The Influence of Orthogeriatric Co-Management on Economical Outcomes After Treatment of Proximal Femoral Fractures: Real-World Data of Comparable Cohorts Originating from the Same Geographic Area
Abstract
1. Background
2. Methods
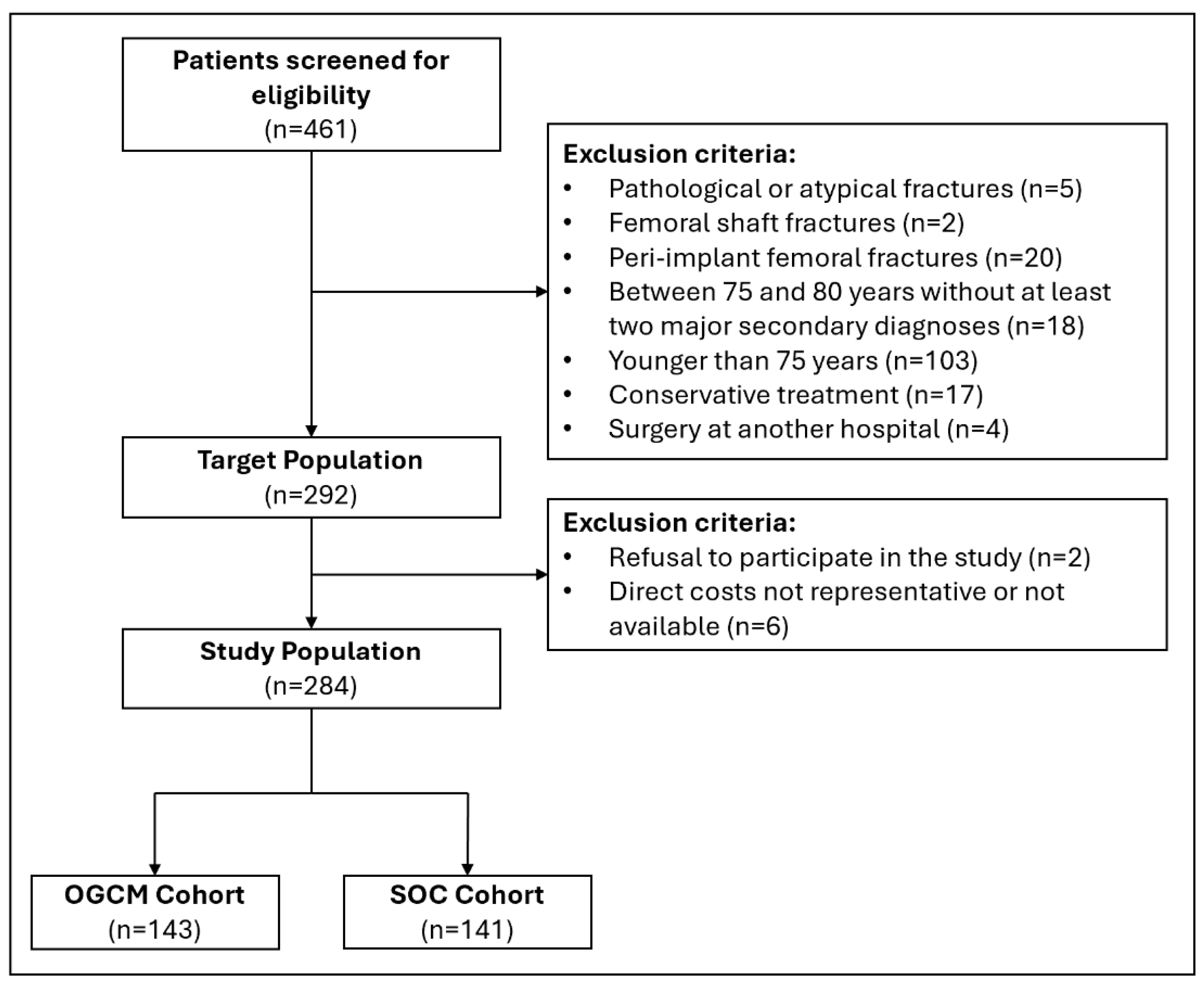
2.1. Study Design
2.2. Orthogeriatric Co-Management
2.3. Standard of Care
2.4. Data Source
2.5. Outcome Measures
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| OGCM | Orthogeriatric co-management |
| SOC | Standard of care |
| LOS | Length of stay |
| CHF | Confoederatio Helvetica Franc |
| USD | United States dollar |
| ICU | Intensive care unit |
| IQR | Interquartile range |
References
- Baroni, M.; Serra, R.; Boccardi, V.; Ercolani, S.; Zengarini, E.; Casucci, P.; Valecchi, R.; Rinonapoli, G.; Caraffa, A.; Mecocci, P.; et al. The orthogeriatric comanagement improves clinical outcomes of hip fracture in older adults. Osteoporos. Int. 2019, 30, 907–916. [Google Scholar] [CrossRef] [PubMed]
- Friedman, S.M.; Mendelson, D.A.; Kates, S.L.; McCann, R.M. Geriatric Co-Management of Proximal Femur Fractures: Total Quality Management and Protocol-Driven Care Result in Better Outcomes for a Frail Patient Population. J. Am. Geriatr. Soc. 2008, 56, 1349–1356. [Google Scholar] [CrossRef] [PubMed]
- Sing, C.; Lin, T.; Bartholomew, S.; Bell, J.S.; Bennett, C.; Beyene, K.; Bosco-Levy, P.; Bradbury, B.D.; Chan, A.H.Y.; Chandran, M.; et al. Global Epidemiology of Hip Fractures: Secular Trends in Incidence Rate, Post-Fracture Treatment, and All-Cause Mortality. J. Bone Miner. Res. 2023, 38, 1064–1075. [Google Scholar] [CrossRef]
- Heyzer, L.; Ramason, R.; De Castro Molina, J.; Lim Chan, W.; Loong, C.; Kee Kwek, E. Integrated hip fracture care pathway (IHFCP): Reducing complications and improving outcomes. Singap. Med. J. 2022, 63, 439. [Google Scholar] [CrossRef]
- Macwan, A.A.; Panda, A.P.; Sondur, S.; Rath, S. Benchmarking institutional geriatric hip fracture management: A prelude to a care quality improvement initiative. Eur. J. Orthop. Surg. Traumatol. 2024, 34, 1571–1580. [Google Scholar] [CrossRef]
- Neuerburg, C.; Förch, S.; Gleich, J.; Böcker, W.; Gosch, M.; Kammerlander, C.; Mayr, E. Improved outcome in hip fracture patients in the aging population following co-managed care compared to conventional surgical treatment: A retrospective, dual-center cohort study. BMC Geriatr. 2019, 19, 330. [Google Scholar] [CrossRef] [PubMed]
- Saul, D.; Riekenberg, J.; Ammon, J.C.; Hoffmann, D.B.; Sehmisch, S. Hip Fractures: Therapy, Timing, and Complication Spectrum. Orthop. Surg. 2019, 11, 994–1002. [Google Scholar] [CrossRef]
