Change in the Location of a Pseudotumor Around the C2 Odontoid Process from Posterior to Anterior to the Odontoid Process in the Natural Course: A Case with “Antero-Odontoid Pseudotumor” or “Peri-Odontoid Pseudotumor”
Abstract
1. Introduction
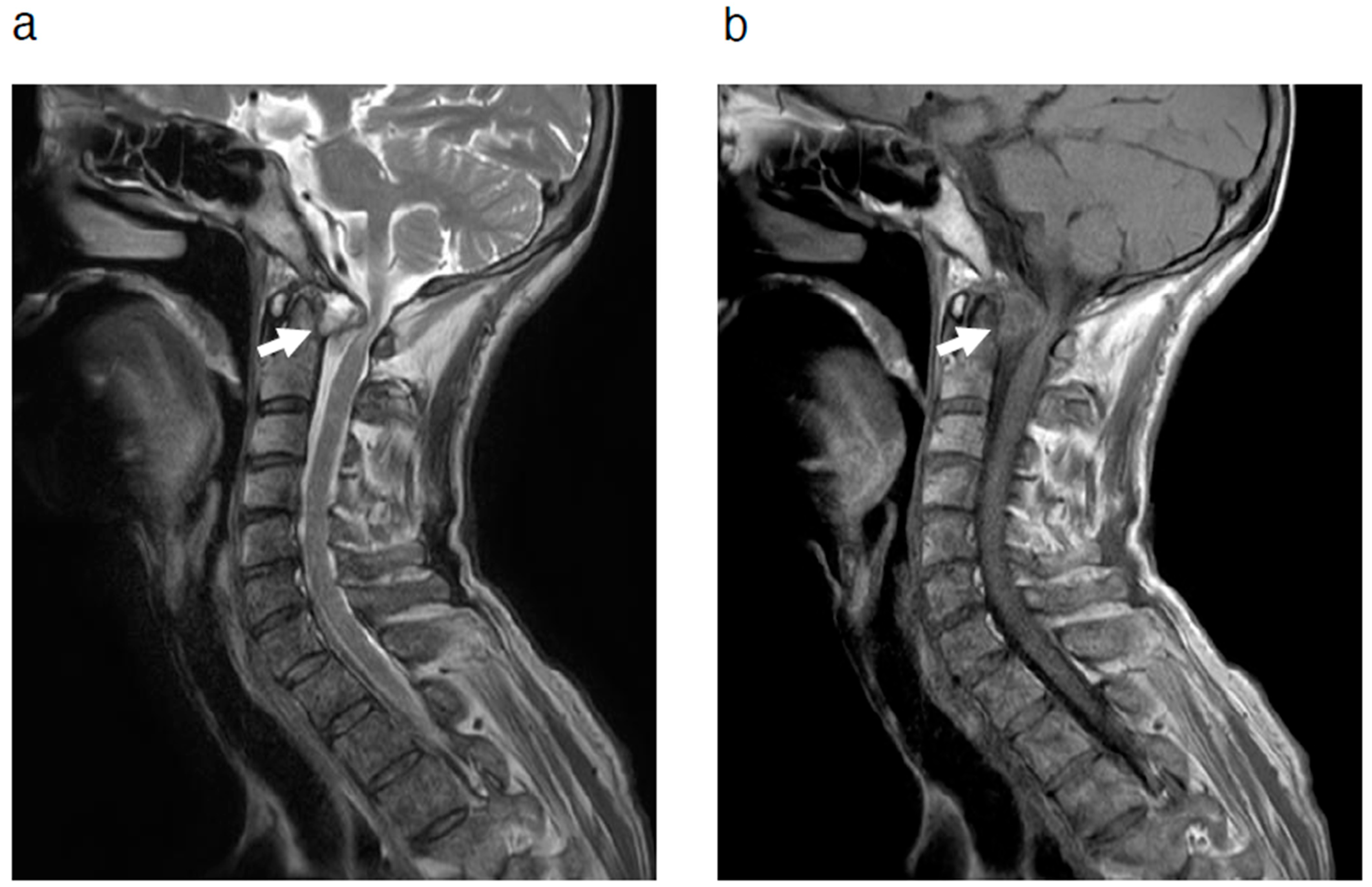
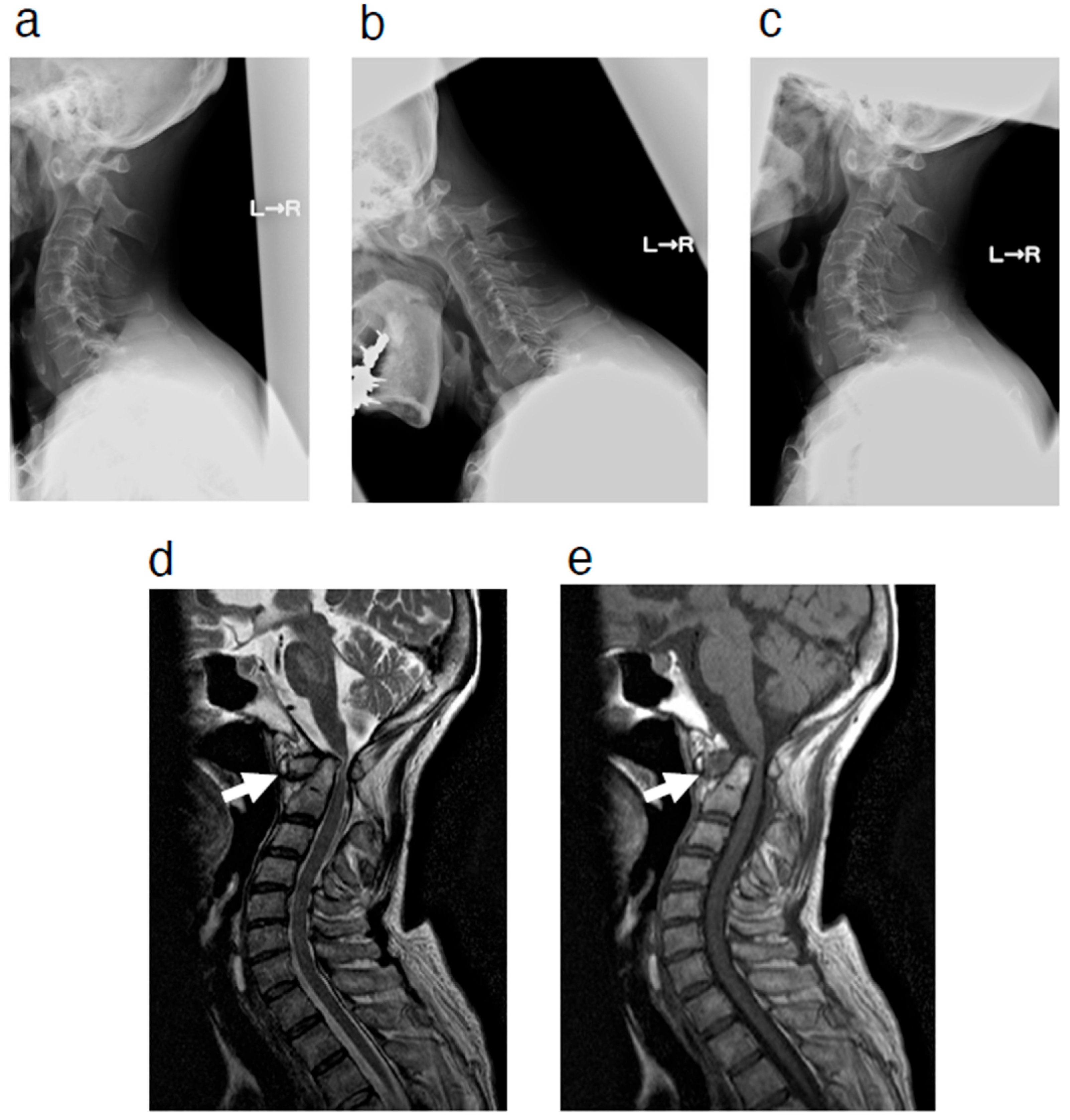
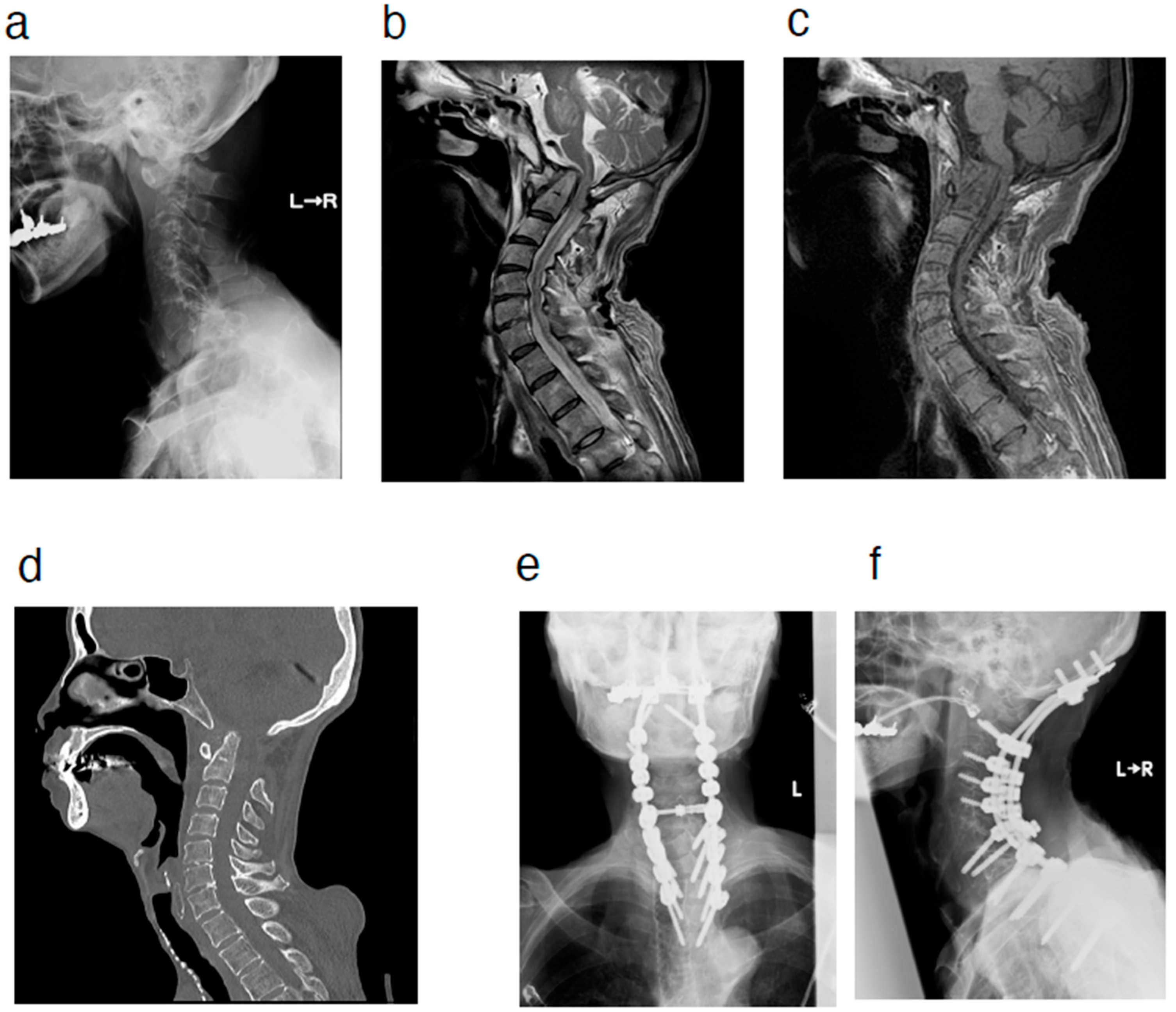
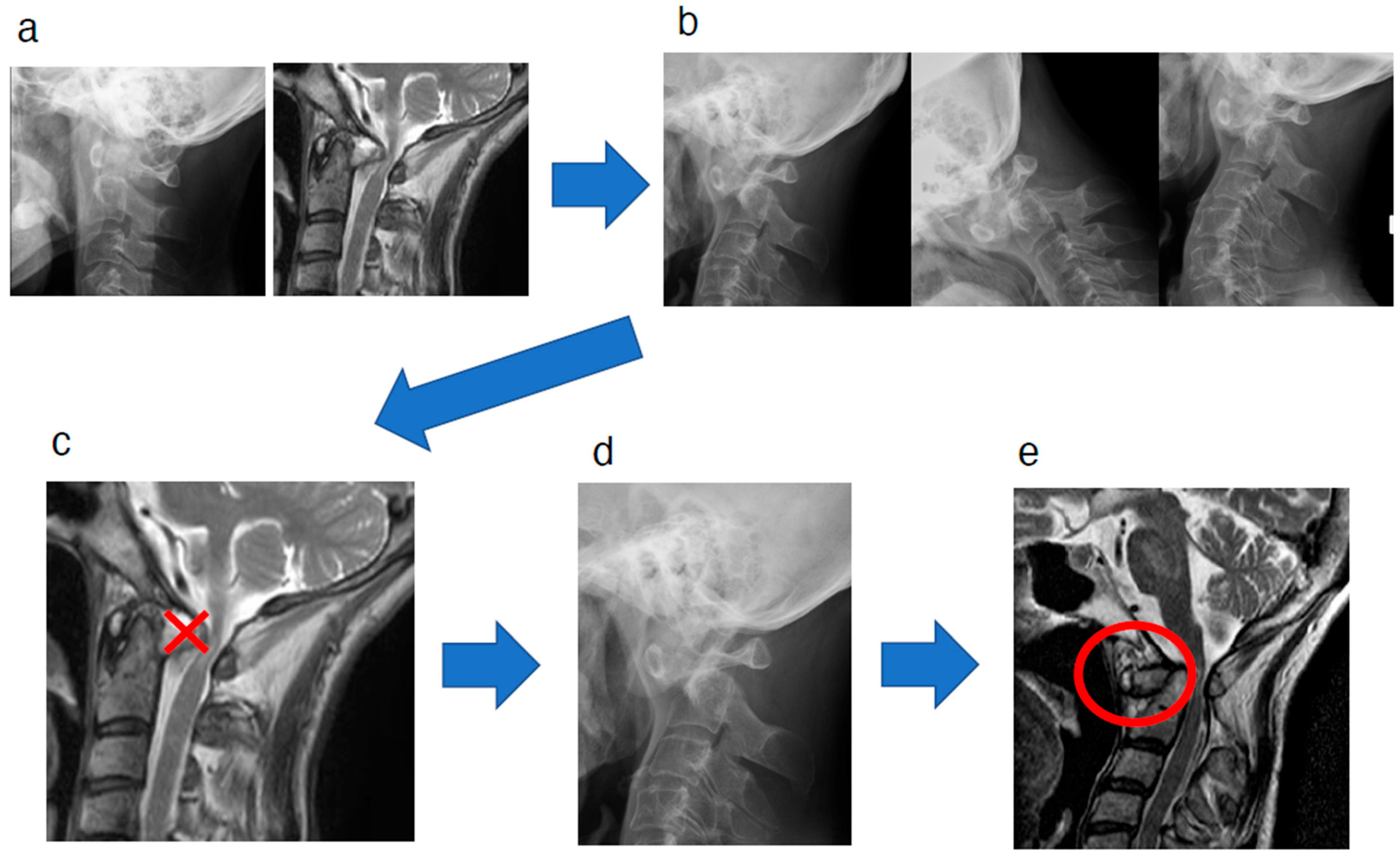
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sze, G.; Brant-Zawadzki, M.N.; Wilson, C.R.; Norman, D.; Newton, T.H. Pseudotumor of the craniovertebral junction associated with chronic subluxation: MR imaging studies. Radiology 1986, 161, 391–394. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, T.; Takada, S.; Tsujimoto, K.; Ozaki, T.; Ishimoto, K.; Tsumura, N.; Shiba, R.; Kurosaka, M. Enlarging retro-odontoid pseudotumor after expanding cervical laminoplasty in the presence of kyphosis. Spine J. 2006, 6, 228–232. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, I.; Shibuya, S.; Arima, N.; Oka, S.; Kanda, Y.; Yamamoto, T. Remarkable reduction or disappearance of retroodontoid pseudotumors after occipitocervical fusion. Report of three cases. J. Neurosurg. Spine 2006, 5, 156–160. [Google Scholar] [CrossRef] [PubMed]
