1. Introduction
Over the past two decades, the management of gynecologic cancers has been significantly influenced by the recognition of hereditary cancer syndromes and the role of preventive surgery. For women carrying mutations in high-risk genes such as BRCA1, BRCA2, or mismatch repair genes associated with Lynch syndrome, risk-reducing salpingo-oophorectomy (RRSO) and hysterectomy are established strategies endorsed by major guidelines [
1,
2,
3].
Traditionally performed via open or laparoscopic approaches, these procedures have evolved to offer improved safety and reduced morbidity. However, despite these advances, visible abdominal scars, postoperative pain, and longer recovery remain concerns, especially for younger, asymptomatic patients seeking preventive interventions [
4,
5].
Vaginal natural orifice transluminal endoscopic surgery (vNOTES) has recently emerged as an innovative, scarless surgical alternative that merges the benefits of laparoscopy with the minimal invasiveness of vaginal surgery [
6]. While initially adopted in benign gynecology, its use is expanding into oncologic prophylaxis [
7].
This narrative review explores the evolving role of vNOTES in risk-reducing gynecologic cancer surgery, with a focus on its application in hereditary cancer syndromes. We aim to synthesize current evidence, technical considerations, and implications for clinical practice.
2. Materials and Methods
This is a narrative review aimed at synthesizing current evidence on the use of vNOTES in the context of risk-reducing gynecologic cancer surgery, particularly for women with BRCA mutations or Lynch syndrome.
2.1. Search Strategy and Sources
We performed a structured literature search using the PubMed and Web of Science databases to identify relevant studies published from January 2000 to April 2025. The following search terms were used in various combinations: “vNOTES”, “vaginal natural orifice transluminal endoscopic surgery”, “risk-reducing surgery”, “salpingo-oophorectomy”, “hysterectomy”, “BRCA”, “Lynch syndrome”, and “hereditary gynecologic cancer”. Additional studies were identified by reviewing the reference lists of included articles.
2.2. Inclusion and Exclusion Criteria
We included studies that reported on the use of vNOTES in gynecologic surgery with specific relevance to risk-reducing or oncologic contexts, such as procedures performed in BRCA mutation carriers or women with Lynch syndrome. Eligible articles provided clinical outcome data, including complication rates, operative time, hospital stay, estimated blood loss, or patient-reported outcomes. Only original research articles—such as case reports, cohort studies, and clinical trials—published in English and indexed in PubMed or Web of Science were considered. Studies were excluded if they focused exclusively on benign indications without relevance to cancer prevention, lacked outcome data, were published only as conference abstracts or technical videos, or were not peer-reviewed.
2.3. Study Selection
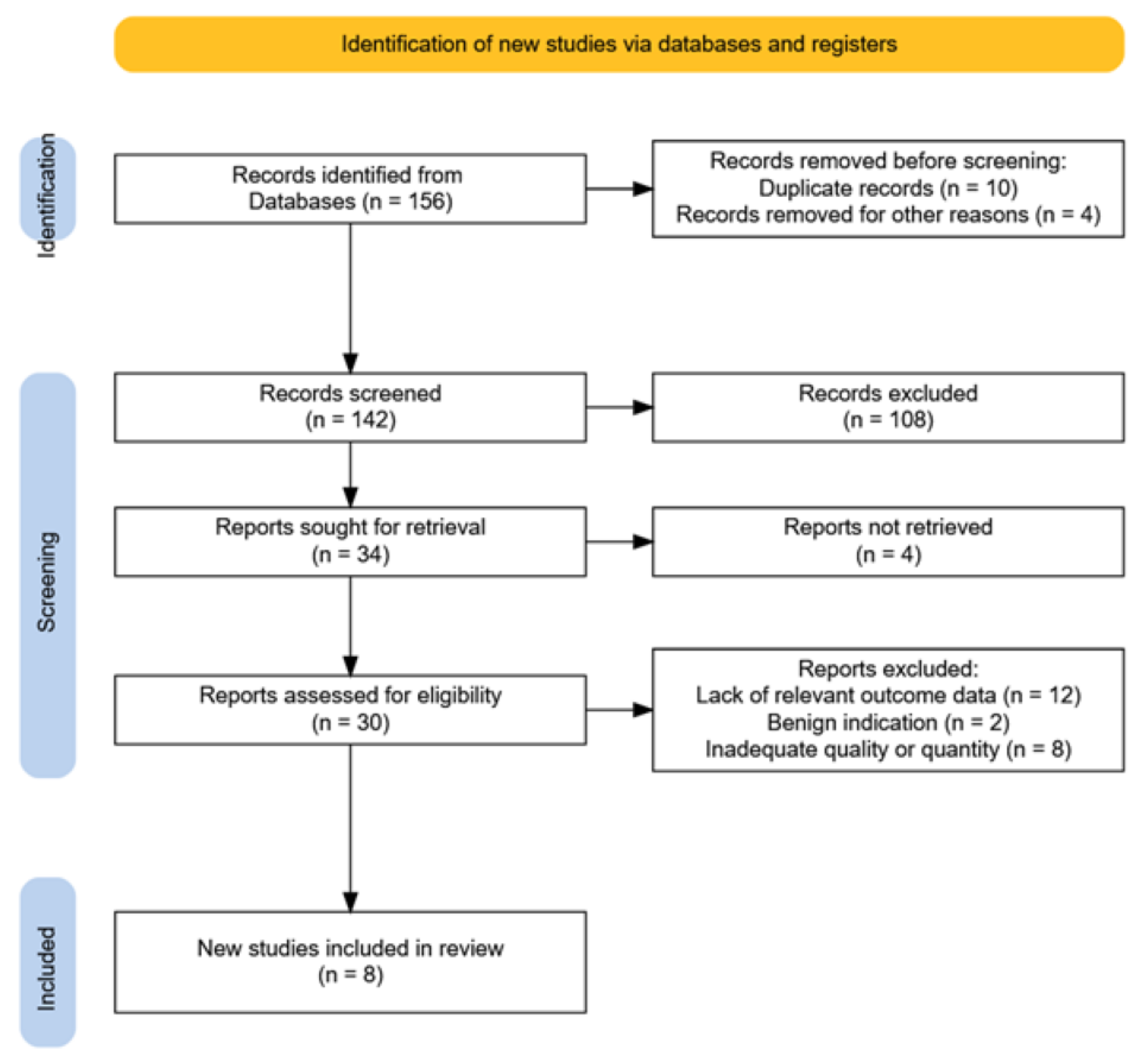
An initial total of 156 articles were identified. After removing duplicates and screening titles and abstracts, 30 full-text articles were assessed for eligibility. Of these, 16 articles met the preliminary inclusion criteria, and eight were ultimately included in the qualitative synthesis for their direct relevance to prophylactic gynecologic surgery using vNOTES (
Figure 1).
