Comparison of the Effectiveness of Low-Level Laser Therapy and Therapeutic Ultrasound in Patients with Rotator Cuff Tendinopathy
Abstract
1. Introduction
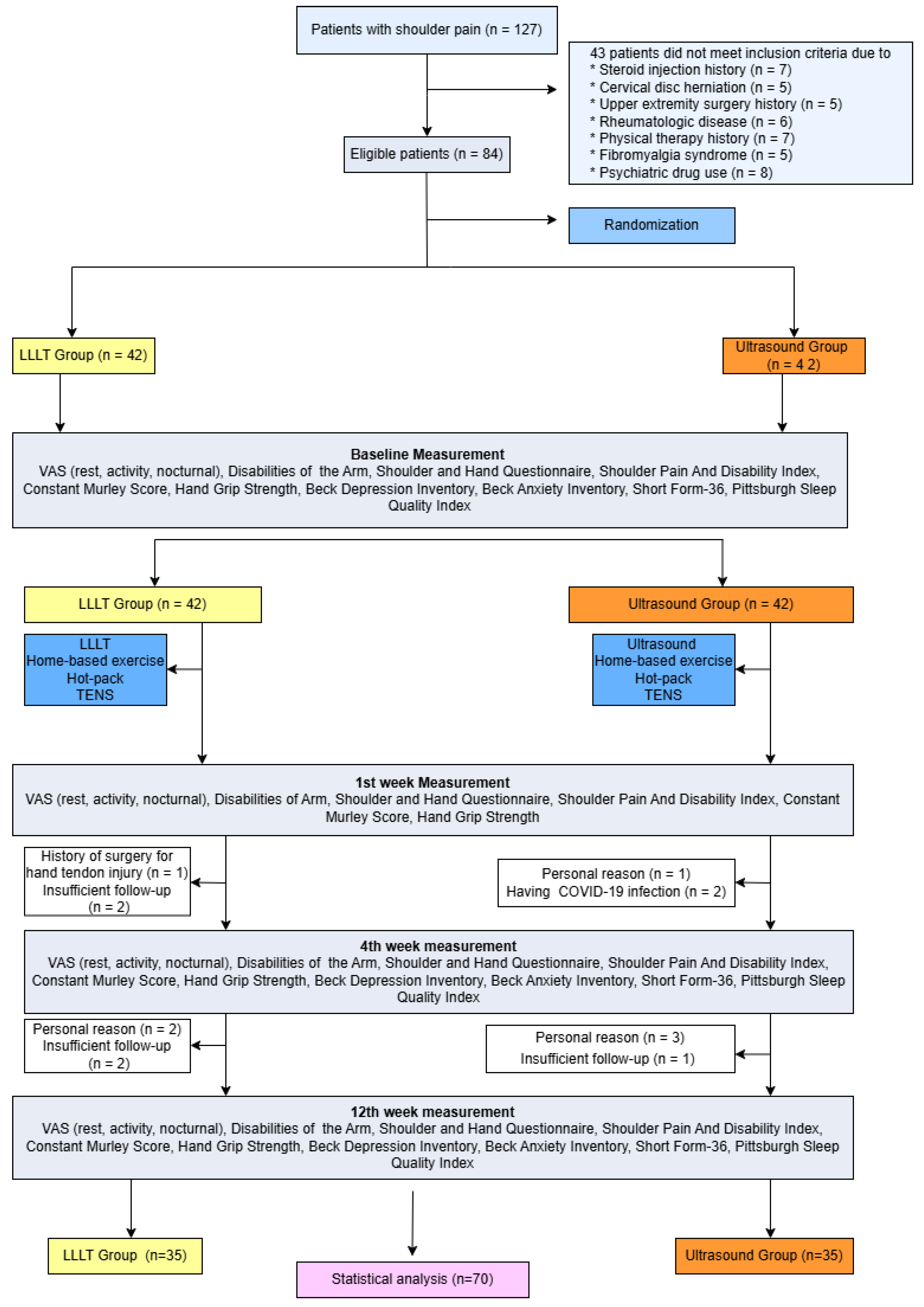
2. Patients and Methods
2.1. Randomization and Interventions
2.2. Outcome Measures
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Luime, J.J.; Koes, B.W.; Hendriksen, I.J.; Burdorf, A.; Verhagen, A.P.; Miedema, H.S.; Verhaar, J.A. Prevalence and incidence of shoulder pain in the general population; a systematic review. Scand J. Rheumatol. 2004, 33, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Harrison, A.K.; Flatow, E.L. Subacromial Impingement Syndrome. J. Am. Acad. Orthop. Surg. 2011, 19, 701–708. [Google Scholar] [CrossRef] [PubMed]
- Hanchard, N.C.A.; Cummins, J.; Jeffries, C. Evidence-Based Clinical Guidelines for the Diagnosis, Assessment and Physiotherapy Management of Shoulder Impingement Syndrome; The Chartered Society of Physiotherapy: London, UK, 2004; p. 1. [Google Scholar]
- Burbank, K.M.; Stevenson, J.H.; Czarnecki, G.R.; Dorfman, J. Chronic Shoulder Pain: Part I. Evaluation and Diagnosis. Am. Fam. Physician 2008, 77, 453–460. [Google Scholar] [PubMed]
- Yavuz, F.; Duman, I.; Taskaynatan, M.A.; Tan, A.K. Low-Level Laser Therapy versus Ultrasound Therapy in the Treatment of Subacromial Impingement Syndrome: A Randomized Clinical Trial. J. Back Musculoskelet. Rehabil. 2014, 27, 315–320. [Google Scholar] [CrossRef]
- Calis, H.T.; Berberoglu, N.; Calis, M. Are Ultrasound, Laser and Exercise Superior to Each Other in the Treatment of Subacromial Impingement Syndrome? A Randomized Clinical Trial. Eur. J. Phys. Rehabil. Med. 2011, 47, 375–380. [Google Scholar]
- Sen, E.I.; Arman, S.; Tseveendorj, N.; Yılmaz, E.; Oral, A.; Capan, N. Low-Level Laser Therapy versus Ultrasound Therapy Combined with Home-Based Exercise in Patients with Subacromial Impingement Syndrome: A Randomized-Controlled Trial. Turk. J. Phys. Med. Rehabil. 2023, 69, 424–433. [Google Scholar] [CrossRef]
- Price, D.D.; McGrath, P.A.; Rafii, A.; Buckingham, B. The Validation of Visual Analogue Scales as Ratio Scale Measures for Chronic and Experimental Pain. Pain 1983, 17, 45–56. [Google Scholar] [CrossRef]
- Carlsson, A.M. Assessment of Chronic Pain. I. Aspects of the Reliability and Validity of the Visual Analogue Scale. Pain 1983, 16, 87–101. [Google Scholar] [CrossRef]
