Variability in Inferior Vena Cava (IVC) Filter Retrieval Rates and Adherence to Guidelines: A Multi-Center Retrospective Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Source
2.2. Inclusion and Exclusion
2.3. Study Outcomes
2.4. Statistical Analysis
2.5. Declaration of Generative AI
3. Results
3.1. Retrieval Rate and Timing
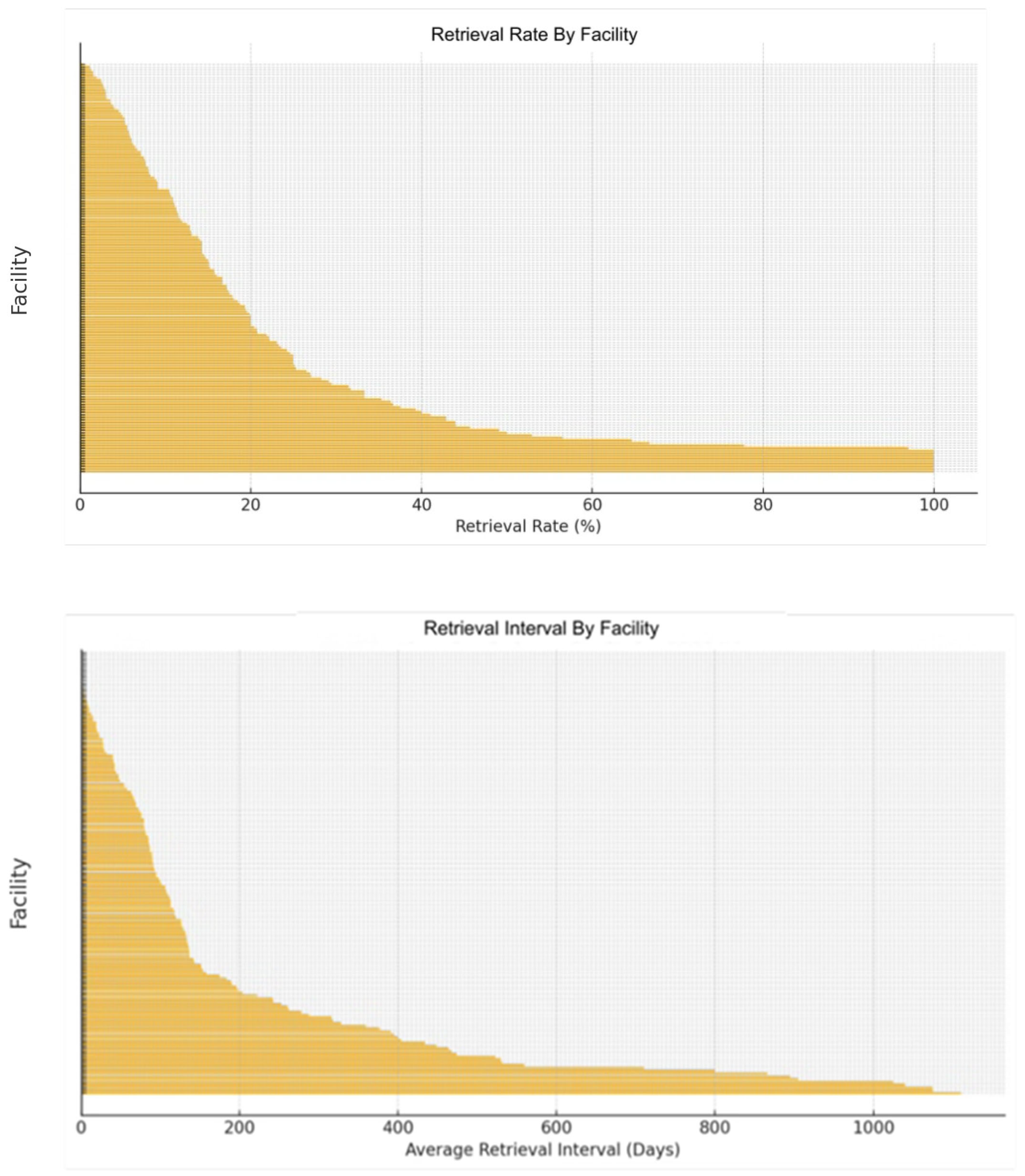
3.2. Facility Comparisons
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| IVC | Inferior vena cava filter |
| DVT | Deep vein thrombosis |
| PE | Pulmonary embolism |
References
- Angel, L.F.; Tapson, V.; Galgon, R.E.; Restrepo, M.I.; Kaufman, J. Systematic review of the use of retrievable inferior vena cava filters. J. Vasc. Interv. Radiol. 2011, 22, 1522–1530. [Google Scholar] [CrossRef] [PubMed]
- U.S. Food and Drug Administration (FDA). Removing Retrievable Inferior Vena Cava Filters: FDA Safety Communication. 2024. Available online: https://www.fda.gov/ (accessed on 25 April 2025).
