Low-Density Lipoprotein Cholesterol Reduction and Therapeutic Adherence During Cardiac Rehabilitation After Myocardial Infarction
Abstract
1. Introduction
2. Materials and Methods
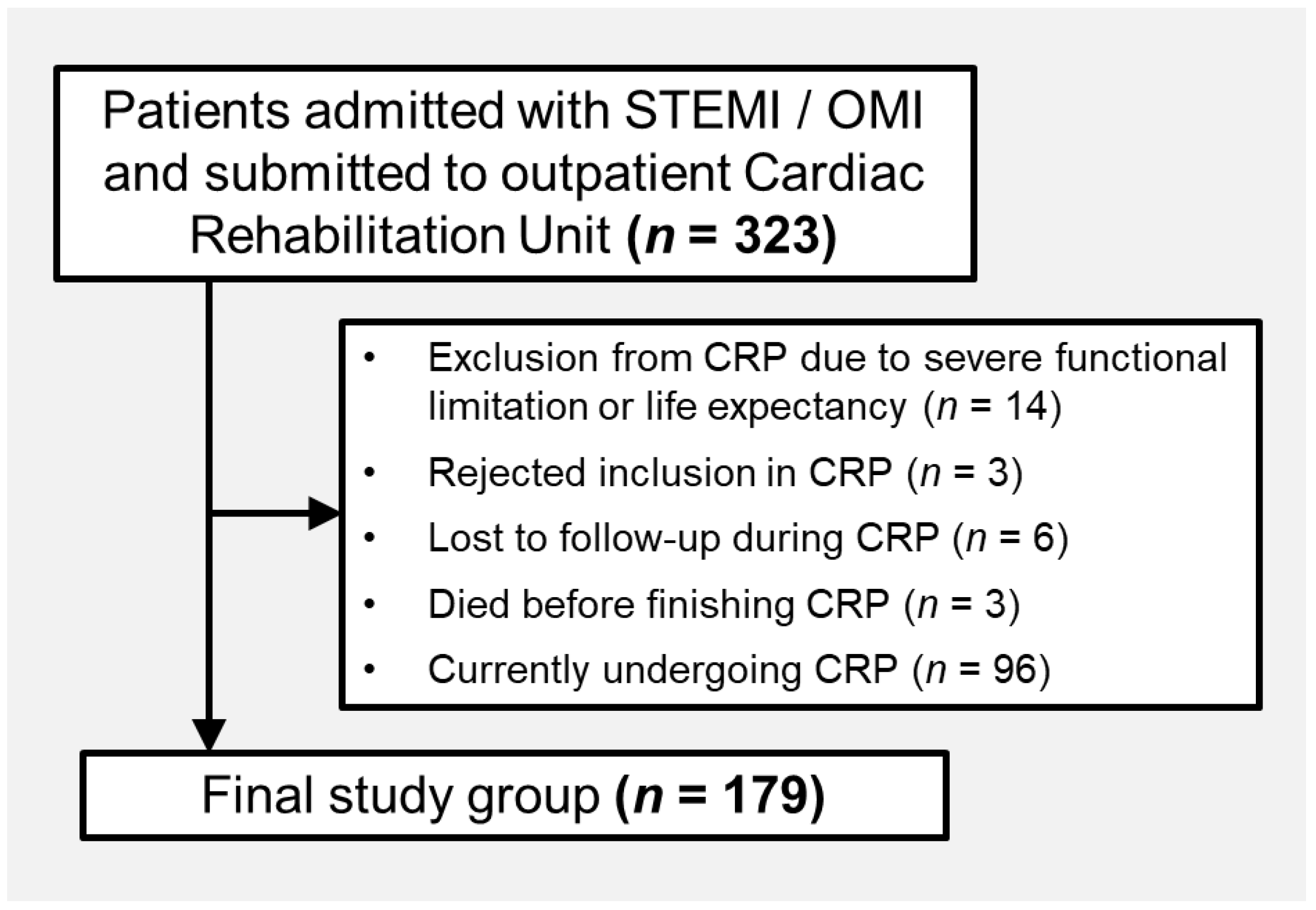
2.1. Population
2.2. Cardiac Rehabilitation Program
2.3. Lipid Profile and LLT Analysis
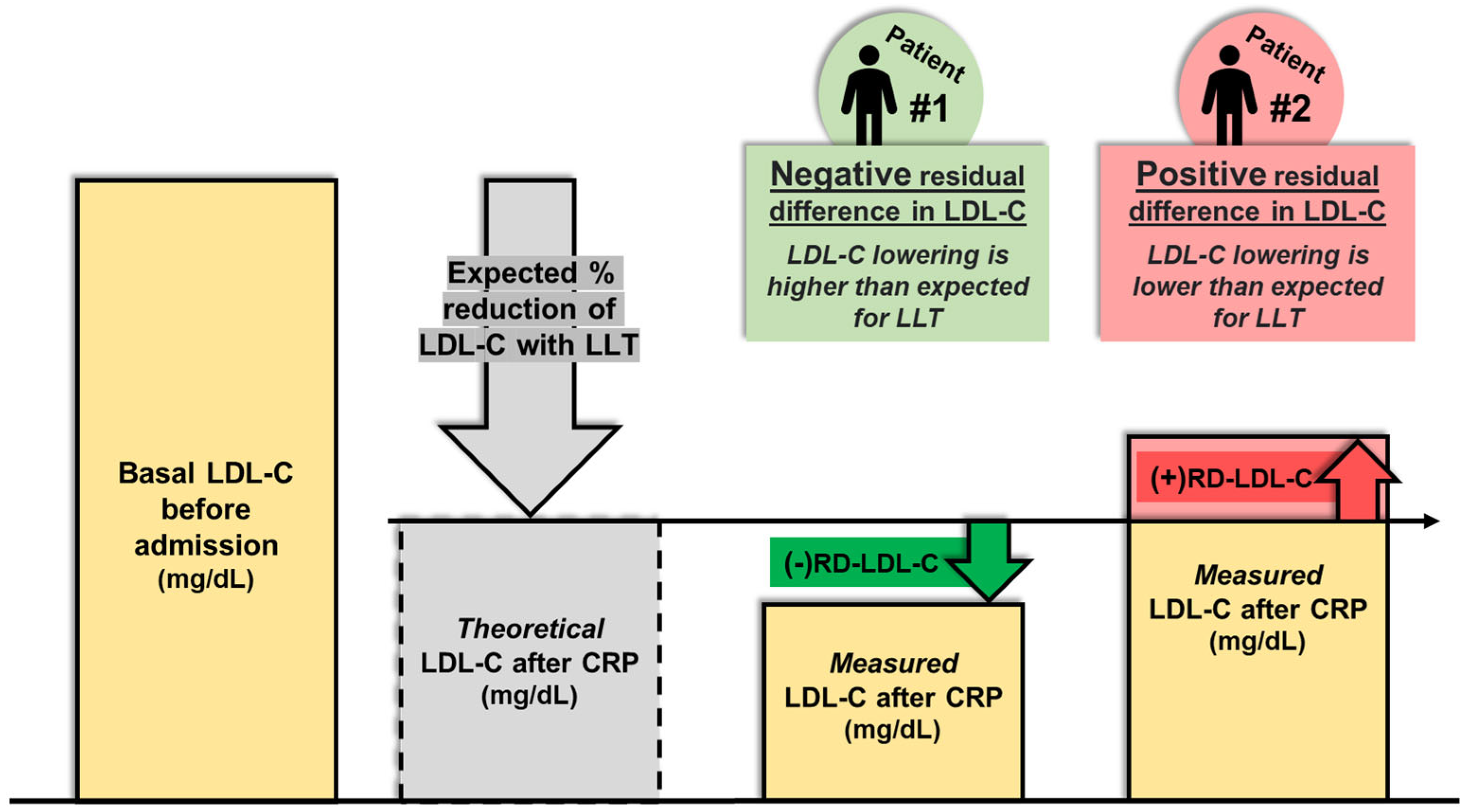
2.4. Corrected Basal LDL-C and Theoretical Potency of LLT
2.5. Residual Difference in LDL-C
2.6. CRP Outcomes
2.7. Objetive of the Study
2.8. Ethics
2.9. Statistical Analysis
3. Results
3.1. Cohort Description
3.2. Lipid-Lowering Therapy Before and After Phase 2 CRP
3.3. Residual Difference in LDL-C
3.4. Predictors of Positive Residual Difference in LDL-C
4. Discussion
4.1. Post-MI LDL-C Goals and Cardiac Rehabilitation
4.2. Lifestyle Habits, Therapeutic Adherence, and Therapeutic Inertia
4.3. Predictors of Positive RD-LDL-C
4.4. Implications for Clinical Practice
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AUC | Area under the curve |
| BMI | Body mass index |
| CET | Conventional exercise testing |
| CI | Confidence Interval |
| CPET | Cardiopulmonary exercise testing |
| CRP | Cardiac Rehabilitation Program |
| GAD-2 | Generalized Anxiety Disorder 2-item |
| GRACE | Global Registry of Acute Coronary Events |
| HDL-C | High-density lipoprotein cholesterol |
| HR | Hazard ratio |
| IPAQ | International Physical Activity Questionnaire |
| LDL-C | Low-Density Lipoprotein Cholesterol |
| LLT | Lipid-lowering therapy |
| LVEF | Left Ventricular Ejection Fraction |
| METS | Metabolic equivalents |
| MI | Myocardial Infarction |
| OMI | Occlusion Myocardial Infarction |
| PHQ-2 | Patient Health Questionnaire 2-item |
| RD-LDL-C | Residual difference in LDL-C |
| ROC | Receiver operating characteristic |
| SF-36 | 36-Item Short Form Survey Instrument |
| SPSS | Statistical Package for the Social Sciences |
| STEMI | ST-segment Elevation Myocardial Infarction |
| TG | Triglycerides |
| VO2 | Oxygen consumption |
References
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.-M.; Capodanno, D.; et al. 2021 ESC Guidelines on Cardiovascular Disease Prevention in Clinical Practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef] [PubMed]
- Ference, B.A.; Ginsberg, H.N.; Graham, I.; Ray, K.K.; Packard, C.J.; Bruckert, E.; Hegele, R.A.; Krauss, R.M.; Raal, F.J.; Schunkert, H.; et al. Low-Density Lipoproteins Cause Atherosclerotic Cardiovascular Disease. 1. Evidence from Genetic, Epidemiologic, and Clinical Studies. A Consensus Statement from the European Atherosclerosis Society Consensus Panel. Eur. Heart J. 2017, 38, 2459–2472. [Google Scholar] [CrossRef] [PubMed]
- Mensah, G.A.; Roth, G.A.; Fuster, V. The Global Burden of Cardiovascular Diseases and Risk Factors. J. Am. Coll. Cardiol. 2019, 74, 2529–2532. [Google Scholar] [CrossRef] [PubMed]
- Byrne, R.A.; Rossello, X.; Coughlan, J.J.; Barbato, E.; Berry, C.; Chieffo, A.; Claeys, M.J.; Dan, G.-A.; Dweck, M.R.; Galbraith, M.; et al. 2023 ESC Guidelines for the Management of Acute Coronary Syndromes. Eur. Heart J. 2023, 44, 3720–3826. [Google Scholar] [CrossRef]
- Knuuti, J.; Wijns, W.; Saraste, A.; Capodanno, D.; Barbato, E.; Funck-Brentano, C.; Prescott, E.; Storey, R.F.; Deaton, C.; Cuisset, T.; et al. 2019 ESC Guidelines for the Diagnosis and Management of Chronic Coronary Syndromes. Eur. Heart J. 2020, 41, 407–477. [Google Scholar] [CrossRef]