- Kakutani, K.; Doita, M.; Yoshikawa, M.; Okamoto, K.; Maeno, K.; Yurube, T.; Sha, N.; Kurosaka, M.; Nishida, K. C1 laminectomy for retro-odontoid pseudotumor without atlantoaxial subluxation: Review of seven consecutive cases. Eur. Spine J. 2013, 22, 1119–1126. [Google Scholar] [CrossRef] [PubMed]
- Yu, S.H.; Choi, H.J.; Cho, W.H.; Cha, S.H.; Han, I.H. Retro-odontoid pseudotumor without atlantoaxial subluxation or rheumatic arthritis. Korean J. Neurotrauma 2016, 12, 180–184. [Google Scholar] [CrossRef] [PubMed]
- Chikuda, H.; Seichi, A.; Takeshita, K.; Shoda, N.; Ono, T.; Matsudaira, K.; Kawaguchi, H.; Nakamura, K. Radiographic analysis of the cervical spine in patients with retro-odontoid pseudotumors. Spine 2009, 34, E110–E114. [Google Scholar] [CrossRef] [PubMed]
- Buttiens, A.; Vandevenne, J.; Van Cauter, S. Retro-odontoid pseudotumor in a patient with atlanto-occipital assimilation. J. Belg. Soc. Radiol. 2018, 102, 62. [Google Scholar] [CrossRef] [PubMed]
