Pulmonary Metastasectomy for Colorectal Cancer: Evidence and Outcomes—A Narrative Review
Abstract
1. Introduction
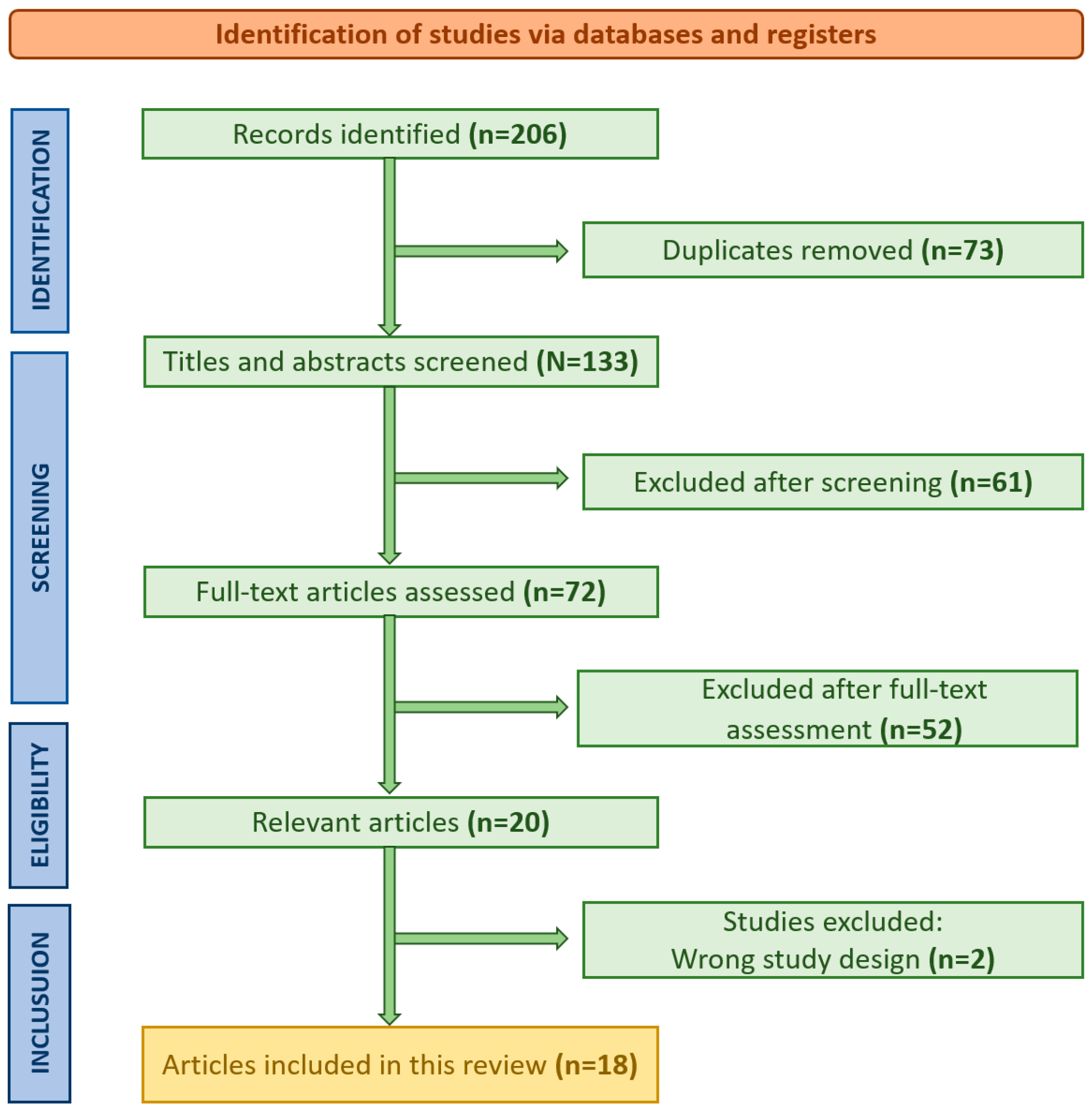
2. Materials and Methods
3. Interdisciplinary Approach and Treatment Efficacy
4. Prognostic Factors
4.1. Disease-Free Interval
4.2. CEA Levels
4.3. Age and Gender
4.4. Performance Status and Comorbidities
4.5. Primary Tumor Characteristics
4.6. Molecular and Genetic Markers
4.7. Response to Systemic Therapy
4.8. Number, Size and Location of Metastases
4.9. Laterality of Lung Metastases
4.10. Resection Extent and Lymphadenectomy
4.11. Radicality
4.12. Primary Tumor Location—Colon vs. Rectum
5. Lung Metastasis Surgery
6. Systemic Therapies and Surgical Synergy
7. Recurrent Metastasis
- Disease-free interval (DFI) after the initial metastasectomy;
- Number and location of recurrent lesions;
- Pulmonary reserve and overall functional status;
8. Survival Outcomes Across Studies
9. Long-Term Outcomes and Challenges
10. Limitations
11. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Petrella, F.; Danuzzo, F.; Sibilia, M.C.; Vaquer, S.; Longarini, R.; Guidi, A.; Raveglia, F.; Libretti, L.; Pirondini, E.; Cara, A.; et al. Colorectal Cancer Pulmonary Metastasectomy: When, Why and How. Cancers 2024, 16, 1408. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mammana, M.; Bergamo, F.; Procaccio, L.; Schiavon, M.; Loupakis, F.; Lonardi, S.; Manai, C.; Schirripa, M.; Fassan, M.; Dei Tos, A.P.; et al. Outcome of patients with colorectal cancer undergoing lung metastases resection: A single-institution retrospective analysis. Tumori J. 2021, 107, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Nanji, S.; Karim, S.; Tang, E.; Brennan, K.; McGuire, A.; Pramesh, C.S.; Booth, C.M. Pulmonary Metastasectomy for Colorectal Cancer: Predictors of Survival in Routine Surgical Practice. Ann. Thorac. Surg. 2018, 105, 1605–1612. [Google Scholar] [CrossRef] [PubMed]
- Al-Ameri, M.; Persson, M.; Bergman, P.; Franco-Cereceda, A.; Sartipy, U. Surgery for pulmonary metastases from colorectal cancer: Survival and prognostic factors. J. Thorac. Dis. 2018, 10, 3372–3380. [Google Scholar] [CrossRef]
- Cao, G.; Cheng, D.; Ye, L.; Pan, Y.; Yang, F.; Lyu, S. Surgical resection of pulmonary metastases from colorectal cancer: 11 years of experiences. PLoS ONE 2017, 12, e0175284. [Google Scholar] [CrossRef] [PubMed]
- Kanzaki, R.; Fukui, E.; Kanou, T.; Ose, N.; Funaki, S.; Minami, M.; Shintani, Y.; Okumura, M. Preoperative evaluation and indications for pulmonary metastasectomy. J. Thorac. Dis. 2021, 13, 2590–2602. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, Y.; Qin, Y. Peri-operative chemotherapy for resectable colorectal lung metastasis: A systematic review and meta-analysis. J. Cancer Res. Clin. Oncol. 2020, 146, 545–553. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Maeda, R.; Suda, T.; Hachimaru, A.; Tochii, D.; Tochii, S.; Takagi, Y. Video-Assisted Thoracoscopic Pulmonary Metastasectomy in Patients with Colorectal Cancer: A Recent 10-Year Single-Institution Experience. World J. Surg. 2016, 40, 1318–1323. [Google Scholar] [CrossRef] [PubMed]
- Hou, Z.; Zhang, H.; Gui, L.; Wang, W.; Zhao, S. Video-assisted thoracoscopic surgery versus open resection of lung metastases from colorectal cancer. Int. J. Clin. Exp. Med. 2015, 8, 13571–13577. [Google Scholar]
- Davini, F.; Ricciardi, S.; Zirafa, C.C.; Romano, G.; Alì, G.; Fontanini, G.; Melfi, F.M.A. Lung metastasectomy after colorectal cancer: Prognostic impact of resection margin on long term survival, a retrospective cohort study. Int. J. Color. Dis. 2020, 35, 9–18, Erratum in: Int. J. Color. Dis. 2020, 35, 371–372. [Google Scholar] [CrossRef] [PubMed]