- Rao, S.V.; O’Donoghue, M.L.; Ruel, M.; Rab, T.; Tamis-Holland, J.E.; Alexander, J.H.; Baber, U.; Baker, H.; Cohen, M.G.; Cruz-Ruiz, M.; et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI Guideline for the Management of Patients With Acute Coronary Syndromes: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2025, 151, e771–e862. [Google Scholar] [CrossRef]
- Chen, Y.-C.; Tsai, J.-C.; Liou, Y.-M.; Chan, P. Effectiveness of Endurance Exercise Training in Patients with Coronary Artery Disease: A Meta-Analysis of Randomised Controlled Trials. Eur. J. Cardiovasc. Nurs. 2017, 16, 397–408. [Google Scholar] [CrossRef]
- Javaherian, M.; Dabbaghipour, N.; Mohammadpour, Z.; Attarbashi Moghadam, B. The Role of the Characteristics of Exercise-Based Cardiac Rehabilitation Program in the Improvement of Lipid Profile Level: A Systematic Review and Meta-Analysis. ARYA Atheroscler. 2020, 16, 192–207. [Google Scholar] [CrossRef]
- Wu, G.; Hu, Y.; Ding, K.; Li, X.; Li, J.; Shang, Z. The Effect of Cardiac Rehabilitation on Lipid Levels in Patients with Coronary Heart Disease. A Systematic Review and Meta-Analysis. Glob. Heart 2022, 17, 83. [Google Scholar] [CrossRef]
- Anderson, L.; Oldridge, N.; Thompson, D.R.; Zwisler, A.-D.; Rees, K.; Martin, N.; Taylor, R.S. Exercise-Based Cardiac Rehabilitation for Coronary Heart Disease. J. Am. Coll. Cardiol. 2016, 67, 1–12. [Google Scholar] [CrossRef]
- Salzwedel, A.; Jensen, K.; Rauch, B.; Doherty, P.; Metzendorf, M.-I.; Hackbusch, M.; Völler, H.; Schmid, J.-P.; Davos, C.H. Effectiveness of Comprehensive Cardiac Rehabilitation in Coronary Artery Disease Patients Treated According to Contemporary Evidence Based Medicine: Update of the Cardiac Rehabilitation Outcome Study (CROS-II). Eur. J. Prev. Cardiol. 2020, 27, 1756–1774. [Google Scholar] [CrossRef] [PubMed]
- Van Halewijn, G.; Deckers, J.; Tay, H.Y.; Van Domburg, R.; Kotseva, K.; Wood, D. Lessons from Contemporary Trials of Cardiovascular Prevention and Rehabilitation: A Systematic Review and Meta-Analysis. Int. J. Cardiol. 2017, 232, 294–303. [Google Scholar] [CrossRef] [PubMed]
- Santiago De Araújo Pio, C.; Marzolini, S.; Pakosh, M.; Grace, S.L. Effect of Cardiac Rehabilitation Dose on Mortality and Morbidity: A Systematic Review and Meta-Regression Analysis. Mayo Clin. Proc. 2017, 92, 1644–1659. [Google Scholar] [CrossRef]
- Bertolín-Boronat, C.; Marcos-Garcés, V.; Merenciano-González, H.; Martínez Mas, M.L.; Climent Alberola, J.I.; Perez, N.; López-Bueno, L.; Esteban Argente, M.C.; Valls Reig, M.; Arizón Benito, A.; et al. Depression, Anxiety, and Quality of Life in a Cardiac Rehabilitation Program Without Dedicated Mental Health Resources Post-Myocardial Infarction. J. Cardiovasc. Dev. Dis. 2025, 12, 92. [Google Scholar] [CrossRef]
- Cosin-Sales, J.; Sidelnikov, E.; Villamayor, S.; Fernández, M.; Merino-Montero, S.; Zamora, A. Identification of Secondary Prevention Patients Eligible for PCSK9 Inhibitors Therapy According to the Routine Clinical Practice in Spain. Adv. Ther. 2023, 40, 2710–2724. [Google Scholar] [CrossRef]