- Bumin, G.; Tuzun, E.H.; Tonga, E. The Shoulder Pain and Disability Index (SPADI): Cross-Cultural Adaptation, Reliability, and Validity of the Turkish Version. J. Back Musculoskelet. Rehabil. 2008, 1, 57–62. [Google Scholar] [CrossRef]
- Duger, T.; Yakut, E.; Oksuz, C.; Yorukan, S.; Bilgutay, B.S.; Kuru, C.S.; Leblebicioglu, G.; Kayihan, H.; Kirdi, N.; Yakut, Y.; et al. Kol Omuz ve El Sorunları Disabilities of the Arm Shoulder and Hand DASH Anketi Türkçe Uyarlamasının Güvenirliği ve Geçerliği. Turk. J. Physiother. Rehabil. -Fiz. Rehabil. 2006, 3, 99–107. [Google Scholar]
- Celik, D. Turkish Version of the Modified Constant-Murley Score and Standardized Test Protocol: Reliability and Validity. Acta. Orthop. Traumatol. Turc. 2016, 50, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, G.F.; McDonald, C.; Chenier, T.C. Measurement of Grip Strength: Validity and Reliability of the Sphygmomanometer and Jamar Grip Dynamometer. J. Orthop. Sports Phys. Ther. 1992, 16, 215–219. [Google Scholar] [CrossRef] [PubMed]
- Hisli, N. A Study on Validity and Reliability Test of the Beck Depression Scale. J. Psychol. 1988, 6, 118–122. [Google Scholar]
- Ulusoy, M.; Sahin, N.H.; Erkmen, H. Turkish Version of the Beck Anxiety Inventory: Psychometric Properties. J. Cogn. Psychother 1998, 12, 163–172. [Google Scholar]
- Agargun, M.Y.; Kara, H.; Anlar, O. The Validity and Reliability of the Pittsburgh Sleep Quality Index. Turk Psikiyatr. Derg. 1996, 7, 107–111. [Google Scholar]
- Demiral, Y.; Ergor, G.; Unal, B.; Semin, S.; Akvardar, Y.; Kıvırcık, B.; Alptekin, K. Normative Data and Discriminative Properties of Short Form 36 (SF-36) in Turkish Urban Population. BMC Public Health 2006, 6, 247. [Google Scholar] [CrossRef]
- Varacallo, M.A.; El Bitar, Y.; Sina, R.E.; Mair, S.D. Rotator Cuff Syndrome. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- van der Windt, D.A.W.M.; van der Heijden, G.J.M.G.; van den Berg, S.G.M.; Ter Riet, G.; de Winter, A.F.; Bouter, L.M. Ultrasound Therapy for Musculoskeletal Disorders: A Systematic Review. Pain 1999, 81, 257–271. [Google Scholar] [CrossRef]
- Page, M.J.; Green, S.; Mrocki, M.A.; Surace, S.J.; Deitch, J.; McBain, B.; Lyttle, N.; Buchbinder, R. Electrotherapy Modalities for Rotator Cuff Disease. Cochrane Database Syst. Rev. 2016, 10, CD012225. [Google Scholar] [CrossRef]
