Green Endoscopy: A Review of Global Perspectives on Environmental Sustainability of Gastrointestinal Endoscopy
Abstract
1. Introduction
2. Environmental and Digestive Health Impact of GI-Related Emissions
3. Sustainable Endoscopy Principles
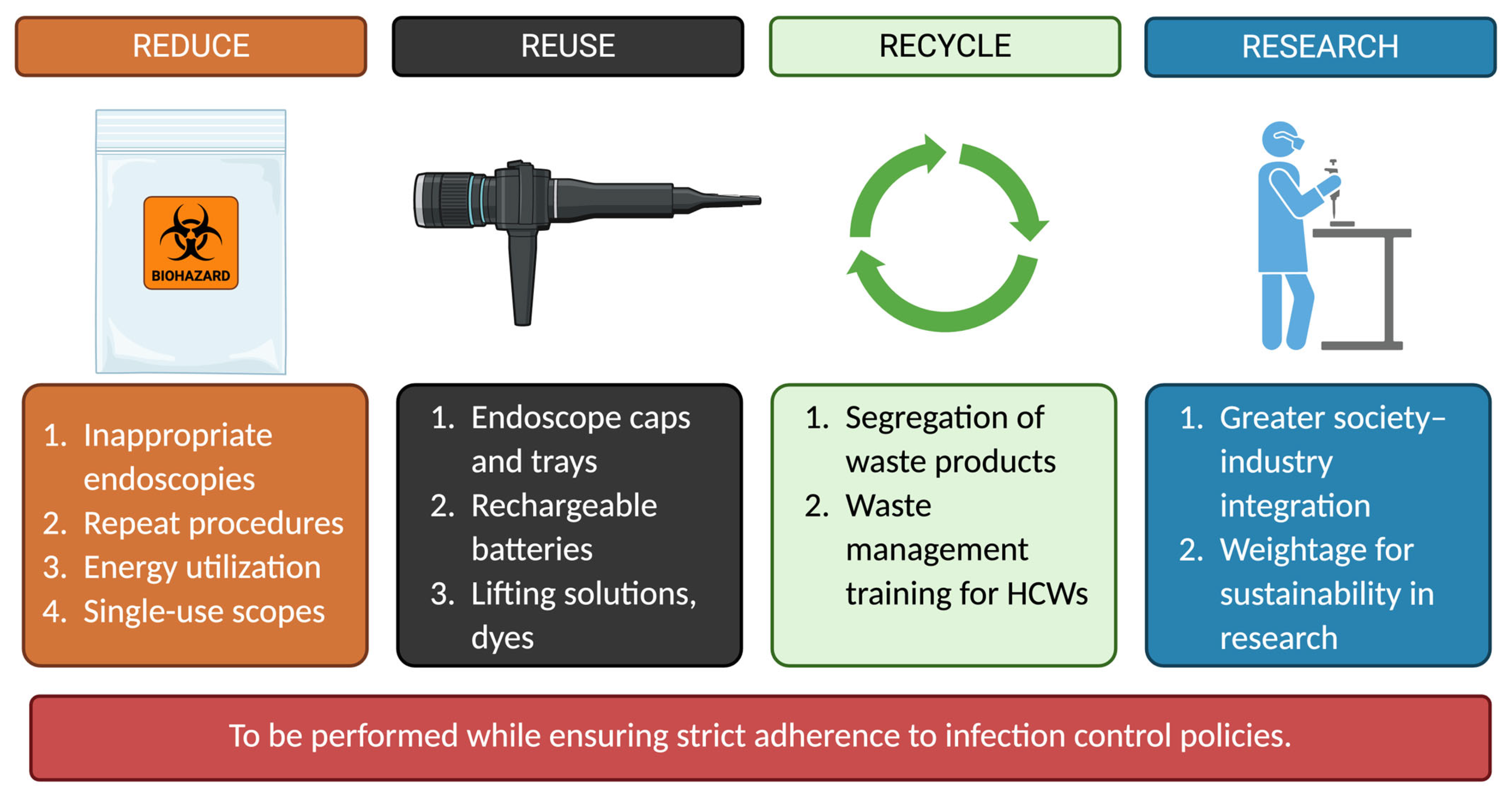
3.1. Current Global Perspectives on Green Endoscopy
3.2. Overcoming Challenges to a Greener Future
3.3. Role of Technology in Sustainability
3.4. Endoscopy in Specific Settings
4. Expert Commentary
5. Conclusions
Funding
Conflicts of Interest
References
- Lenzen, M.; Malik, A.; Li, M.; Fry, J.; Weisz, H.; Pichler, P.-P.; Chaves, L.S.M.; Capon, A.; Pencheon, D. The Environmental Footprint of Health Care: A Global Assessment. Lancet Planet. Health 2020, 4, e271–e279. [Google Scholar] [CrossRef]
- Storr, J.; Twyman, A.; Zingg, W.; Damani, N.; Kilpatrick, C.; Reilly, J.; Price, L.; Egger, M.; Grayson, M.L.; Kelley, E.; et al. Core Components for Effective Infection Prevention and Control Programmes: New WHO Evidence-Based Recommendations. Antimicrob. Resist. Infect. Control 2017, 6, 6. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.S.; Frantzis, I.; Abeles, S.R. Greening Infection Prevention and Control: Multifaceted Approaches to a Sustainable Future. Open Forum Infect. Dis. 2025, 12, ofae371. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, L.V.; Agrawal, D.; Skole, K.S.; Crockett, S.D.; Shimpi, R.A.; Renteln, D.v.; Pohl, H. Meeting the Environmental Challenges of Endoscopy: A Pathway from Strategy to Implementation. Gastrointest. Endosc. 2023, 98, 881–888.e1. [Google Scholar] [CrossRef] [PubMed]
- Crippa, M.; Guizzardi, D.; Muntean, M.; Schaaf, E.; Solazzo, E.; Monforti-Ferrario, F.; Olivier, J.G.J.; Vignati, E. Fossil CO2 and GHG Emissions of All World Countries: 2020 Report; Publications Office of the European Union: Luxembourg, 2020; ISBN 978-92-76-21515-8. [Google Scholar]
- Namburar, S.; von Renteln, D.; Damianos, J.; Bradish, L.; Barrett, J.; Aguilera-Fish, A.; Cushman-Roisin, B.; Pohl, H. Estimating the Environmental Impact of Disposable Endoscopic Equipment and Endoscopes. Gut 2022, 71, 1326–1331. [Google Scholar] [CrossRef]
- Tomson, C. Reducing the Carbon Footprint of Hospital-Based Care. Future Hosp. J. 2015, 2, 57–62. [Google Scholar] [CrossRef]
- Pichler, P.-P.; Jaccard, I.S.; Weisz, U.; Weisz, H. International Comparison of Health Care Carbon Footprints. Environ. Res. Lett. 2019, 14, 064004. [Google Scholar] [CrossRef]