- Shiono, S.; Okumura, T.; Boku, N.; Hishida, T.; Ohde, Y.; Sakao, Y.; Yoshiya, K.; Hyodo, I.; Mori, K.; Kondo, H. Outcomes of segmentectomy and wedge resection for pulmonary metastases from colorectal cancer. Eur. J. Cardiothorac. Surg. 2017, 51, 504–510. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.S.; Yun, S.H.; Chun, H.K.; Lee, W.Y.; Yun, H.R.; Kim, J.; Kim, K.; Shim, Y.M. Pulmonary resection for metastases from colorectal cancer: Prognostic factors and survival. Int. J. Colorectal Dis. 2007, 22, 699–704. [Google Scholar] [CrossRef] [PubMed]
- Carvajal, C.; Facundo, H.; Puerto, P.; Carreño, J.; Beltrán, R. Lung Metastasectomy from Colorectal Cancer, 10-year Experience in a South American Cancer Center. Front. Surg. 2022, 9, 913678. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Iizasa, T.; Suzuki, M.; Yoshida, S.; Motohashi, S.; Yasufuku, K.; Iyoda, A.; Shibuya, K.; Hiroshima, K.; Nakatani, Y.; Fujisawa, T. Prediction of prognosis and surgical indications for pulmonary metastasectomy from colorectal cancer. Ann. Thorac. Surg. 2006, 82, 254–260. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.H.; Kim, S.; Namgung, M.; Choi, Y.S.; Kim, H.K.; Zo, J.I.; Shim, Y.M.; Kim, J. The prognostic importance of the number of metastases in pulmonary metastasectomy of colorectal cancer. World J. Surg. Oncol. 2015, 13, 222. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gkikas, A.; Kakos, C.; Lampridis, S.; Godolphin, P.J.; Patrini, D. Preoperative prognostic factors for 5-year survival following pulmonary metastasectomy from colorectal cancer: A systematic review and meta-analysis. Eur. J. Cardiothorac. Surg. 2023, 63, ezad059. [Google Scholar] [CrossRef] [PubMed]
- Maniwa, T.; Mori, K.; Ohde, Y.; Okumura, T.; Boku, N.; Hishida, T.; Sakao, Y.; Yoshiya, K.; Hyodo, I.; Kondo, H. Heterogeneity of Tumor Sizes in Multiple Pulmonary Metastases of Colorectal Cancer as a Prognostic Factor. Ann. Thorac. Surg. 2017, 103, 254–260. [Google Scholar] [CrossRef][Green Version]
- Gössling, G.C.L.; Chedid, M.F.; Pereira, F.S.; da Silva, R.K.; Andrade, L.B.; Peruzzo, N.; Saueressig, M.G.; Schwartsmann, G.; Parikh, A.R. Outcomes and Prognostic Factors of Patients with Metastatic Colorectal Cancer Who Underwent Pulmonary Metastasectomy with Curative Intent: A Brazilian Experience. Oncologist 2021, 26, e1581–e1588. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Beckers, P.; Berzenji, L.; Yogeswaran, S.K.; Lauwers, P.; Bilotta, G.; Shkarpa, N.; Hendriks, J.; Van Schil, P.E. Pulmonary metastasectomy in colorectal carcinoma. J. Thorac. Dis. 2021, 13, 2628–2635. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pastorino, U.; Buyse, M.; Friedel, G.; Ginsberg, R.J.; Girard, P.; Goldstraw, P.; Johnston, M.; McCormack, P.; Pass, H.; Putnam, J.B., Jr.; et al. Long-term results of lung metastasectomy: Prognostic analyses based on 5206 cases. J. Thorac. Cardiovasc. Surg. 1997, 113, 37–49. [Google Scholar] [CrossRef] [PubMed]
- Rena, O.; Casadio, C.; Viano, F.; Cristofori, R.; Ruffini, E.; Filosso, P.L.; Maggi, G. Pulmonary resection for metastases from colorectal cancer: Factors influencing prognosis. Twenty-year experience. Eur. J. Cardiothorac. Surg. 2002, 21, 906–912. [Google Scholar] [CrossRef] [PubMed]