- Veronese, N.; Maggi, S. Epidemiology and social costs of hip fracture. Injury 2018, 49, 1458–1460. [Google Scholar] [CrossRef]
- González Montalvo, J.I.; Gotor Pérez, P.; Martín Vega, A.; Alarcón Alarcón, T.; Mauleón Álvarez de Linera, J.L.; Gil Garay, E.; Cimbrelo, E.G.; Biarge, J.A. La unidad de ortogeriatría de agudos. Evaluación de su efecto en el curso clínico de los pacientes con fractura de cadera y estimación de su impacto económico. Rev. Esp. Geriatr. Gerontol. 2011, 46, 193–199. [Google Scholar] [CrossRef]
- Folbert, E.C.; Hegeman, J.H.; Vermeer, M.; Regtuijt, E.M.; van der Velde, D.; Duis, H.J.T.; Slaets, J.P. Improved 1-year mortality in elderly patients with a hip fracture following integrated orthogeriatric treatment. Osteoporos. Int. 2017, 28, 269–277. [Google Scholar] [CrossRef]
- Schoeneberg, C.; Pass, B.; Volland, R.; Knobe, M.; Eschbach, D.; Ketter, V.; Lendemans, S.; Aigner, R. Four-month outcome after proximal femur fractures and influence of early geriatric rehabilitation: Data from the German Centres of Geriatric Trauma DGU. Arch. Osteoporos. 2021, 16, 68. [Google Scholar] [CrossRef] [PubMed]
- Kates, S.L.; Mendelson, D.A.; Friedman, S.M. The value of an organized fracture program for the elderly: Early results. J. Orthop. Trauma. 2011, 25, 233–237. [Google Scholar] [CrossRef]
- Schulz, C.; Büchele, G.; Peter, R.S.; Rothenbacher, D.; Brettschneider, C.; Liener, U.C.; Becker, C.; Rapp, K.; König, H.-H. Health-economic evaluation of collaborative orthogeriatric care for patients with a hip fracture in Germany: A retrospective cohort study using health and long-term care insurance claims data. Eur. J. Health Econ. 2021, 22, 873–885. [Google Scholar] [CrossRef] [PubMed]
- Rocca GJDella Moylan, K.C.; Crist, B.D.; Volgas, D.A.; Stannard, J.P.; Mehr, D.R. Comanagement of Geriatric Patients With Hip Fractures. Geriatr. Orthop. Surg. Rehabil. 2013, 4, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Titler, M.; Dochterman, J.; Kim, T.; Kanak, M.; Shever, L.; Picone, D.M.; Everett, L.; Budreau, G. Cost of care for seniors hospitalized for hip fracture and related procedures. Nurs. Outlook 2007, 55, 5–14.e4. [Google Scholar] [CrossRef]
- Ginsberg, G.; Adunsky, A.; Rasooly, I. A cost-utility analysis of a comprehensive orthogeriatric care for hip fracture patients, compared with standard of care treatment. HIP Int. 2013, 23, 570–575. [Google Scholar] [CrossRef]