- Eckelman, M.J.; Sherman, J.D. Estimated Global Disease Burden From US Health Care Sector Greenhouse Gas Emissions. Am. J. Public Health 2018, 108, S120–S122. [Google Scholar] [CrossRef]
- Keil, M.; Frehse, L.; Hagemeister, M.; Knieß, M.; Lange, O.; Kronenberg, T.; Rogowski, W. Carbon Footprint of Healthcare Systems: A Systematic Review of Evidence and Methods. BMJ Open 2024, 14, e078464. [Google Scholar] [CrossRef]
- Peery, A.F.; Crockett, S.D.; Murphy, C.C.; Lund, J.L.; Dellon, E.S.; Williams, J.L.; Jensen, E.T.; Shaheen, N.J.; Barritt, A.S.; Lieber, S.R.; et al. Burden and Cost of Gastrointestinal, Liver, and Pancreatic Diseases in the United States: Update 2018. Gastroenterology 2019, 156, 254–272.e11. [Google Scholar] [CrossRef]
- Leffler, D.A.; Kheraj, R.; Garud, S.; Neeman, N.; Nathanson, L.A.; Kelly, C.P.; Sawhney, M.; Landon, B.; Doyle, R.; Rosenberg, S.; et al. The Incidence and Cost of Unexpected Hospital Use after Scheduled Outpatient Endoscopy. Arch. Intern. Med. 2010, 170, 1752–1757. [Google Scholar] [CrossRef] [PubMed]
- Vaccari, M.; Tudor, T.; Perteghella, A. Costs Associated with the Management of Waste from Healthcare Facilities: An Analysis at National and Site Level. Waste Manag. Res. 2018, 36, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Desai, M.; Campbell, C.; Perisetti, A.; Srinivasan, S.; Radadiya, D.; Patel, H.; Melquist, S.; Rex, D.K.; Sharma, P. The Environmental Impact of Gastrointestinal Procedures: A Prospective Study of Waste Generation, Energy Consumption, and Auditing in an Endoscopy Unit. Gastroenterology 2024, 166, 496–502.e3. [Google Scholar] [CrossRef] [PubMed]
- Koo, T.H.; Tee, V.; Lee, Y.Y.; Roslan, N.S.; Ibrahim, Y.S. Green Endoscopy and Sustainable Practices: A Scoping Review. J. Dig. Endosc. 2024, 15, 184–191. [Google Scholar] [CrossRef]
- Malik, A.; Lenzen, M.; McAlister, S.; McGain, F. The Carbon Footprint of Australian Health Care. Lancet Planet. Health 2018, 2, e27–e35. [Google Scholar] [CrossRef]
- Patz, J.A.; Epstein, P.R.; Burke, T.A.; Balbus, J.M. Global Climate Change and Emerging Infectious Diseases. JAMA 1996, 275, 217–223. [Google Scholar] [CrossRef]
- Rocklöv, J.; Dubrow, R. Climate Change: An Enduring Challenge for Vector-Borne Disease Prevention and Control. Nat. Immunol. 2020, 21, 479–483. [Google Scholar] [CrossRef]
- Leddin, D.; Omary, M.B.; Veitch, A.; Metz, G.; Amrani, N.; Aabakken, L.; Ali, R.A.R.; Alvares-da-Silva, M.R.; Armstrong, D.; Boyacioglu, S.; et al. Uniting the Global Gastroenterology Community to Meet the Challenge of Climate Change and Nonrecyclable Waste. J. Clin. Gastroenterol. 2021, 55, 823. [Google Scholar] [CrossRef]
