Comparison of Demographics and Oxford Knee Score in Total Knee Arthroplasty Patients Between the United Kingdom and Saudi Arabia: A Cohort Study
Abstract
1. Introduction
2. Materials and Methods
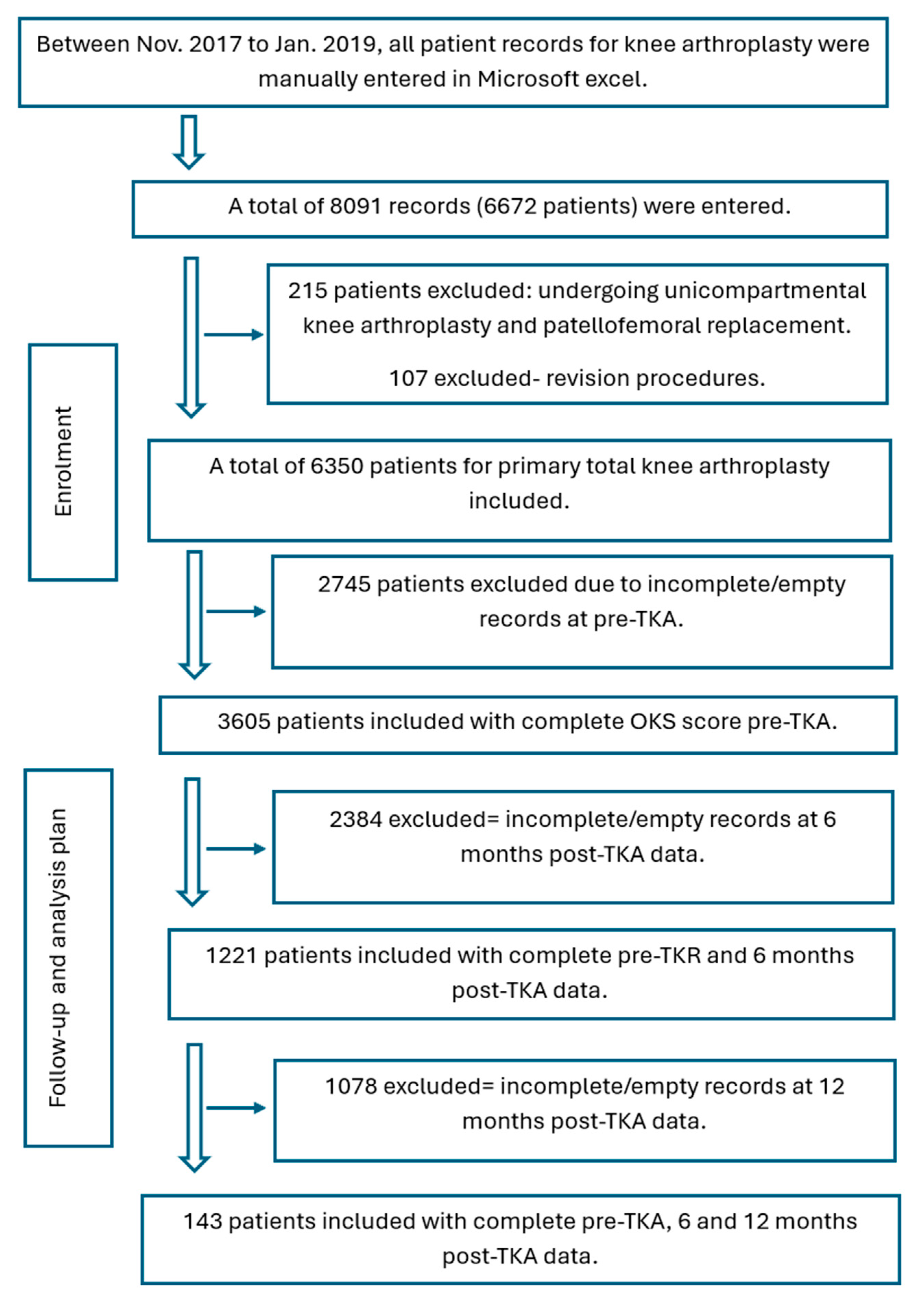
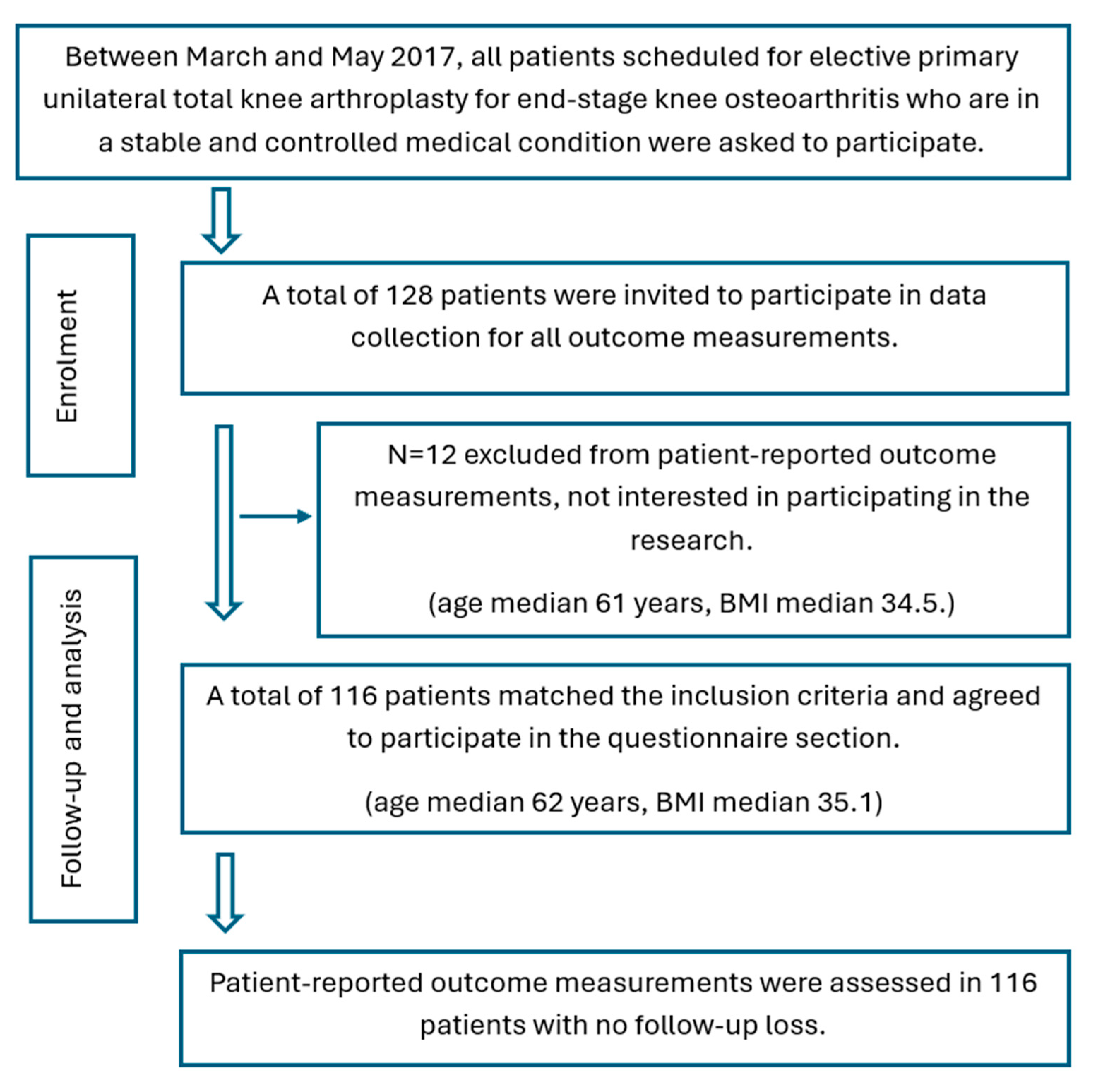
2.1. Study Design in the UK
2.2. Study Design in KSA
2.3. Sample-Size Estimation
2.4. Surgical Management and Physical Rehabilitation
2.5. Data Processing
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Al-Otaibi, M.L. Predictive Factors in Selecting Patients with Knee Osteoarthritis for Knee Replacement: A Single Center Experience. Bahrain Med. Bull. 2021, 43, 682–688. [Google Scholar]
- Affatato, S. The History of Total Knee Arthroplasty (TKA). In Surgical Techniques in Total Knee Arthroplasty and Alternative Procedures; Elsevier: Amsterdam, The Netherlands, 2015; pp. 3–16. [Google Scholar]
- Evans, J.T.; Walker, R.W.; Evans, J.P.; Blom, A.W.; Sayers, A.; Whitehouse, M.R. How Long Does a Knee Replacement Last? A Systematic Review and Meta-Analysis of Case Series and National Registry Reports with More than 15 Years of Follow-Up. Lancet 2019, 393, 655–663. [Google Scholar] [CrossRef] [PubMed]
- Price, A.J.; Alvand, A.; Troelsen, A.; Katz, J.N.; Hooper, G.; Gray, A.; Carr, A.; Beard, D. Knee Replacement. Lancet 2018, 392, 1672–1682. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, S.M.; Lau, E.; Ong, K.; Zhao, K.; Kelly, M.; Bozic, K.J. Future Young Patient Demand for Primary and Revision Joint Replacement: National Projections from 2010 to 2030. Clin. Orthop. Relat. Res. 2009, 467, 2606–2612. [Google Scholar] [CrossRef]