- Rapp, K.; Becker, C.; Todd, C.; Rothenbacher, D.; Schulz, C.; König, H.-H.; Liener, U.; Hartwig, E.; Büchele, G. The Association Between Orthogeriatric Co-Management and Mortality Following Hip Fracture. Dtsch. Arztebl. Int. 2020, 117, 53. [Google Scholar] [CrossRef]
- Joeris, A.; Sprague, S.; Blauth, M.; Gosch, M.; Wattanapanom, P.; Jarayabhand, R.; Poeze, M.; Wong, M.K.; Kwek, E.B.K.; Hegeman, J.H.; et al. Cost-effectiveness analysis of the Geriatric Fracture Center (GFC) concept: A prospective multicentre cohort study. BMJ Open 2023, 13, e072744. [Google Scholar] [CrossRef]
- Kates, S.L.; Mendelson, D.A.; Friedman, S.M. Co-managed care for fragility hip fractures (Rochester model). Osteoporos. Int. 2010, 21, 621–625. [Google Scholar] [CrossRef]
- Leal, J.; Gray, A.M.; Hawley, S.; Prieto-Alhambra, D.; Delmestri, A.; Arden, N.K.; Cooper, C.; Javaid, M.K.; Judge, A. Cost-Effectiveness of Orthogeriatric and Fracture Liaison Service Models of Care for Hip Fracture Patients: A Population-Based Study. J. Bone Miner. Res. 2017, 32, 203–211. [Google Scholar] [CrossRef]
- Miura, L.N.; DiPiero, A.R.; Homer, L.D. Effects of a Geriatrician-Led Hip Fracture Program: Improvements in Clinical and Economic Outcomes. J. Am. Geriatr. Soc. 2009, 57, 159–167. [Google Scholar] [CrossRef] [PubMed]
- Tan, L.; Wong, S.; Kwek, E. Inpatient cost for hip fracture patients managed with an orthogeriatric care model in Singapore. Singap. Med. J. 2017, 58, 139–144. [Google Scholar] [CrossRef]
- Swart, E.; Vasudeva, E.; Makhni, E.C.; Macaulay, W.; Bozic, K.J. Dedicated Perioperative Hip Fracture Comanagement Programs are Cost-effective in High-volume Centers: An Economic Analysis. Clin. Orthop. Relat. Res. 2016, 474, 222–233. [Google Scholar] [CrossRef]
- Kates, S.L.; Blake, D.; Bingham, K.W.; Kates, O.S.; Mendelson, D.A.; Friedman, S.M. Comparison of an Organized Geriatric Fracture Program to United States Government Data. Geriatr. Orthop. Surg. Rehabil. 2010, 1, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.H.; Lim, Y.W.; Lam, K.S. Economic cost of osteoporotic hip fractures in Singapore. Singap. Med. J. 2008, 49, 980–984. [Google Scholar]
- Khasraghi, F.A.; Christmas, C.; Lee, E.J.; Mears, S.C.; Wenz, J.F. Effectiveness of a multidisciplinary team approach to hip fracture management. J. Surg. Orthop. Adv. 2005, 14, 27–31. [Google Scholar] [PubMed]
- Callan, K.T.; Donnelly, M.; Lung, B.; McLellan, M.; DiGiovanni, R.; McMaster, W.; Yang, S.; Stitzlein, R. Risk factors for postoperative delirium in orthopaedic hip surgery patients: A database review. BMC Musculoskelet. Disord. 2024, 25, 71. [Google Scholar] [CrossRef]