- Yedibela, S.; Klein, P.; Feuchter, K.; Hoffmann, M.; Meyer, T.; Papadopoulos, T.; Göhl, J.; Hohenberger, W. Surgical management of pulmonary metastases from colorectal cancer in 153 patients. Ann. Surg. Oncol. 2006, 13, 1538–1544. [Google Scholar] [CrossRef] [PubMed]
- Lin, B.R.; Chang, T.C.; Lee, Y.C.; Lee, P.H.; Chang, K.J.; Liang, J.T. Pulmonary resection for colorectal cancer metastases: Duration between cancer onset and lung metastasis as an important prognostic factor. Ann. Surg. Oncol. 2009, 16, 1026–1032. [Google Scholar] [CrossRef] [PubMed]
- Takakura, Y.; Miyata, Y.; Okajima, M.; Okada, M.; Ohdan, H. Short disease-free interval is a significant risk factor for intrapulmonary recurrence after resection of pulmonary metastases in colorectal cancer. Colorectal Dis. 2010, 12, e68–e75. [Google Scholar] [CrossRef] [PubMed]
- Rama, N.; Monteiro, A.; Bernardo, J.E.; Eugénio, L.; Antunes, M.J. Lung metastases from colorectal cancer: Surgical resection and prognostic factors. Eur. J. Cardiothorac. Surg. 2009, 35, 444–449. [Google Scholar] [CrossRef] [PubMed]
- Gutman, M.; Fidler, I.J. Biology of human colon cancer metastasis. World J. Surg. 1995, 19, 226–234. [Google Scholar] [CrossRef] [PubMed]
- Hammarström, S. The carcinoembryonic antigen (CEA) family: Structures, suggested functions and expression in normal and malignant tissues. Semin. Cancer Biol. 1999, 9, 67–81. [Google Scholar] [CrossRef] [PubMed]
- Meijer, R.P.J.; Galema, H.A.; Faber, R.A.; Bijlstra, O.D.; Maat, A.P.W.M.; Cailler, F.; Braun, J.; Keereweer, S.; Hilling, D.E.; Burggraaf, J.; et al. Intraoperative molecular imaging of colorectal lung metastases with SGM-101: A feasibility study. Eur. J. Nucl. Med. Mol. Imaging 2024, 51, 2970–2979. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Huang, W.L.; Chen, Y.Y.; Chang, C.C.; Yen, Y.T.; Lai, W.W.; Lin, B.W.; Lee, J.C.; Tseng, Y.L. Pulmonary metastasectomy for colorectal cancer: Prognosis analysis disaggregated by the origin of the primary tumor. Asian J. Surg. 2020, 43, 1069–1073. [Google Scholar] [CrossRef] [PubMed]
- Denz, A.; Hahn, V.; Weber, K.; Weber, G.F.; Grützmann, R.; Krautz, C.; Brunner, M. Survival outcome following surgical versus non-surgical treatment of colorectal lung metastasis-a retrospective cohort study. Langenbecks Arch. Surg. 2024, 409, 121. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Choi, H.S.; Jeong, B.K.; Kang, K.M.; Jeong, H.; Song, J.H.; Ha, I.B.; Kwon, O.Y. Tumor Control and Overall Survival after Stereotactic Body Radiotherapy for Pulmonary Oligometastases from Colorectal Cancer: A Meta-Analysis. Cancer Res. Treat. 2020, 52, 1188–1198. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chen, F.; Hanaoka, N.; Sato, K.; Fujinaga, T.; Sonobe, M.; Shoji, T.; Sakai, H.; Miyahara, R.; Bando, T.; Okubo, K.; et al. Prognostic factors of pulmonary metastasectomy for colorectal carcinomas. World J. Surg. 2009, 33, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Kang, D.; Li, J.; Li, Y.; Xu, J.; Yang, J.; Zhang, Z. Prognostic significance of KRAS, NRAS, BRAF, and PIK3CA mutations in stage II/III colorectal cancer: A retrospective study and meta-analysis. PLoS ONE 2025, 20, e0320783. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Uutela, A.; Osterlund, E.; Halonen, P.; Kallio, R.; Ålgars, A.; Salminen, T.; Lamminmäki, A.; Soveri, L.M.; Ristamäki, R.; Lehtomäki, K.; et al. Resectability, conversion, metastasectomy and outcome according to RAS and BRAF status for metastatic colorectal cancer in the prospective RAXO study. Br. J. Cancer 2022, 127, 686–694. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vogelsang, H.; Haas, S.; Hierholzer, C.; Berger, U.; Siewert, J.R.; Präuer, H. Factors influencing survival after resection of pulmonary metastases from colorectal cancer. Br. J. Surg. 2004, 91, 1066–1071. [Google Scholar] [CrossRef] [PubMed]