- Moran, C.G.; Horton, T.C. Total Knee Replacement: The Joint of the Decade. Br. Med. J. 2000, 320, 820. [Google Scholar] [CrossRef]
- Stephens, G.; Maarabouni, A.; Mansell, G.; Littlewood, C. Pre-Habilitation for Patients Awaiting Total Knee Replacement in the United Kingdom National Health Service: A Review of Publicly Facing Information. Physiother. Pract. Res. 2021, 42, 137–143. [Google Scholar] [CrossRef]
- Mehta, A. Operation Theater Setup for Joint Replacement Surgery. In A Practical Operative Guide for Total Knee and Hip Replacement; McGraw-Hill: New York, NY, USA, 2015; p. 14. [Google Scholar]
- Bin Sheeha, B.; Williams, A.; Johnson, D.; Bin Nasser, A.; Granat, M.; Jones, R. A Validation Study of the Arabic Version of the Oxford Knee Score for Use in End Stage Knee Osteoarthritis. Osteoarthr. Cartil. 2018, 26, S261. [Google Scholar] [CrossRef]
- Bin Sheeha, B.; Williams, A.; Johnson, D.S.; Granat, M.; Bin Nasser, A.; Jones, R. Responsiveness, Reliability, and Validity of Arabic Version of Oxford Knee Score for Total Knee Arthroplasty. J. Bone Jt. Surg. Am. 2020, 102, e89. [Google Scholar] [CrossRef]
- Collins, N.J.; Misra, D.; Felson, D.T.; Crossley, K.M.; Roos, E.M. Measures of Knee Function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee O. Arthritis Care Res. 2011, 63 (Suppl. S1), S208–S228. [Google Scholar] [CrossRef]