- Ray, K.K.; Molemans, B.; Schoonen, W.M.; Giovas, P.; Bray, S.; Kiru, G.; Murphy, J.; Banach, M.; De Servi, S.; Gaita, D.; et al. EU-Wide Cross-Sectional Observational Study of Lipid-Modifying Therapy Use in Secondary and Primary Care: The DA VINCI Study. Eur. J. Prev. Cardiol. 2021, 28, 1279–1289. [Google Scholar] [CrossRef]
- De Backer, G.; Jankowski, P.; Kotseva, K.; Mirrakhimov, E.; Reiner, Ž.; Rydén, L.; Tokgözoğlu, L.; Wood, D.; De Bacquer, D.; De Backer, G.; et al. Management of Dyslipidaemia in Patients with Coronary Heart Disease: Results from the ESC-EORP EUROASPIRE V Survey in 27 Countries. Atherosclerosis 2019, 285, 135–146. [Google Scholar] [CrossRef]
- Grau, M.; Elosua, R.; Cabrera De León, A.; Guembe, M.J.; Baena-Díez, J.M.; Vega Alonso, T.; Javier Félix, F.; Zorrilla, B.; Rigo, F.; Lapetra, J.; et al. Factores de riesgo cardiovascular en España en la primera década del siglo xxi: Análisis agrupado con datos individuales de 11 estudios de base poblacional, estudio DARIOS. Rev. Esp. Cardiol. 2011, 64, 295–304. [Google Scholar] [CrossRef] [PubMed]
- Cosín Sales, J.; Escobar Cervantes, C.; Gómez-Barrado, J.J.; Andreu Cayuelas, J.M.; García Del Egido, A.; Castro Martín, J.J.; Huelmos Rodrigo, A.I.; Corbi-Pascual, M.; Varela Cancelo, A.; Vidal-Pérez, R.; et al. Impact of Therapeutic Inertia in Lipid-Lowering Therapy in Patients at Very High Cardiovascular Risk. Clin. Investig. Arterioscler. 2025, 500773. [Google Scholar] [CrossRef]
- Faggiano, A.; Gualeni, A.; Barbieri, L.; Mureddu, G.F.; Venturini, E.; Giallauria, F.; Ambrosetti, M.; Ruzzolini, M.; Maranta, F.; Silverii, M.V.; et al. Therapeutic Inertia in Dyslipidemia Management for Secondary Cardiovascular Prevention: Results from the Italian ITACARE-P Network. J. Clin. Med. 2025, 14, 493. [Google Scholar] [CrossRef]
- Dixon, D.L.; Sharma, G.; Sandesara, P.B.; Yang, E.; Braun, L.T.; Mensah, G.A.; Sperling, L.S.; Deedwania, P.C.; Virani, S.S. Therapeutic Inertia in Cardiovascular Disease Prevention. J. Am. Coll. Cardiol. 2019, 74, 1728–1731. [Google Scholar] [CrossRef] [PubMed]
- Zheng, E.; Madura, P.; Grandos, J.; Broncel, M.; Pawlos, A.; Woźniak, E.; Gorzelak-Pabiś, P. When the Same Treatment Has Different Response: The Role of Pharmacogenomics in Statin Therapy. Biomed. Pharmacother. 2024, 170, 115966. [Google Scholar] [CrossRef] [PubMed]
- Patnaik, S.; Pollevick, M.E.; Lara-Breitinger, K.M.; Stone, N.J. Inter-Individual Variability in Lipid Response: A Narrative Review. Am. J. Med. 2022, 135, 1427–1433.e7. [Google Scholar] [CrossRef]
- Velasco (Coordinador), J.A.; Cosín, J.; Maroto, J.M.; Muñiz, J.; Casasnovas, J.A.; Plaza, I.; Tomás Abadal, L. Guías de práctica clínica de la Sociedad Española de Cardiología en prevención cardiovascular y rehabilitación cardíaca. Rev. Esp. Cardiol. 2000, 53, 1095–1120. [Google Scholar] [CrossRef]
- Ambrosetti, M.; Abreu, A.; Corrà, U.; Davos, C.H.; Hansen, D.; Frederix, I.; Iliou, M.C.; Pedretti, R.F.E.; Schmid, J.-P.; Vigorito, C.; et al. Secondary Prevention through Comprehensive Cardiovascular Rehabilitation: From Knowledge to Implementation. 2020 Update. A Position Paper from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur. J. Prev. Cardiol. 2021, 28, 460–495. [Google Scholar] [CrossRef]
- AACVPR Stratification Algorithm for Risk of Event. Available online: https://www.aacvpr.org/Portals/0/2014_AACVPR-Risk-Stratification-Algorithm.pdf (accessed on 12 May 2025).