- Inoue, M.; Ohta, M.; Iuchi, K.; Matsumura, A.; Ideguchi, K.; Yasumitsu, T.; Nakagawa, K.; Fukuhara, K.; Maeda, H.; Takeda, S.; et al. Benefits of surgery for patients with pulmonary metastases from colorectal carcinoma. Ann. Thorac. Surg. 2004, 78, 238–244. [Google Scholar] [CrossRef] [PubMed]
- Dudek, W.; Schreiner, W.; Hohenberger, W.; Klein, P.; Sirbu, H. Forty-Two Years’ Experience with Pulmonary Resections of Metastases from Colorectal Cancer. Thorac. Cardiovasc. Surg. 2017, 65, 560–566. [Google Scholar]
- Yokoyama, S.; Mitsuoka, M.; Kinugasa, T.; Hashiguchi, T.; Matsumoto, R.; Murakami, D.; Nishi, T.; Yoshiyama, K.; Kashihara, M.; Takamori, S.; et al. Survival after initial lung metastasectomy for metastatic colorectal cancer in the modern chemotherapeutic era. BMC Surg. 2017, 17, 54. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kumar, N.A.N.; Verma, K.; Shinde, R.S.; Kammar, P.; Dusane, R.; Desouza, A.; Ostwal, V.; Patil, P.; Engineer, R.; Karimundackal, G.; et al. Pulmonary metastasectomy of colorectal cancer origin: Evaluating process and outcomes. J. Surg. Oncol. 2018, 118, 1292–1300. [Google Scholar] [CrossRef] [PubMed]
- Borasio, P.; Gisabella, M.; Billé, A.; Righi, L.; Longo, M.; Tampellini, M.; Ardissone, F. Role of surgical resection in colorectal lung metastases: Analysis of 137 patients. Int. J. Colorectal Dis. 2011, 26, 183–190. [Google Scholar] [CrossRef] [PubMed]
- Melloni, G.; Doglioni, C.; Bandiera, A.; Carretta, A.; Ciriaco, P.; Arrigoni, G.; Zannini, P. Prognostic factors and analysis of microsatellite instability in resected pulmonary metastases from colorectal carcinoma. Ann. Thorac. Surg. 2006, 81, 2008–2013. [Google Scholar] [CrossRef] [PubMed]
- Moore, K.H.; McCaughan, B.C. Surgical resection for pulmonary metastases from colorectal cancer. ANZ J. Surg. 2001, 71, 143–146. [Google Scholar] [CrossRef] [PubMed]
- Fukada, M.; Matsuhashi, N.; Takahashi, T.; Tanaka, Y.; Okumura, N.; Yamamoto, H.; Shirahashi, K.; Iwata, H.; Doi, K.; Yoshida, K. Prognostic factors in pulmonary metastasectomy and efficacy of repeat pulmonary metastasectomy from colorectal cancer. World J. Surg. Oncol. 2020, 18, 314. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ossoegawa, A.; Kometani, T.; Fukuyama, S.; Hirai, F.; Seto, T.; Sugio, K.; Ichinose, Y. Prognostic Factors for Survival after Resection of Pulmonary Metastases from Colorectal Carcinoma. Ann. Thorac. Cardiovasc. Surg. 2016, 22, 6–11. [Google Scholar] [CrossRef]
- Treasure, T.; Macbeth, F. The belief in clinical benefit from lung metastasectomy in colorectal cancer is questioned by the PulMiCC study and its nested randomised controlled trial. Langenbecks Arch. Surg. 2024, 409, 262. [Google Scholar] [CrossRef] [PubMed]
- Sponholz, S.; Schirren, J. Pulmonary metastasectomy: The discussion continues. Eur. J. Cardiothorac. Surg. 2022, 62, ezac315. [Google Scholar] [CrossRef] [PubMed]
- Ratnayake, C.B.B.; Wells, C.I.; Atherton, P.; Hammond, J.S.; White, S.; French, J.J.; Manas, D.; Pandanaboyana, S. Meta-analysis of survival outcomes following surgical and non surgical treatments for colorectal cancer metastasis to the lung. ANZ J. Surg. 2021, 91, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Zang, Q.; Wen, Y.; Pan, Z.; Yao, Z.; Huang, M.; Huang, J.; Chen, J.; Wang, R. Prognostic value of KRAS mutation in patients undergoing pulmonary metastasectomy for colorectal cancer: A systematic review and meta-analysis. Crit. Rev. Oncol. Hematol. 2021, 160, 103308. [Google Scholar] [CrossRef] [PubMed]