- Pohl, H.; de Latour, R.; Reuben, A.; Ahuja, N.K.; Gayam, S.; Kohli, R.; Agrawal, D.; Omary, M.B. GI Multisociety Strategic Plan on Environmental Sustainability. Gastroenterology 2022, 163, 1695–1701.e2. [Google Scholar] [CrossRef]
- Ibrahim, Y.S.; Tuan Anuar, S.; Azmi, A.A.; Wan Mohd Khalik, W.M.A.; Lehata, S.; Hamzah, S.R.; Ismail, D.; Ma, Z.F.; Dzulkarnaen, A.; Zakaria, Z.; et al. Detection of Microplastics in Human Colectomy Specimens. JGH Open 2021, 5, 116–121. [Google Scholar] [CrossRef]
- Sebastian, S.; Dhar, A.; Baddeley, R.; Donnelly, L.; Haddock, R.; Arasaradnam, R.; Coulter, A.; Disney, B.R.; Griffiths, H.; Healey, C.; et al. Green Endoscopy: British Society of Gastroenterology (BSG), Joint Accreditation Group (JAG) and Centre for Sustainable Health (CSH) Joint Consensus on Practical Measures for Environmental Sustainability in Endoscopy. Gut 2023, 72, 12–26. [Google Scholar] [CrossRef] [PubMed]
- Ang, T.L.; Hang, D.V.; Li, J.W.; Ho, J.C.L.; Sy-Janairo, M.L.; Raja Ali, R.A.; Makharia, G.K.; Sundaram, S.; Chantarojanasiri, T.; Kim, H.-G.; et al. APAGE Position Statements on Green and Sustainability in Gastroenterology, Hepatology, and Gastrointestinal Endoscopy. J. Gastroenterol. Hepatol. 2025, 40, 821–831. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez de Santiago, E.; Dinis-Ribeiro, M.; Pohl, H.; Agrawal, D.; Arvanitakis, M.; Baddeley, R.; Bak, E.; Bhandari, P.; Bretthauer, M.; Burga, P.; et al. Reducing the Environmental Footprint of Gastrointestinal Endoscopy: European Society of Gastrointestinal Endoscopy (ESGE) and European Society of Gastroenterology and Endoscopy Nurses and Associates (ESGENA) Position Statement. Endoscopy 2022, 54, 797–826. [Google Scholar] [CrossRef] [PubMed]
- Maida, M.; Vitello, A.; Shahini, E.; Vassallo, R.; Sinagra, E.; Pallio, S.; Melita, G.; Ramai, D.; Spadaccini, M.; Hassan, C.; et al. Green Endoscopy, One Step toward a Sustainable Future: Literature Review. Endosc. Int. Open 2024, 12, E968–E980. [Google Scholar] [CrossRef]
- Petruzziello, L.; Hassan, C.; Alvaro, D.; Kohn, A.; Rossi, Z.; Zullo, A.; Cesaro, P.; Annibale, B.; Barca, A.; Di Giulio, E.; et al. Appropriateness of the Indication for Colonoscopy: Is the Endoscopist the ‘Gold Standard’? J. Clin. Gastroenterol. 2012, 46, 590. [Google Scholar] [CrossRef]
- Rao, A. BioRender. 2025. Available online: https://BioRender.com/n6hvqyo (accessed on 13 April 2025).