- Kim, G.-W. Patient-Reported Outcome Measure of Knee Function: Knee Injury and Osteoarthritis Outcome Score (KOOS). Ann. Rehabil. Med. 2023, 47, 441–443. [Google Scholar] [CrossRef] [PubMed]
- Scott, C.E.H.; Howie, C.R.; MacDonald, D.; Biant, L.C. Predicting Dissatisfaction Following Total Knee Replacement. J. Bone Jt. Surg. Br. Vol. 2010, 92-B, 1253–1258. [Google Scholar] [CrossRef] [PubMed]
- Saleh, A.; Nam, D. Patient-Reported Outcomes in Total Knee Arthroplasty. In Essentials in Total Knee Arthroplasty; SLACK Incorporated: West Deptford, NJ, USA, 2022; pp. 123–133. [Google Scholar]
- Sauder, N.; Galea, V.P.; Rojanasopondist, P.; Colon Iban, Y.E.; Florissi, I.S.; Nielsen, C.S.; Kappel, A.; Bragdon, C.R.; Malchau, H.; Troelsen, A. Regional Differences between the US, Scandinavia, and South Korea in Patient Demographics and Patient-Reported Outcomes for Primary Total Knee Arthroplasty. Arch. Orthop. Trauma Surg. 2019, 140, 93–108. [Google Scholar] [CrossRef] [PubMed]
- Yelton, M.J.; Jildeh, T.R. Cultural Competence and the Postoperative Experience: Pain Control and Rehabilitation. Arthrosc. Sport. Med. Rehabil. 2023, 5, 100733. [Google Scholar] [CrossRef] [PubMed]