- Marcos-Garcés, V.; Merenciano-González, H.; Martínez Mas, M.L.; Palau, P.; Climent Alberola, J.I.; Perez, N.; López-Bueno, L.; Esteban Argente, M.C.; Valls Reig, M.; Muñoz Alcover, R.; et al. Short-Course High-Intensity Statin Treatment during Admission for Myocardial Infarction and LDL-Cholesterol Reduction—Impact on Tailored Lipid-Lowering Therapy at Discharge. J. Clin. Med. 2023, 13, 127. [Google Scholar] [CrossRef] [PubMed]
- Bertolín-Boronat, C.; Merenciano-González, H.; Marcos-Garcés, V.; Martínez-Mas, M.L.; Climent Alberola, J.I.; Pérez, N.; López-Bueno, L.; Esteban-Argente, M.C.; Valls Reig, M.; Arizón Benito, A.; et al. Dynamics of HDL-Cholesterol Following a Post-Myocardial Infarction Cardiac Rehabilitation Program. Rev. Cardiovasc. Med. 2025, 26, 25399. [Google Scholar] [CrossRef]
- Bertolín-Boronat, C.; Marcos-Garcés, V.; Merenciano-González, H.; Martínez Mas, M.L.; Climent Alberola, J.I.; Perez, N.; López Bueno, L.; Esteban Argente, M.C.; Valls Reig, M.; Arizón Benito, A.; et al. Familial Hypercholesterolemia Screening in a Cardiac Rehabilitation Program After Myocardial Infarction. Cardiogenetics 2025, 15, 6. [Google Scholar] [CrossRef]
- Masana, L.; Ibarretxe, D.; Plana, N. Reasons Why Combination Therapy Should Be the New Standard of Care to Achieve the LDL-Cholesterol Targets: Lipid-Lowering Combination Therapy. Curr. Cardiol. Rep. 2020, 22, 66. [Google Scholar] [CrossRef]
- Cholesterol Treatment Trialists’ (Ctt) Collaboration; Baigent, C.; Blackwell, L.; Emberson, J.; Holland, L.E.; Reith, C.; Bhala, N.; Peto, R.; Barnes, E.H.; Keech, A.; et al. Efficacy and Safety of More Intensive Lowering of LDL Cholesterol: A Meta-Analysis of Data from 170 000 Participants in 26 Randomised Trials. Lancet 2010, 376, 1670–1681. [Google Scholar] [CrossRef]
- Cholesterol Treatment Trialists’ (Ctt) Collaborators; Mihaylova, B.; Emberson, J.; Blackwell, L.; Keech, A.; Simes, J.; Barnes, E.H.; Voysey, M.; Gray, A.; Collins, R.; et al. The Effects of Lowering LDL Cholesterol with Statin Therapy in People at Low Risk of Vascular Disease: Meta-Analysis of Individual Data from 27 Randomised Trials. Lancet 2012, 380, 581–590. [Google Scholar] [CrossRef]
- Leening, M.J.G. Overcoming Therapeutic Inertia in LDL Cholesterol-Lowering Treatment with Education and Simplified Treatment Algorithms. Neth. Heart J. 2024, 32, 198–199. [Google Scholar] [CrossRef] [PubMed]
- Phillips, L.S.; Branch, W.T.; Cook, C.B.; Doyle, J.P.; El-Kebbi, I.M.; Gallina, D.L.; Miller, C.D.; Ziemer, D.C.; Barnes, C.S. Clinical Inertia. Ann. Intern. Med. 2001, 135, 825–834. [Google Scholar] [CrossRef]
- Lavoie, K.L.; Rash, J.A.; Campbell, T.S. Changing Provider Behavior in the Context of Chronic Disease Management: Focus on Clinical Inertia. Annu. Rev. Pharmacol. Toxicol. 2017, 57, 263–283. [Google Scholar] [CrossRef] [PubMed]
- Descamps, O.; Tomassini, J.E.; Lin, J.; Polis, A.B.; Shah, A.; Brudi, P.; Hanson, M.E.; Tershakovec, A.M. Variability of the LDL-C Lowering Response to Ezetimibe and Ezetimibe + Statin Therapy in Hypercholesterolemic Patients. Atherosclerosis 2015, 240, 482–489. [Google Scholar] [CrossRef]
- Makhmudova, U.; Schatz, U.; Perakakis, N.; Kassner, U.; Schumann, F.; Axthelm, C.; Stürzebecher, P.; Sinning, D.L.; Doevelaar, A.; Rohn, B.; et al. High Interindividual Variability in LDL-Cholesterol Reductions after Inclisiran Administration in a Real-World Multicenter Setting in Germany. Clin. Res. Cardiol. 2023, 112, 1639–1649. [Google Scholar] [CrossRef]
- Ouyang, M.; Li, C.; Hu, D.; Peng, D.; Yu, B. Mechanisms of Unusual Response to Lipid-Lowering Therapy: PCSK9 Inhibition. Clin. Chim. Acta 2023, 538, 113–123. [Google Scholar] [CrossRef]
- Smith, J.R.; Thomas, R.J.; Bonikowske, A.R.; Hammer, S.M.; Olson, T.P. Sex Differences in Cardiac Rehabilitation Outcomes. Circ. Res. 2022, 130, 552–565. [Google Scholar] [CrossRef] [PubMed]
- Samayoa, L.; Grace, S.L.; Gravely, S.; Scott, L.B.; Marzolini, S.; Colella, T.J.F. Sex Differences in Cardiac Rehabilitation Enrollment: A Meta-Analysis. Can. J. Cardiol. 2014, 30, 793–800. [Google Scholar] [CrossRef]
- Oosenbrug, E.; Marinho, R.P.; Zhang, J.; Marzolini, S.; Colella, T.J.F.; Pakosh, M.; Grace, S.L. Sex Differences in Cardiac Rehabilitation Adherence: A Meta-Analysis. Can. J. Cardiol. 2016, 32, 1316–1324. [Google Scholar] [CrossRef]
- Peters, S.A.E.; Colantonio, L.D.; Zhao, H.; Bittner, V.; Dai, Y.; Farkouh, M.E.; Monda, K.L.; Safford, M.M.; Muntner, P.; Woodward, M. Sex Differences in High-Intensity Statin Use Following Myocardial Infarction in the United States. J. Am. Coll. Cardiol. 2018, 71, 1729–1737. [Google Scholar] [CrossRef] [PubMed]
