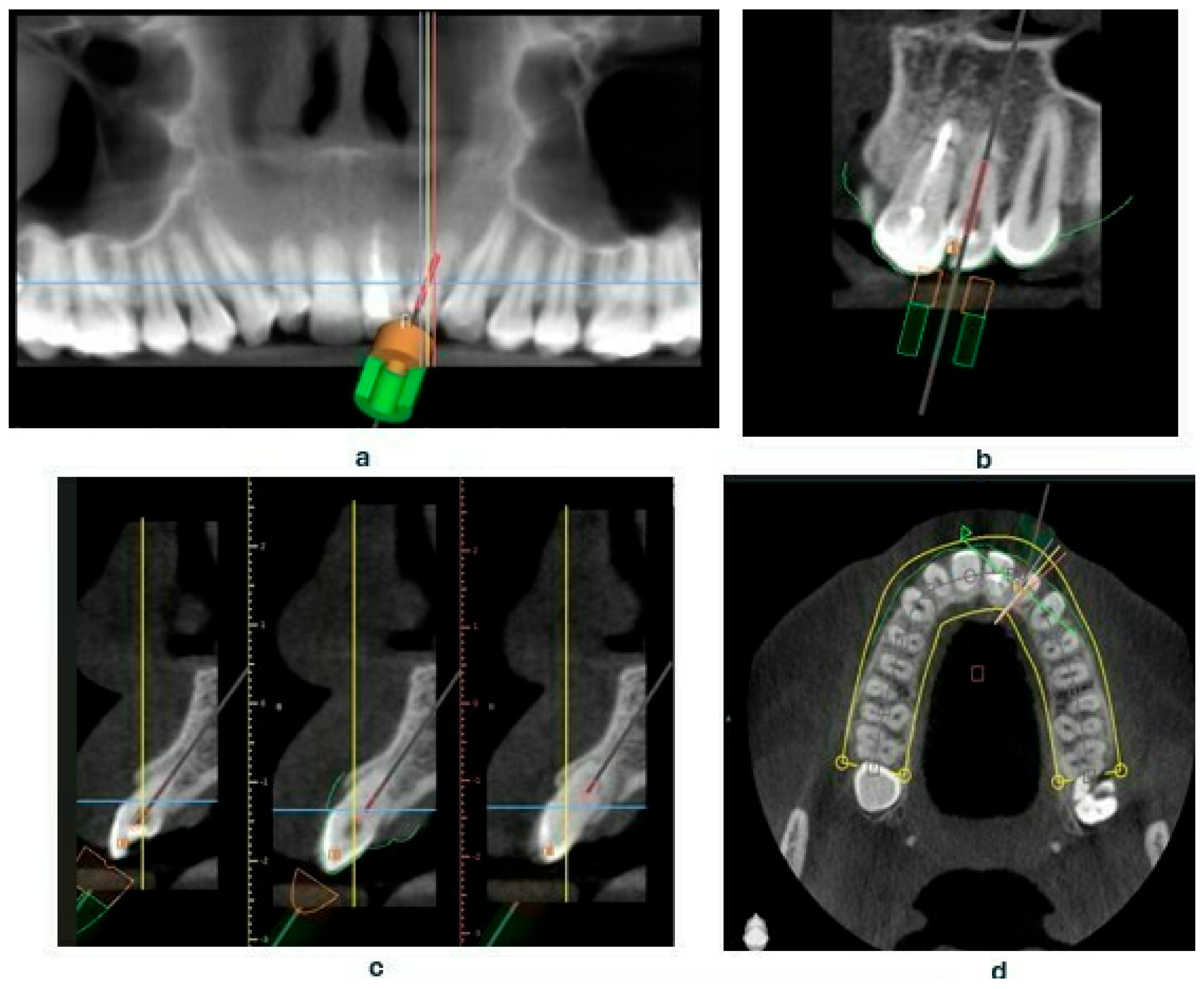
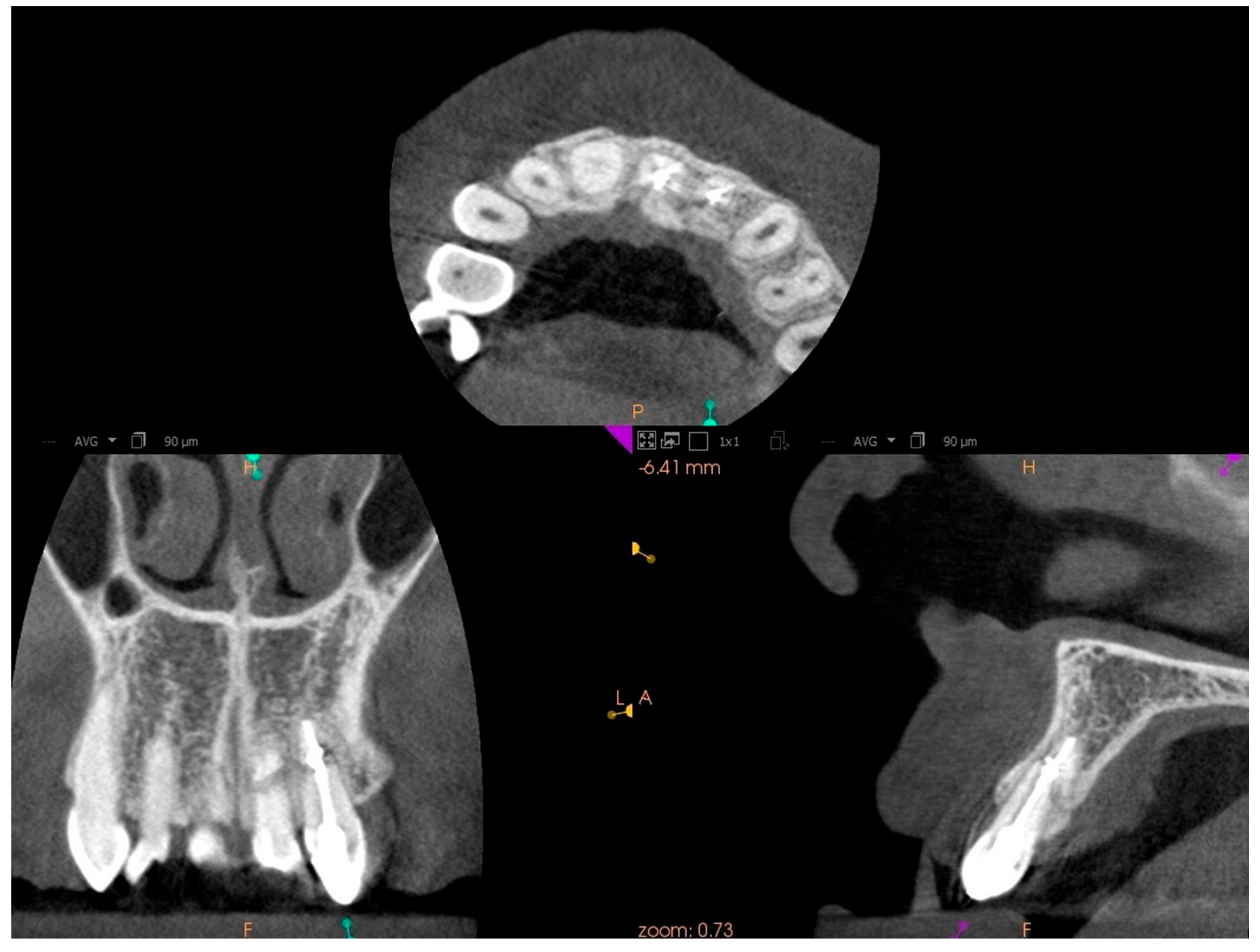
Guided Endodontics for a Tooth with Root Fracture: A Case Report
Abstract
1. Introduction
2. Materials and Methods
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CBCT | Cone-Beam Computed Tomography |
| PCO | Pulp Canal Obliteration |
| Il-1 | Interleukin-1 |
| Il-6 | Interleukin-6 |
| TGF-β | Transforming grow factor-beta |
| TNF-α | Tumor necrosis factor-alpha |
| FGF | Fibroblast growth factor |
| FDI | Federal Dentaire Internationale |
| RVG | Radiovisiography |
| STL | Standard tessellation language |
| CWO | Continous Wave Obturation |
| PUI | Passive Ultrasonic Irrigation |
References
- Duong, H.Y.; Roccuzzo, A.; Stähli, A.; Salvi, G.E.; Lang, N.P.; Sculean, A. Oral Health-Related Quality of Life of Patients Rehabilitated with Fixed and Removable Implant-Supported Dental Prostheses. Periodontol. 2000 2022, 88, 201–237. [Google Scholar] [CrossRef]
- Lekaviciute, R.; Kriauciunas, A. Relationship Between Occlusal Factors and Temporomandibular Disorders: A Systematic Literature Review. Cureus 2024, 16, e54130. [Google Scholar] [CrossRef] [PubMed]
- Vinagre, A.; Castanheira, C.; Messias, A.; Palma, P.J.; Ramos, J.C. Management of Pulp Canal Obliteration-Systematic Review of Case Reports. Medicina 2021, 57, 1237. [Google Scholar] [CrossRef]
- Amir, F.A.; Gutmann, J.L.; Witherspoon, D.E. Calcific Metamorphosis: A Challenge in Endodontic Diagnosis and Treatment. Quintessence Int. 2001, 32, 447–455. [Google Scholar] [PubMed]
- Lübbers, H.T.; Bornstein, M.M.; Dagassan-Berndt, D.; Filippi, A.; Suter, V.G.A.; Dula, K. Revised Consensus Guidelines for the Use of Cone-Beam Computed Tomography/Digital Volume Tomography. Swiss Dent. J. 2024, 134, 86–115. [Google Scholar] [CrossRef]