- Bayliss, L.E.; Culliford, D.; Monk, A.P.; Glyn-Jones, S.; Prieto-Alhambra, D.; Judge, A.; Cooper, C.; Carr, A.J.; Arden, N.K.; Beard, D.J.; et al. The Effect of Patient Age at Intervention on Risk of Implant Revision after Total Replacement of the Hip or Knee: A Population-Based Cohort Study. Lancet 2017, 389, 1424–1430. [Google Scholar] [CrossRef]
- Al-Otaibi, M.L.; Alshumrani, G.A. Western-Designed Total Knee Implants Mismatch Saudi Patient Knees: Anatomical Bony Measurements Documented by Computed Tomography. Saudi Med. J. 2020, 41, 1227–1233. [Google Scholar] [CrossRef]
- AlTahan, H.; AlTurki, A.; AlTawayjri, I.; Khan, A.; AlMalki, M. Glycosylated Hemoglobin Level Changes Following Total Knee Arthroplasty in Type II Diabetic Patients: A Retrospective Cohort Study. J. Musculoskelet. Surg. Res. 2018, 2, 57. [Google Scholar] [CrossRef]
- Beard, D.J.; Harris, K.; Dawson, J.; Doll, H.; Murray, D.W.; Carr, A.J.; Price, A.J. Meaningful Changes for the Oxford Hip and Knee Scores after Joint Replacement Surgery. J. Clin. Epidemiol. 2015, 68, 73–79. [Google Scholar] [CrossRef]
- Saeed, N.; Pervaiz, M.K.; Shahbaz, M.Q. Determination of Sample Size. Eur. J. Sci. Res. 2006, 14, 319–325. [Google Scholar] [CrossRef]
- Baek, J.-H.; Lee, S.C.; Choi, K.; Ahn, H.S.; Nam, C.H. Long-Term Survivorship of Total Knee Arthroplasty with a Single-Radius, High-Flexion Posterior Stabilized Prosthesis. Knee 2021, 30, 275–282. [Google Scholar] [CrossRef]
- Field, A.P. Discovering Statistics Using SPSS, 3rd ed.; SAGE Publications: London, UK, 2009; ISBN 9781847879073. [Google Scholar]