Although this review follows a narrative design, a basic quality assessment of the included studies was performed to enhance transparency. We applied a simplified version of the ROBINS-I tool (Risk Of Bias In Non-randomized Studies of Interventions), assessing each included study based on the following domains: selection bias, outcome reporting, comparability of groups, and completeness of follow-up. Most included studies were retrospective and small in scale, often with limited follow-up and without control groups, which introduces a moderate-to-high risk of bias. The absence of randomization and heterogeneity in surgical expertise across centers were further limiting factors. Future systematic reviews should incorporate formal tools such as ROBIS or full ROBINS-I to better quantify study quality and evidence strength. Such limitations will further be elaborated.
2.4. Data Extraction and Synthesis
From each eligible study, we extracted information regarding the type of surgical procedure (e.g., hysterectomy, salpingo-oophorectomy), patient population (including mutation status), operative metrics (e.g., blood loss, operative time), complications, hospital stay, and postoperative recovery.
Where available, comparative outcomes with conventional laparoscopy or vaginal hysterectomy were highlighted. Particular attention was given to studies involving BRCA mutation carriers and women with Lynch syndrome undergoing risk-reducing procedures. Sectioning and Extensively Examining the FIMbriated End (SEE-FIM) protocol adherence was tracked when reported.
2.5. Review Design
Given the emerging nature of this surgical approach and the limited number of randomized trials, a narrative (non-systematic) review format was chosen to allow for thematic synthesis of clinical, surgical, and technical outcomes. Given the narrative nature of this review, a formal risk-of-bias assessment tool (such as the Cochrane Risk of Bias tool or ROBINS-I for non-randomized studies) was not applied. While care was taken to include high-quality and peer-reviewed literature, this limitation should be acknowledged, and future systematic reviews may benefit from structured quality appraisal frameworks to more rigorously evaluate evidence strength.
3. Overview of Hereditary Gynecologic Cancer Syndromes
Hereditary gynecologic cancers account for a small but significant subset of malignancies affecting women, and for those who carry genetic mutations, the lifetime risk is dramatically elevated [
8]. The most well-characterized hereditary syndromes in this context are Hereditary Breast and Ovarian Cancer (HBOC) syndrome—typically involving
BRCA1 and
BRCA2 mutations—and Lynch syndrome, which arises from germline mutations in one of several mismatch repair (MMR) genes, including
MLH1,
MSH2,
MSH6, and
PMS2 [
9].
In women with BRCA1 or BRCA2 mutations, the lifetime risk of ovarian cancer ranges from approximately 10% to 50%, depending on the specific gene and family history [
10,
11,
12]. Importantly, the origin of these so-called “ovarian” cancers is now understood to lie, in many cases, within the fimbrial end of the fallopian tubes. This insight has redefined the anatomic targets of prophylactic intervention, with bilateral salpingo-oophorectomy (BSO) being the standard recommendation, usually between the ages of 35 and 45, and earlier if childbearing is complete [
13,
14]. These procedures not only significantly reduce the risk of high-grade serous carcinoma, but also confer a measurable reduction in breast cancer risk, particularly in premenopausal women [
14].
In contrast, Lynch syndrome confers a distinct pattern of cancer risk. Women with this condition face a 30–60% lifetime risk of endometrial cancer and a 10–20% risk of ovarian cancer, typically arising at a younger age than in sporadic cases [
15]. Unlike BRCA, where breast surveillance often substitutes for prophylactic mastectomy, the risk of endometrial cancer in Lynch syndrome is best mitigated through surgical removal of the uterus and adnexa [
16,
17]. Guidelines from major societies such as NCCN and ESGO recommend considering prophylactic hysterectomy with BSO by the end of childbearing, especially if the patient is undergoing abdominal or pelvic surgery for another indication [
18,
19].
It is precisely within this delicate clinical picture that vNOTES has the potential to offer an ideal solution. As a scarless, endoscopic approach capable of meeting the oncologic objectives of prophylactic surgery, vNOTES may reduce the psychological and physical barriers that currently delay or deter risk-reducing interventions.
4. Principles and Technical Aspects of vNOTES
At its core, vNOTES provides direct access to the peritoneal cavity through the posterior vaginal fornix. The approach is both anatomically elegant and technically innovative, bypassing the need for abdominal incisions while preserving the visual and instrumental advantages of endoscopic surgery.