- Diaz, L.A., Jr.; Shiu, K.K.; Kim, T.W.; Jensen, B.V.; Jensen, L.H.; Punt, C.; Smith, D.; Garcia-Carbonero, R.; Benavides, M.; Gibbs, P.; et al. Pembrolizumab versus chemotherapy for microsatellite instability-high or mismatch repair-deficient metastatic colorectal cancer (KEYNOTE-177): Final analysis of a randomised, open-label, phase 3 study. Lancet Oncol. 2022, 23, 659–670. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Treasure, T.; Leonard, P.; Milosevic, M.; Williams, N.R.; Macbeth, F.; Farewell, V. Pulmonary Metastasectomy in Colorectal Cancer: The PulMiCC randomised controlled trial. Br. J. Surg. 2020, 107, e489–e490. [Google Scholar] [CrossRef] [PubMed]
- Ihn, M.H.; Kim, D.W.; Cho, S.; Oh, H.K.; Jheon, S.; Kim, K.; Shin, E.; Lee, H.S.; Chung, J.H.; Kang, S.B. Curative Resection for Metachronous Pulmonary Metastases from Colorectal Cancer: Analysis of Survival Rates and Prognostic Factors. Cancer Res. Treat. 2017, 49, 104–115. [Google Scholar] [CrossRef] [PubMed]
- Gao, Z.; Jin, X.; Wu, Y.C.; Zhang, S.J.; Wu, S.K.; Wang, X. Effect of perioperative chemotherapy on resection of isolated pulmonary metastases from colorectal cancer: A single center experience. World J. Gastrointest. Oncol. 2024, 16, 3457–3470. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sponholz, S.; Oguzhan, S.; Mese, M.; Schirren, M.; Kirschbaum, A.; Schirren, J. The impact of primary tumor location on prognosis after colorectal lung metastasectomy. Int. J. Colorectal Dis. 2021, 36, 1731–1737. [Google Scholar] [CrossRef] [PubMed]
- Vidarsdottir, H.; Siesing, C.; Nodin, B.; Jönsson, P.; Eberhard, J.; Jirström, K.; Brunnström, H. Clinical significance of RBM3 expression in surgically treated colorectal lung metastases and paired primary tumors. J. Surg. Oncol. 2021, 123, 1144–1156. [Google Scholar] [CrossRef] [PubMed]
- VodiČka, J.; Fichtl, J.; Šebek, J.; ProchÁzkovÁ, K.; SkÁla, M.; TŘeŠka, V.; Kormunda, S.; VaŇkovÁ, B.; SvatoŇ, M.; TopolČan, O.; et al. Outcomes and Prognostic Factors Following Surgical Treatment of Pulmonary Metastases from Colorectal Carcinoma. Anticancer Res. 2020, 40, 7045–7051. [Google Scholar] [CrossRef] [PubMed]
- Corsini, E.M.; Mitchell, K.G.; Correa, A.; Morris, V.K.; Antonoff, M.B.; MD Anderson Pulmonary Metastasectomy Working Group. Effect of primary colorectal cancer tumor location on survival after pulmonary metastasectomy. J. Thorac. Cardiovasc. Surg. 2021, 162, 296–305. [Google Scholar] [CrossRef] [PubMed]
- Rapicetta, C.; Lococo, F.; Davini, F.; Carleo, F.; Kauppi, J.; Di Stefano, T.S.; Ricciardi, S.; Di Martino, M.; Räsänen, J.; Paci, M.; et al. Is Adjuvant Chemotherapy Worthwhile After Radical Resection for Single Lung Metastasis From Colorectal Cancer? A Multicentric Analysis Evaluating the Risk of Recurrence. Front. Oncol. 2019, 9, 763. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Renaud, S.; Seitlinger, J.; St-Pierre, D.; Garfinkle, R.; Al Lawati, Y.; Guerrera, F.; Ruffini, E.; Falcoz, P.E.; Massard, G.; Ferri, L.; et al. Prognostic value of neutrophil to lymphocyte ratio in lung metastasectomy for colorectal cancer. Eur. J. Cardiothorac. Surg. 2019, 55, 948–955. [Google Scholar] [CrossRef] [PubMed]