- Joshi, P.S.; Pachore, J.A. The Impact of Morbid Obesity on Patient Outcomes after Total Knee Replacement Arthroplasty: A Matched Prospective Study. Int. J. Sci. Res. Publ. 2014, 4, 795–800. [Google Scholar]
- Cooper, Z.N.; McGuire, A.; Jones, S.; Le Grand, J. Equity, Waiting Times, and NHS Reforms: Retrospective Study. BMJ 2009, 339, b3264. [Google Scholar] [CrossRef] [PubMed]
- Jabbal, M.; Burt, J.; Clarke, J.; Moran, M.; Walmsley, P.; Jenkins, P.J. Trends in Incidence and Average Waiting Time for Arthroplasty from 1998-2021: An Observational Study of 282,367 Patients from the Scottish Arthroplasty Project. Ann. R. Coll. Surg. Engl. 2024, 106, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Ayers, D.C.; Yousef, M.; Yang, W.; Zheng, H. Age-Related Differences in Pain, Function, and Quality of Life Following Primary Total Knee Arthroplasty: Results From a FORCE-TJR (Function and Outcomes Research for Comparative Effectiveness in Total Joint Replacement) Cohort. J. Arthroplast. 2023, 38, S169–S176. [Google Scholar] [CrossRef] [PubMed]
- McCalden, R.W.; Robert, C.E.; Howard, J.L.; Naudie, D.D.; McAuley, J.P.; MacDonald, S.J. Comparison of Outcomes and Survivorship between Patients of Different Age Groups Following TKA. J. Arthroplast. 2013, 28, 83–86. [Google Scholar] [CrossRef]