The procedure begins with a colpotomy, typically in the posterior fornix, through which a multi-channel single-port device is installed. Carbon dioxide insufflation creates pneumoperitoneum, and a laparoscopic camera provides visualization. Through the same port, standard laparoscopic instruments are used to perform adnexal surgery, hysterectomy, or combined procedures, with surgical steps nearly identical to those of transabdominal laparoscopy [
20].
In risk-reducing surgery, vNOTES must be adapted to meet oncologic standards. A clear view of the pelvic and lower abdominal peritoneum is essential, especially in BRCA carriers, where detailed inspection of the fimbrial ends of the fallopian tubes is critical due to the risk of occult serous tubal intraepithelial carcinoma lesions (STICs) [
13]. Regarding tissue processing, we emphasize the SEE-FIM, which is a protocol used to detect early, non-invasive precancerous lesions—particularly STICs—in the fallopian tubes of high-risk women, such as BRCA mutation carriers. It involves amputating the fimbrial (distal) end of the tube, serially sectioning it at 2–3 mm intervals, embedding all slices in paraffin, and performing detailed histologic examination. This method increases the likelihood of identifying microscopic lesions that may otherwise go undetected with routine sectioning [
21].
Tissue retrieval must follow strict protocols; all specimens should be placed in endobags before removal to prevent potential cancer cell spillage [
22,
23].
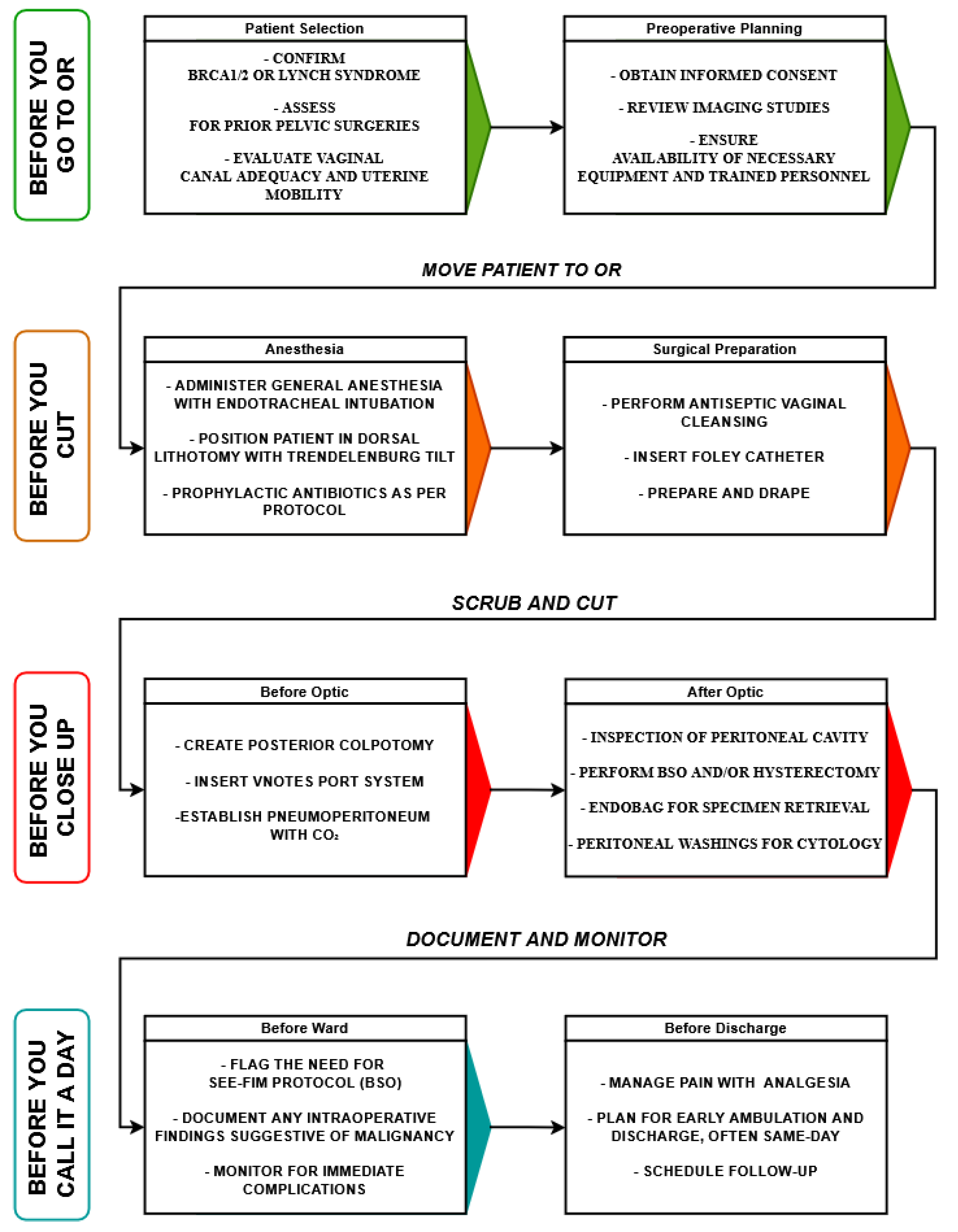
To ensure safe and standardized implementation of vNOTES in risk-reducing gynecologic surgery, a procedural workflow has been proposed and summarized in
Figure 2.
The diagram follows a stepwise patient journey from preoperative assessment to postoperative discharge. Key stages are color-coded and grouped by surgical phases: Before You Go to OR includes patient selection and preoperative planning, ensuring appropriate genetic confirmation, surgical risk assessment, and logistical preparation. Before You Cut focuses on anesthesia induction, patient positioning, prophylactic measures, and surgical field preparation. Before You Close Up delineates intraoperative steps divided into pre-optic and post-optic phases, highlighting port insertion, peritoneal inspection, specimen retrieval in endobags, and cytological sampling. Before You Call it a Day emphasizes critical oncologic steps, including adherence to the SEE-FIM protocol and documentation of findings, along with postoperative care, pain management, early mobilization, discharge planning, and follow-up scheduling. This structured pathway reinforces procedural safety, oncologic rigor, and patient-centered recovery within vNOTES.