- Fournel, L.; Maria, S.; Seminel, M.; Nesci, J.; Mansuet-Lupo, A.; Guinet, C.; Magdeleinat, P.; Bobbio, A.; Regnard, J.F.; Alifano, M. Prognostic factors after pulmonary metastasectomy of colorectal cancers: A single-center experience. J. Thorac. Dis. 2017, 9 (Suppl. S12), S1259–S1266. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sun, F.; Chen, L.; Shi, M.; Yang, X.; Li, M.; Yang, X.; Dai, X.; Zhan, C.; Shi, Y.; Wang, Q. Prognosis of video-assisted thoracoscopic pulmonary metastasectomy in patients with colorectal cancer lung metastases: An analysis of 154 cases. Int. J. Colorectal Dis. 2017, 32, 897–905. [Google Scholar] [CrossRef]
- Karim, S.; Nanji, S.; Brennan, K.; Pramesh, C.S.; Booth, C.M. Chemotherapy for resected colorectal cancer pulmonary metastases: Utilization and outcomes in routine clinical practice. Eur. J. Surg. Oncol. 2017, 43, 1481–1487. [Google Scholar] [CrossRef] [PubMed]
- Batchelor, T.; Hasan, J.; Macbeth, F.; Shackcloth, M.; Treasure, T. Randomised Controlled Trial Evidence Questions the Assumption that Pulmonary Metastasectomy Benefits Patients with Colorectal Cancer. Ann. Surg. Oncol. 2021, 28, 4066–4067. [Google Scholar] [CrossRef] [PubMed]
- Treasure, T.; Williams, N.R.; Macbeth, F. The full cohort of 512 patients and the nested controlled trial in 93 patients in the Pulmonary Metastasectomy in Colorectal Cancer (PulMiCC) study raise doubts about the effective size at present claimed. J. Cardiothorac. Surg. 2022, 17, 9. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Brew-Graves, C.; Farewell, V.; Monson, K.; Milošević, M.; Williams, N.R.; Morris, E.; Macbeth, F.; Treasure, T.; Fallowfield, L. Pulmonary metastasectomy in colorectal cancer: Health utility scores by EQ-5D-3L in a randomized controlled trial show no benefit from lung metastasectomy. Colorectal Dis. 2021, 23, 200–205. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Milosevic, M.; Edwards, J.; Tsang, D.; Dunning, J.; Shackcloth, M.; Batchelor, T.; Coonar, A.; Hasan, J.; Davidson, B.; Marchbank, A.; et al. Pulmonary Metastasectomy in Colorectal Cancer: Updated analysis of 93 randomized patients—Control survival is much better than previously assumed. Colorectal Dis. 2020, 22, 1314–1324. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Study | Year | Number of Patients | 5-Year Survival | Patient Characteristics | Contribution | Limitations | Key Clinical Insights |
|---|---|---|---|---|---|---|---|
| Gao et al. [52] | 2024 | 120 | 72% | Selected patients with single or few metastases; CEA monitoring; most received perioperative chemotherapy. | Highlighted both survival benefit and recurrence risk post-PM, emphasizing need for patient selection and long-term monitoring. | Retrospective, single-center; no control group; potential selection bias. | Longer disease-free interval and solitary lesions predict better survival. |
| Denz et al. [30] | 2024 | 418 | 81.2% | Median age 65; mainly 1–3 nodules; R0 resections; no MSI/MMR data reported. | Demonstrated a significant survival advantage with PM over non-surgical care, reinforcing surgical value in selected cases. | Retrospective study; no comparison with non-surgical treatment. | Repeat metastasectomy feasible with 58% 5-yr OS; selection is critical. |
| Carvajal et al. [13] | 2022 | 82 | 33.2% | Younger patients; some with extrapulmonary disease; low disease volume overall. | Provided real-world survival outcomes from a South American cancer center, offering insight into feasibility and effectiveness of PM in LMIC settings. | Retrospective, single-institution; limited generalizability. | Surgical intent leads to improved OS; patient comorbidities impact outcomes. |