- Latour, R.d.; Crockett, S.D.; Palchaudhuri, S.; Skole, K.S.; Agrawal, D.; Hernandez, L.V.; von Renteln, D.; Shimpi, R.A.; Collins, J.; Pohl, H. Practical Steps to Green Your Endoscopy Unit: Appropriate Management of Endoscopic Waste. Gastrointest. Endosc. 2025, 101, 745–750.e3. [Google Scholar] [CrossRef]
- Maurice, J.B.; Siau, K.; Sebastian, S.; Ahuja, N.; Wesley, E.; Stableforth, W.; Hayee, B. Green Endoscopy: A Call for Sustainability in the Midst of COVID-19. Lancet Gastroenterol. Hepatol. 2020, 5, 636–638. [Google Scholar] [CrossRef]
- Kaul, V. Green Endoscopy. Am. J. Gastroenterol. 2024, 119, 1714–1718. [Google Scholar] [CrossRef]
- Menees, S.B.; Powell, C.; Kurlander, J.; Goel, A.; Chey, W.D. A Meta-Analysis of the Utility of C-Reactive Protein, Erythrocyte Sedimentation Rate, Fecal Calprotectin, and Fecal Lactoferrin to Exclude Inflammatory Bowel Disease in Adults with IBS. Am. J. Gastroenterol. 2015, 110, 444–454. [Google Scholar] [CrossRef]
- Levine, D.S.; Haggitt, R.C.; Blount, P.L.; Rabinovitch, P.S.; Rusch, V.W.; Reid, B.J. An Endoscopic Biopsy Protocol Can Differentiate High-Grade Dysplasia from Early Adenocarcinoma in Barrett’s Esophagus. Gastroenterology 1993, 105, 40–50. [Google Scholar] [CrossRef]
- Shaheen, N.J.; Falk, G.W.; Iyer, P.G.; Souza, R.F.; Yadlapati, R.H.; Sauer, B.G.; Wani, S. Diagnosis and Management of Barrett’s Esophagus: An Updated ACG Guideline. Am. J. Gastroenterol. 2022, 117, 559–587. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Russell, D.; Mohamadnejad, M.; Makker, J.; Sedarat, A.; Watson, R.R.; Yang, S.; Hemarajata, P.; Humphries, R.; Rubin, Z.; et al. Risk Factors Associated with the Transmission of Carbapenem-Resistant Enterobacteriaceae via Contaminated Duodenoscopes. Gastrointest. Endosc. 2016, 83, 1121–1129. [Google Scholar] [CrossRef]
- Rahman, M.R.; Perisetti, A.; Coman, R.; Bansal, P.; Chhabra, R.; Goyal, H. Duodenoscope-Associated Infections: Update on an Emerging Problem. Dig. Dis. Sci. 2019, 64, 1409–1418. [Google Scholar] [CrossRef] [PubMed]
- Ramai, D.; Smit, E.; Kani, H.T.; Papaefthymiou, A.; Warner, L.; Chandan, S.; Dhindsa, B.; Facciorusso, A.; Gkolfakis, P.; Ofosu, A.; et al. Cannulation Rates and Technical Performance Evaluation of Commericially Available Single-Use Duodenoscopes for Endoscopic Retrograde Cholangiopancreatography: A Systematic Review and Meta-Analysis. Dig. Liver Dis. Off. J. Ital. Soc. Gastroenterol. Ital. Assoc. Study Liver 2024, 56, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Nabi, Z.; Tang, R.S.Y.; Sundaram, S.; Lakhtakia, S.; Reddy, D.N. Single-Use Accessories and Endoscopes in the Era of Sustainability and Climate Change-A Balancing Act. J. Gastroenterol. Hepatol. 2024, 39, 7–17. [Google Scholar] [CrossRef]
- Le, N.N.T.; Hernandez, L.V.; Vakil, N.; Guda, N.; Patnode, C.; Jolliet, O. Environmental and Health Outcomes of Single-Use versus Reusable Duodenoscopes. Gastrointest. Endosc. 2022, 96, 1002–1008. [Google Scholar] [CrossRef]
- Barakat, M.T.; Ghosh, S.; Banerjee, S. Cost Utility Analysis of Strategies for Minimizing Risk of Duodenoscope-Related Infections. Gastrointest. Endosc. 2022, 95, 929–938.e2. [Google Scholar] [CrossRef]