- Zoltowska, A.; Machut, K.; Pawlowska, E.; Derwich, M. Plasma Rich in Growth Factors in the Treatment of Endodontic Periapical Lesions in Adult Patients: A Narrative Review. Pharmaceuticals 2021, 14, 1041. [Google Scholar] [CrossRef]
- Machut, K.; Żółtowska, A. Plasma Rich in Growth Factors in the Treatment of Endodontic Periapical Lesions in Adult Patients: 3-Dimensional Analysis Using Cone-Beam Computed Tomography on the Outcomes of Non-Surgical Endodontic Treatment Using A-PRF+ and Calcium Hydroxide: A Retrospective Cohort Study. J. Clin. Med. 2022, 11, 6092. [Google Scholar] [PubMed]
- Lewis, N.V.; Aggarwal, S. Static Guided Endodontic Approach for Pulp Canal Obliteration: A Case Report. Cureus 2023, 15, e42379. [Google Scholar] [CrossRef]
- Holcomb, J.; Gregory, W. Calcific Metamorphosis of the Pulp: Its Incidence and Treatment. Oral Surg. Oral Med. Oral Pathol. 1967, 24, 825–830. [Google Scholar] [CrossRef]
- Jacobsen, I.; Kerekes, K. Long Term Prognosis of Traumatized Permanent Anterior Teeth Showing Calcifying Processes in the Pulp Cavity. Scand. J. Dent. Res. 1977, 85, 588–598. [Google Scholar] [CrossRef]
- Dąbrowski, W.; Puchalska, W.; Ziemlewski, A.; Ordyniec-Kwaśnica, I. Guided Endodontics as a Personalized Tool for Complicated Clinical Cases. Int. J. Environ. Res. Public Health 2022, 19, 9958. [Google Scholar] [CrossRef]
- Patel, S.; Dawood, A. Cone Beam Computed Tomography in Endodontics: A Review. Ocean. J. Dent. Sci. 2011, 1, 37–47. [Google Scholar]
- McCabe, P.S.; Dummer, P.M. Pulp Canal Obliteration: An Endodontic Diagnosis and Treatment Challenge. Int. Endod. J. 2012, 45, 177–197. [Google Scholar] [CrossRef] [PubMed]