- Desmeules, F.; Boudreault, J.; Roy, J.S.; Dionne, C.; Frémont, P.; MacDermid, J.C. The Efficacy of Therapeutic Ultrasound for Rotator Cuff Tendinopathy: A Systematic Review and Meta-Analysis. Phys. Ther. Sport 2015, 16, 276–284. [Google Scholar] [CrossRef]
- Yildirim, M.A.; Ones, K.; Celik, E.C. Comparision of Ultrasound Therapy of Various Durations in the Treatment of Subacromial Impingement Syndrome. J. Phys. Ther. Sci. 2013, 25, 1151–1154. [Google Scholar] [CrossRef]
- Kingsley, J.D.; Demchak, T.; Mathis, R. Low-Level Laser Therapy as a Treatment for Chronic Pain. Front Physiol. 2014, 5, 306. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tombak, Y.; Karaahmet, O.Z.; Tombak, A.; Gurcay, E. Effects of Low-Level Laser Therapy on Symptomatic Calcific Rotator Cuff Tendinopathy: A Prospective Randomized Controlled Study. Wien Klin. Wochenschr 2024, 5, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Castaldo, M.; De Angelis D’Ossat, A.; Gnessi, P.; Galeoto, G. A Systematic Review on Low-Level Laser Therapy in the Management of Shoulder Impingement Syndrome. Appl. Sci. 2023, 13, 3536. [Google Scholar] [CrossRef]
- Atıcı Ozturk, P.; Sengül, I.; Karatepe, A.G.; Kaya, T.; Günaydın, R. Effectiveness of Low-Level Laser Therapy in Patients with Subacromial Impingement Syndrome: A Randomized, Placebo Controlled, Prospective Study. J. Tepecik Educ. Res. Hosp. 2015, 25, 78–84. [Google Scholar] [CrossRef]
- Ranjithkumar, N.; Paul, J.; Alagesan, J.; Viswanathan, R. Comparative Effectiveness of Extracorporeal Short-Wave Therapy, Low-Level Laser Therapy, and Ultrasound in the Treatment of Rotator Cuff Tendinopathy. Biomed. Pharmacol. J. 2025, 18, 849–866. [Google Scholar] [CrossRef]
- Saunders, L. Laser versus Ultrasound in the Treatment of Supraspinatus Tendinosis: Randomised Controlled Trial. Physiotherapy 2003, 89, 365–373. [Google Scholar] [CrossRef]
- Santamato, A.; Solfrizzi, V.; Panza, F.; Tondi, G.; Frisardi, V.; Leggin, B.G.; Ranieri, M.; Fiore, P. Short-Term Effects of High-Intensity Laser Therapy versus Ultrasound Therapy in the Treatment of People with Subacromial Impingement Syndrome: A Randomized Clinical Trial. Phys. Ther. 2009, 89, 643–652. [Google Scholar] [CrossRef]
| Ultrasound Group (n = 35) | LLLT Group (n = 35) | p-Value | |
|---|---|---|---|
| Age, years (mean ± SD) | 51.7 ± 8.8 | 49.9 ± 9.4 | 0.410 |