- Uriz-Otano, F.; Uriz-Otano, J.I.; Malafarina, V. Factors Associated With Short-Term Functional Recovery in Elderly People With a Hip Fracture. Influ. Cogn. Impairment. J. Am. Med. Dir. Assoc. 2015, 16, 215–220. [Google Scholar] [CrossRef]
- Roberts, H.C. The effectiveness of implementing a care pathway for femoral neck fracture in older people: A prospective controlled before and after study. Age Ageing 2004, 33, 178–184. [Google Scholar] [CrossRef]
- Kimmel, L.A.; Liew, S.M.; Sayer, J.M.; Holland, A.E. HIP4Hips (High Intensity Physiotherapy for Hip fractures in the acute hospital setting): A randomised controlled trial. Med. J. Aust. 2016, 205, 73–78. [Google Scholar] [CrossRef]
- Arkley, J.; Dixon, J.; Wilson, F.; Charlton, K.; Ollivere, B.J.; Eardley, W. Assessment of Nutrition and Supplementation in Patients With Hip Fractures. Geriatr. Orthop. Surg. Rehabil. 2019, 10, 2151459319879804. [Google Scholar] [CrossRef] [PubMed]
- Henderson, C.Y.; Shanahan, E.; Butler, A.; Lenehan, B.; O’cOnnor, M.; Lyons, D.; Ryan, J.P. Dedicated orthogeriatric service reduces hip fracture mortality. Ir. J. Med. Sci. (1971-) 2017, 186, 179–184. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | OGCM (n = 143) | SOC (n = 141) | p-Value |
|---|---|---|---|
| Age [years], mean (±SD) | 87.3 (5.6) | 86.5 (6.2) | 0.25 |
| Women, n (%) | 112 (78.3) | 99 (70.2) | 0.15 |
| BMI [kg/m2], mean (±SD) | 23.1 (4.2) | 23.9 (5.7) | 0.22 |
| Fracture type, n (%) | |||
| Trochanteric | 72 (50.3) | 79 (56) | 0.40 |
| Femoral neck | 71 (49.7) | 62 (44) | 0.40 |
| Left side fractures, n (%) | 69 (48.3) | 55 (39) | 0.15 |
| Residence before admission, n (%) | |||
| Home | 84 (58.7) | 86 (61) | 0.79 |
| Retirement home | 14 (9.8) | 27 (19.1) | 0.038 |
| Nursing home | 45 (31.5) | 27 (19.1) | 0.025 |
| Other hospital | 0 (0) | 1 (0.8) | 0.99 |
| Mobility before admission, n (%) | |||
| Independent | 55 (39.3) | 50 (35.7) | 0.62 |
| Stick | 19 (13.6) | 21 (15) | 0.86 |
| Rollator | 49 (35) | 55 (39.3) | 0.54 |
| Walker | 0 (0) | 1 (0.7) | 1 |
| Helping person | 4 (2.8) | 2 (1.4) | 0.68 |
| Wheelchair | 13 (9.3) | 11 (7.9) | 0.83 |
| Barthel Index [0–100], mean (±SD) | 30 (17.5) | 45.9 (20) | <0.0001 |
| SOMC Test [0–28], mean (±SD) | 13.5 (10.1) | 9.7 (7.4) | 0.018 |
| NRS [0–7], mean (±SD) | 3.4 (1) | 3 (1.4) | 0.06 |
| ASA classification [1–6], n (%) | |||
| 2 | 22 (15.4) | 33 (23.4) | 0.12 |
| 3 | 108 (75.5) | 96 (68.1) | 0.21 |
| 4 | 13 (9.1) | 12 (8.5) | 1 |
| Antithrombotic agents, n (%) | 75 (52.4) | 81 (57.4) | 0.47 |