5. Clinical Applications of vNOTES in Prophylactic Oncology
5.1. RRSO in BRCA Mutation Carriers
RRSO reduces the risk of tubo-ovarian cancer by over 80% and modestly decreases breast cancer risk when performed before menopause. Several growing case series have demonstrated the feasibility and safety of vNOTES-RRSO in BRCA mutation carriers [
1].
From the patient perspective, vNOTES offers significant benefits in terms of postoperative recovery and satisfaction. One prospective cohort study of BRCA carriers undergoing vNOTES-RRSO reported that over 90% of patients were discharged within 12 h postoperatively, with significantly lower analgesic requirements compared to matched laparoscopic controls [
24]. Moreover, the cosmetic advantage of a truly scarless approach is highly valued by this younger patient population.
5.2. Prophylactic Hysterectomy ± BSO in Lynch Syndrome
While risk-reducing surgery in BRCA mutation carriers primarily targets the adnexa, women with Lynch syndrome face a distinct cancer risk profile, including a markedly increased lifetime risk of both endometrial and ovarian cancer. Consequently, prophylactic hysterectomy with or without BSO is recommended once childbearing is complete [
25,
26,
27].
Traditionally performed via laparoscopic or robotic routes, hysterectomy has long been feasible via the vaginal approach. However, conventional vaginal hysterectomy can be limited by uterine size, prior surgeries, or lack of descent.
In the specific context of Lynch syndrome, where lymphadenectomy is not routinely indicated in purely preventive surgeries, vNOTES hysterectomy with or without BSO offers a safe and patient-centered alternative. Early feasibility studies suggest that vNOTES can achieve comparable operative times, complication rates, and patient outcomes to conventional laparoscopy [
28,
29].
6. Surgical Outcomes, Oncologic Safety, and Summary of Key Clinical Studies
As with any emerging surgical approach, the credibility of vNOTES in the setting of risk-reducing gynecologic oncology depends on its ability to match the oncologic safety and surgical efficacy established by conventional minimally invasive methods [
1,
30,
31].
Below is a synthesis of selected studies that provide valuable outcome data—ranging from surgical safety to quality of life—and offer comparison points with traditional laparoscopic or vaginal approaches (
Table 1).
In a large-scale, multicenter observational study, Housmans et al. (2020) reported outcomes from the International vNOTES Registry (iNOTES), which included over 1000 patients undergoing vNOTES procedures, the majority of which were hysterectomies. The overall complication rate was 5.2%, comprising 1.4% intraoperative and 3.8% postoperative complications. While blood loss and hospital stay were not consistently reported across all cases, the study confirmed the broad feasibility and acceptability of vNOTES in a wide patient population. Notably, the authors emphasized the low conversion rate and the reproducibility of the technique across multiple centers and surgeons [
6].
Another prospective study conducted by Kim et al. (2024) compared 33 women undergoing vNOTES hysterectomy with 40 patients undergoing single-port access (SPA) laparoscopy, all performed by a single experienced surgeon. The groups were similar in age and BMI. The vNOTES group had significantly lower pain scores at 12 h postoperatively (mean VAS score: 2.7 vs. 4.2,
p < 0.001). One ureteral injury occurred in the vNOTES group, while no intraoperative complications were reported in the SPA laparoscopy group. The findings support the conclusion that vNOTES may offer superior early postoperative pain control [
32].
A meta-analysis of 13 studies including 1340 patients was published by Yang et al. (2019), directly comparing vNOTES to conventional laparoscopic surgery found that vNOTES was associated with significantly shorter operative times (mean difference: −10.2 min,
p < 0.01), less blood loss (mean difference: −28.5 mL,
p < 0.01), and shorter hospital stay (mean difference: −0.6 days,
p = 0.03). Additionally, vNOTES patients experienced lower pain scores on postoperative days 1 through 3 (
p < 0.001). Importantly, no significant differences in complication rates were found between the two approaches, suggesting that vNOTES offers a safer, less invasive alternative without compromising outcomes [
33].
In a randomized controlled trial comparing 30 patients undergoing vNOTES hysterectomy and 30 undergoing conventional vaginal hysterectomy (CVH), Lowenstein et al. (2024) reported that blood loss was significantly lower in the vNOTES group (mean: 60 mL vs. 143 mL,
p < 0.01). No complications occurred in the vNOTES group, while 10% of patients in the CVH group experienced intraoperative or early postoperative complications. While pain scores were similar between groups, the study found that vNOTES procedures had shorter operative durations and greater procedural precision, especially in patients requiring concurrent pelvic reconstruction [
34].
Another retrospective study by Goldenberg et al. (2022) included 46 patients, some of whom were BRCA mutation carriers undergoing risk-reducing surgery. The overall complication rate was 4.3%, with no major adverse events or conversions to open surgery. Though hospital stay and blood loss were not consistently reported, the authors emphasized the applicability of vNOTES in oncologic risk contexts, including cases with endometriosis and prior surgeries. The study supports the technique’s extension into more complex or high-risk surgical indications [
35].
While not focused on oncologic prevention, one study by Liu et al. (2019) is valuable for its detailed assessment of postoperative quality of life following vNOTES sacrocolpopexy in 26 patients. Using the Pelvic Floor Impact Questionnaire, patients reported significant improvements in urinary and pelvic symptoms following vNOTES [
36].