| Gender, F/M (n, %) | 20/15(57.1/42.9) | 20/15 (57.1/42.9) | 1.000 |
| BMI (mean ± SD) | 30.4 ± 5.8 | 29.1 ± 4.9 | 0.310 |
| Disease duration, months (mean ± SD) | 13.6 ± 16.2 | 9.4 ± 1.2 | 0.210 |
| Side of involvement (R/L), n (%) | 23/12 (65.7/34.3) | 24/11 (68.6/31.4) | 0.790 |
| Occupation, n (%) | 0.730 | ||
| Housewife | 18 (51.4) | 13 (37.2) | |
| Retired | 4 (11.4) | 6 (17.1) | |
| Active employee | 13 (37.2) | 16 (45.7) | |
| VAS (mean ± SD) | |||
| Activity | 8.3 ± 1.5 | 8.6 ± 0.8 | 0.330 |
| Rest | 5.4 ± 0.8 | 5.4 ± 0.9 | 0.680 |
| Night | 6.9 ± 1.9 | 7.6 ± 1.5 | 0.170 |
| DASH (mean ± SD) | |||
| Function-symptom | 51.8 ± 15.6 | 50.3 ± 16.9 | 0.714 |
| Work | 64.1 ± 20.9 | 55.3 ± 20.5 | 0.870 |
| CMS (mean ± SD) | |||
| Total | 60.5 ± 7.6 | 58.4 ± 4.7 | 0.170 |
| Objective assessment | 49.5 ± 5.7 | 49.1 ± 3.7 | 0.747 |
| SPADI (mean ± SD) | |||
| Pain | 80.8 ± 17.3 | 77.5 ± 10.9 | 0.342 |
| Disability | 68.6 ± 19.1 | 63.5 ± 13.1 | 0.202 |
| Total | 73.3 ± 17.7 | 68.9 ± 11.6 | 0.225 |
| HGS, kg (mean ± SD) | |||
| Right | 28.6 ± 9.6 | 29.6 ± 10.5 | 0.600 |
| Left | 28.1 ± 9.2 | 30.2 ± 9.7 | 0.300 |
| SF-36 (mean ± SD) | |||
| Physical functioning | 63.3 ± 16.93 | 60.3 ± 21.5 | 0.500 |
| Role physical | 17.9 ± 33.52 | 33.6 ± 39.7 | 0.070 |
| Role emotional | 56.2 ± 44.11 | 49.5 ± 39.9 | 0.500 |
| Vitality | 64.1 ± 20.38 | 48.6 ± 20.3 | 0.002 * |
| Mental health | 69.3 ± 14.41 | 58.9 ± 15.9 | 0.006 * |
| Social functioning | 67.5 ± 25.4 | 63.6 ± 20.4 | 0.470 |
| Bodily pain | 34.8 ± 23.1 | 33.7 ± 20.9 | 0.840 |
| General Health | 55.9 ± 16.3 | 48.0 ± 16.4 | 0.040 * |
| BDI (mean ± SD) | 7.9 ± 5.9 | 12.5 ± 8.8 | 0.010 * |
| BAI (mean ± SD) | 13.1 ± 11.6 | 14.2 ± 8.5 | 0.600 |
| PSQI (mean ± SD) | 7.3 ± 3.9 | 7.6 ± 3.3 | 0.700 |
| Ultrasound Group (n = 35) | Baseline | Post-Treatment 1st Week | Post-Treatment 4th Week | Post-Treatment 12th Week | p-Value * | Effect Size (Kendall’s W) |
|---|---|---|---|---|---|---|
| DASH | ||||||
| Function Symptom | 51.8 ± 15.6 | 34.8 ± 21.9 | 28.1 ± 18.8 | 15.1 ± 17.5 | <0.001 ** | 0.665 |
| Work | 64.1 ± 20.9 | 45.9 ± 25.7 | 39.5 ± 24.3 | 19.7 ± 22.2 | <0.001 ** | 0.586 |
| SPADI | ||||||
| Pain | 80.8 ± 17.3 | 47.5 ± 24.5 | 43.1 ± 30.2 | 25.6 ± 25.9 | <0.001 ** | 0.691 |
| Disability | 68.6 ± 19.1 | 41.1 ± 27.6 | 35.0 ± 24.0 | 18.0 ± 20.6 | <0.001 ** | 0.609 |
| Total | 73.3 ± 17.7 | 43.0 ± 25.9 | 38.2 ± 26.1 | 20.3 ± 22.2 | <0.001 ** | 0.717 |