- Van Oortmerssen, J.A.E.; Mulder, J.W.C.M.; Van Der Bijl, M.F.; Mijnster, R.J.M.; Kavousi, M.; Roeters Van Lennep, J.E. on behalf of the IMPRESS consortium Lipid Lowering Therapy Utilization and Lipid Goal Attainment in Women. Curr. Atheroscler. Rep. 2025, 27, 29. [Google Scholar] [CrossRef]
- Colantonio, L.D.; Huang, L.; Monda, K.L.; Bittner, V.; Serban, M.-C.; Taylor, B.; Brown, T.M.; Glasser, S.P.; Muntner, P.; Rosenson, R.S. Adherence to High-Intensity Statins Following a Myocardial Infarction Hospitalization Among Medicare Beneficiaries. JAMA Cardiol. 2017, 2, 890. [Google Scholar] [CrossRef] [PubMed]
- Bots, S.H.; Inia, J.A.; Peters, S.A.E. Medication Adherence After Acute Coronary Syndrome in Women Compared with Men: A Systematic Review and Meta-Analysis. Front. Glob. Womens Health 2021, 2, 637398. [Google Scholar] [CrossRef]
- O’Donoghue, M.L.; Morrow, D.A.; Tsimikas, S.; Sloan, S.; Ren, A.F.; Hoffman, E.B.; Desai, N.R.; Solomon, S.D.; Domanski, M.; Arai, K.; et al. Lipoprotein(a) for Risk Assessment in Patients with Established Coronary Artery Disease. J. Am. Coll. Cardiol. 2014, 63, 520–527. [Google Scholar] [CrossRef]
- Afshar, M.; Pilote, L.; Dufresne, L.; Engert, J.C.; Thanassoulis, G. Lipoprotein(a) Interactions with Low-Density Lipoprotein Cholesterol and Other Cardiovascular Risk Factors in Premature Acute Coronary Syndrome (ACS). J. Am. Heart Assoc. 2016, 5, e003012. [Google Scholar] [CrossRef]
- Sheashaa, H.; Mousa, H.; Abbas, M.T.; Farina, J.M.; Awad, K.; Pereyra, M.; Scalia, I.G.; Ali, N.B.; Javadi, N.; Bismee, N.N.; et al. Interaction Between Lipoprotein(a) and Other Lipid Molecules: A Review of the Current Literature. Biomolecules 2025, 15, 162. [Google Scholar] [CrossRef] [PubMed]
- Arnold, N.; Blaum, C.; Goßling, A.; Brunner, F.J.; Bay, B.; Zeller, T.; Ferrario, M.M.; Brambilla, P.; Cesana, G.; Leoni, V.; et al. Impact of Lipoprotein(a) Level on Low-Density Lipoprotein Cholesterol– or Apolipoprotein B–Related Risk of Coronary Heart Disease. J. Am. Coll. Cardiol. 2024, 84, 165–177. [Google Scholar] [CrossRef]
- Chait, A.; Eckel, R.H.; Vrablik, M.; Zambon, A. Lipid-Lowering in Diabetes: An Update. Atherosclerosis 2024, 394, 117313. [Google Scholar] [CrossRef]
- Armillotta, M.; Angeli, F.; Paolisso, P.; Belmonte, M.; Raschi, E.; Di Dalmazi, G.; Amicone, S.; Canton, L.; Fedele, D.; Suma, N.; et al. Cardiovascular Therapeutic Targets of Sodium-Glucose Co-Transporter 2 (SGLT2) Inhibitors beyond Heart Failure. Pharmacol. Ther. 2025, 270, 108861. [Google Scholar] [CrossRef]
- Velidakis, N.; Stachteas, P.; Gkougkoudi, E.; Papadopoulos, C.; Kadoglou, N.P.E. Classical and Novel Lipid-Lowering Therapies for Diabetic Patients with Established Coronary Artery Disease or High Risk of Coronary Artery Disease—A Narrative Clinical Review. Pharmaceuticals 2024, 17, 568. [Google Scholar] [CrossRef]
- Wittlinger, T.; Schwaab, B.; Völler, H.; Bongarth, C.; Heinze, V.; Eckrich, K.; Guha, M.; Richter, M.; Schlitt, A. Efficacy of Lipid-Lowering Therapy during Cardiac Rehabilitation in Patients with Diabetes Mellitus and Coronary Heart Disease. J. Cardiovasc. Dev. Dis. 2021, 8, 105. [Google Scholar] [CrossRef]
- Schwaab, B.; Waldmann, A.; Katalinic, A.; Sheikhzadeh, A.; Raspe, H. In-Patient Cardiac Rehabilitation versus Medical Care—A Prospective Multicentre Controlled 12 Months Follow-up in Patients with Coronary Heart Disease. Eur. J. Cardiovasc. Prev. Rehabil. 2011, 18, 581–586. [Google Scholar] [CrossRef] [PubMed]
- Mänttäri, M.; Tenkanen, L.; Mäenpää, H.; Manninen, V.; Huttunen, J.K. High-Density Lipoprotein Cholesterol Elevation with Gemfibrozil: Effects of Baseline Level and Modifying Factors. Clin. Pharmacol. Ther. 1993, 54, 437–447. [Google Scholar] [CrossRef]
- Thomas, R.J.; Beatty, A.L.; Beckie, T.M.; Brewer, L.C.; Brown, T.M.; Forman, D.E.; Franklin, B.A.; Keteyian, S.J.; Kitzman, D.W.; Regensteiner, J.G.; et al. Home-Based Cardiac Rehabilitation: A Scientific Statement from the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. Circulation 2019, 140, e69–e89. [Google Scholar] [CrossRef]
- Hama, T.; Chacin Suarez, A.S.; Bissen, T.G.; Bonikowske, A.R.; Smith, J.R.; Taylor, B.J.; Wheatley-Guy, C.M.; Scales, R.; Rogers, M.J.; Ahlskog, A.L.; et al. Home-Based Cardiac Rehabilitation Among Attendees from a Large Health Care System During the Covid-19 Pandemic. JACC Adv. 2024, 3, 101403. [Google Scholar] [CrossRef] [PubMed]