- Neves, J.A.C.; Santiago, E.R.d.; Pohl, H.; Lorenzo-Zúñiga, V.; Cunha, M.F.; Voiosu, A.M.; Römmele, C.; Penman, D.G.; Albéniz, E.; Siau, K.; et al. Perspectives and Awareness of Endoscopy Healthcare Professionals on Sustainable Practices in Gastrointestinal Endoscopy: Results of the LEAFGREEN Survey. Endoscopy 2024, 56, 355–363. [Google Scholar] [CrossRef]
- Wilcox, C.M.; Waites, K.; Brookings, E.S. Use of Sterile Compared with Tap Water in Gastrointestinal Endoscopic Procedures. Am. J. Infect. Control 1996, 24, 407–410. [Google Scholar] [CrossRef]
- Puterbaugh, M.; Barde, C.; Van Enk, R. Endoscopy Water Source: Tap or Sterile Water? Gastroenterol. Nurs. Off. J. Soc. Gastroenterol. Nurses Assoc. 1997, 20, 203–206. [Google Scholar] [CrossRef]
- Gayam, S. Environmental Impact of Endoscopy: “Scope” of the Problem. Am. J. Gastroenterol. 2020, 115, 1931–1932. [Google Scholar] [CrossRef] [PubMed]
- Naito, S.; Nakamura, I.; Muramatsu, T.; Kagawa, Y.; Fukuzawa, M.; Itoi, T. Micro-Bacterial Assessment of Disposable Gowns with a Focus on Green Endoscopy in Gastrointestinal Endoscopy Procedures: A Japanese Pilot Study for Healthcare Waste Reduction. DEN Open 2025, 5, e70016. [Google Scholar] [CrossRef] [PubMed]
- Mohapatra, S.; Fukami, N. Reloadable Clips Versus Single-Use Repositionable Clips for Closure of Mucosal Incision After Peroral Endoscopic Myotomy (POEM). Gastrointest. Endosc. 2022, 95, AB263. [Google Scholar] [CrossRef]
- Fan, X.; Cai, X.; Jiao, J.; Luo, L.; Maihemuti, A.; Wang, T.; Chen, X.; Zheng, Z.; Liu, W. Efficacy Analysis of Modified Double Band Ligation-Assisted Endoscopic Submucosal Resection and Endoscopic Mucosal Dissection in the Treatment of Gastric Gastrointestinal Stromal Tumors (≤1.5 Cm). Surg. Endosc. 2025, 39, 2471–2480. [Google Scholar] [CrossRef]
- De Jong, D.; Volkers, A.; De Ridder, E.; Neijenhuis, M.; Duijvestein, M. Steps Toward a Greener Endoscopy Unit. Clin. Gastroenterol. Hepatol. 2023, 21, 2723–2726.e2. [Google Scholar] [CrossRef]
- Jeon, T.J.; Cha, J.M. Awareness of Green Endoscopy Is Low among Healthcare Professionals Performing Gastrointestinal Endoscopy. Clin. Endosc. 2024, 57, 836–838. [Google Scholar] [CrossRef]
- Cammarota, G.; Ianiro, G. A Greener Gastroenterology: Challenges and Opportunities for an Eco-Sustainable Approach to Digestive Diseases. Nat. Rev. Gastroenterol. Hepatol. 2024, 21, 744–745. [Google Scholar] [CrossRef]
- Harne, P.S.; Harne, V.; Rehman, A.; Thosani, N.; Desai, M. First Step to Environmentally Sustainable Endoscopy Practice: A Prospective Study of Minimizing Multiple Device Use during Screening Colonoscopy at a Large Tertiary Center. Endoscopy 2024, 57, 500–503. [Google Scholar] [CrossRef]
- Rex, D.K.; Gallagher, J.A.; Lahr, R.E.; Vemulapalli, K.C.; Sharma, P.; Hassan, C. One-Device Colonoscopy: Feasibility, Cost Savings, and Plastic Waste Reduction by Procedure Indication, When Performed by a High Detecting Colonoscopist. Endoscopy 2024, 56, 102–107. [Google Scholar] [CrossRef]