| Gössling et al. [18] | 2021 | 58 | 49.80% | ECOG 0–1; 1–3 pulmonary lesions; most had preoperative chemotherapy. | Reported a 5-year survival of 49.8%, supporting curative-intent pulmonary metastasectomy as a viable option in selected mCRC patients. | Retrospective, small sample; selection bias possible. | Curative resection linked to improved survival in real-world practice. |
| Sponholz et al. [53] | 2021 | 233 | 47% | Left vs. right primary tumor location; limited number of metastases; molecular status not reported. | Demonstrated that primary tumor location significantly impacts survival outcomes after lung metastasectomy for CRC. | Retrospective data; no randomization or comparison group. | Primary tumor location influences post-metastasectomy survival. |
| Vidarsdottir et al. [54] | 2021 | 216 | 56% | ~40% KRAS mutant; elevated preoperative CEA; all had complete lung resections. | Analyzed surgically treated CRC lung metastases and highlighted the prognostic relevance of tumor biology in survival outcomes. | Retrospective; small cohort; lacked molecular stratification. | CEA and KRAS mutation status affect prognosis post-metastasectomy. |
| Davini et al. [10] | 2020 | 210 | 54% | Majority with solitary lesions; older age group; good performance status. | Showed that negative resection margins are strongly associated with improved long-term survival post-metastasectomy. | Retrospective analysis; surgical candidates only; no systemic therapy control. | Pulmonary resection feasible even in elderly with good selection. |
| Vodička et al. [55] | 2020 | 104 | 54.30% | Solitary lesions; R0 resections; patients without major organ dysfunction. | Analyzed prognostic factors and outcomes, supporting metastasectomy as a valid treatment in multimodal CRC management. | Retrospective design; potential lead-time and selection biases. | Good outcomes achieved after resection of solitary metastases. |
| Huang et al. [29] | 2020 | 179 | 40.80% | Variable primary tumor locations; clinically stable; preoperative therapy not detailed. | Emphasized the prognostic relevance of primary tumor location in CRC patients undergoing lung metastasectomy. | Small sample size; retrospective; no standard criteria for surgery. | Right-sided primary tumors associated with better outcomes. |
| Corsini et al. [56] | 2020 | 194 | 57% | DFI > 12 months common; ~50% VATS; few underwent repeat resections. | Revealed significant survival differences depending on whether the primary tumor was right- or left-sided. | Retrospective; lacked uniform treatment protocols. | VATS resection is safe and effective; short DFI predicts recurrence. |
| Rapicetta et al. [57] | 2019 | 344 | 61.90% | Solitary metastasis predominant; good functional status; frequent adjuvant therapy use. | Assessed the value of adjuvant chemotherapy after resection of a single metastasis, indicating possible reduction in recurrence. | Retrospective; no comparison to non-surgical alternatives. | Repeat metastasectomy offers durable outcomes in oligometastatic patients. |
| Renaud et al. [58] | 2019 | 574 | 58% | Good general health; moderate metastatic burden; low NLR associated with benefit. | Found that elevated neutrophil-to-lymphocyte ratio is linked to worse prognosis in lung metastasectomy for CRC. | Retrospective; surgical approach varied between centers. | Multicenter data support surgery in selected metastatic CRC cases. |