- Kawabata, S.; Kuroshima, K.; Kawaguchi, K.; Takegami, N.; Yurube, T.; Michikawa, T.; Akeda, K.; Kakutani, K.; Fujita, N. Imaging characteristics of non-rheumatoid arthritis patients with retro-odontoid pseudotumor: A multicenter case-control study. Spine 2024, 49, E315–E321. [Google Scholar] [CrossRef] [PubMed]
- Crockard, H.A.; Sett, P.; Geddes, J.F.; Stevens, J.M.; Kendall, B.E.; Pringle, J.A. Damaged ligaments at the craniocervical junction presenting as an extradural tumour: A differential diagnosis in the elderly. J. Neurol. Neurosurg. Psychiatry 1991, 54, 817–821. [Google Scholar] [CrossRef] [PubMed]
- Pettersson, H.; Larsson, E.M.; Holtås, S.; Cronqvist, S.; Egund, N.; Zygmunt, S.; Brattström, H. MR imaging of the cervical spine in rheumatoid arthritis. AJNR Am. J. Neuroradiol. 1988, 9, 573–577. [Google Scholar] [PubMed]
- Yoshida, K.; Hanyu, T.; Takahashi, H.E. Progression of rheumatoid arthritis of the cervical spine: Radiographic and clinical evaluation. J. Orthop. Sci. 1999, 4, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Goel, A.; Dange, N. Immediate postoperative regression