- Duong, D. Improper Disposal of Medical Waste Costs Health Systems and the Environment. CMAJ Can. Med. Assoc. J. 2023, 195, E518–E519. [Google Scholar] [CrossRef]
- Neves, J.A.C.; Roseira, J.; Queirós, P.; Sousa, H.T.; Pellino, G.; Cunha, M.F. Targeted Intervention to Achieve Waste Reduction in Gastrointestinal Endoscopy. Gut 2023, 72, 306–313. [Google Scholar] [CrossRef] [PubMed]
- Anees, A.; Ali, A.; Hassan, S.; Fatima, S.; Jameel, H. Narrow Band Imaging: Important Tool for Early Diagnosis, Management, and Improved Outcomes in Gastrointestinal Lesions. World J. Surg. 2024, 48, 2505–2514. [Google Scholar] [CrossRef] [PubMed]
- Katagiri, A.; Fu, K.-I.; Sano, Y.; Ikematsu, H.; Horimatsu, T.; Kaneko, K.; Muto, M.; Yoshida, S. Narrow Band Imaging with Magnifying Colonoscopy as Diagnostic Tool for Predicting Histology of Early Colorectal Neoplasia. Aliment. Pharmacol. Ther. 2008, 27, 1269–1274. [Google Scholar] [CrossRef] [PubMed]
- MacNeill, A.J.; Hopf, H.; Khanuja, A.; Alizamir, S.; Bilec, M.; Eckelman, M.J.; Hernandez, L.; McGain, F.; Simonsen, K.; Thiel, C.; et al. Transforming The Medical Device Industry: Road Map To A Circular Economy. Health Aff. 2020, 39, 2088–2097. [Google Scholar] [CrossRef]
- Leddin, D.; Galts, C.; McRobert, E.; Igoe, J.; Singh, H.; Sinclair, P. The Carbon Cost of Travel to a Medical Conference: Modelling the Annual Meeting of the Canadian Association of Gastroenterology. J. Can. Assoc. Gastroenterol. 2021, 5, 52–58. [Google Scholar] [CrossRef]
- Nakaji, K. Colon Capsule Endoscopy: Can It Contribute to Green Endoscopy? World J. Gastrointest. Endosc. 2024, 16, 627–631. [Google Scholar] [CrossRef]
- Jalayeri Nia, G.; Arasaradnam, R.P.; Koulaouzidis, A. Clinical Utility of Colon Capsule Endoscopy: A Moving Target? Ther. Adv. Gastroenterol. 2023, 16, 17562848231195680. [Google Scholar] [CrossRef]
- Möllers, T.; Schwab, M.; Gildein, L.; Hoffmeister, M.; Albert, J.; Brenner, H.; Jäger, S. Second-Generation Colon Capsule Endoscopy for Detection of Colorectal Polyps: Systematic Review and Meta-Analysis of Clinical Trials. Endosc. Int. Open 2021, 9, E562–E571. [Google Scholar] [CrossRef]
- Benech, N.; Vinet, O.; Gaudin, J.-L.; Benamouzig, R.; Dray, X.; Ponchon, T.; Galmiche, J.-P.; Sacher-Huvelin, S.; Samaha, E.; Saurin, J.-C.; et al. Colon Capsule Endoscopy in Clinical Practice: Lessons from a National 5-Year Observational Prospective Cohort. Endosc. Int. Open 2021, 9, E1542–E1548. [Google Scholar] [CrossRef]
- Grau, R.; Cottinet, P.-J.; Le, M.-Q.; Schaefer, M.; Wallenhorst, T.; Rösch, T.; Lépilliez, V.; Chaussade, S.; Rivory, J.; Legros, R.; et al. Endoscopic En Bloc Vs Piecemeal Resection of Large Colonic Adenomas: Carbon Footprint Post Hoc Analysis of a Randomized Trial. Clin. Gastroenterol. Hepatol. Off. Clin. Pract. J. Am. Gastroenterol. Assoc. 2025, S1542-3565(25)00150-8. [Google Scholar] [CrossRef]
- Jacques, J.; Schaefer, M.; Wallenhorst, T.; Rösch, T.; Lépilliez, V.; Chaussade, S.; Rivory, J.; Legros, R.; Chevaux, J.-B.; Leblanc, S.; et al. Endoscopic En Bloc Versus Piecemeal Resection of Large Nonpedunculated Colonic Adenomas: A Randomized Comparative Trial. Ann. Intern. Med. 2024, 177, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Henniger, D.; Lux, T.; Windsheimer, M.; Brand, M.; Weich, A.; Kudlich, T.; Schöttker, K.; Hann, A.; Meining, A. Reducing Scope 3 Carbon Emissions in Gastrointestinal Endoscopy: Results of the Prospective Study of the “Green Endoscopy Project Würzburg”. Gut 2024, 73, 442–447. [Google Scholar] [CrossRef] [PubMed]