Lathouras et al. (2019) presented a case of a 52-year-old BRCA1 mutation carrier who underwent prophylactic BSO via vNOTES. The procedure was completed without complications, with intact specimen retrieval and same-day discharge. The patient reported high satisfaction with cosmetic and recovery outcomes, highlighting the feasibility of vNOTES for preventive surgery in high-risk patients [
37].
Hurni et al. (2022) described two cases where vNOTES was used for surgical staging in presumed early-stage ovarian cancer. The transvaginal approach allowed for peritoneal washings, pelvic inspection, and biopsy collection without conversion. Although para-aortic access was limited, both procedures were completed safely, suggesting vNOTES may be applicable in selected diagnostic and early oncologic contexts [
38].
Based on the current literature, we highlight the qualitative comparison between vNOTES and other surgical approaches (
Table 2).
vNOTES offers notable advantages in cosmetic outcomes and postoperative recovery, with the added benefit of reduced instrumentation costs. While comprehensive cost-effectiveness analyses of vNOTES are still emerging, preliminary studies suggest potential economic advantages over conventional laparoscopic approaches. vNOTES may reduce operative times, hospital stays, and postoperative complications, leading to decreased healthcare costs. Additionally, the technique eliminates the need for abdominal incisions, potentially reducing the use of disposable instruments and associated expenses. However, some analyses indicate that initial procedural costs for vNOTES can be higher than those for traditional laparoscopy, underscoring the need for further research to assess long-term cost-effectiveness [
39].
However, it does have limitations in accessing upper abdominal structures, which may restrict its application in staging or advanced oncologic procedures. In contrast, laparoscopy and robotic-assisted surgery offer broad anatomic access but at higher cost and resource intensity. Conventional vaginal surgery remains cost-effective and cosmetically favorable but may be limited by anatomic constraints and reduced intraoperative visualization. These comparisons underscore the importance of tailoring surgical approaches based on patient risk profile, anatomical considerations, and institutional capabilities.
Another key challenge is the learning curve, which requires proficiency in both vaginal and laparoscopic surgery. While data suggest that proficiency can be reached after approximately 20–30 cases, access to formalized training programs remains limited and inconsistent across institutions [
30,
40,
41].
While the current review focuses on the application of vNOTES in prophylactic gynecologic oncology, it is important to acknowledge ongoing debate regarding its broader use in diagnostic or therapeutic oncologic surgery. Technical limitations, such as restricted access to the retroperitoneum and upper abdominal quadrants, present significant challenges—particularly in the presence of adhesions, endometriosis, or peritoneal carcinomatosis. These anatomical constraints may compromise peritoneal inspection or lymph node assessment, thereby limiting the oncologic completeness of staging procedures. Until further data emerge, its use should remain restricted to well-selected patients and primarily for prophylactic purposes, where oncologic staging is not required.
7. Limitations and Future Prospects
Despite the promising evidence supporting the feasibility and safety of vNOTES in risk-reducing gynecologic surgery, several important limitations must be acknowledged. First, the current body of literature is predominantly composed of retrospective series, case reports, and small prospective cohorts, with a notable paucity of randomized controlled trials specifically evaluating vNOTES in hereditary cancer prevention contexts. This limits the generalizability and strength of the conclusions that can be drawn, particularly regarding long-term oncologic outcomes and recurrence rates. Furthermore, the absence of structured, long-term follow-up data regarding patient-centered outcomes such as sexual function, pelvic floor integrity, and quality of life after vNOTES in risk-reducing contexts remains a critical gap. These parameters are particularly relevant given the preventive, asymptomatic profile of the patient population undergoing such procedures. Looking forward, there is a clear need for well-designed, multicenter randomized trials comparing vNOTES with conventional laparoscopic or robotic approaches in risk-reducing surgery, with a focus on both oncologic and patient-reported outcomes. Additionally, integration of vNOTES into broader personalized cancer prevention strategies will require interdisciplinary collaboration, standardized procedural pathways, and health-economic evaluations to clarify its cost-effectiveness relative to established techniques.
A major limitation of this review is the small number of studies (n = 8) eligible for inclusion, which restricts the generalizability of our conclusions. Moreover, the included studies were heterogeneous in multiple domains: surgical approach (pure vNOTES vs. hybrid), patient populations (BRCA vs. Lynch vs. general oncologic), procedural type (RRSO, hysterectomy, or both), and follow-up durations. This heterogeneity precluded meaningful subgroup analyses or meta-analytical pooling. These limitations highlight the need for greater harmonization in future study designs and multicenter collaborations that enable more robust statistical comparisons, including stratified analyses by genetic mutation type, procedure type, and institutional surgical expertise.
8. Conclusions
vNOTES represents a promising advancement in minimally invasive approaches for risk-reducing gynecologic surgery in women with hereditary cancer syndromes. Current evidence supports its feasibility, safety, and favorable perioperative outcomes, including reduced postoperative pain, faster recovery, and high patient satisfaction, while maintaining adherence to oncologic surgical standards. Despite these advantages, limitations such as the learning curve and restricted upper abdominal access necessitate careful patient selection and, in some cases, hybrid approaches. Further research is warranted to standardize surgical protocols, assess long-term oncologic safety, and clarify the cost-effectiveness of vNOTES in this preventive context. As surgical strategies continue to evolve within personalized cancer prevention programs, vNOTES may offer an important, patient-centered option that aligns with both surgical and psychosocial priorities.