| CMS | ||||||
| Total | 60.5 ± 7.6 | 80.0 ± 13.8 | 88.9 ± 11.5 | 96.4 ± 5.2 | <0.001 ** | 0.806 |
| Objective Assessment | 49.5 ± 5.7 | 58.9 ± 7.0 | 61.9 ± 5.7 | 64.5 ± 1.2 | <0.001 ** | 0.733 |
| VAS | ||||||
| Activity | 8.3 ± 1.5 | 5.8 ± 2.4 | 4.5 ± 1.9 | 2.5 ± 2.3 | <0.001 ** | 0.783 |
| Rest | 5.4 ± 0.8 | 3.0 ± 2.1 | 1.1 ± 1.7 | 0.5 ± 1.2 | <0.001 ** | 0.777 |
| Night | 6.9 ± 2.0 | 3.0 ± 2.7 | 1.0 ± 1.8 | 0.9 ± 1.5 | <0.001 ** | 0.788 |
| HGS | ||||||
| Right | 28.6 ± 9.6 | 32.2 ± 9.8 | 31.5 ± 9.9 | 33.5 ± 9.4 | <0.001 ** | 0.248 |
| Left | 28.2 ± 9.2 | 32.2 ± 8.6 | 31.9 ± 9.3 | 33.1 ± 9.3 | <0.001 ** | 0.306 |
| BDI | 7.9 ± 6.0 | x | 5.4 ± 5.2 | 5.0 ± 6.5 | <0.001 ** | 0.276 |
| BAI | 13.1 ± 11.6 | x | 8.3 ± 7.3 | 8.1 ± 9.0 | 0.002 ** | 0.181 |
| PSQI | 7.3 ± 3.9 | x | 4.5 ± 3.7 | 3.1 ± 3.4 | <0.001 ** | 0.325 |
| SF-36 | ||||||
| Physical Functioning | 63.3 ± 16.9 | x | 78.4 ± 15.2 | 77.6 ± 20.3 | <0.001 ** | 0.290 |
| Role Physical | 17.9 ± 33.5 | x | 60.7 ± 42.1 | 64.3 ± 43.0 | <0.001 ** | 0.394 |
| Role Emotional | 56.2 ± 44.1 | x | 84.8 ± 31.7 | 75.2 ± 39.9 | 0.001 ** | 0.205 |
| Vitality | 64.1 ± 20.4 | x | 70.7 ± 18.2 | 69.1 ± 18.0 | 0.074 | 0.075 |
| Mental Health | 69.3 ± 14.4 | x | 73.8 ± 12.8 | 72.8 ± 15.6 | 0.021 ** | 0.110 |
| Social Functioning | 67.5 ± 25.4 | x | 80.2 ± 21.3 | 84.6 ± 19.5 | 0.001 ** | 0.217 |
| Bodily Pain | 34.8 ± 23.1 | x | 58.6 ± 26.1 | 69.2 ± 26.5 | <0.001 ** | 0.527 |
| General Health | 55.9 ± 16.3 | x | 67.3 ± 12.7 | 70.0 ± 22.5 | <0.001 ** | 0.375 |
| LLLT Group (n = 35) | Baseline | Post-Treatment 1st Week | Post-Treatment 4th Week | Post-Treatment 12th Week | p-Value * | Effect Size (Kendall’s W) |
|---|---|---|---|---|---|---|
| DASH | ||||||
| Function Symptom | 50.4 ± 16.9 | 30.4 ± 17.8 | 29.5 ± 22.5 | 16.4 ± 19.5 | <0.001 ** | 0.530 |
| Work | 55.4 ± 20.8 | 37.5 ± 21.0 | 28.6 ± 24.0 | 16.1 ± 24.9 | <0.001 ** | 0.508 |
| SPADI | ||||||
| Pain | 77.5 ± 10.9 | 47.5 ± 20.8 | 43.3 ± 30.0 | 25.1 ± 28.9 | <0.001 ** | 0.554 |
| Disability | 63.5 ± 13.1 | 41.9 ± 19.4 | 35.8 ± 24.9 | 23.2 ± 26.6 | <0.001 ** | 0.544 |
| Total | 68.9 ± 11.6 | 45.6 ± 19.0 | 38.7 ± 26.7 | 23.9 ± 27.1 | <0.001 ** | 0.559 |
| CMS | ||||||
| Total | 58.4 ± 4.7 | 81.8 ± 10.3 | 86.7 ± 9.9 | 95.4 ± 8.8 | <0.001 ** | 0.820 |
| Objective Assessment | 49.1 ± 3.7 | 61.2 ± 5.0 | 63.2 ± 3.5 | 64.3 ± 2.0 | <0.001 ** | 0.790 |