| Antiosteoporotic medication, n (%) | 87 (60.8) | 63 (44.7) | 0.009 |
| Outcome | OGCM (n = 143) | SOC (n = 141) | p-Value |
|---|---|---|---|
| Length of stay [days], median (IQR) | 6 (5–8) | 7 (6–9) | 0.002 |
| Time to surgery [h], median (IQR) | 15.8 (7–26) | 15.4 (10–23) | 0.77 |
| Readmissions, n (%) | |||
| 30 days | 40 (35.7) | 41 (38.7) | 0.40 |
| 1 year | 9 (6.1) | 21 (14.7) | 0.76 |
| Revisions, n (%) | |||
| 30 days | 3 (2.4) | 3 (2.4) | 1 |
| 1 year | 9 (8.7) | 11 (11.5) | 0.67 |
| Mortality, n (%) | |||
| 30 days | 12 (8.8) | 11 (8) | 1 |
| 1 year | 33 (24.1) | 43 (31.4) | 0.23 |
| Complications, n (%) | |||
| Medical | 78 (54.5) | 92 (65.2) | 0.09 |
| Surgical | 9 (6.3) | 14 (9.9) | 0.37 |
| Delirium, n (%) | 54 (37.8) | 66 (46.8) | 0.16 |
| Residence after discharge, n (%) | |||
| Home | 3 (2.1) | 4 (2.8) | 0.99 |
| Retirement home | 9 (6.3) | 21 (14.9) | 0.030 |
| Nursing home | 47 (32.9) | 29 (20.6) | 0.027 |
| Geriatric rehabilitation | 45 (31.5) | 65 (46.1) | 0.013 |
| Musculoskeletal rehabilitation | 33 (23.1) | 18 (12.7) | 0.035 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Känel, S.; Känel, M.; Kabelitz, M.; Aggeler, K.; Dietrich, M. The Influence of Orthogeriatric Co-Management on Economical Outcomes After Treatment of Proximal Femoral Fractures: Real-World Data of Comparable Cohorts Originating from the Same Geographic Area. J. Clin. Med. 2025, 14, 4149. https://doi.org/10.3390/jcm14124149
Känel S, Känel M, Kabelitz M, Aggeler K, Dietrich M. The Influence of Orthogeriatric Co-Management on Economical Outcomes After Treatment of Proximal Femoral Fractures: Real-World Data of Comparable Cohorts Originating from the Same Geographic Area. Journal of Clinical Medicine. 2025; 14(12):4149. https://doi.org/10.3390/jcm14124149
Chicago/Turabian StyleKänel, Samuel, Manuel Känel, Method Kabelitz, Kim Aggeler, and Michael Dietrich. 2025. "The Influence of Orthogeriatric Co-Management on Economical Outcomes After Treatment of Proximal Femoral Fractures: Real-World Data of Comparable Cohorts Originating from the Same Geographic Area" Journal of Clinical Medicine 14, no. 12: 4149. https://doi.org/10.3390/jcm14124149
APA StyleKänel, S., Känel, M., Kabelitz, M., Aggeler, K., & Dietrich, M. (2025). The Influence of Orthogeriatric Co-Management on Economical Outcomes After Treatment of Proximal Femoral Fractures: Real-World Data of Comparable Cohorts Originating from the Same Geographic Area. Journal of Clinical Medicine, 14(12), 4149. https://doi.org/10.3390/jcm14124149