Author Contributions
Conceptualization, V.B.B., D.N., and A.R.; methodology, V.B.B., D.M.Ș., and M.I.; software, S.C., E.L.R., and S.O.; validation, N.N., S.O., and I.S.; formal analysis, E.L.R., S.C., and N.N.; investigation, A.R., L.T., and V.B.B.; resources, L.T., S.C., and S.O.; data curation, M.I., S.O., and N.N.; writing—original draft preparation, V.B.B. and D.M.Ș.; writing—review and editing, I.S., M.I., and D.M.Ș.; visualization, D.M.Ș., V.B.B., and I.S.; supervision, I.S. and D.M.Ș.; project administration, V.B.B. and M.I.; funding acquisition, E.L.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research did not receive any external funding.
Data Availability Statement
The raw data supporting the conclusions and results of this article will be made available on request.
Acknowledgments
We would like to acknowledge Victor Babes University of Medicine and Pharmacy Timisoara for their support in covering the costs of publication of this research paper.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
| vNOTES | Vaginal Natural Orifice Transluminal Endoscopic Surgery |
| BRCA | Breast Cancer gene (BRCA1, BRCA2) |
| RRSO | Risk-Reducing Salpingo-Oophorectomy |
| SEE-FIM | Sectioning and Extensively Examining the FIMbriated End |
| STIC | Serous Tubal Intraepithelial Carcinoma |
| BSO | Bilateral Salpingo-Oophorectomy |
| HBOC | Hereditary Breast and Ovarian Cancer |
| MMR | Mismatch Repair |
| NCCN | National Comprehensive Cancer Network |
| ESGO | European Society of Gynecological Oncology |
| SPA | Single-Port Access |
| CVH | Conventional Vaginal Hysterectomy |
| QoL | Quality of Life |
| VAS | Visual Analog Scale |
| PFIQ | Pelvic Floor Impact Questionnaire |
| RCT | Randomized Controlled Trial |
| iNOTES | International vNOTES Registry |
References
- Wang, Y.; Song, Z.; Zhang, S.; Wang, X.; Li, P. Risk-reducing salpingo-oophorectomy and breast cancer risk in BRCA1 or BRCA2 mutation carriers: A systematic review and meta-analysis. Eur. J. Surg. Oncol. (EJSO) 2022, 48, 1209–1216. [Google Scholar] [CrossRef]
- Li, X.; You, R.; Wang, X.; Liu, C.; Xu, Z.; Zhou, J.; Yu, B.; Xu, T.; Cai, H.; Zou, Q. Effectiveness of Prophylactic Surgeries in BRCA1 or BRCA2 Mutation Carriers: A Meta-analysis and Systematic Review. Clin. Cancer Res. 2016, 22, 3971–3981. [Google Scholar] [CrossRef]
- Sroczynski, G.; Gogollari, A.; Conrads-Frank, A.; Hallsson, L.R.; Pashayan, N.; Widschwendter, M.; Siebert, U. Cost-Effectiveness of Early Detection and Prevention Strategies for Endometrial Cancer-A Systematic Review. Cancers 2020, 12, 1874. [Google Scholar] [CrossRef] [PubMed]
- Jerbaka, M.; Laganà, A.S.; Petousis, S.; Mjaess, G.; Ayed, A.; Ghezzi, F.; Terzic, S.; Sleiman, Z. Outcomes of robotic and laparoscopic surgery for benign gynaecological disease: A systematic review. J. Obstet. Gynaecol. 2022, 42, 1635–1641. [Google Scholar] [CrossRef] [PubMed]
- Bahadur, A.; Zaman, R.; Mundhra, R.; Mani, K. Robotic-assisted Versus Conventional Laparoscopic Hysterectomy for Benign Gynecological Conditions: A Systematic Review and Meta-analysis. J. Mid Life Health 2024, 15, 91–98. [Google Scholar] [CrossRef]
- Housmans, S.; Noori, N.; Kapurubandara, S.; Bosteels, J.J.A.; Cattani, L.; Alkatout, I.; Deprest, J.; Baekelandt, J. Systematic Review and Meta-Analysis on Hysterectomy by Vaginal Natural Orifice Transluminal Endoscopic Surgery (vNOTES) Compared to Laparoscopic Hysterectomy for Benign Indications. J. Clin. Med. 2020, 9, 3959. [Google Scholar] [CrossRef] [PubMed]
- Marchand, G.J.; Masoud, A.T.; Ulibarri, H.; Arroyo, A.; Moir, C.; Blanco, M.; Herrera, D.G.; Hamilton, B.; Ruffley, K.; Petersen, M.; et al. Systematic review and meta-analysis of vaginal natural orifice transluminal endoscopic surgery vs laparoscopic hysterectomy. AJOG Glob. Rep. 2024, 4, 100320. [Google Scholar] [CrossRef]
- Kershaw, V.; Hickey, I.; Wyld, L.; Jha, S. The impact of risk reducing bilateral salpingo-oophorectomy on sexual function in BRCA1/2 mutation carriers and women with Lynch syndrome: A systematic review and meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021, 265, 7–17. [Google Scholar] [CrossRef]
- Rabban, J.T.; Crawford, B.; Chen, L.M.; Powell, C.B.; Zaloudek, C.J. Transitional cell metaplasia of fallopian tube fimbriae: A potential mimic of early tubal carcinoma in risk reduction salpingo-oophorectomies from women With BRCA mutations. Am. J. Surg. Pathol. 2009, 33, 111–119. [Google Scholar] [CrossRef]