| Intervention | Environmental Impact | Economic Viability | Feasibility | Resource Accessibility-Based Applicability |
|---|---|---|---|---|
| Clinical appropriateness | Lower energy wastage due to procedural volume stewardship. | High | High | Universal |
| Bundling two or more procedures | Lower human resource and endoscopic suite utilization per patient. | Moderate | Moderate | Resource-abundant |
| Advanced imaging and artificial intelligence | Higher upfront manufacturing energy expenditure but lower downstream logistical utilization. | Low | Low | Resource-abundant |
| Use of reusable equipment | Potential avoidance of emissions during the disposal of single-use equipment. | Moderate | High | Resource-limited |
| Waste sorting and recycling | Appropriate segregation can reduce disposal emissions substantially. | High | High | Universal |
| Water conservation | Low-risk, high-yield energy conservation strategy. | High | High | Resource-limited |
| Energy/resource efficiency | Low-risk, high-yield modifications like motion-sensing lights support sustainability and energy efficiency. | Moderate | High | Universal |
| Innovative device design | Lower per-procedure wastage. | Moderate | Low | Resource-abundant |
| Human resource development (education, training) | Directly or indirectly drives all the above interventions. | High | High | Universal |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rao, A.; Sultany, A.; Gondal, A.; Chakinala, R.C.; Bharadwaj, H.R.; Chandan, S.; Ali, H.; Malik, S.; Alsakarneh, S.; Dahiya, D.S. Green Endoscopy: A Review of Global Perspectives on Environmental Sustainability of Gastrointestinal Endoscopy. J. Clin. Med. 2025, 14, 3936. https://doi.org/10.3390/jcm14113936
Rao A, Sultany A, Gondal A, Chakinala RC, Bharadwaj HR, Chandan S, Ali H, Malik S, Alsakarneh S, Dahiya DS. Green Endoscopy: A Review of Global Perspectives on Environmental Sustainability of Gastrointestinal Endoscopy. Journal of Clinical Medicine. 2025; 14(11):3936. https://doi.org/10.3390/jcm14113936
Chicago/Turabian StyleRao, Adishwar, Abdullah Sultany, Amlish Gondal, Raja Chandra Chakinala, Hareesha Rishab Bharadwaj, Saurabh Chandan, Hassam Ali, Sheza Malik, Saqr Alsakarneh, and Dushyant Singh Dahiya. 2025. "Green Endoscopy: A Review of Global Perspectives on Environmental Sustainability of Gastrointestinal Endoscopy" Journal of Clinical Medicine 14, no. 11: 3936. https://doi.org/10.3390/jcm14113936
APA StyleRao, A., Sultany, A., Gondal, A., Chakinala, R. C., Bharadwaj, H. R., Chandan, S., Ali, H., Malik, S., Alsakarneh, S., & Dahiya, D. S. (2025). Green Endoscopy: A Review of Global Perspectives on Environmental Sustainability of Gastrointestinal Endoscopy. Journal of Clinical Medicine, 14(11), 3936. https://doi.org/10.3390/jcm14113936