- Husaini, M.; Deych, E.; Waken, R.J.; Sells, B.; Lai, A.; Racette, S.B.; Rich, M.W.; Joynt Maddox, K.E.; Peterson, L.R. Intensive Versus Traditional Cardiac Rehabilitation: Mortality and Cardiovascular Outcomes in a 2016–2020 Retrospective Medicare Cohort. Circ. Cardiovasc. Qual. Outcomes 2023, 16, e010131. [Google Scholar] [CrossRef] [PubMed]
- Merenciano-Gonzalez, H.; Marcos Garces, V.; Martinez Mas, M.L.; Palau, P.; Climent Alberola, J.I.; Perez, N.; Lopez-Bueno, L.; Esteban Argente, M.C.; Valls Reig, M.; Munoz Alcover, R.; et al. Residual Difference in LDL Cholesterol as an Indicator of Adherence to Lifestyle Changes during Cardiac Rehabilitation. Eur. Heart J. 2023, 44 (Suppl. S2), ehad655.2592. [Google Scholar] [CrossRef]
- Merenciano-González, H.; Marcos-Garcés, V.; Martínez Mas, M.L.; Palau Sampío, P.; Climent Alberola, J.I.; Pérez Solé, N.; López Bueno, L.; Esteban Argente, M.C.; Valls Reig, M.; Muñoz Alcover, R.; et al. Diferencia Residual en Colesterol LDL como Indicador de Adherencia a Cambios en el Estilo de Vida Durante un Programa Ambulatorio de Rehabilitación Cardiaca. Rev. Esp. Cardiol. 2023, 76 (Suppl. S1), 99. Available online: https://www.revespcardiol.org/es-congresos-sec--el-congreso-de-la-salud-cardiovascu-157-sesion-rehabilitacion-cardiaca-y-adherencia-7567-diferencia-residual-en-colesterol-ldl-co-92384 (accessed on 10 April 2025). [CrossRef]

| Variable | All Patients (n = 179) | Negative RD-LDL-C (n = 125) | Positive RD-LDL-C (n = 54) | p-Value |
|---|---|---|---|---|
| Clinical variables | ||||
| Age (years) | 63.04 ± 10.56 | 61.83 ± 9.8 | 65.84 ± 11.77 | 0.03 |
| Male sex (%) | 152 (84.9) | 99 (79.2) | 53 (98.1) | 0.001 |
| Hypercholesterolemia (%) | 160 (89.4) | 115 (92) | 45 (83.3) | 0.08 |
| Hypertension (%) | 102 (57) | 65 (52) | 37 (68.5) | 0.04 |
| Diabetes mellitus (%) | 42 (23.5) | 36 (28.8) | 6 (11.1) | 0.01 |
| Killip class ≥ 2 (%) | 51 (28.5) | 31 (24.8) | 20 (37) | 0.1 |
| GRACE risk score | 118.3 ± 28.88 | 114.72 ± 26.2 | 126.61 ± 33.08 | 0.02 |
| Infarct location | 0.46 | |||
| Anterior (%) | 80 (44.7) | 51 (40.8) | 29 (53.7) | |
| Inferior (%) | 78 (43.6) | 58 (46.4) | 20 (37) | |
| Lateral (%) | 12 (6.7) | 9 (7.2) | 3 (5.6) | |
| OMI (%) | 9 (5) | 7 (5.6) | 2 (3.7) | |
| LVEF (%) | 52.29 ± 10.57 | 52.74 ± 10.7 | 51.26 ± 10.28 | 0.39 |
| LVEF < 50% (%) | 63 (35.2) | 44 (35.2) | 19 (35.2) | 1 |
| Exercise training modality during CRP | 0.02 | |||
| Ambulatory training (%) | 142 (79.3) | 93 (74.4) | 49 (90.7) | |
| Supervised in-hospital training (%) | 37 (20.7) | 32 (25.6) | 5 (9.3) | |
| Lipid and metabolic profile before admission | ||||
| Fasting blood glucose (mg/dL) | 99.59 ± 23.69 | 103.27 ± 24.66 | 91.15 ± 18.95 | 0.002 |
| Total cholesterol (mg/dL) | 199.83 ± 54.72 | 205.78 ± 54.13 | 186.04 ± 54.05 | 0.03 |
| Triglycerides (mg/dL) | 124 [90, 169] | 156.76 [97, 184] | 117.54 [84, 150.25] | 0.002 |
| HDL-C (mg/dL) | 46.25 ± 11.1 | 45.99 ± 9.99 | 46.85 ± 13.41 | 0.67 |
| Non-HDL-C (mg/dL) | 153.58 ± 51.4 | 159.79 ± 51.92 | 139.19 ± 47.58 | 0.01 |
| LDL-C (mg/dL) | 131.66 ± 45.02 | 136.06 ± 45.36 | 121.46 ± 42.91 | 0.04 |
| Corrected basal LDL-C (mg/dL) # | 159.72 ± 45.14 | 166.9 ± 44.69 | 143.09 ± 42.03 | 0.001 |
| LLT before admission (%) | 64 (35.8) | 47 (37.6) | 17 (31.5) | 0.43 |
| HbA1c (%) * | 6.25 ± 1.51 | 6.5 ± 1.33 | 5.32 ± 1.81 | 0.01 |
| Lipid and metabolic profile after CRP | ||||
| Fasting blood glucose (mg/dL) | 94.91 ± 18.7 | 97.33 ± 20.08 | 89.41 ± 13.72 | 0.009 |
| Median change (mg/dL) | −4.5 [−12.8, 5.75] | −5.5 [−13.25, 5.5] | −3 [−12, 6] | 0.47 |
| Total cholesterol (mg/dL) | 102.63 ± 17.85 | 99.44 ± 17.81 | 109.96 ± 15.79 | <0.001 |
| Mean change (mg/dL) | −97.31 ± 52.44 | −106.56 ± 50.23 | −76.07 ± 51.68 | <0.001 |
| Triglycerides (mg/dL) | 86.5 [65–118] | 93 [68.25, 122.5] | 78 [59.5, 103] | 0.02 |
| Median change (mg/dL) | −36.5 [−73.25, −6.75] | −40 [−75.5, −12.5] | −27 [−67.25, 0] | 0.1 |
| HDL-C (mg/dL) | 43.28 ± 9.03 | 42.76 ± 8.71 | 44.48 ± 9.71 | 0.24 |
| Median change (mg/dL) | −3 [−8, 2] | −3 [−8, 2] | −3 [−7.25, 2.5] | 0.99 |
| Non-HDL-C (mg/dL) | 59.35 ± 16.17 | 56.69 ± 16.64 | 65.48 ± 13.24 | 0.001 |
| Mean change (mg/dL) | −94.26 ± 49.72 | −103.22 ± 48.24 | −73.7 ± 47.3 | <0.001 |
| LDL-C (mg/dL) | 43.05 ± 13.8 | 39.3 ± 13.52 | 51.72 ± 10.13 | <0.001 |
| Mean change (mg/dL) | −88.61 ± 42.71 | −96.76 ± 41.13 | −69.74 ± 40.62 | <0.001 |