- Han, H.-S.; Kim, J.S.; Lee, B.; Won, S.; Lee, M.C. A High Degree of Knee Flexion after TKA Promotes the Ability to Perform High-Flexion Activities and Patient Satisfaction in Asian Population. BMC Musculoskelet. Disord. 2021, 22, 565. [Google Scholar] [CrossRef]
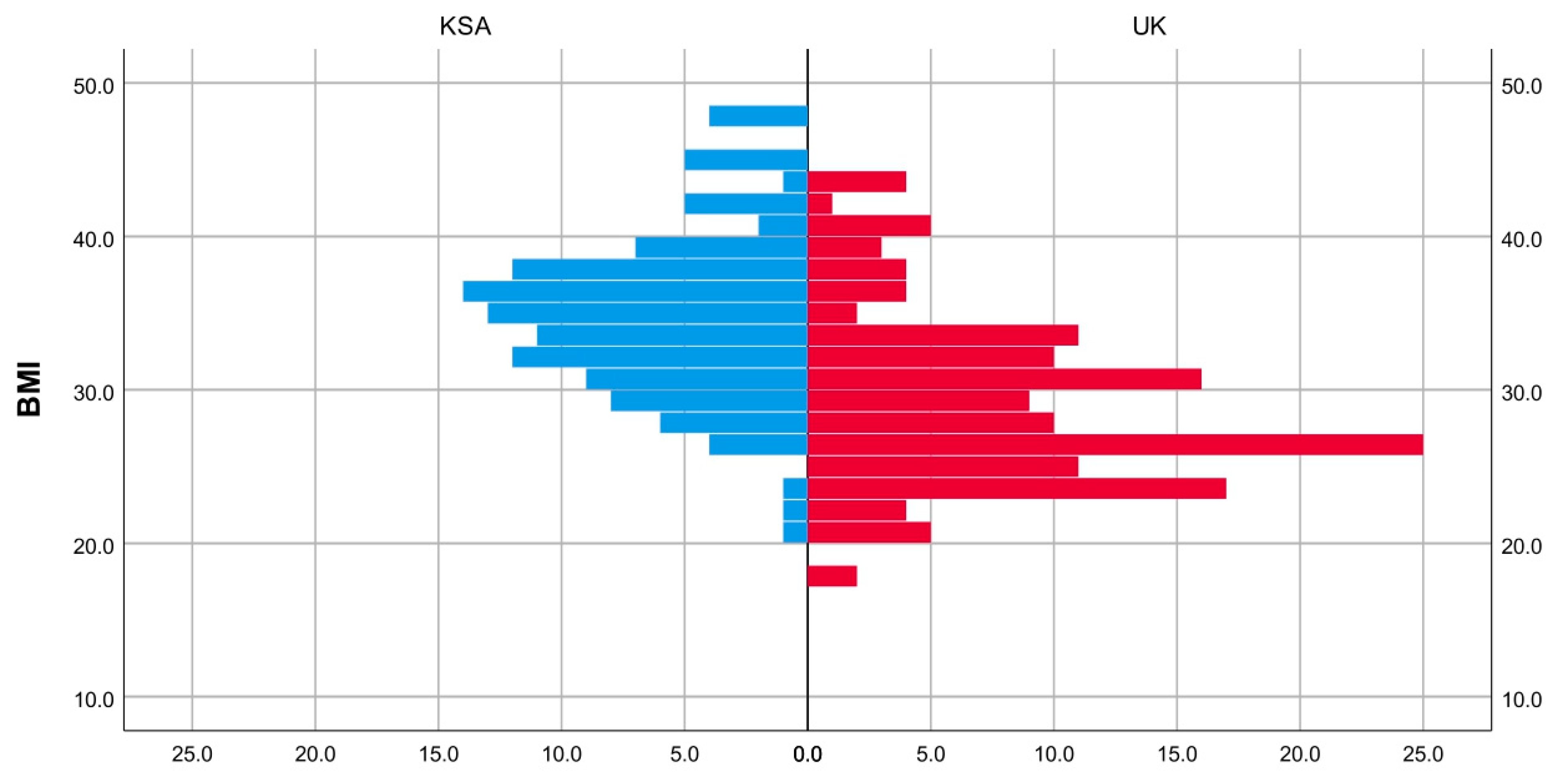
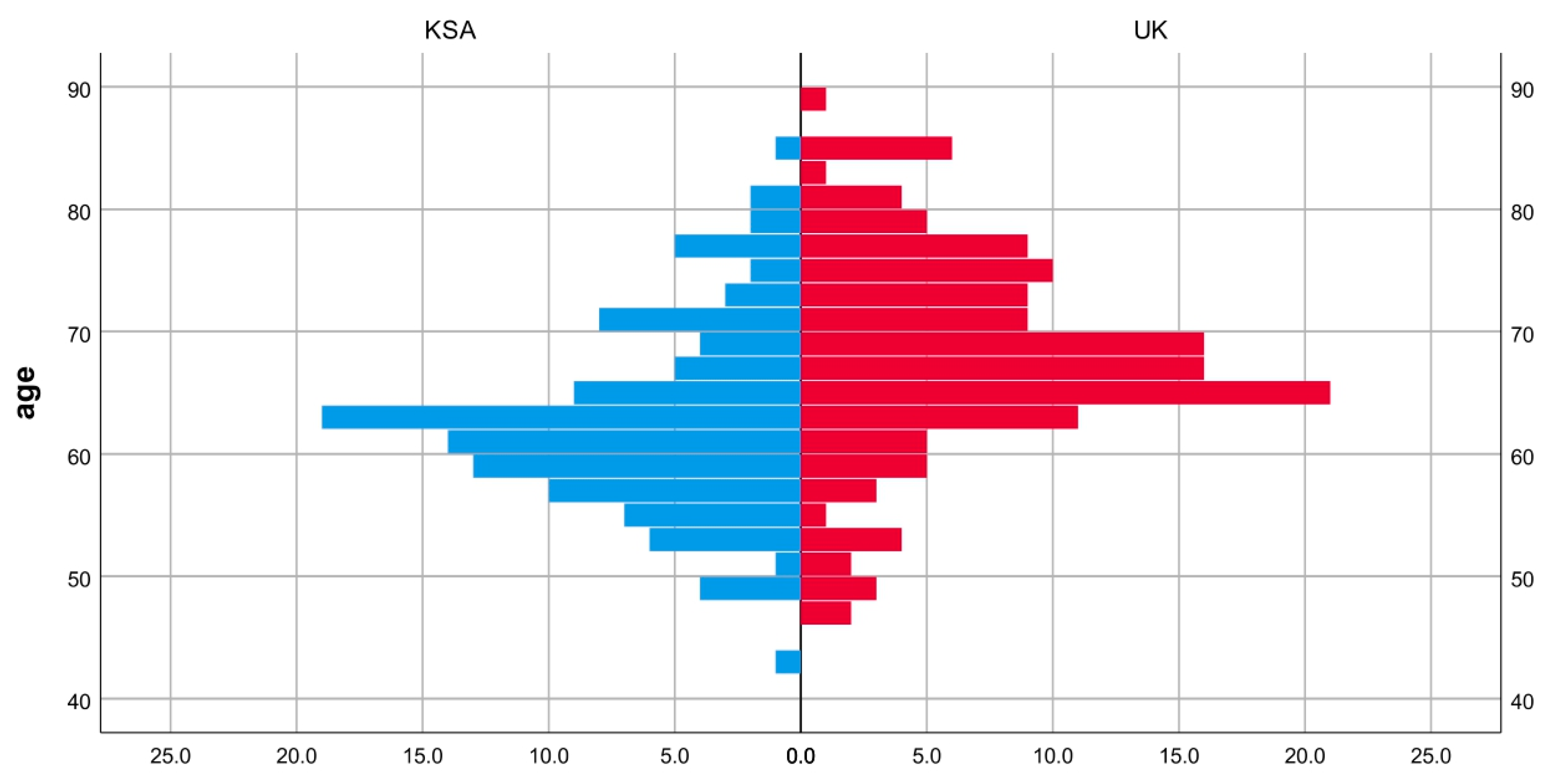
| Variable | Cohort | Median | Interquartile Range | Maximum–Minimum | Mann–Whitney U Test | |
|---|---|---|---|---|---|---|
| Standardized Test Statistic Z | p-Value | |||||
| Age | UK Cohort | 67 | 11 | 88–47 | 5.39 | <0.01 |
| KSA Cohort | 62 | 10 | 85–43 | |||
| Body mass index (BMI) | UK Cohort | 28 | 7 | 44–18 | 7.56 | <0.01 |
| KSA Cohort | 35.1 | 6.6 | 48.5–20.6 | |||
| Variable | Male | Female | Total | Chi-Square Test p-Value | |
|---|---|---|---|---|---|
| UK Cohort | Count | 53 | 90 | 143 | <0.01 |
| Expected count | 40.3 | 102.7 | 143 | ||
| % within group | 37.1% | 62.9% | 100% | ||
| KSA Cohort | Count | 20 | 96 | 116 | |
| Expected count | 32.7 | 83.3 | 116 | ||
| % within group | 17.2% | 82.8% | 100% | ||
| Total | Count | 73 | 186 | 259 | |
| Expected count | 73 | 186 | 259 | ||
| % within group | 28.2% | 71.8% | 100% | ||
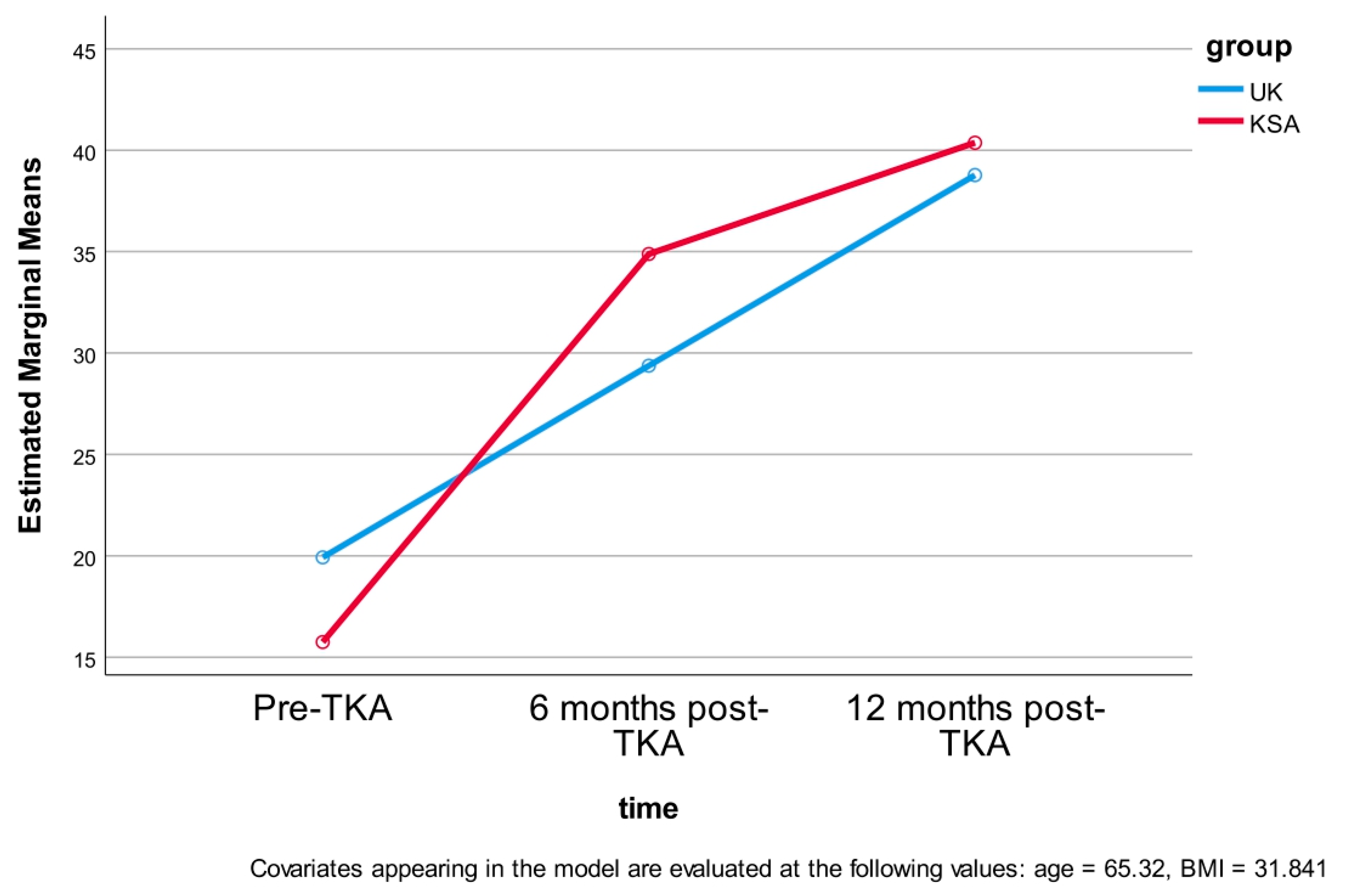
| Cohort | Time | Mean (SD) | Lower and Upper 95% Confidence Interval |
|---|---|---|---|
| Lower Bound–Upper Bound | |||
| UK Cohort | Pre-surgery | 19.4 (6.8) | 18.16–20.65 |
| 6 months post-surgery | 28.9 (4.9) | 28.03–29.92 | |
| 12 months post-surgery | 38.4 (3.6) | 37.68–39.07 | |