- Friebel, T.M.; Domchek, S.M.; Rebbeck, T.R. Modifiers of cancer risk in BRCA1 and BRCA2 mutation carriers: Systematic review and meta-analysis. J. Natl. Cancer Inst. 2014, 106, dju091. [Google Scholar] [CrossRef]
- Matanes, E.; Volodarsky-Perel, A.; Eisenberg, N.; Rottenstreich, M.; Yasmeen, A.; Mitric, C.; Lau, S.; Salvador, S.; Gotlieb, W.H.; Kogan, L. Endometrial Cancer in Germline BRCA Mutation Carriers: A Systematic Review and Meta-analysis. J. Minim. Invasive Gynecol. 2021, 28, 947–956. [Google Scholar] [CrossRef] [PubMed]
- Cullinane, C.M.; Creavin, B.; O’Connell, E.P.; Kelly, L.; O’Sullivan, M.J.; Corrigan, M.A.; Redmond, H.P. Risk of colorectal cancer associated with BRCA1 and/or BRCA2 mutation carriers: Systematic review and meta-analysis. Br. J. Surg. 2020, 107, 951–959. [Google Scholar] [CrossRef]
- Roche, K.C.L.; Abu-Rustum, N.R.; Nourmoussavi, M.; Zivanovic, O. Risk-Reducing Salpingectomy: Let Us Be Opportunistic. Cancer 2017, 123, 1714–1720. [Google Scholar] [CrossRef]
- Wilhite, A.M.; Oestreich, M.C.; Olson, M.; Bedell, S.M.; Westenberg, D.; Bangdiwala, A.; Ikramuddin, S.; Sanchez-Avila, M.; Madoff, R.D.; Khalifa, M.A.; et al. Health Care Provider Adherence to Surgical Guidelines for Risk-Reducing Salpingo-Oophorectomy. Obstet. Gynecol. 2019, 134, 520–526. [Google Scholar] [CrossRef] [PubMed]
- Power, R.F.; Doherty, D.E.; Parker, I.; Gallagher, D.J.; Lowery, M.A.; Cadoo, K.A. Modifiable Risk Factors and Risk of Colorectal and Endometrial Cancers in Lynch Syndrome: A Systematic Review and Meta-Analysis. JCO Precis. Oncol. 2024, 8, e2300196. [Google Scholar] [CrossRef]
- Stinton, C.; Jordan, M.; Fraser, H.; Auguste, P.; Court, R.; Al-Khudairy, L.; Madan, J.; Grammatopoulos, D.; Taylor-Phillips, S. Testing strategies for Lynch syndrome in people with endometrial cancer: Systematic reviews and economic evaluation. Health Technol. Assess. 2021, 25, 1–216. [Google Scholar] [CrossRef] [PubMed]
- Auranen, A.; Joutsiniemi, T. A systematic review of gynecological cancer surveillance in women belonging to hereditary nonpolyposis colorectal cancer (Lynch syndrome) families. Acta Obstet. Gynecol. Scand. 2011, 90, 437–444. [Google Scholar] [CrossRef]
- NCCN Guidelines for Patients: Ovarian Cancer. Ovarian Cancer. 2024. Available online: https://www.nccn.org/patients/guidelines/content/PDF/ovarian-patient.pdf (accessed on 13 May 2025).
- NCCN Guidelines for Patients: Genetic Testing for Hereditary Breast, Ovarian, Pancreatic, and Prostate Cancers. 2025. Available online: https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1545 (accessed on 13 May 2025).
- Li, C.-B.; Hua, K.-Q. Transvaginal natural orifice transluminal endoscopic surgery (vNOTES) in gynecologic surgeries: A systematic review. Asian J. Surg. 2020, 43, 44–51. [Google Scholar] [CrossRef]
- Arora, S.; Yelikar, B.R.; Karigoudar, M.H. Evaluation of SEE-FIM (Sectioning and Extensively Examining the FIMbriated End) Protocol in Identifying Fallopian Tube Precursor Lesions in Women with Ovarian Tumors. J. Obstet. Gynecol. India 2019, 69 (Suppl. S2), 153–159. [Google Scholar] [CrossRef]
- El Hajj, H.; Hudry, D.; Gomez, C.M.; Boscher, A.; Duchatelet, M.; Leblanc, E.; Narducci, F. Protected Laparoscopic Large Ovarian Cyst Aspiration: A 5-Step Alternative to Laparotomy. J. Minim. Invasive Gynecol. 2022, 29, 1038–1039. [Google Scholar] [CrossRef]
- Petryshyn, N.; Dražić, T.; Hogendorf, P.; Strzelczyk, J.; Strzałka, A.; Szwedziak, K.; Durczyński, A. Port site metastases a year after initial laparoscopic cholecystectomy. Should the use of retrieval bags during laparoscopic cholecystectomy be the new gold standard? Pol. Przegl. Chir. 2021, 93, 61–65. [Google Scholar] [PubMed]
- (PDF) Comparison of Vaginal Natural Orifice Transluminal Endoscopic Surgery (vNOTES) and Laparoendoscopic Single-Site (LESS) Hysterectomy on Postoperative Pain Reduction: A Randomized Pilot Study. Available online: https://www.researchgate.net/publication/353806007_Comparison_of_Vaginal_Natural_Orifice_Transluminal_Endoscopic_Surgery_vNOTES_and_Laparoendoscopic_Single-Site_LESS_Hysterectomy_on_Postoperative_Pain_Reduction_A_Randomized_Pilot_Study (accessed on 6 May 2025).