| Theoretical LDL-C after CRP (mg/dL) | 50.82 ± 16.18 | 54.79 ± 16.24 | 41.64 ± 11.8 | <0.001 |
| RD-LDL-C (mg/dL) | −7.54 [−16.8, 2.8] | −13.6 [−20.12, −6.91] | 8.92 [3.97, 14.39] | <0.001 |
| LDL-C < 55 mg/dL after CRP (%) | 153 (85.5) | 117 (93.6) | 36 (66.7) | <0.001 |
| HbA1c (%) | 6 ± 0.6 | 6.06 ± 0.66 | 5.86 ± 0.39 | 0.04 |
| Median change (%) | 0.1 [−0.3, 0.4] | 0 [−0.4, 0.28] | 0.3 [0.2, 0.4] | 0.13 |
| HbA1c < 7% after CRP (%) | 168 (94.9) | 116 (93.5) | 52 (98.1) | 0.21 |
| Other cardiovascular risk factors | ||||
| Lipoprotein (a) (mg/dL) | 28 [12.25, 76.75] | 25 [12, 60] | 49 [15, 90] | 0.03 |
| Smoking habit before CRP (%) | 87 (48.6) | 61 (48.8) | 26 (48.1) | 0.94 |
| Smoking habit after CRP (%) | 12 (6.7) | 6 (4.8) | 6 (11.1) | 0.12 |
| Systolic pressure before CRP (mmHg) | 124.6 ± 15.42 | 125 ± 15.52 | 123.67 ± 15.28 | 0.6 |
| Systolic pressure after CRP (mmHg) | 115.14 ± 9.69 | 115.02 ± 9.44 | 115.43 ± 10.35 | 0.8 |
| Median change (mmHg) | −10 [−20, 0] | −10 [−20, −4] | −6 [−16, 0] | 0.2 |
| Diastolic pressure before CRP (mmHg) | 77.6 ± 8.51 | 78.22 ± 7.78 | 76.15 ± 9.1 | 0.71 |
| Diastolic pressure after CRP (mmHg) | 73.54 ± 7.12 | 74.36 ± 6.87 | 72.95 ± 7.56 | 0.82 |
| Median change (mmHg) | −4 [−7, 0] | −4 [−8, −2] | −4 [−6, 0] | 0.87 |
| Weight before CRP (kg) | 79.85 ± 13.4 | 79.93 ± 13.99 | 79.68 ± 12.06 | 0.91 |
| Weight after CRP (kg) | 78.03 ± 12.78 | 78.18 ±13.14 | 77.68 ± 12 | 0.81 |
| Median change (kg) | −1 [−4, 1.5] | −1.5 [−4, 1.5] | −0.7 [−4.63, 1.25] | 0.81 |
| BMI before CRP | 27.47 ± 4.2 | 27.8 ± 4.48 | 26.7 ± 3.41 | 0.11 |
| BMI after CRP | 26.87 ± 3.98 | 27.22 ± 4.18 | 26.08 ± 3.39 | 0.08 |
| Median change | −0.33 [−1.49, 0.37] | −0.41 [−1.48, 0.47] | −0.24 [−1.53, 0.21] | 0.92 |
| BMI ≥ 30 before CRP (%) | 39 (21.8) | 31 (24.8) | 8 (14.8) | 0.14 |
| BMI ≥ 30 after CRP (%) | 34 (19) | 27 (21.6) | 7 (13) | 0.18 |
| Adherence to Mediterranean diet after CRP (≥8 points in PREDIMED) | 155 (88.1) | 106 (86.2) | 49 (92.5) | 0.24 |
| Therapeutic adherence after CRP (4 points in Morisky–Green) | 158 (89.8) | 109 (88.6) | 49 (92.5) | 0.44 |
| Quality of life outcomes | ||||
| SF-36 (mean) before CRP (points) | 64 ± 19.4 | 64.19 ± 18.7 | 63.54 ± 21.09 | 0.84 |
| SF-36 (mean) after CRP (points) | 71.27 ± 18.88 | 71.01 ± 19.04 | 71.88 ± 18.66 | 0.78 |
| Median change (points) | 5.61 [−3.66, 18.38] | 5.28 [−3.73, 15.48] | 5.88 [−3.08, 21.48] | 0.49 |
| PHQ-2 before CRP (points) | 1 [0, 2] | 1 [0, 2] | 1 [0, 2] | 0.74 |
| PHQ-2 after CRP (points) | 0 [0, 2] | 0 [0, 2] | 0 [0, 2] | 0.43 |
| Median change (points) | 0 [−1, 0] | 0 [−1, 0] | 0 [−1, 0] | 0.22 |
| GAD-2 before CRP (points) | 2 [0, 3] | 2 [0, 3] | 2 [0, 3] | 0.74 |
| GAD-2 after CRP (points) | 1 [0, 2] | 1 [0, 2] | 1 [0, 2] | 0.94 |
| Median change (points) | 0 [−2, 0] | 0 [−1, 0] | 0 [−2, 0] | 0.99 |
| Physical fitness variables | ||||
| IPAQ before CRP (METS/week) | 1386 [641.25, 2772] | 1386 [495, 2772] | 1386 [693, 2826.75] | 0.5 |
| IPAQ after CRP (METS/week) | 3545 [1980, 6132] | 3339 [1980, 5670] | 4531 [1998, 6774] | 0.1 |
| Median change (METS/week) | 1636 [461.75, 3572.63] | 1565 [489, 3031.5] | 2528.75 [373.88, 5311.5] | 0.19 |
| Peak VO2 before CRP (mL/kg/min) | 25.66 ± 9.26 | 26.39 ± 9.47 | 23.96 ± 8.6 | 0.11 |
| Peak VO2 after CRP (mL/kg/min) | 29.25 ± 10.43 | 30.03 ± 10.6 | 27.44 ± 9.89 | 0.13 |
| Mean change (mL/kg/min) | 3.6 ± 4.73 | 3.64 ± 4.77 | 3.49 ± 4.67 | 0.84 |
| All Patients (n = 179) | Negative RD-LDL-C (n = 125) | Positive RD-LDL-C (n = 54) | p-Value | |
|---|---|---|---|---|
| LLT at discharge | ||||
| Statins | 0.74 | |||
| No statin | 6 (3.4) | 4 (3.2) | 2 (3.7) | |
| Fluvastatin 80 mg o.d. | 1 (0.6) | 1 (0.8) | 0 (0) | |
| Pitavastatin 4 mg o.d. | 1 (0.6) | 1 (0.8) | 0 (0) | |
| Atorvastatin 20 mg o.d. | 2 (1.1) | 2 (1.6) | 0 (0) | |
| Atorvastatin 40 mg o.d. | 20 (11.2) | 16 (12.8) | 4 (7.4) | |
| Atorvastatin 60 mg o.d. | 3 (1.7) | 2 (1.6) | 1 (1.9) | |
| Atorvastatin 80 mg o.d. | 63 (35.2) | 39 (31.2) | 24 (44.4) | |
| Rosuvastatin 10 mg o.d. | 9 (5) | 7 (5.6) | 2 (3.7) | |
| Rosuvastatin 15 mg o.d. | 2 (1.1) | 1 (0.8) | 1 (1.9) | |
| Rosuvastatin 20 mg o.d. | 71 (39.7) | 51 (40.8) | 20 (37) | |
| Rosuvastatin 30 mg o.d. | 1 (0.6) | 1 (0.8) | 0 (0) | |
| Ezetimibe 10 mg o.d. | 97 (54.2) | 72 (57.6) | 25 (46.3) | 0.16 |
| Bempedoic acid 180 mg o.d. | 1 (0.6) | 1 (0.8) | 0 (0) | 0.51 |
| PCSK9 inhibitors | 1 (0.6) | 1 (0.8) | 0 (0) | 0.51 |
| Inclisiran | 0 (0) | 0 (0) | 0 (0) | - |
| Fibrates | 0 (0) | 0 (0) | 0 (0) | - |