| VAS | ||||||
| Activity | 8.6 ± 0.8 | 5.7 ± 1.8 | 4.6 ± 2.0 | 2.7 ± 2.4 | <0.001 ** | 0.884 |
| Rest | 5.5 ± 1.0 | 2.9 ± 1.4 | 2.0 ± 1.8 | 0.9 ± 1.4 | <0.001 ** | 0.785 |
| Night | 7.6 ± 1.5 | 3.5 ± 2.3 | 2.3 ± 2.1 | 1.1 ± 1.9 | <0.001 ** | 0.853 |
| HGS (kg) | ||||||
| Right | 29.6 ± 10.5 | 30.1 ± 9.3 | 30.9 ± 8.7 | 33.1 ± 9.0 | <0.001 ** | 0.243 |
| Left | 30.2 ± 9.8 | 31.1 ± 9.9 | 31.1 ± 8.7 | 32.5 ± 8.9 | <0.001 ** | 0.117 |
| BDI | 12.5 ± 8.8 | x | 8.8 ± 9.1 | 8.4 ± 7.9 | <0.001 ** | 0.235 |
| BAI | 14.2 ± 8.5 | x | 10.6 ± 8.4 | 9.4 ± 8.5 | <0.001 ** | 0.319 |
| PSQI | 7.6 ± 3.3 | x | 5.4 ± 4.2 | 4.9 ± 3.9 | <0.001 ** | 0.245 |
| SF-36 | ||||||
| Physical Functioning | 60.3 ± 21.5 | x | 74.0 ± 19.7 | 77.4 ± 18.4 | 0.001 ** | 0.210 |
| Role Physical | 33.6 ± 39.7 | x | 64.3 ± 39.9 | 74.3 ± 36.6 | <0.001 ** | 0.342 |
| Role Emotional | 49.5 ± 39.9 | x | 66.7 ± 36.2 | 81.0 ± 32.6 | 0.001 ** | 0.207 |
| Vitality | 48.6 ± 20.3 | x | 63.4 ± 16.2 | 64.3 ± 23.6 | <0.001 ** | 0.321 |
| Mental Health | 58.9 ± 15.9 | x | 66.3 ± 14.0 | 70.7 ± 16.3 | 0.001 ** | 0.213 |
| Social Functioning | 63.6 ± 20.4 | x | 75.4 ± 21.2 | 83.5 ± 17.6 | <0.001 ** | 0.337 |
| Bodily Pain | 33.7 ± 21.0 | x | 63.3 ± 27.3 | 74.4 ± 25.3 | <0.001 ** | 0.600 |
| General Health | 48.0 ± 16.4 | x | 61.1 ± 22.9 | 65.3 ± 18.2 | <0.001 ** | 0.274 |
| Ultrasound Group (n = 35) | LLLT Group (n = 35) | p-Value | Effect Size (r) | |
|---|---|---|---|---|
| VAS: | ||||
| Activity | ||||
| Baseline vs. W1 | −2.5 ± 2.8 | −2.9 ± 1.7 | 0.280 | 0.128 |
| Baseline vs. W4 | −3.8 ± 2.4 | −4.0 ± 1.9 | 0.910 | 0.013 |
| Baseline vs. W12 | −5.8 ± 2.6 | −5.9 ± 2.3 | 0.980 | 0.002 |
| Rest | ||||
| Baseline vs. W1 | −2.4 ± 2.0 | −2.6 ± 1.4 | 0.620 | 0.059 |
| Baseline vs. W4 | −4.3 ± 1.7 | −3.5 ± 2.0 | 0.050 | 0.232 |
| Baseline vs. W12 | −4.9 ± 1.1 | −4.6 ± 1.6 | 0.410 | 0.098 |
| Night | ||||
| Baseline vs. W1 | −3.9 ± 2.5 | −4.1 ± 2.0 | 0.600 | 0.062 |
| Baseline vs. W4 | −5.9 ± 2.3 | −5.3 ± 2.1 | 0.240 | 0.139 |
| Baseline vs. W12 | −6.2 ± 2.1 | −6.5 ± 1.8 | 0.530 | 0.074 |
| DASH: | ||||
| Function-symptom | ||||
| Baseline vs. W1 | −17.0 ± 16.7 | −20.0 ± 17.9 | 0.660 | 0.053 |
| Baseline vs. W4 | −23.7 ± 15.0 | −20.8 ± 20.4 | 0.390 | 0.101 |
| Baseline vs. W12 | −36.7 ± 17.9 | −34.0 ± 23.7 | 0.550 | 0.070 |
| Work | ||||