| KSA Cohort | Pre-surgery | 15.2 (4.6) | 14.33–16.03 |
| 6 months post-surgery | 34.7 (3.5) | 33.9 2–35.21 | |
| 12 months post-surgery | 40.2 (1.6) | 39.94–40.52 |
| OKS Score Within Subjects’ Effect | Degree of Freedom | Mean Square | F | p-Value | Partial Eta Squared | |
|---|---|---|---|---|---|---|
| Time | Sphericity assumed | 2 | 159.98 | 12.23 | <0.01 | 0.046 |
| Greenhouse–Geisser | 1.29 | 246.34 | 12.23 | <0.01 | 0.046 | |
| time * age | Sphericity assumed | 2 | 8.68 | 0.66 | 0.52 | 0.003 |
| Greenhouse–Geisser | 1.29 | 13.37 | 0.66 | 0.45 | 0.003 | |
| time * BMI | Sphericity assumed | 2 | 21.85 | 1.67 | 0.19 | 0.007 |
| Greenhouse–Geisser | 1.29 | 33.65 | 1.67 | 0.20 | 0.007 | |
| time * group | Sphericity assumed | 2 | 947.03 | 72.40 | <0.01 | 0.222 |
| Greenhouse–Geisser | 1.29 | 1458.23 | 72.40 | <0.01 | 0.222 | |
| time * Gender | Sphericity assumed | 2 | 20.43 | 1.56 | 0.21 | 0.006 |
| Greenhouse–Geisser | 1.29 | 31.45 | 1.56 | 0.22 | 0.006 | |
| time * group * Gender | Sphericity assumed | 2 | 7.45 | 0.57 | 0.57 | 0.002 |
| Greenhouse–Geisser | 1.29 | 11.48 | 0.57 | 0.49 | 0.002 | |
| Error (time) | Sphericity assumed | 506 | 13.08 | |||
| Greenhouse–Geisser | 328.62 | 20.14 | ||||
| Time Point | Mean Difference | Standard Error | p-Value | Lower and Upper 95% Confidence Interval |
|---|---|---|---|---|
| Pre-surgery | 4.23 | 0.77 | <0.01 | 2.70–5.76 |
| 6 months post-surgery | −5.60 | 0.57 | <0.01 | −6.73–−4.46 |