| Theoretical potency of LLT at discharge (% reduction of LDL-C) | 58.99 ± 10.96 | 59.41 ± 11.03 | 58.04 ± 10.83 | 0.44 |
| LLT after CRP | ||||
| Statins | 0.04 | |||
| No statin | 1 (0.6) | 1 (0.8) | 0 (0) | |
| Pitavastatin 1 mg o.d. | 1 (0.6) | 0 (0) | 1 (1.9) | |
| Pitavastatin 4 mg o.d. | 2 (1.1) | 2 (1.6) | 0 (0) | |
| Atorvastatin 20 mg o.d. | 1 (0.6) | 0 (0) | 1 (1.9) | |
| Atorvastatin 40 mg o.d. | 23 (12.8) | 18 (14.4) | 5 (9.3) | |
| Atorvastatin 80 mg o.d. | 45 (25.1) | 27 (21.6) | 18 (33.3) | |
| Rosuvastatin 10 mg o.d. | 9 (5) | 8 (6.4) | 1 (1.9) | |
| Rosuvastatin 20 mg o.d. | 85 (47.5) | 65 (52) | 20 (37) | |
| Rosuvastatin 30 mg o.d. | 5 (2.8) | 2 (1.6) | 3 (5.6) | |
| Rosuvastatin 40 mg o.d. | 7 (3.9) | 2 (1.6) | 5 (9.3) | |
| Ezetimibe 10 mg o.d. | 164 (91.6) | 111 (88.8) | 53 (98.1) | 0.04 |
| Bempedoic acid 180 mg o.d. | 19 (10.6) | 8 (6.4) | 11 (20.4) | 0.005 |
| PCSK9 inhibitors | 24 (13.4) | 15 (12) | 9 (16.7) | 0.5 |
| Inclisiran | 6 (3.4) | 5 (4) | 1 (1.9) | 0.52 |
| Fibrates | 1 (0.6) | 1 (0.8) | 0 (0) | 0.54 |
| Theoretical potency of LLT after CRP (% reduction of LDL-C) | 67.44 ± 7.51 | 66.41 ± 7.48 | 69.81 ± 7.07 | 0.005 |
| Median change (%) | 6 [0, 15] | 0 [0, 13] | 9 [3.75, 16.25] | <0.001 |
| Variable | HR [95% CI] | Change in Model’s Nagelkerke’s R2 | Change in Model’s Chi-Squared | p-Value |
|---|---|---|---|---|
| Model 1—clinical variables | ||||
| Age (years) | 1.02 [0.97, 1.08] | - | - | 0.4 |
| Male sex (%) | 16.02 [2.08, 123.34] | 0.107 | 14.07 | 0.008 |
| Hypercholesterolemia (%) | 0.4 [0.13, 1.27] | - | - | 0.12 |
| Hypertension (%) | 1.87 [0.86, 4.07] | - | - | 0.11 |
| Diabetes mellitus (%) | 0.26 [0.1, 0.69] | 0.056 | 7.87 | 0.006 |
| GRACE risk score | 1.01 [0.99, 1.03] | - | - | 0.43 |
| Supervised in-hospital training | 0.26 [0.09, 0.73] | 0.055 | 7.96 | 0.01 |
| Model 2—clinical variables and lipid and metabolic profile variables before admission | ||||
| Male sex | 17.96 [2.15, 149.92] | 0.117 | 14.79 | 0.008 |
| Diabetes mellitus | 0.17 [0.06, 0.51] | 0.07 | 10.85 | 0.002 |
| Supervised in-hospital training | 0.28 [0.09, 0.86] | 0.035 | 5.69 | 0.03 |
| Fasting blood glucose (mg/dL) | 1 [0.98, 1.02] | - | - | 0.91 |
| Total cholesterol (mg/dL) | 0.99 [0.94, 1.05] | - | - | 0.82 |
| Triglycerides (mg/dL) | 0.99 [0.97, 1.01] | - | - | 0.22 |
| Non-HDL-C (mg/dL) | 1.04 [0.94, 1.15] | - | - | 0.43 |
| LDL-C (mg/dL) | 0.98 [0.89, 1.07] | - | - | 0.61 |
| Corrected basal LDL-C (mg/dL) | 0.98 [0.97, 0.99] | 0.077 | 11.2 | 0.001 |
| HbA1c (%) | 0.58 [0.17, 1.92] | - | - | 0.37 |
| Lipoprotein (a) (mg/dL) | 1.02 [1.01, 1.03] | 0.077 | 10.53 | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bertolín-Boronat, C.; Merenciano-González, H.; Marcos-Garcés, V.; Martínez Mas, M.L.; Climent Alberola, J.I.; Civera, J.M.; Valls Reig, M.; Ruiz Hueso, M.; Castro Carmona, P.; Perez, N.; et al. Low-Density Lipoprotein Cholesterol Reduction and Therapeutic Adherence During Cardiac Rehabilitation After Myocardial Infarction. J. Clin. Med. 2025, 14, 4242. https://doi.org/10.3390/jcm14124242
Bertolín-Boronat C, Merenciano-González H, Marcos-Garcés V, Martínez Mas ML, Climent Alberola JI, Civera JM, Valls Reig M, Ruiz Hueso M, Castro Carmona P, Perez N, et al. Low-Density Lipoprotein Cholesterol Reduction and Therapeutic Adherence During Cardiac Rehabilitation After Myocardial Infarction. Journal of Clinical Medicine. 2025; 14(12):4242. https://doi.org/10.3390/jcm14124242
Chicago/Turabian StyleBertolín-Boronat, Carlos, Héctor Merenciano-González, Víctor Marcos-Garcés, María Luz Martínez Mas, Josefa Inés Climent Alberola, José Manuel Civera, María Valls Reig, Marta Ruiz Hueso, Patricia Castro Carmona, Nerea Perez, and et al. 2025. "Low-Density Lipoprotein Cholesterol Reduction and Therapeutic Adherence During Cardiac Rehabilitation After Myocardial Infarction" Journal of Clinical Medicine 14, no. 12: 4242. https://doi.org/10.3390/jcm14124242
APA StyleBertolín-Boronat, C., Merenciano-González, H., Marcos-Garcés, V., Martínez Mas, M. L., Climent Alberola, J. I., Civera, J. M., Valls Reig, M., Ruiz Hueso, M., Castro Carmona, P., Perez, N., López-Bueno, L., Díaz Díaz, B., Miñano Martínez, I., Payá Rubio, A., Ríos-Navarro, C., de Dios, E., Gavara, J., Jiménez-Navarro, M. F., Sanchis, J., & Bodi, V. (2025). Low-Density Lipoprotein Cholesterol Reduction and Therapeutic Adherence During Cardiac Rehabilitation After Myocardial Infarction. Journal of Clinical Medicine, 14(12), 4242. https://doi.org/10.3390/jcm14124242