| Nanji et al. [3] | 2018 | 420 | 40% | 45% with multiple lesions; comorbidities recorded; adequate pulmonary reserve. | Highlighted key predictors of survival in real-world metastasectomy practice, including margin status and comorbidity burden. | Single-center; lacked molecular profiling data. | Worse prognosis in patients with multiple heterogeneous lesions. |
| Al-Ameri et al. [4] | 2018 | 756 | 56% | Middle-aged; typically 2 lesions; R0 resections in most cases. | Identified several clinicopathological factors influencing survival, supporting surgical intervention in selected patients. | Retrospective; outcomes possibly influenced by surgical technique. | Multiple surgeries do not compromise long-term survival. |
| Fournel et al. [59] | 2017 | 306 | 59% | Solitary or double peripheral lesions; all treated with curative intent. | Confirmed the prognostic value of complete resection and highlighted recurrence risks even after radical surgery. | Selection bias; heterogeneous patient population. | Molecular profiling may guide future patient selection. |
| Sun et al. [60] | 2017 | 154 | 71.30% | All underwent VATS; lesions < 3 cm; limited metastatic spread. | Demonstrated favorable outcomes of VATS approach in CRC lung metastasectomy with a high 5-year survival rate. | Retrospective cohort; unclear systemic treatment details. | Surgical margin status key for long-term survival. |
| Karim et al. [61] | 2017 | 377 | 40% | All had resected primary CRC; good performance status; molecular profile unclear. | Evaluated the use of chemotherapy post-metastasectomy, showing real-world trends and variable outcome benefits. | No survival benefit in adjusted analysis; matched control group. | RCT (PulMiCC) challenges survival benefit of PM in unselected patients. |
| Yokoyama et al. [38] | 2017 | 59 | 54.30% | KRAS/BRAF status known; modern chemotherapy use; mostly solitary lung lesions. | Evaluated outcomes of initial lung metastasectomy in mCRC patients, demonstrating favorable survival in the era of modern chemotherapy. | Retrospective; KRAS/BRAF status not uniformly reported. | KRAS/BRAF status linked to survival post-metastasectomy. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Papatriantafyllou, A.; Grapatsas, K.; Mulita, F.; Baikoussis, N.G.; Liolis, E.; Tchabashvili, L.; Tasios, K.; Papadoulas, S.; Dahm, M.; Leivaditis, V. Pulmonary Metastasectomy for Colorectal Cancer: Evidence and Outcomes—A Narrative Review. J. Clin. Med. 2025, 14, 4172. https://doi.org/10.3390/jcm14124172
Papatriantafyllou A, Grapatsas K, Mulita F, Baikoussis NG, Liolis E, Tchabashvili L, Tasios K, Papadoulas S, Dahm M, Leivaditis V. Pulmonary Metastasectomy for Colorectal Cancer: Evidence and Outcomes—A Narrative Review. Journal of Clinical Medicine. 2025; 14(12):4172. https://doi.org/10.3390/jcm14124172
Chicago/Turabian StylePapatriantafyllou, Athanasios, Konstantinos Grapatsas, Francesk Mulita, Nikolaos G. Baikoussis, Elias Liolis, Levan Tchabashvili, Konstantinos Tasios, Spyros Papadoulas, Manfred Dahm, and Vasileios Leivaditis. 2025. "Pulmonary Metastasectomy for Colorectal Cancer: Evidence and Outcomes—A Narrative Review" Journal of Clinical Medicine 14, no. 12: 4172. https://doi.org/10.3390/jcm14124172
APA StylePapatriantafyllou, A., Grapatsas, K., Mulita, F., Baikoussis, N. G., Liolis, E., Tchabashvili, L., Tasios, K., Papadoulas, S., Dahm, M., & Leivaditis, V. (2025). Pulmonary Metastasectomy for Colorectal Cancer: Evidence and Outcomes—A Narrative Review. Journal of Clinical Medicine, 14(12), 4172. https://doi.org/10.3390/jcm14124172