- Toureno, L.; Park, J.H.; Cederberg, R.A.; Hwang, E.H.; Shin, J.W. Identification of Supernumerary Teeth in 2D and 3D: Review of Literature and a Proposal. J. Dent. Educ. 2013, 77, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Aminoshariae, A.; Mackey, S.A.; Palomo, L.; Kulild, J.C. Declassifying Mobility Classification. J. Endod. 2020, 46, 1539–1544. [Google Scholar] [CrossRef]
- Ellis, G.E.; Davey, K.W. The Classification and Treatment of Injuries to the Teeth of Children; Year Book Medical Publishers Publisher: Chicago, IL, USA, 1970. [Google Scholar]
- Reddy, M.S.; Mayfield-Donahoo, T.; Vanderven, F.J.; Jeffcoat, M.K. A Comparison of the Diagnostic Advantages of Panoramic Radiography and Computed Tomography Scanning for Placement of Root Form Dental Implants. Clin. Oral Implants Res. 1994, 5, 229–238. [Google Scholar] [CrossRef]
- Krastl, G.; Zehnder, M.S.; Connert, T.; Weiger, R.; Kühl, S. Guided Endodontics: A Novel Treatment Approach for Teeth with Pulp Canal Calcification and Apical Pathology. Dent. Traumatol. 2016, 32, 240–246. [Google Scholar] [CrossRef]
- Keßler, A.; Dosch, M.; Reymus, M.; Folwaczny, M. Influence of 3D-Printing Method, Resin Material, and Sterilization on the Accuracy of Virtually Designed Surgical Implant Guides. J. Prosthet. Dent. 2022, 128, 196–204. [Google Scholar] [CrossRef]
- Buchgreitz, J.; Buchgreitz, M.; Bjørndal, L. Guided Root Canal Preparation Using Cone Beam Computed Tomography and Optical Surface Scans—An Observational Study of Pulp Space Obliteration and Drill Path Depth in 50 Patients. Int. Endod. J. 2019, 52, 559–568. [Google Scholar] [CrossRef]
- VanDerMeer, W.J.; Vissink, A.; Ng, Y.L.; Gulabivala, K. 3D Computer-Aided Treatment Planning in Endodontics. J. Dent. 2016, 45, 67–72. [Google Scholar] [CrossRef]