| Baseline vs. W1 | −18.2 ± 21.6 | −18.2 ± 22.3 | 0.850 | 0.022 |
| Baseline vs. W4 | −24.6 ± 19.9 | −27.0 ± 20.3 | 0.510 | 0.078 |
| Baseline vs. W12 | −44.4 ± 25.5 | −39.3 ± 26.9 | 0.520 | 0.077 |
| SPADI: | ||||
| Pain | ||||
| Baseline vs. W1 | −33.3 ± 22.7 | −30.0 ± 20.7 | 0.484 | 0.084 |
| Baseline vs. W4 | −37.7 ± 25.8 | −34.1 ± 30.4 | 0.742 | 0.039 |
| Baseline vs. W12 | −55.2 ± 23.0 | −52.4 ± 29.7 | 0.930 | 0.010 |
| Disability | ||||
| Baseline vs. W1 | −27.4 ± 26.3 | −21.6 ± 18.5 | 0.470 | 0.086 |
| Baseline vs. W4 | −33.6 ± 21.6 | −27.7 ± 24.4 | 0.350 | 0.109 |
| Baseline vs. W12 | −50.6 ± 21.2 | −40.3 ± 26.8 | 0.100 | 0.192 |
| Total | ||||
| Baseline vs. W1 | −30.3 ± 24.8 | −23.3 ± 17.8 | 0.260 | 0.132 |
| Baseline vs. W4 | −35.1 ± 22.5 | −30.2 ± 26.1 | 0.400 | 0.100 |
| Baseline vs. W12 | −53.0 ± 21.1 | −45.0 ± 27.4 | 0.290 | 0.125 |
| CMS: | ||||
| Total | ||||
| Baseline vs. W1 | 19.5 ± 13.2 | 23.4 ± 9.6 | 0.120 | 0.183 |
| Baseline vs. W4 | 28.5 ± 12.3 | 28.3 ± 9.8 | 0.710 | 0.044 |
| Baseline vs. W12 | 35.9 ± 7.5 | 37.0 ± 9.2 | 0.240 | 0.138 |
| CMS | ||||
| Objective assessment | ||||
| Baseline vs. W1 | 9.4 ± 6.8 | 12.1 ± 5.1 | 0.050 | 0.229 |
| Baseline vs. W4 | 12.5 ± 6.7 | 14.1 ± 4.2 | 0.320 | 0.117 |
| Baseline vs. W12 | 46.9 ± 6.2 | 46.3 ± 9.2 | 0.540 | 0.072 |
| HGS | ||||
| Right | ||||
| Baseline vs. W1 | 3.7 ± 4.7 | 0.4 ± 5.5 | 0.010 ** | 0.306 |
| Baseline vs. W4 | 3.0 ± 5.1 | 1.2 ± 6.4 | 0.370 | 0.107 |
| Baseline vs. W12 | 4.9 ± 5.4 | 3.5 ± 7.3 | 0.460 | 0.088 |
| Left | ||||
| Baseline vs. W1 | 4.0 ± 5.0 | 0.9 ± 3.7 | 0.007 ** | 0.320 |
| Baseline vs. W4 | 3.7 ± 5.1 | 0.8 ± 4.3 | 0.040 ** | 0.240 |
| Baseline vs. W12 | 4.9 ± 4.9 | 2.2 ± 5.0 | 0.030 ** | 0.252 |
| US Group (n = 35) | LLLT Group (n = 35) | p Value | Effect Size (r) | |
|---|---|---|---|---|
| SF-36: | ||||
| Physical functioning | ||||
| Baseline vs. W4 | 15.1 ± 1.6 | 13.7 ± 18.2 | 0.870 | 0.019 |
| Baseline vs. W12 | 14.3 ± 24.7 | 17.1 ± 25.7 | 0.760 | 0.037 |
| Role Physical | ||||
| Baseline vs. W4 | 42.9 ± 44.0 | 30.7 ± 43.3 | 0.230 | 0.142 |
| Baseline vs. W12 | 46.4 ± 45.8 | 40.7 ± 43.8 | 0.560 | 0.068 |
| Role emotional | ||||
| Baseline vs. W4 | 28.6 ± 39.7 | 17.1 ± 54.5 | 0.480 | 0.083 |
| Baseline vs. W12 | 19.0 ± 41.4 | 31.4 ± 42.7 | 0.130 | 0.181 |
| Vitality | ||||
| Baseline vs. W4 | 6.5 ± 11.5 | 14.9 ± 21.9 | 0.070 | 0.210 |