- Meyer, L.A.; Broaddus, R.R.; Lu, K.H. Endometrial cancer and Lynch syndrome: Clinical and pathologic considerations. Cancer Control 2009, 16, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Schmeler, K.M.; Lynch, H.T.; Chen, L.-M.; Munsell, M.F.; Soliman, P.T.; Clark, M.B.; Daniels, M.S.; White, K.G.; Boyd-Rogers, S.G.; Conrad, P.G.; et al. Prophylactic surgery to reduce the risk of gynecologic cancers in the Lynch syndrome. N. Engl. J. Med. 2006, 354, 261–269. [Google Scholar] [CrossRef]
- Maudot, C.; Koual, M.; Azaïs, H.; Benoit, L.; Bentivegna, E.; Nguyen-Xuan, H.-T.; Mereaux, J.; Bailleul, A.; Nos, C.; Moliere, D.; et al. [Prophylactic hysterectomy (Lynch syndrome, BRCA and others)]. Bull. Cancer 2025, 112, 326–334. [Google Scholar] [CrossRef] [PubMed]
- Idos, G.; Valle, L. Lynch Syndrome. In GeneReviews®; Adam, M.P., Feldman, J., Mirzaa, G.M., Pagon, R.A., Wallace, S.E., Amemiya, A., Eds.; University of Washington: Seattle, WA, USA, 1993. Available online: http://www.ncbi.nlm.nih.gov/books/NBK1211/ (accessed on 6 May 2025).
- Bekkers, I.P.; Henschen, R.; Smeets, N.A.; van Vliet, H.A.; Damoiseaux, A.; Wassen, M.M. Vaginal assisted NOTES hysterectomy in The Netherlands; A prospective cohort study. Eur. J. Obstet. Gynecol. Reprod. Biol. X 2024, 23, 100323. [Google Scholar] [CrossRef] [PubMed]
- Feng, D.; Liu, T.; Li, X.; Huang, L.; Xiao, L.; He, L.; Lin, Y. Learning curve analysis of transvaginal natural orifice transluminal endoscopic surgery in treating ovarian cysts: A retrospective cohort study. BMC Women’s Health 2024, 24, 424. [Google Scholar] [CrossRef] [PubMed]
- Kaya, C.; Yıldız, Ş.; Alay, I.; Aslan, Ö.; Aydıner, İ.E.; Yaşar, L. The Comparison of Surgical Outcomes following Laparoscopic Hysterectomy and vNOTES Hysterectomy in Obese Patients. J. Investig. Surg. 2022, 35, 862–867. [Google Scholar] [CrossRef]
- Kim, J.C.; Yim, G.W.; Kim, Y.T. Clinical relevance of vaginal natural orifice transluminal endoscopic surgery (vNOTES) in gynecology. Obstet. Gynecol. Sci. 2024, 67, 199–211. [Google Scholar] [CrossRef]
- Yang, E.; Nie, D.; Li, Z. Comparison of Major Clinical Outcomes Between Transvaginal NOTES and Traditional Laparoscopic Surgery: A Systematic Review and Meta-analysis. J. Surg. Res. 2019, 244, 278–290. [Google Scholar] [CrossRef]
- Lowenstein, L.; Mor, O.; Matanes, E.; Justman, N.; Stuart, A.; Baekelandt, J. Conventional vaginal approach vs. transvaginal natural orifice transluminal endoscopic surgery for treating apical prolapse, a randomized controlled study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2024, 303, 180–185. [Google Scholar] [CrossRef]
- Goldenberg, M.; Revivo, P.E.; Gurevitch, S.; Mashiach, R.; Mohr-Sasson, A. Risk-reducing bilateral salpingo-oopherectomy for BRCA mutation carriers via the transvaginal natural orifice transluminal endoscopic surgery approach. Int. J. Gynaecol. Obstet. 2022, 158, 764–765. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Kohn, J.; Fu, H.; Guan, Z.; Guan, X. Transvaginal natural orifice transluminal endoscopic surgery for sacrocolpopexy: A pilot study of 26 cases. J. Minim. Invasive Gynecol. 2019, 26, 748–753. [Google Scholar] [CrossRef] [PubMed]
- Lathouras, K.; Saso, S.; Jones, B.P.; Bowden, S.; Kyrgiou, M.; Stienen-Durand, A.; Beynon, G. Transvaginal laparoscopic salpingo-oophorectomy: An oncological risk-reducing procedure. Futur. Sci. OA 2019, 6, FSO429. [Google Scholar] [CrossRef]
- Hurni, Y.; Romito, F.; Huber, D. Transvaginal Natural Orifice Transluminal Endoscopic Surgery for Surgical Staging of Early-Stage Ovarian Cancers: A Report of Two Cases. Front. Surg. 2022, 9, 833126. [Google Scholar] [CrossRef] [PubMed]
- Nef, J.; Hurni, Y.; Simonson, C.; Fournier, I.; Di Serio, M.; Lachat, R.; Bodenmann, P.; Seidler, S.; Huber, D. Safety and efficacy of transvaginal natural orifice endoscopic surgery (vNOTES) for gynecologic procedures in the elderly: A case series of 119 consecutive patients. Eur. J. Obstet. Gynecol. Reprod. Biol. 2025, 308, 23–28. [Google Scholar] [CrossRef]
- Mereu, L.; Pecorino, B.; Ferrara, M.; Siniscalchi, M.; Garraffa, G.; D’Agate, M.G.; Scollo, P. Cumulative Sum Analysis of Learning Curve Process for Vaginal Natural Orifice Transluminal Endoscopic Surgery Hysterectomy. J. Minim. Invasive Gynecol. 2023, 30, 582–586. [Google Scholar] [CrossRef]
- Wang, C.-J.; Go, J.; Huang, H.-Y.; Wu, K.-Y.; Huang, Y.-T.; Liu, Y.-C.; Weng, C.H. Learning curve analysis of transvaginal natural orifice transluminal endoscopic hysterectomy. BMC Surg. 2019, 19, 88. [Google Scholar] [CrossRef]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).