| 12 months post-surgery | −1.85 | 0.36 | =0.063 | −2.56–−1.15 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Althomali, O.W.; Bin sheeha, B.; Johnson, D.S.; Ibrahim, Z.M.; Altoury, S.A.; Jones, R. Comparison of Demographics and Oxford Knee Score in Total Knee Arthroplasty Patients Between the United Kingdom and Saudi Arabia: A Cohort Study. J. Clin. Med. 2025, 14, 4148. https://doi.org/10.3390/jcm14124148
Althomali OW, Bin sheeha B, Johnson DS, Ibrahim ZM, Altoury SA, Jones R. Comparison of Demographics and Oxford Knee Score in Total Knee Arthroplasty Patients Between the United Kingdom and Saudi Arabia: A Cohort Study. Journal of Clinical Medicine. 2025; 14(12):4148. https://doi.org/10.3390/jcm14124148
Chicago/Turabian StyleAlthomali, Omar W., Bodor Bin sheeha, David Sands Johnson, Zizi M. Ibrahim, Shaimaa Abdelhamid Altoury, and Richard Jones. 2025. "Comparison of Demographics and Oxford Knee Score in Total Knee Arthroplasty Patients Between the United Kingdom and Saudi Arabia: A Cohort Study" Journal of Clinical Medicine 14, no. 12: 4148. https://doi.org/10.3390/jcm14124148
APA StyleAlthomali, O. W., Bin sheeha, B., Johnson, D. S., Ibrahim, Z. M., Altoury, S. A., & Jones, R. (2025). Comparison of Demographics and Oxford Knee Score in Total Knee Arthroplasty Patients Between the United Kingdom and Saudi Arabia: A Cohort Study. Journal of Clinical Medicine, 14(12), 4148. https://doi.org/10.3390/jcm14124148