- Dodds, R.; Holcomb, J.; McVicker, D. Endodontic Management of Teeth with Calcific Metamorphosis. Compend. Contin. Educ. Dent. 1985, 6, 515–520. [Google Scholar] [PubMed]
- Maia, L.M.; Machado, V.D.C.; Da Silva, N.R.F.A.; Brito-Júnior, M.; Silveira, R.; Júnior, G.M.; Sobrinho, A.P.R. Case Reports in Maxillary Posterior Teeth by Guided Endodontic Access. J. Endod. 2019, 45, 214–218. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.; Shi, W.; Wu, J.; Wu, Y.; Liu, W.; Zhu, Q. The Clinical Treatment of Complicated Root Canal Therapy with the Aid of a Dental Operating Microscope. Int. Dent. J. 2011, 61, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Rabié, C.; Torres, A.; Lambrechts, P.; Jacobs, R. Clinical Applications, Accuracy, and Limitations of Guided Endodontics: A Systematic Review. Int. Endod. J. 2020, 53, 214–223. [Google Scholar] [CrossRef]





| CBCT scan and digital impression |
|
| Design and print endodontic guide |
|
| To access the canal |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuczmaja, M.; Żółtowska, A. Guided Endodontics for a Tooth with Root Fracture: A Case Report. J. Clin. Med. 2025, 14, 4079. https://doi.org/10.3390/jcm14124079
Kuczmaja M, Żółtowska A. Guided Endodontics for a Tooth with Root Fracture: A Case Report. Journal of Clinical Medicine. 2025; 14(12):4079. https://doi.org/10.3390/jcm14124079
Chicago/Turabian StyleKuczmaja, Monika, and Agata Żółtowska. 2025. "Guided Endodontics for a Tooth with Root Fracture: A Case Report" Journal of Clinical Medicine 14, no. 12: 4079. https://doi.org/10.3390/jcm14124079
APA StyleKuczmaja, M., & Żółtowska, A. (2025). Guided Endodontics for a Tooth with Root Fracture: A Case Report. Journal of Clinical Medicine, 14(12), 4079. https://doi.org/10.3390/jcm14124079







