face and neck lift surgery: A systematic review. J. Plast. Reconstr. Aesthet. Surg. 2025, 104, 369–385. [Google Scholar] [CrossRef]
- Ors, S. High Superficial Musculoaponeurotic System Lamellar Facelift Under Local Anesthesia. J. Craniofac. Surg. 2021, 32, 1788–1793. [Google Scholar] [CrossRef] [PubMed]
- DeJoseph, L.M.; Pou, J.D. Local Anesthetic Facelift. Facial Plast. Surg. Clin. N. Am. 2020, 28, 409–418. [Google Scholar] [CrossRef]
- Moris, V.; Bensa, P.; Gerenton, B.; Rizzi, P.; Cristofari, S.; Zwetyenga, N.; Guilier, D. The cervicofacial lift under pure local anaesthesia diminishes the incidence of post-operative haematoma. J. Plast. Reconstr. Aesthet. Surg. 2019, 72, 821–829. [Google Scholar] [CrossRef]
- Gallo, L.; Kim, P.; Yuan, M.; Gallo, M.; Thoma, A.; Voineskos, S.H.; Cano, S.J.; Pusic, A.L.; Klassen, A.F. Best Practices for FACE-Q Aesthetics Research: A Systematic Review of Study Methodology. Aesthet. Surg. J. 2023, 43, NP674–NP686. [Google Scholar] [CrossRef]


| Technique | Examples |
|---|---|
| Superficial | Subcutaneous |
| SMAS manipulation | SMASectomy SMAS plication SMAS stacking |
| SMAS elevation | High SMAS SMAS flap/extended SMAS Deep plane Composite |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boyd, C.J.; Ceradini, D.J. Current Trends in Facelift and Necklift Procedures. J. Clin. Med. 2025, 14, 4273. https://doi.org/10.3390/jcm14124273
Boyd CJ, Ceradini DJ. Current Trends in Facelift and Necklift Procedures. Journal of Clinical Medicine. 2025; 14(12):4273. https://doi.org/10.3390/jcm14124273
Chicago/Turabian StyleBoyd, Carter J., and Daniel J. Ceradini. 2025. "Current Trends in Facelift and Necklift Procedures" Journal of Clinical Medicine 14, no. 12: 4273. https://doi.org/10.3390/jcm14124273
APA StyleBoyd, C. J., & Ceradini, D. J. (2025). Current Trends in Facelift and Necklift Procedures. Journal of Clinical Medicine, 14(12), 4273. https://doi.org/10.3390/jcm14124273