of retroodontoid pannus after lateral mass reconstruction in a patient with rheumatoid disease of the craniovertebral junction. Case report. J. Neurosurg. Spine 2008, 9, 273–276. [Google Scholar] [CrossRef] [PubMed]
- Goel, A. Retro-odontoid mass: An evidence of craniovertebral instability. J. Craniovertebr. Junction Spine 2015, 6, 6–7. [Google Scholar] [CrossRef] [PubMed]
- Kaneko, S.; Ishii, K.; Watanabe, K.; Tsuji, T.; Nakamura, M.; Matsumoto, M.; Yato, Y.; Asazuma, T. Exploration of a reliable radiographic assessment method for hinge-like hypermobility at the atlanto-occipital joint. Eur. Spine J. 2018, 27, 1303–1308. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Takeda, H.; Imai, T.; Akaike, Y.; Kawabata, S.; Fujita, N.; Kaneko, S. Change in the Location of a Pseudotumor Around the C2 Odontoid Process from Posterior to Anterior to the Odontoid Process in the Natural Course: A Case with “Antero-Odontoid Pseudotumor” or “Peri-Odontoid Pseudotumor”. J. Clin. Med. 2025, 14, 4182. https://doi.org/10.3390/jcm14124182
Takeda H, Imai T, Akaike Y, Kawabata S, Fujita N, Kaneko S. Change in the Location of a Pseudotumor Around the C2 Odontoid Process from Posterior to Anterior to the Odontoid Process in the Natural Course: A Case with “Antero-Odontoid Pseudotumor” or “Peri-Odontoid Pseudotumor”. Journal of Clinical Medicine. 2025; 14(12):4182. https://doi.org/10.3390/jcm14124182
Chicago/Turabian StyleTakeda, Hiroki, Takaya Imai, Yuki Akaike, Soya Kawabata, Nobuyuki Fujita, and Shinjiro Kaneko. 2025. "Change in the Location of a Pseudotumor Around the C2 Odontoid Process from Posterior to Anterior to the Odontoid Process in the Natural Course: A Case with “Antero-Odontoid Pseudotumor” or “Peri-Odontoid Pseudotumor”" Journal of Clinical Medicine 14, no. 12: 4182. https://doi.org/10.3390/jcm14124182
APA StyleTakeda, H., Imai, T., Akaike, Y., Kawabata, S., Fujita, N., & Kaneko, S. (2025). Change in the Location of a Pseudotumor Around the C2 Odontoid Process from Posterior to Anterior to the Odontoid Process in the Natural Course: A Case with “Antero-Odontoid Pseudotumor” or “Peri-Odontoid Pseudotumor”. Journal of Clinical Medicine, 14(12), 4182. https://doi.org/10.3390/jcm14124182