| Baseline vs. W12 | 5.0 ± 22.1 | 15.7 ± 21.2 | 0.040 | 0.238 |
| Mental health | ||||
| Baseline vs. W4 | 4.6 ± 12.2 | 7.4 ± 15.5 | 0.640 | 0.055 |
| Baseline vs. W12 | 3.5 ± 18.2 | 11.9 ± 16.9 | 0.160 | 0.166 |
| Social functioning | ||||
| Baseline vs. W4 | 12.7 ± 18.4 | 11.8 ± 24.3 | 0.880 | 0.017 |
| Baseline vs. W12 | 17.1 ± 32.5 | 19.9 ± 22.3 | 0.860 | 0.021 |
| Bodily pain | ||||
| Baseline vs. W4 | 45.4 ± 26.1 | 41.6 ± 23.6 | 0.560 | 0.070 |
| Baseline vs. W12 | 34.4 ± 31.5 | 40.7 ± 31.7 | 0.480 | 0.083 |
| General Health | ||||
| Baseline vs. W4 | 11.3 ± 13.5 | 13.1 ± 21.1 | 0.830 | 0.025 |
| Baseline vs. W12 | 14.1 ± 21.6 | 17.3 ± 19.5 | 0.800 | 0.030 |
| BDI | ||||
| Baseline vs. W4 | −2.5 ± 5.2 | −3.7 ± 7.1 | 0.290 | 0.124 |
| Baseline vs. W12 | −2.9 ± 6.2 | −4.1 ± 6.7 | 0.670 | 0.049 |
| BAI | ||||
| Baseline vs. W4 | −4.7 ± 8.9 | −3.6 ± 5.8 | 0.860 | 0.021 |
| Baseline vs. W12 | −4.9 ± 12.8 | −4.9 ± 6.5 | 0.850 | 0.022 |
| PSQI | ||||
| Baseline vs. W4 | −2.8 ± 3.4 | −2.2 ± 3.9 | 0.490 | 0.081 |
| Baseline vs. W12 | −4.2 ± 4.5 | −2.6 ± 4.1 | 0.140 | 0.173 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Diyarbakır, Ş.; Serdaroğlu Beyazal, M.; Devrimsel, G.; Yıldırım, M.; Topaloğlu, M.S. Comparison of the Effectiveness of Low-Level Laser Therapy and Therapeutic Ultrasound in Patients with Rotator Cuff Tendinopathy. J. Clin. Med. 2025, 14, 4197. https://doi.org/10.3390/jcm14124197
Diyarbakır Ş, Serdaroğlu Beyazal M, Devrimsel G, Yıldırım M, Topaloğlu MS. Comparison of the Effectiveness of Low-Level Laser Therapy and Therapeutic Ultrasound in Patients with Rotator Cuff Tendinopathy. Journal of Clinical Medicine. 2025; 14(12):4197. https://doi.org/10.3390/jcm14124197
Chicago/Turabian StyleDiyarbakır, Şeyma, Münevver Serdaroğlu Beyazal, Gül Devrimsel, Murat Yıldırım, and Mehmet Serhat Topaloğlu. 2025. "Comparison of the Effectiveness of Low-Level Laser Therapy and Therapeutic Ultrasound in Patients with Rotator Cuff Tendinopathy" Journal of Clinical Medicine 14, no. 12: 4197. https://doi.org/10.3390/jcm14124197
APA StyleDiyarbakır, Ş., Serdaroğlu Beyazal, M., Devrimsel, G., Yıldırım, M., & Topaloğlu, M. S. (2025). Comparison of the Effectiveness of Low-Level Laser Therapy and Therapeutic Ultrasound in Patients with Rotator Cuff Tendinopathy. Journal of Clinical Medicine, 14(12), 4197. https://doi.org/10.3390/jcm14124197