- Kaufman, J.A.; Barnes, G.D.; Chaer, R.A.; Cuschieri, J.; Eberhardt, R.T.; Johnson, M.S.; Kuo, W.T.; Murin, S.; Patel, S.; Rajasekhar, A.; et al. Society of Interventional Radiology Clinical Practice Guideline for Inferior Vena Cava Filters. J. Vasc. Interv. Radiol. 2020, 31, 1529–1544. [Google Scholar] [CrossRef] [PubMed]
- Kearon, C.; Akl, E.A.; Ornelas, J.; Blaivas, A.; Jimenez, D.; Bounameaux, H.; Huisman, M.; King, C.S.; Morris, T.A.; Sood, N.; et al. Antithrombotic Therapy for VTE Disease: CHEST Guideline and Expert Panel Report. Chest 2016, 149, 315–352. [Google Scholar] [CrossRef] [PubMed]
- Sutphin, P.D.; Reis, S.P.; McKune, A.; Ravanzo, M.; Kalva, S.P.; Pillai, A.K. Improving inferior vena cava filter retrieval rates with the define, measure, analyze, improve, control methodology. J. Vasc. Interv. Radiol. 2015, 26, 491–498.e1. [Google Scholar] [CrossRef] [PubMed]
- Sarosiek, S.; Crowther, M.; Sloan, J.M. Indications, complications, and management of inferior vena cava filters: The experience at an academic medical center. Am. J. Med. 2013, 126, 513–517. [Google Scholar] [CrossRef]
- Geisbüsch, P.; Benenati, J.F.; Peña, C.S.; Couvillon, J.; Powell, A.; Gandhi, R.; Samuels, S.; Uthoff, H. Retrievable IVC filters: Factors that affect retrieval success. Cardiovasc. Intervent. Radiol. 2012, 35, 1059–1065. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, J.A.; Kinney, T.B.; Streiff, M.B.; Sing, R.F.; Proctor, M.C.; Becker, D.; Cippole, M.; Comerota, A.J.; Millward, S.F.; Rogers, F.B.; et al. Guidelines for the use of retrievable and permanent inferior vena cava filters: Report from the Society of Interventional Radiology multidisciplinary consensus conference. J. Vasc. Interv. Radiol. 2012, 23, 1493–1505. [Google Scholar] [CrossRef]
- Watson, J.D.B.; Morrison, J.J.; McNamee, I.L.; Evans, T.W.; Rasmussen, T.E. Impact of a dedicated inferior vena cava (IVC) filter clinic on IVC filter retrieval rates. J. Vasc. Surg. 2013, 57, 11S. [Google Scholar] [CrossRef][Green Version]
- Minocha, J.; Idakoji, I.; Riaz, A.; Karp, J.; Gupta, R.; Chrisman, H.B.; Salem, R.; Ryu, R.K.; Lewandowski, R.J. Improving inferior vena cava filter retrieval rates with the use of a dedicated inferior vena cava filter registry. J. Vasc. Interv. Radiol. 2010, 21, 1847–1851. [Google Scholar] [CrossRef] [PubMed]
- PREPIC Study Group. Eight-year follow-up of patients with permanent vena cava filters in the prevention of pulmonary embolism: The PREPIC (Prévention du Risque d’Embolie Pulmonaire par Interruption Cave) randomized study. Circulation 2005, 112, 416–422. [Google Scholar] [CrossRef] [PubMed]
- Caplin, D.M.; Nikolic, B.; Kalva, S.P.; Ganguli, S.; Saad, W.E.A.; Zuckerman, D.A.; Society of Interventional Radiology Standards of Practice Committee. Quality improvement guidelines for the performance of inferior vena cava filter placement for the prevention of pulmonary embolism. J. Vasc. Interv. Radiol. 2011, 22, 1509–1515. [Google Scholar] [CrossRef] [PubMed]
- Kuo, W.T.; Robertson, S.W.; Odegaard, J.I.; Hofmann, L.V. Complex retrieval of fractured, embedded, and penetrating inferior vena cava filters: Techniques for removal and clinical outcomes. J. Vasc. Interv. Radiol. 2013, 24, 717–723. [Google Scholar] [CrossRef] [PubMed]
- Mismetti, P.; Laporte, S.; Pellerin, O.; Ennezat, P.-Y.; Couturaud, F.; Elias, A.; Falvo, N.; Meneveau, N.; Quéré, I.; Roy, P.-M.; et al. Effect of a Retrievable Inferior Vena Cava Filter Plus Anticoagulation vs Anticoagulation Alone on Risk of Recurrent Pulmonary Embolism: The PREPIC2 Randomized Clinical Trial. JAMA 2015, 313, 1627–1635. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nuffer, Z.; Ramis, P.; Rohren, E.M.; Horn, G. Variability in Inferior Vena Cava (IVC) Filter Retrieval Rates and Adherence to Guidelines: A Multi-Center Retrospective Analysis. J. Clin. Med. 2025, 14, 4034. https://doi.org/10.3390/jcm14124034
Nuffer Z, Ramis P, Rohren EM, Horn G. Variability in Inferior Vena Cava (IVC) Filter Retrieval Rates and Adherence to Guidelines: A Multi-Center Retrospective Analysis. Journal of Clinical Medicine. 2025; 14(12):4034. https://doi.org/10.3390/jcm14124034
Chicago/Turabian StyleNuffer, Zachary, Phil Ramis, Eric M. Rohren, and Gary Horn. 2025. "Variability in Inferior Vena Cava (IVC) Filter Retrieval Rates and Adherence to Guidelines: A Multi-Center Retrospective Analysis" Journal of Clinical Medicine 14, no. 12: 4034. https://doi.org/10.3390/jcm14124034
APA StyleNuffer, Z., Ramis, P., Rohren, E. M., & Horn, G. (2025). Variability in Inferior Vena Cava (IVC) Filter Retrieval Rates and Adherence to Guidelines: A Multi-Center Retrospective Analysis. Journal of Clinical Medicine, 14(12), 4034. https://doi.org/10.3390/jcm14124034






